Abstract
We developed an interactive, customizable, Web-based program focused on the prevention of HIV, sexually transmitted infections, and hepatitis among youth. Results from a randomized, controlled trial with youth in treatment for substance use demonstrated that this Web-based tool, when provided as an adjunct to an educator-delivered prevention intervention, increased accurate prevention knowledge, increased intentions to carefully choose partners, and was perceived as significantly more useful relative to the educator-delivered intervention when provided alone. Results suggest this Web-based program may be effective and engaging and may increase the adoption of effective HIV and disease prevention science for youth. Limitations are discussed.
Keywords: HIV prevention, adolescent, Web-based, Internet, substance abuse treatment, hepatitis, sexually transmitted, infections (STIs)
INTRODUCTION
Although the current HIV epidemic differs greatly in various parts of the world, young people are frequently at the center of the epidemic, and HIV has been referred to as a “youth-driven disease” worldwide (Benton & Ifeagwu, 2008). Almost half of all new HIV infections worldwide are among youth aged 15–24 years (UNAIDS, 2008). In the United States, 40% of all HIV infections occur in persons under 25 years of age, and HIV is the sixth leading cause of death among adolescents (Benton & Ifeagwu, 2008).
The majority of HIV infections among youth are due to sexual transmission (Benton & Ifeagwu, 2008). Young people are sexually active at early ages, are not often monogamous and do not use condoms regularly. Adolescents and young adults make up only 25% of the sexually active population but represent almost 50% of all new sexually transmitted infections (STIs; Da Ros&Silva Schmitt, 2008).
Additionally, the period of adolescence and young adulthood is more often a time of experimentation with and use of alcohol and drugs, which may make youth at particularly high-risk for infection with HIV. Indeed, substance use impairs decision-making and is linked with risk for HIV infection more often for youth than for adults. Additionally, some drugs (e.g., some stimulants) may heighten perceptions of sexual arousal and promote high-risk sexual activity (e.g., Rotheram-Borus, Ingram, Swendeman, & Flannery, 1999).
Drug-using youth report having sex at an earlier age, having higher numbers of sexual partners, using condoms less frequently, and engaging in different types of risk behaviors (e.g., prostitution for drugs, money or shelter) compared with their nondrug-using peers. Additionally, youth who use drugs are shown to have less HIV-related knowledge, lower perceived susceptibility to HIV, higher levels of impulsivity, and less self-efficacy to engage in preventive behavior. They are also at a greater risk of other infectious diseases with similar transmission dynamics, including hepatitis and STIs (e.g., D’Angelo & DiClemente, 1996).
Undoubtedly, these trends underscore the importance of providing youth, and particularly youth involved in substance use, with access to effective HIV and infectious disease prevention interventions and highlight the potential for youth to have a large impact in changing the trajectory of the HIV epidemic. Fortunately, a number of effective HIV prevention interventions for young people exist, and typically target HIV-related sexual and drug-use behaviors (Auerbach & Kandathil, 2006). Such primary prevention programs are typically designed to increase accurate knowledge about HIV and preventive actions that provide effective deterrents against infection, increase youth’s intentions to reduce risk behavior and communicate about condom use with partners, improve attitudes toward condom use and safer sex, increase youth’s self-efficacy/ability to effectively use condoms, and reduce youth’s perceived invulnerability to HIV, as these variables are strongly predictive of progression to consistent condom use and safer sex as youth get older. Additionally, these programs may impact youth’s rates of condom use and their number of sexual partners, as evidenced by studies that include longer-term follow-up (e.g., Gerressu, 2008; Grossman et al., 2008).
However, few such evidence-based interventions are actually provided to youth, even in formal systems, such as community-based adolescent treatment for substance use programs, and are thus of limited reach. A recent UNAIDS survey of youth in 64 countries indicated that only 40% of males and 38% of females aged 15–24 years had an accurate and comprehensive knowledge about HIV and effective strategies to avoid transmission (UNAIDS, 2008). Accurate HIV prevention knowledge and skills are even lower among youth who use “substances of abuse” (Kleinman, Goldsmith, Friedman, Hopkins, & Des Jarlais, 1990). Additionally, although the Centers for Disease Control and Prevention have created program materials and training to help promote greater adoption of such evidence-based prevention interventions in youth community agencies (e.g., Replicating Effective Programs and Diffusion of Effective Behavioral Interventions projects), the majority of teens in community-based treatment for substance use do not receive evidence-based HIV prevention interventions, and virtually none provide evidence-based interventions targeting STIs or hepatitis (which may have similar transmission dynamics). Among the minority of community-based adolescent treatment for substance use programs that do provide some prevention programming, the types of programs they offer are often “homegrown” (and of unknown effectiveness) rather than “interventions in a box” (Collins, Harshbarger, Sawyer, & Hamdallah, 2006).
Barriers to the Widespread Adoption of Science-Based HIV and Infectious Disease Prevention Interventions for Adolescents With Substance Use Disorders
One significant barrier to providing evidence-based HIV and infectious disease prevention interventions to youth in treatment for substance use is cost. Evidence-based prevention interventions are expensive to implement and strain available resources, given the limited staffing and high caseloads at the average treatment program. Delivering evidence-based HIV prevention interventions requires considerable staff training and ongoing supervision. Even if evidence-based HIV prevention interventions are initiated by staff in community treatment programs, it may be difficult to ensure their fidelity (Ingram, Flannery, Elkavich, & Rotheram-Borus, 2008; Rotheram-Borus, Simmons, Coelho, Sloop, & Collins, 2009). Indeed, demonstration projects have shown that even brief, single-session HIV prevention interventions are implemented in community-based treatment for substance use settings by only about 38% of staff who have been trained to deliver them (e.g., Harshbarger, Simmons, Coelho, Sloop, & Collins, 2006). Barriers include significant staff turnover at many such programs, high patient caseloads maintained by program counselors, and counselors’ limited contact time with any one patient. Additionally, many program staff may feel uncomfortable or unprepared to discuss youth’s behavior that may place them at risk for HIV and other infectious diseases (e.g., sexual behavior) and/or to customize prevention efforts based on the needs of a given adolescent (e.g., Ingram et al., 2008). Thus, the limited compatibility of research-based interventions with treatment agency realities may present numerous operational barriers to the transfer of evidence-based practice into community-based settings. Additionally, even though many youth report struggling with their lack of knowledge about sexual health (e.g., Andrew et al., 2003), they are often reluctant to discuss their health behavior with clinicians or educators.
