The burden of neuropsychiatric illnesses is enormous. These conditions, which include schizophrenia, mood disorders, and autism, affect thought, emotions, and a person’s very sense of self. Together, they are the leading cause of disability in North America and Europe and constitute 40% of all years lost to disability. In the United States, the cost in lost earnings due to psychiatric disease is estimated conservatively to be $200 billion per year (1). The burden to individuals, families, and society is all the more tragic because these illnesses typically begin early in life, are life-long, and damage the affected individuals’ self-perception, productivity, and ability to relate to others.
Unfortunately, there have been no major breakthroughs in the treatment of schizophrenia in the last 50 years and no major breakthroughs in the treatment of depression in the last 20 years (2). Over the last few decades, drug treatments have emerged that help a subset of these patients (3), but a sizable proportion are resistant to all currently available treatments. This heterogeneity points to the complexity of the underlying biology and underscores the urgent need for a more sophisticated understanding of the causes of these illnesses.
Psychiatric disorders present a unique challenge, even relative to other brain disorders, such as Alzheimer’s, Huntington’s, or Parkinson’s disease, because for psychiatric disorders we know much less about underlying genetic, molecular, and cellular causes oreven the primary anatomical sites of the brain defects. This frustrating lack of progress requires us to confront the complexity of the brain, especially in the context of higher-order functions, such as cognition and mood. This calls for a new perspective and a combination of novel tools and analytical methods.
Disruption of Neural Circuits
Illnesses such as schizophrenia, autism, and mood disorders are likely the result of disruptions of neural circuits, the functional ensembles of brain cells that mediate thought, feelings, and behavior. A defect in the development, anatomical structure, functional integration, or dynamics of such a circuit can lead to a constellation of symptoms.
Given the complexity of neural circuits, there are many possible ways to disrupt them (4). Thousands of genes are involved in regulating neural development and function. It is not surprising, therefore, that disturbances in the structure and function of one or several of these genes can lead to broad and complex neuropsychiatric phenotypes. This complexity explains the high prevalence of neuropsychiatric disorders. It also indicates that many genetic mutations, epigenetic changes, and other cellular and morphological brain lesions can converge on disturbing a given brain circuit and result in shared clinical manifestations (e.g., delusions and hallucinations) that lead to the same clinical diagnosis (e.g., schizophrenia). Thus, starting from a diagnosis and searching broadly for genetic causes that are commonly shared across all affected individuals is not likely to succeed, because a great deal of biological heterogeneity lies at the basis of circuit dysfunction.
This does not mean, however, that these diseases are not genetically based and transmitted, nor does it suggest that the search for genetic causes will be fruitless. Indeed, ample evidence demonstrates the heritability of these disorders. For example, there is much greater concordance of diseased states in identical twins versus fraternal twins. In autism, in as many as 80% of families of identical twins, both display autistic features if one is affected (5).
Concordance of schizophrenia is estimated to be ~50% in identical twins, as opposed to ~5 to 10% in fraternal twins (6, 7). In some persons, nongenetic factors—such as intrauterine infection, malnutrition, or stress—may also be required to trigger the illness (8). Because of these complexities, most of the genes involved in the major psychiatric illnesses have not yet been identified, and animal models for them are limited.
Recent studies indicate that for many patients, psychiatric illnesses are due to genetic vulnerabilities that are shared by affected members of a given family, but vary across families, such that a given family has a unique, or “private,” mutational profile (9). It is therefore critical to focus on approaches that can detect private mutations and will take into account the genetic and neurobiological heterogeneity of psychiatric disorders.
Genomics and Circuit Analysis
What is the best strategy for unraveling the biological causes of psychiatric illnesses? We suggest that their solution will require the integration of two general approaches that have matured dramatically in the last three years: Genomics and Circuit Analysis.
Genomics is the combination of large-scale sequencing with systematic computational analysis of genomes. In the last two years, sequencing the human genome has become significantly faster and much less expensive. This makes it feasible to sequence the complete genome of many afflicted individuals to discover the genetic bases of these disorders within subjects and families. It is no longer necessary to target specific genes or chromosomal regions based on preconceived notions about the nature of the genetic defect. This approach has already proven useful in the analysis of X-linked mental retardation (10). New insight into the complex genetic basis of psychiatric disease comes from recent analysis of gene copy number variants present in patients with autism, schizophrenia, and bipolar disorder (11). Some of these mutations are absent from either parent’s DNA, which suggests that they are de novo mutations. Many deleted or amplified DNA segments contain genes needed primarily for the functioning of nerve cells, not for cells in other tissues. Most of the neural genes thus far identified as mutant have been observed only once, which suggests that the total number of genes whose disruption can result in the severe mental illnesses is at least several hundred. Mutations in many different genes have the potential to cause the neural circuit malfunction of psychiatric illness. It is therefore critical that computational biologists be engaged in analyzing the results of this sequencing effort in order to ascertain the contribution of the observed variants or allelic combinations to the disease in the general population.