Consequently, there is a need to employ innovative approaches to address these challenges and enable rapid and widespread diffusion of evidence-based HIV and infectious disease prevention interventions to adolescents with substance use disorders in community-based treatment settings in a manner that ensures the fidelity of the intervention and is cost-effective.
Technology-based models for delivering HIV prevention to youth may enable rapid and widespread diffusion of science-based HIV prevention interventions to this population. An interactive, customizable, Web-delivered HIV, hepatitis, and STI prevention intervention has the potential to address these challenges. It allows a complex intervention to be delivered with high fidelity and at a low cost, without increasing demands on staff time or training needs. Also, a computerized program may be less threatening to patients and may provide greater anonymity. This may be particularly relevant when sensitive issues of sexual behavior and drug taking are addressed. Use of this technology with computer-generated speech can also accommodate individuals who have difficulty reading. It may also appeal to individuals who normally resist other forms of learning. Computer-based interventions, when delivered via the Web, can also be quickly and centrally updated to accommodate new information as it becomes available. They may also enable the provision of tailored interventions based on the risk factors and knowledge and skills deficits of a given individual. These technologies also permit temporal flexibility, allowing a user to choose to access the intervention at a convenient time. Finally, computerized interventions may allow individuals to engage in therapeutic activities for a greater period of time than would be possible with a therapist alone, review repetitive but necessary skills training, and complete educational tasks that a therapist may find uninteresting or repetitive (e.g., Bickel & Marsch, 2007). Thus, a Web-based tool offers strong potential for widespread dissemination of evidence-based HIV and infectious disease prevention.
A Web-delivered HIV and infectious disease prevention intervention offered as part of treatment for substance use may be particularly attractive to adolescents. Prior work has shown that existing models of care offered to youth in treatment for substance use may have limited acceptability for youth. For example, among the most significant barriers to participation in treatment for substance use by adolescents are reports of dislike for their therapist, feeling uncomfortable talking about personal problems with another person, and feeling like counselor-provided interventions were not helpful (Mensinger, Diamond, Kaminer, & Wintersteen, 2006). Computer-based interventions may thus be appealing to youth because of the anonymous and non-judgmental environment they afford. Indeed, one study found that youth indicated that they would prefer Internet-delivered interventions as part of treatment for substance use instead of more traditional interventions (Chambers, Connor, & McElhinney, 2005). Additionally, many youth report that they find interactive computer learning environments to be preferable to traditional learning environments in that computer-based learning provides the opportunity for active and independent problem solving and individualized feedback (e.g., Roker & Coleman, 1997).
This article reports on a randomized, controlled trial to evaluate an interactive, customizable, Web-based program focused on the prevention of HIV and other infectious diseases with similar transmission dynamics, including STIs and hepatitis, for adolescents in treatment for substance use. This program was designed to incorporate effective components of both prevention science and educational technologies that promote mastery and long-term retention of key information and skills. We conducted a randomized, controlled trial to evaluate the efficacy of this program in increasing a wide array of variables that have been shown to be strongly predictive of a reduced HIV risk, including accurate HIV/disease prevention knowledge, intentions to engage in safer behavior, positive attitudes toward safer behavior, confidence to adopt and maintain safe practices, and ability to properly use condoms. This program extended the line of research our group has been conducting focused on the development and evaluation of technology-delivered interventions (e.g., Bickel, Marsch, Buchhalter, & Badger, 2008; Marsch, Bickel, & Grabinski, 2007; Marsch, Bickel, Grabinski, & Badger, 2007). To our knowledge, the program described in this article was the first, interactive, Web-based HIV and infectious disease prevention intervention specifically designed for, and evaluated in a controlled study with, adolescents in treatment for substance use.
METHODS
Participants and Project Setting
New patients (n = 56) entering outpatient adolescent treatment for substance use disorders participated in this randomized, controlled trial. As approximately two-thirds of youth in treatment for substance use receive treatment on an outpatient basis (Dennis et al., 2003), this study was conducted in an outpatient setting. In order to be eligible for participation, youth could not have yet been offered any formal HIV prevention intervention as part of their current substance use treatment episode. Participants aged 12–18 years of age were eligible. A wide range of contact information was obtained at baseline in order to locate subjects and achieve maximum adherence and follow-up rates.
The study was conducted at two community-based adolescent treatment for substance use programs in New York City. The characteristics of patients at these sites and their program policies were consistent with patient characteristics and program policies typically observed in outpatient treatment settings for adolescent substance use disorders (e.g., Muck et al., 2001), thereby enhancing the generalizability of study results. Both programs offered outpatient substance user counseling to adolescent patients 3–5 days per week. These sessions typically included youth participation in on-site, psycho-educational, and cognitive-behaviorally oriented groups facilitated by a counselor and included some individual sessions with the counselor. The goal of both the groups and individual sessions was drug abstinence. Youth were encouraged to focus on a series of treatment and lifestyle goals to stop using substances and develop a plan for a new lifestyle. Counselors also offered limited case management to patients, including recommending social service liaisons and referrals for patients as needed.
Adolescents’ parent/legal guardian provided informed consent for their child if under 18 years of age, and adolescents provided assent (if under 18 years of age) or consent (if 18 years) to participate. The planned randomized, controlled trial was approved by all relevant institutional review boards (IRBs).
Intervention Conditions
Participants were randomly assigned to one of the two study conditions using a computer-generated randomization procedure in SAS. Randomization occurred immediately after an individual had been determined to be eligible for the trial and appropriate informed consent procedures and intake assessments had been completed.
Condition A: Traditional Prevention Intervention (n = 28)
Participants in this condition completed one session (of approximately 1 hour in duration) conducted by a trained HIV and infectious disease prevention educator. To best reflect traditional approaches to delivering HIV prevention to adolescents in treatment for substance use, these sessions were typically conducted in small groups of 2–4 participants. In these sessions, the educator provided (using bullet-pointed visual aids) descriptions of HIV/AIDS, hepatitis and STIs, basic transmission dynamics for each, and strategies to reduce risk of becoming infected with these diseases from sexual activity (including a demonstration on how to correctly use a condom using a wooden penis model), strategies to reduce drug-related risk, and information on getting tested for HIV, hepatitis, and STIs. The content of these sessions was based on the Principles of HIV Prevention in Drug Using Populations published by National Institute on Drug Abuse (NIDA) and the NIDA HIV Counseling and Education Manual. Additionally, as part of these sessions, participants viewed a 15-minute video on HIV prevention, largely geared toward youth (“Stopping the spread of HIV and AIDS,” Milner-Fenwick, 1996).
Condition B: Enhanced Prevention Intervention (n = 28)
Participants in this study condition were offered the same educator-delivered prevention intervention as provided to participants in condition A (described above) as well as access to the Web-based HIV, hepatitis, and STI prevention program. This self-directed, interactive, Web-based program was composed of age-appropriate content delivered across 25 program modules that address important drug- and sex-related factors that may place youth involved in substance use at risk for HIV, STIs, or other serious diseases (see Table 1 for a detailed list of module topics). Modules provided information about HIV, hepatitis, and STIs, taught how alcohol and other substance use may increase one’s risk for contracting various infections/diseases, provided information on risk reduction (e.g., selecting and correcting using condoms, identifying and managing triggers for risky sexual behavior or drug use), and taught relevant skills (e.g., decision-making and negotiation skills). Additionally, several modules were developed specifically for youth who may be infected with hepatitis or with HIV. The program also included a customization program that was used to tailor the program to meet the individual prevention needs of a given adolescent. In this process, program users completed a computerized assessment, and the program then suggested which modules may be relevant to a given adolescent and the order in which they may access the modules, on the basis of their risk profile of responses on the assessment. This customization feature considered alcohol and other substance use, intentions to use alcohol and other substances, injection drug use as well as whether a youth may be infected with HIV and/or hepatitis. The evidence-based content in this program was provided using evidence-based informational technologies. Specifically, this program uses “fluency-based” computer-assisted instruction (CAI), grounded in the “precision teaching” approach (Binder, 1993), to continually assess (via interactive quizzes) a user’s grasp of the material and adjust the pace and level of repetition of material in order to promote mastery and long-term retention of the skills and information being taught (HealthSim, LLC, ©1997). It also creates experiential learning environments via the use of interactive videos of actors modeling various behaviors in order for the program user to better learn the modeled behavior (e.g., how to effectively negotiate safer sex). Additionally, it employs a variety of interactive exercises (e.g., graphics and animation) to better enhance learning (e.g., how to use a female condom).
TABLE 1.
Module topics in the Web-based prevention program
| Topics |
|---|
| Training module |
| HIV and AIDS |
| STIs |
| Hepatitis |
| Sexual transmission of HIV and STIs |
| Selecting and correctly using condoms |
| The female condom |
| Negotiating safer sex |
| Decision-making skills |
| Birth control use and HIV and STIs |
| Drug use, HIV, and hepatitis |
| Alcohol use and risk for HIV, STIs, and hepatitis |
| Increasing self-confidence in decision-making |
| Identifying and managing triggers for risky sex |
| Identifying and managing triggers for risky drug use |
| Getting tested for HIV, STIs, and hepatitis |
| Finding more HIV, STI, and hepatitis information |
| Media influences on drug use and sex |
| Taking responsibility for choices |
| Living with HIV: Coping skills and managing stigma |
| Living with HIV: Communication skills for disclosing HIV status |
| Living with HIV: Managing treatment and medications |
| Living with HIV: Drug use and the immune system |
| Living with HIV: Daily routines to promote healthy behavior |
| Living with hepatitis C: Coping skills |
| Living with hepatitis C: Promoting healthy behavior |
Outcome Measures
Youth in both study conditions completed the following measures assessing HIV/disease prevention knowledge, intentions to engage in safer sex, and attitudes about safer sex before completing their respective prevention intervention as well as post-intervention (approximately 1-month post-baseline) and 1 and 3 months after completing the intervention.
HIV/Disease Prevention Knowledge
(Kelly, St. Lawrence, Hood, & Brasfield, 1988): This objective, true–false questionnaire assesses participants’ knowledge of high-risk sexual behaviors and drug practices, risk-reduction steps, and misconceptions regarding HIV/AIDS. This questionnaire was expanded to cover updated information on HIV as well as non-HIV related topics, including questions on STIs and hepatitis.
Behavioral Intentions Scale
(Malow, Dévieux, Jennings, Lucenko, & Kalichman, 2001; Otto-Salaj, Heckman, Stevenson, & Kelley, 1998): This measure assesses participants’ intention to use condoms in the future to reduce their HIV risk behavior. Participants respond using a four-point Likert scale ranging from “strongly disagree” to “strongly agree.”
AIDS Risk Reduction Model Questionnaire-Revised
(Gibson, Lovelle-Drache, Young, & Chesney, 1992): This assessment has been shown to be a valid and reliable measure of HIV-specific constructs hypothesized to be predictive of HIV risk behavior, including sexual self-efficacy (confidence to adopt and maintain HIV preventive behavior) and personal attitudes toward condoms. Participants answer four-point questions ranging from “strongly disagree” to “strongly agree.”
Condom Use Skills
(Malow et al., 2001; Sorenson, London, & Morales, 1991): Participants were asked to properly enact nine steps involved in correctly placing a condom on a penis model and the total number of correct steps was documented.
Feedback on Usefulness of Intervention
Participants were asked to complete a visual analog scale (ranging from 0–100 mm) to indicate the extent to which they found their prevention intervention to be useful (where 0 was “not at all useful” and 100 was “very useful”).
Statistical Analyses
Comparisons between study conditions on baseline characteristics were performed using ANOVA for continuous measures and chi-square tests for categorical variables. Analyses were based on all participants randomized to a study condition. Pairwise comparisons among treatment groups were performed using Fisher’s least significant difference (LSD) procedure.