Circuit analysis is the study of the structure, function, and dysregulation of relevant neural circuits We are now beginning to identify the possible locations of aberrant circuitry in some diseases, including depression, which is associated with hyperactivity in the subgenual cingulate region (Brodmann area 25) of the prefrontal cortex (12), anxiety states, where there is hyperactivity in the amygdala (13), and obsessive-compulsive disorder, where there is an abnormality in the striatum (14). We need biological markers for the disruptions in neural circuitry involved in mental disorders in order to fully elucidate the anatomical basis of each illness, to provide more objective diagnoses, and to follow responses to treatment.
Fortunately, there have been parallel advances in the development of a variety of powerful new methods for selectively analyzing neural circuitry, which allow the delineation of the brain-wide neuroanatomical connectivity patterns in normal experimental animals, in animal models of psychiatric illnesses, and in people. One example is the introduction of noninvasive ways to selectively activate or shut off specific neurons in a given circuit of a behaving animal using optical methods (15). Also effective for selectively turning neurons on or off are ligand-gated protein variants with customized binding sites, such as the Drosophila allostatin receptor and the G1 protein–coupled receptor (16). Neither of these techniques can be readily used in humans. However, other very recent technical advances include methods for tracing neural connections in humans using diffusion tensor imaging (17) (See Figure 1, Above); approaches to the analysis of gene expression and epigenetic modifications in animal and human brains (18, 19); and tools for studying cellular and circuit dynamics in the brain, including multiphoton imaging and calcium imaging coupled to creative electrophysiological strategies (20).
Fig. 1.
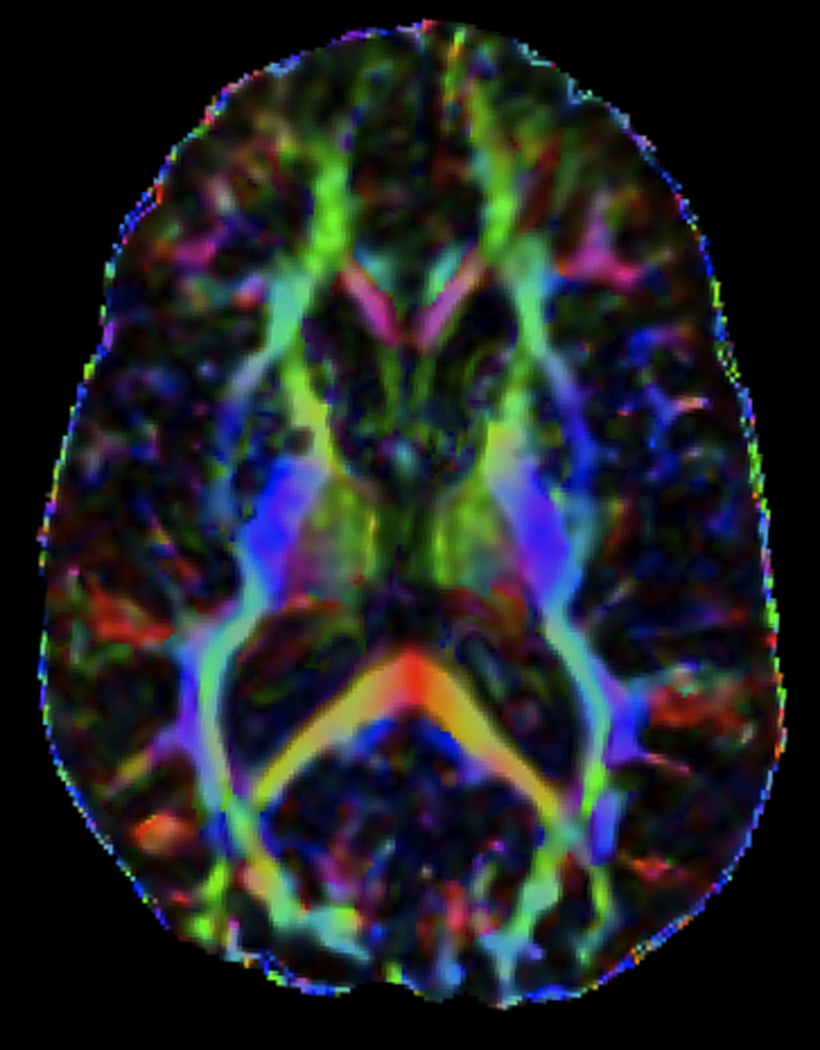
Diffusion tensor imaging (DTI) of a normal adult brain depicting white matter pathways (15 directions, b = 800 mm/s2). This tool can be used to assess changes in neural connectivity associated with brain disorders. [Courtesy of R. C. Welsh and J.-K. Zubieta, University of Michigan].
Because genes responsible for Huntington’s disease, Rett syndrome, Fragile X, and early-onset Alzheimer’s disease have been discovered, it has been possible to express these genes in mouse models and to learn a great deal about the mechanisms of pathogenesis. As new genetic variants are discovered for psychiatric disorders, it will be possible to introduce these mutations into mouse models to simulate the human disorder, providing badly needed insights into the pathogenesis of these disorders. The impact of these mutant genes on circuit development, structure, function, and pathogenesis can now be studied using the innovative approaches described above. The convergence of findings from multiple animal models with the critical mutations will help to identify the central features of circuit dysregulation that are shared regardless of the initial genetic defect. It is these shared features that are likely to underlie the human disease that is being modeled. This understanding will also allow us to devise new treatment strategies that target either specific defects or their final common path and can reset circuit function in spite of the heterogeneity of the genetic causes of its malfunction.