RESULTS
Participant Characteristics
As shown in Table 2, characteristics of participants across the two study conditions did not differ.
TABLE 2.
Participant characteristics by study condition
| Characteristic | Standard condition (n = 28) |
Enhanced condition (n = 28) |
|---|---|---|
| Agea | 16.1 (1.0) | 16 (1.2) |
| Years educationa | 9.1 (0.8) | 8.7 (1.1) |
| Male | 71% | 68% |
| Race | ||
| African American | 68% | 50% |
| White | 7% | 14% |
| Other | 25% | 36% |
| Hispanic | 29% | 39% |
| Prior substance abuse treatment | 25% | 32% |
| HIV+ status | 3.6% | 0% |
| Hepatitis C status | 3.6% | 0% |
| Primary substance of abuse | ||
| Alcohol | 4% | 0% |
| Cocaine | 0% | 4% |
| Heroin | 0% | 4% |
| Marijuana | 96% | 89% |
| Other | 0% | 3% |
Note: All p-values > .05 for cross-condition comparisons. Values in the table are percents unless otherwise indicated; statistical significance based on chi-squared test.
Mean + SD based on the F-test.
Participation Rates
One participant in the enhanced condition discontinued study participation after completing the entire intervention but before completing the post-intervention assessments, and another participant in this condition discontinued participation after the baseline assessment (and before the intervention) due to a hospitalization. Youth in the enhanced condition completed their computerized intervention in an average of 3.25 sessions (range of 2–5 sessions). Of all scheduled follow-up assessments, 93% were completed at the 1-month post-intervention follow-up time point, and 57% were completed at the 3-month post-intervention time point. Follow-up completion rates did not differ by study condition.
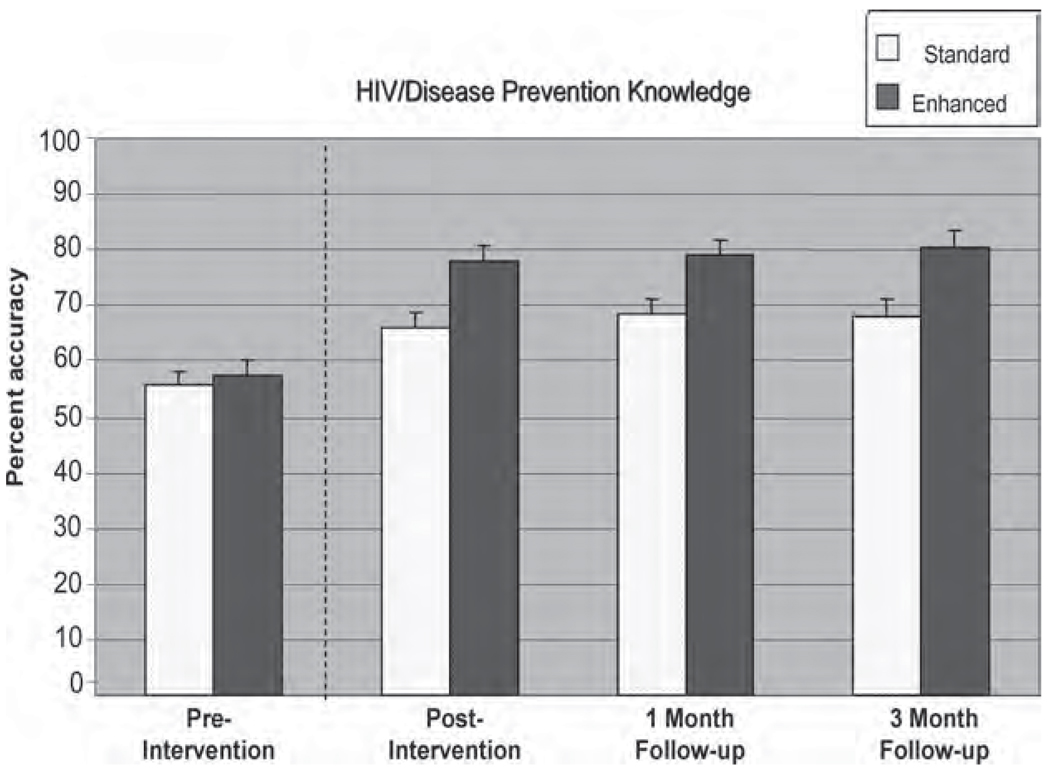
HIV/Disease Prevention Knowledge
Individuals who received both the educator-delivered intervention and the Web-based intervention (the enhanced intervention) experienced significant increases in HIV/disease prevention knowledge at the initial post-intervention time point relative to baseline knowledge levels, with such gains being maintained at all post-intervention assessment time points (time effect: F(3,102) = 65.06; p < .0001; group by time: F(3,102) = 5.46; p = .001). It is clear from Figure 1 that participants in both conditions had baseline levels of accuracy on this measure of approximately 55%–57%. Those in the standard condition demonstrated increases in accuracy to approximately 66%–68% at the post-intervention assessment time points, while those in the enhanced condition showed much larger increases, i.e., 78%–80% accuracy post-intervention.
FIGURE 1.
Changes in HIV/disease prevention knowledge over time by intervention condition.
Behavioral Intentions
Both groups reported significant increases in their intentions to use condoms during sex (time effect: F(3,104) = 4.93; p = .003). This effect did not differ across study conditions (group × time effect: F(3,104) = 0.87; p = .46). No changes were observed in either group on participants’ willingness to talk with a sexual partner about HIV/AIDS, intent to refuse sex if a condom is not available, and intent to consistently insist on condom use (all p-values > .05).
AIDS Risk Reduction
Both groups reported significant increases in their intentions to limit their number of sex partners (time effect: F(3,103) = 5.17; p = .002), and no differential effect was observed across study conditions (group × time effect: F(3,103) = 0.85; p = .47). Additionally, both groups reported an increased understanding of the extent to which condoms can help protect one against HIV infection (time effect: F(3,103) = 2.76; p = .05). This finding did not differ across study conditions (group × time: F(3,103) = 0.30; p = .82). Both groups also reported significantly more positive attitudes about engaging in safer sex (time effect: F(3,94) = 6.35; p < .001) relative to baseline levels, with no differences observed across study conditions (group × time: F(3,94) = 0.64; p = .59). Participants in the enhanced condition, but not the standard condition, experienced significantly greater increases in their perception of the importance of carefully choosing sex partners (time effect: group × time effect: F(3,103) = 2.99; p = .03). No effects were observed on measures assessing participants’ perceived likelihood of having or becoming infected with HIV, the extent to which participants were troubled with thoughts of HIV infection, the extent to which condoms were perceived as exciting, or the extent to which condoms were perceived to be awkward, to be a hassle or to reduce pleasure from sexual activity (all p-values > .05).
Condom Use Skills
Both groups showed significant increases in their ability to correctly use condoms on the condom-use skills demonstration test (time effect: F(3,103) = 4.12; p = .008), and no differential effect was observed across conditions (group × time effect: F(3,103) = 2.26; p = .08).
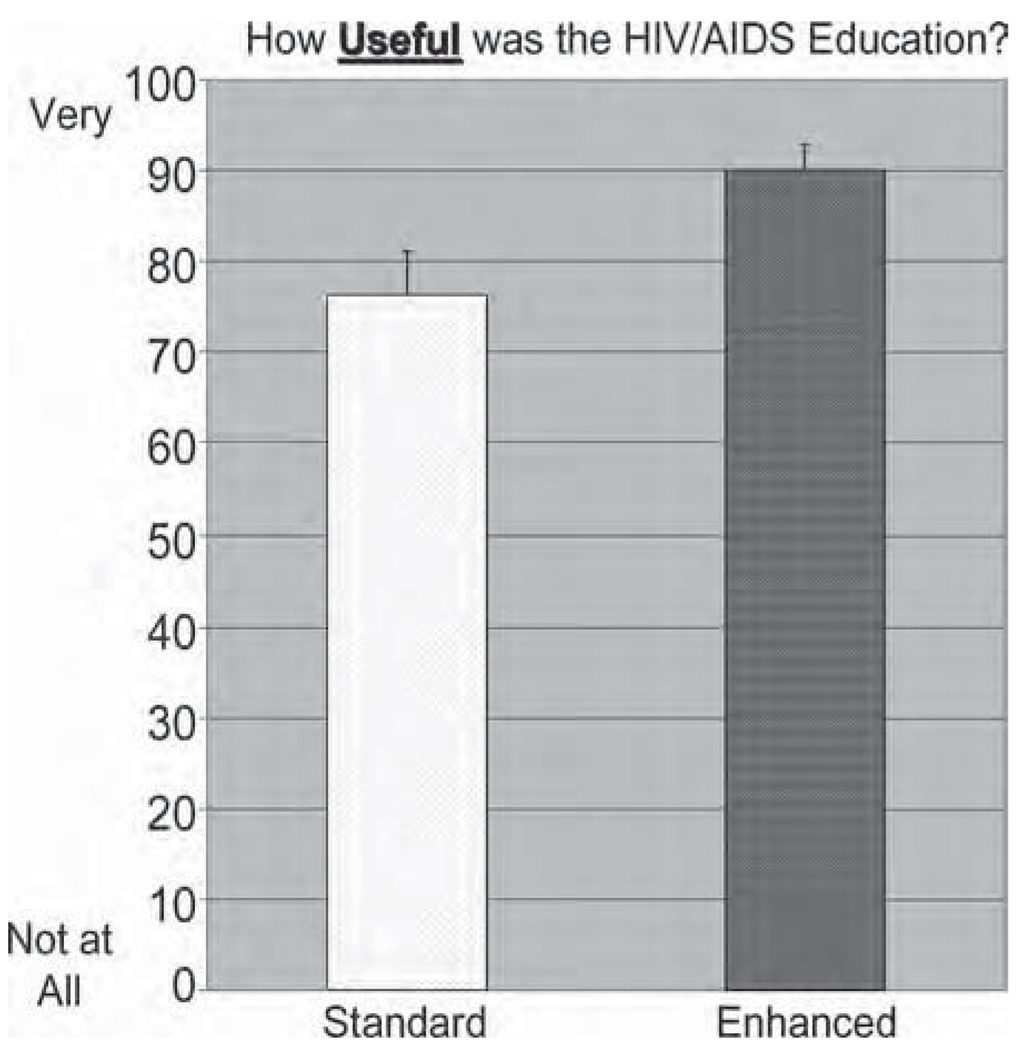
Feedback on Usefulness of Intervention
The enhanced condition was perceived by participants as significantly more useful (t(33) = −2.47; p = 0.02) relative to the standard condition (see Figure 2).
FIGURE 2.
Feedback on intervention usefulness by intervention condition.
DISCUSSION
This article reports on a randomized, controlled trial evaluating a novel, Web-based program focused on teaching knowledge and skills that have been shown to be important in the prevention of HIV and other infectious diseases among youth in treatment for substance use. Results indicated that an HIV prevention intervention delivered by a skilled educator can effectively promote knowledge and skills predictive of reduced HIV risk, including youth’s accurate prevention-related knowledge, intentions to reduce risk behavior, positive attitudes toward safer sex, and ability to effectively use condoms. Results further indicated that the addition of the Web-based intervention enhanced outcomes beyond those produced by the educator-delivered intervention alone. Specifically, participants who received the Web-based intervention had significantly greater prevention-related knowledge and intentions to carefully choose partners and perceived the intervention to be significantly more useful compared with those who received the educator-delivered intervention alone.