An International Project
Now is the time to initiate an effort that relies on the combined power of these two critical sets of tools. One component of this effort would aim to provide the world of medical neuroscience, over the next decade, with the personal genomes of many patients who have been afflicted with severe psychiatric diseases, especially those with the clearest evidence for a genetic contribution, along with appropriate controls. The effort would begin by focusing on autism, schizophrenia, and bipolar disease, but would eventually include the study of other severe psychiatric disorders, especially major depression. For schizophrenia and bipolar disorder, thousands of DNA samples from carefully evaluated patients and their families are already available, and thousands more are being collected.
A parallel component of this effort is tackling the study of neural circuitry, in animal models and in human subjects, to allow functional insights into the way that these altered genes can disrupt circuit formation, function, and dynamics. The neuroscience technologies described above tend to exist in highly specialized settings. Significant intellectual, technical, and financial investments are needed to refine them, to establish them broadly, and to integrate them with each other and with genetic analysis, so as to provide the tool kits needed by the scientific community.
Soon the cost of sequencing and analyzing single personal genomes will be in the $5000 to $10,000 range. Assuming that the inherent complexity of neural circuitry disease demands that we need to consider 100,000 personal genomes, we would need only a billion dollars over the next 10 years to do so. A similar figure for tackling neural circuitry would allow functional insights into these genes and inform us about how these genes can malfunction and cause disease. Two hundred million dollars a year, the sum of monies that will be needed, is a very small price to pay to reduce or eliminate the awful misery and burden to society caused by mental illness.
References and Notes
- 1.Eaton WW, et al. Epidemiol. Rev. 2008;30:1. doi: 10.1093/epirev/mxn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lieberman JA, et al. Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. N. Engl. J. Med. 2005;353:1209. [Google Scholar]
- 3.Gartlehner G, et al. Ann. Intern. Med. 2008;149:734. doi: 10.7326/0003-4819-149-10-200811180-00008. [DOI] [PubMed] [Google Scholar]
- 4.Jaaro-Peled H, et al. Trends Neurosci. 2009;32:485. doi: 10.1016/j.tins.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bailey A, et al. Psychol. Med. 1995;25:63. doi: 10.1017/s0033291700028099. [DOI] [PubMed] [Google Scholar]
- 6.Gottesman II. Schizophrenia Genesis: The Origins of Madness. New York: W. H. Freeman; 1991. [Google Scholar]
- 7.Sullivan PF, Kendler KS, Neale MC. Arch. Gen. Psychiatry. 2003;60:1187. doi: 10.1001/archpsyc.60.12.1187. [DOI] [PubMed] [Google Scholar]
- 8.Messias EL, Chen CY, Eaton WW. Psychiatr. Clin. North Am. 2007;30:323. doi: 10.1016/j.psc.2007.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McClellan JM, Susser E, King M-C. Br. J. Psychiatry. 2007;190:194. doi: 10.1192/bjp.bp.106.025585. [DOI] [PubMed] [Google Scholar]
- 10.Tarpey PS, et al. Nat. Genet. 2009;41:535. doi: 10.1038/ng.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook EH, Jr, Scherer SW. Nature. 2008;455:919. doi: 10.1038/nature07458. [DOI] [PubMed] [Google Scholar]
- 12.Mayberg HS, et al. Neuron. 2005;45:651. doi: 10.1016/j.neuron.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Shah SG, Klumpp H, Angstadt M, Nathan PJ, Phan KL. J. Psychiatry Neurosci. 2009;34:296. [PMC free article] [PubMed] [Google Scholar]
- 14.Baxter LR, Jr, et al. Arch. Gen. Psychiatry. 1992;49:681. doi: 10.1001/archpsyc.1992.01820090009002. [DOI] [PubMed] [Google Scholar]
- 15.Berndt A, Yizhar O, Gunaydin LA, Hegemann P, Deisseroth K. Nat. Neurosci. 2009;12:229. doi: 10.1038/nn.2247. [DOI] [PubMed] [Google Scholar]
- 16.Tan EM, et al. Neuron. 2006;51:157. doi: 10.1016/j.neuron.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Le Bihan D, et al. J. Magn. Reson. Imaging. 2001;13:534. doi: 10.1002/jmri.1076. [DOI] [PubMed] [Google Scholar]
- 18.Bernard R, et al. J. Neurosci. Methods. 2009;178:46. doi: 10.1016/j.jneumeth.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fagiolini M, Jensen CL, Champagne FA. Curr. Opin. Neurobiol. 2009;19:207. doi: 10.1016/j.conb.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacLean JN, Watson BO, Aaron GB, Yuste R. Neuron. 2005;48:811. doi: 10.1016/j.neuron.2005.09.035. [DOI] [PubMed] [Google Scholar]