These findings, which underscore the potential utility of a Web-based HIV/infectious disease prevention intervention for youth in treatment for substance use, are particularly important, as the majority of adolescent treatment for substance use programs in the United States do not have the resources to provide traditionally delivered HIV prevention interventions (Collins et al., 2006). Thus, a Web-based intervention may allow for the delivery of evidence-based HIV prevention in a manner that is less complex, less costly, and able to be implemented with fidelity, while retaining or improving the effectiveness of the prevention intervention. Furthermore, the finding that youth who received the Web-based intervention perceived it to be more useful than those in the comparison condition is another important outcome. Indeed, although intervention effectiveness is critical, the acceptability of an intervention is important for it to reach and engage intended audiences and have the desired public health impact. A Web-based prevention tool thus offers the potential to substantially advance the adolescent treatment for substance use system by improving the availability and quality of HIV prevention interventions delivered to youth in such treatment settings. These findings are consistent with evaluations of Web-based, HIV prevention programs that have been evaluated with other populations of youth, including programs for non-clinical samples of adolescent males and females (Lightfoot, Comulada, & Stover, 2007), adolescent girls (DiNoia, Schinke, Pena, & Schwinn, 2004; Morrison-Beedy, Carey, Seibold-Simpson, Xia, & Tu, 2009), and rural adolescents (Roberto, Zimmerman, Carlyle, & Abner, 2007).
This study examined the utility of the Web-based intervention when offered as an adjunct to a traditionally delivered intervention. Given that very few adolescent treatment programs in the United States offer evidence-based HIV prevention interventions delivered by expert educators, we are now investigating the comparative effectiveness and cost-effectiveness of traditionally delivered and Web-based prevention (as a direct comparison). Furthermore, although we evaluated the HIV prevention intervention with youth in treatment for substance use, many modules within the prevention program may be relevant and acceptable to a wide variety of adolescents, and future research could examine the utility of this tool with a broader population of youth.
Although results of the study are promising, the study is not without limitations. The study included a modest sample size and a brief follow-up period; thus, the impact of this intervention on future behavior could not be assessed. Furthermore, although the interventions evaluated in this study impacted a number of desired outcomes, several variables were not impacted. Specifically, no increases were observed in participants’ positive attitudes about condoms (e.g., enjoyment/awkwardness associated with their use), although this finding is not surprising given that the interventions focused more on condom use skills and less on the enjoyment associated with condoms or lack thereof. Additionally, no changes were observed in youth’s intentions to refuse sex when condoms are not available or in youth’s perceived susceptibility to HIV. Again, although this finding is not entirely surprising, given the impulsivity and perceived invulnerability common among youth, these findings suggest that future iterations of program development may consider including modular content to more directly target self-control training and myopic thinking as part of prevention efforts.
Although Web-based interventions may be appealing to a wide array of individuals (e.g., refer to other articles in this Special Issue), they may be particularly appealing to adolescents. On average, 8–18-year olds in the United States spend about 7.5 hours/day using some electronic device, and often more than one such device at a time. More than 84% of this group has Internet access at home, and over two-thirds of youth own a mobile phone and spend an average of 2.5 hours per day on mobile devices. Although the majority of youth’s recreational time using computers is spent on online social networks (such as MySpace), over half report that they have looked up health information online (Kaiser Family Foundation, 2010).
Importantly, the Web-based program we evaluated in this study is browser-based and can be delivered via Internet, intranet or CD-ROM installation. Key elements of the intervention could also be made available for use on mobile devices. This allows the program to transcend geographic boundaries and to reach broader audiences. This is particularly important, as only 1 in 10 youth needing treatment for substance use (and related HIV prevention services) receive any care (Center for Substance Abuse Treatment, 2001; NIDA, 2001), suggesting that current models of care are either inaccessible or unacceptable to most substance-abusing youth. The delivery of this intervention via a variety of electronic devices may enable its use in a wide variety of treatment as well as non-treatment settings, including home, community organizations, schools, emergency rooms, health care providers’ offices, and online social networks, which are arenas where evidence-based HIV prevention interventions for youth are also typically limited. Finally, an expansion of the content within this Web-based system may promote comprehensive evidence-based skills training for youth by addressing other youth risk behavior (e.g., substance use psychosocial treatment/relapse prevention, impulsivity), and/or target mental health issues in youth. We are currently developing a Web-based psychosocial treatment program for adolescents with substance use disorders and can integrate the HIV prevention content into this program in future research.
It is particularly noteworthy that the majority of youth in this study that demonstrated the utility of the Web-based prevention program were African American, a group that is disproportionately represented among HIV/AIDS cases and for which effective interventions are sorely needed (Centers for Disease Control and Prevention, 2009). Although White (80%) Americans are more likely to use the Internet than African (72%) or Hispanic (61%) Americans, African Americans are the most active users of the mobile Internet (accessed via mobile devices). The rate of increase in the use of mobile devices to access the Internet among minority groups is twice the national average since 2007—e.g., 141% increased use for African Americans versus the 73% average (Horrigan, 2009). By offering interventions on a wide variety of platforms to optimally capitalize on the technology most frequently used by various target populations (e.g., developing interventions for mobile devices for specific minority groups), technology-based interventions also offer great potential to eliminate the “digital divide” and address healthcare disparities that exist in many traditional models of care (Gibbons, 2007). Overall, a technology-based approach to HIV prevention creates new opportunities and outlets for intervention efforts that are not tied to traditional strategies and may enable widespread access to evidence-based prevention programming.
Acknowledgments
This study was funded by NIDA grant 1 R01 DA015964 (Principal Investigator: Lisa A. Marsch, PhD).
GLOSSARY
- Fluency-Based Computer-Assisted Instruction (CAI)
CAI refers to a computerized process of continually assessing (via interactive quizzes) a user’s grasp of material presented via an interactive computer program and adjusting the pace and level of repetition of material in order to promote mastery and long-term retention of the skills and information being taught (HealthSim, LLC, ©1997).
- Hepatitis
Inflammation of the liver, typically caused by a virus.
- HIV (Human Immunodeficiency Virus)
A virus in humans which causes acquired immunodeficiency syndrome (AIDS), in which the immune system begins to fail, leading to life-threatening opportunistic infections.
Biographies
Lisa A. Marsch, PhD, is the Director of the Center for Technology and Health at National Development and Research Institutes, Inc., New York, New York. She has conducted numerous research studies focused on examining how technology can be used to enhance the reach of science-based prevention and treatment interventions. She has directed several projects focused on developing and evaluating interactive, computer-based systems that deliver evidence-based interventions using effective learning and informational technologies, including computer-based behavioral therapy for individuals with substance use disorders, HIV prevention for injection drug users, HIV and STI prevention for young drug users, and substance abuse prevention for children and adolescents. This research has provided novel empirical information regarding the role that technology may play in improving substance abuse prevention and treatment in a manner that is cost-effective, ensures fidelity, and enables the rapid diffusion and widespread adoption of science-based interventions. Dr. Marsch serves as a scientific reviewer for the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism and the National Institute on Mental Health. Dr. Marsch is also on the editorial boards of the Journal of Child and Adolescent Substance Abuse, Substance Use and Misuse, and Experimental and Clinical Psychopharmacology.

Michael J. Grabinski, BA, is President of Red 5 Group, LLC and Chief Technology Officer of HealthSim, LLC. He has architected and supervised the development of numerous commercial Internet, intranet, and extranet applications, including dozens of novel technology-based therapeutic interventions. He also serves on the Board of Directors of the Center for Learning and Health (CLH) at Johns Hopkins University, where he advises on the use of technology in substance abuse treatment settings and has developed Web-based applications for managing CLH’s Data Services Division, a non-profit organization whose goal is to provide job skills training and lifestyle counseling to at-risk populations in a therapeutic workplace setting.

Warren K. Bickel, PhD, is Wilbur D. Mills Chair of Alcoholism and Drug Abuse Prevention, Professor of Psychiatry, and Director, Center for Addiction Research, University of Arkansas for Medical Sciences, Little Rock, Arkansas. Dr. Bickel also serves as Director of COPH’s Center for the Study of Tobacco Addiction at UAMS. He has been continuously funded as Principal Investigator with several concurrent grants since 1988. His recent research includes the application of behavioral and neuro-economics to drug dependence with an emphasis on the discounting of the future and the use of information technologies to deliver science-based prevention and treatment. Dr. Bickel is the recipient of numerous awards and honors, including the Joseph Cochin Young Investigator Award from the College on Problems of Drug Dependence (CPDD), the Young Psychopharmacologist Award from the Division of Psychopharmacology and Substance Abuse of the American Psychological Association, an NIH Merit Award from NIDA, and Researcher of the Year from the Arkansas Psychological Association (ArPA) Honors for Outstanding Contribution. He served as President of the Division of Psychopharmacology and Substance Abuse, American Psychological Association, and as President of CPDD. Dr. Bickel was the Editor of the journal Experimental and Clinical Psychopharmacology, has co-edited five books, and published over 250 papers.

Alethea Desrosiers, MPhil, is a fifth-year doctoral candidate in clinical psychology at Teachers College, Columbia University. She worked at National Development and Research Institutes as a senior research assistant overseeing several studies on computer-based prevention education in children and adolescents from 2004 to 2008. At present, she works for Brown University, Center for Alcohol and Addiction Studies, providing motivational interviewing-based interventions for substance abusing teens and their parents. Her other research interests include clinical benefits of meditation and mindfulness-based interventions in both adolescents and adults.

Honoria Guarino, PhD, is a Project Director at National Development and Research Institutes. Since 2004, she has managed several research projects evaluating computer-based behavioral health interventions, including projects evaluating substance abuse treatment interventions for adults in methadone maintenance treatment and an HIV and disease prevention intervention for adolescents in substance abuse treatment. She has also worked as an ethnographer for the Bienvenidos study which implemented and evaluated a peer-based HIV prevention intervention for Puerto Rican migrant drug users. Dr. Guarino received her PhD in Anthropology from the University of Arizona in 2003. Her current research interests include qualitative research methods, ethnography and young Russian–American opioid users in New York City.

Britta Muehlbach, MS, has been working in the substance abuse field for 18 years in diverse roles both in Europe and in the United States. Trained as a psychologist, she started out as a clinician in residential drug abuse treatment, later assumed a role of program evaluator and researcher, and currently works as Director of Program Planning and Business Development for a national provider of residential and outpatient treatment and prevention services. Britta has a particular interest in the areas of translating research into practice, and organizational functioning.

Ramon Solhkhah, MD, is the Vice Chairman for Education in the Department of Psychiatry at Maimonides Medical Center in Brooklyn, New York. Prior to this role, he was the Director of the Child and Family Institute and the Chief of the Division of Child and Adolescent Psychiatry in the Department of Psychiatry at St. Luke’s-Roosevelt Hospital Center, a University Hospital of the Columbia University College of Physicians and Surgeons. Previously, he also held the position of Coordinator of Substance Abuse Services at the Child Study Center at New York University Medical Center. Dr. Solhkhah, a member of the American Psychiatric Association, the American Society of Addiction Medicine, and the American Academy of Child and Adolescent Psychiatry, is an active clinical researcher who has taught, lectured, and written extensively in child psychiatry and in the area of adolescent substance abuse.

Shilpa R. Taufique, PhD, is a Supervising Psychologist and the Assistant Clinical Director of the Comprehensive Adolescent Rehabilitation and Education Service (CARES) in the Child and Family Institute of St. Luke’s and Roosevelt Hospitals. Dr. Taufique has over a decade of experience working directly with diverse groups of adolescents, supervising emerging professionals, and developing programs relevant for teens. Her adolescent specialities include teen pregnancy and parenting, substance abuse, gang involvement, sexual identity, racial and ethnic identity, parent–teen relationships, and academic achievement.

Michelle Acosta, PhD, is a Co-Investigator in the Center for Technology and Health at National Development and Research Institutes (NDRI) in New York, New York. Dr. Acosta received her PhD in Clinical Psychology at the University of Delaware, and completed a predoctoral internship in Pediatric Psychology at the A.I. DuPont Hospital for Children. She completed a postdoctoral fellowship in Addiction Psychology at the Medical College of Virginia, Virginia Commonwealth University. Dr. Acosta’s research activities have focused on novel adaptations of evidence-based substance abuse interventions in non-traditional settings (e.g., psychiatric, medical, remote/telephone, and computer/Web-based) that may improve the reach and acceptability of these treatments for vulnerable populations. She has served as Project Manager, Co-Investigator, and Principal Investigator on several studies funded by the U.S. National Institute on Drug Abuse. She has collaborated on research developing and evaluating substance abuse interventions for medically ill patients and has collaborated on substance use research in youth, including young adult smokers, behavioral interventions to address teen substance use, and the adaptation of a computer-delivered assessment for teen substance use.

Footnotes
Portions of this study were presented at the meeting of the International Society of Addiction Medicine (ISAM, 2005), the 67th annual scientific meeting of the College on Problems of Drug Dependence (CPDD, 2005), the American Psychological Association meeting (APA, 2006), and the 6th International Conference on Urban Health (2007).
Declaration of Interest
In addition to their affiliations listed above, the first three authors are affiliated with HealthSim, LLC, the health-promotion software development organization that developed the web-based intervention evaluated in this study. The authors have worked extensively with their institutions to manage any potential conflict of interest. Additionally, all statistical analyses were conducted by an independent statistician.
REFERENCES
- Andrew G, Patel V, Ramakrishna J. What to integrate in adolescent health services. Reproductive Health Matters. 2003;11:120–129. doi: 10.1016/s0968-8080(03)02167-0. [DOI] [PubMed] [Google Scholar]
- Auerbach JD, Kandathil SM. Overview of effective and promising interventions to prevent HIV infection. World Health Organization Technical Report Series. 2006;938:43–78. [PubMed]
- Benton T, Ifeagwu J. HIV in adolescents: What we know and need to know. Current Psychiatry Reports. 2008;10:109–115. doi: 10.1007/s11920-008-0020-7. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. A future for drug abuse prevention and treatment in the 21st century: Applications of computer-based information technologies. In: Henningfield J, Santora PB, Bickel WK, editors. Addiction treatment: Science and policy for the 21st century. Baltimore, MD: Johns Hopkins Press; 2007. pp. 35–43. [Google Scholar]
- Bickel WK, Marsch LA, Buchhalter A, Badger G. Computerized behavior therapy for opioid-dependent outpatients: A randomized, controlled trial. Experimental and Clinical Psychopharmacology. 2008;16:132–143. doi: 10.1037/1064-1297.16.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binder C. Behavioral fluency: A new paradigm. Educational Technology. 1993 October;:8–14. [Google Scholar]
- Center for Substance Abuse Treatment. Treatment episode data set. Washington, DC: Substance Abuse and Mental Health Services Administration, Department of Health and Human Services; 2001. [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2007. Vol. 19. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Retrieved March, 2009]. pp. 12–21. from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2007report/default.htm. [Google Scholar]
- Chambers M, Connor SL, McElhinney S. Substance use and young people: The potential of technology. Journal of Psychiatric and Mental Health Nursing. 2005;12:179–186. doi: 10.1111/j.1365-2850.2004.00815.x. [DOI] [PubMed] [Google Scholar]
- Collins C, Harshbarger C, Sawyer R, Hamdallah M. The diffusion of effective behavioral interventions project: Development, implementation, and lessons learned. AIDS Education and Prevention. 2006;18(4) Suppl. A:520. doi: 10.1521/aeap.2006.18.supp.5. [DOI] [PubMed] [Google Scholar]
- Da Ros CT, Silva Schmitt CD. Global epidemiology of STDs. Asian Journal of Andrology. 2008;10:110–114. doi: 10.1111/j.1745-7262.2008.00367.x. [DOI] [PubMed] [Google Scholar]
- D’Angelo L, DiClemente R. STDs including HIV infection. In: DiClemente RJ, Hansen WB, Ponton LE, editors. Handbook of adolescent health risk behavior. New York: Plenum; 1996. pp. 333–367. [Google Scholar]
- DiNoia J, Schinke SP, Pena JB, Schwinn TM. Evaluation of a brief computer-mediated intervention to reduce HIV risk among early adolescent females. Journal of Adolescent Health. 2004;35:62–64. doi: 10.1016/j.jadohealth.2003.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerressu N, Stephenson JM. Sexual behavior in young people. Current Opinion in Infectious Diseases. 2008;21:37–41. doi: 10.1097/QCO.0b013e3282f3d9bd. [DOI] [PubMed] [Google Scholar]
- Gibbons MC. eHealth solutions for healthcare disparities. New York: Springer Science + Business Media, LLC; 2007. [Google Scholar]
- Gibson DR, Lovelle-Drache J, Young MT, Chesney M. HIV risk linked to psychopathology in i.v. drug users. International Conference on AIDS; 1992. Abstract, POC, 4691. [Google Scholar]
- Grossman C, Hadley W, Brown LK, Houck CD, Peters A, Tolou-Shams M, et al. Adolescent sexual risk: Factors predicting condom use across the stages of change. AIDS and Behavior. 2008;12:913–922. doi: 10.1007/s10461-008-9396-y. [DOI] [PubMed] [Google Scholar]
- Harshbarger C, Simmons G, Coelho H, Sloop K, Collins C. An empirical assessment of implementation, adaptation, and tailoring: Evaluation of CDC’s national diffusion of VOICES. AIDS Education and Prevention. 2006;18(4) Suppl. A:184–197. doi: 10.1521/aeap.2006.18.supp.184. [DOI] [PubMed] [Google Scholar]
- Horrigan J. Pew Internet & American Life Project. [Retrieved November, 2009, Nov. 10, 2009];Wireless Internet use. 2009 July 22;2009 from http://pewinternet.org/Reports/2009/12-Wireless-Internet-Use.aspx.
- Ingram BL, Flannery D, Elkavich A, Rotheram-Borus MJ. Common processes in evidence-based adolescent HIV prevention programs. AIDS Behavior. 2008;12:374–383. doi: 10.1007/s10461-008-9369-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Generation M2: Media in the lives of 8 to 18 year olds: A Kaiser Family Foundation Study. [Retrieved November, 2009];2010 January; from http://www.kff.org/entmedia/mh012010pkg.cfm. [Google Scholar]
- Kelly JA, St. Lawrence JS, Hood HV, Brasfield TL. An objective test AIDS risk behavior knowledge: Scale development, validation, and norms. Journal of Behavior Therapy and Experimental Psychiatry. 1988;20:227–234. doi: 10.1016/0005-7916(89)90027-x. [DOI] [PubMed] [Google Scholar]
- Kleinman PH, Goldsmith DS, Friedman SR, Hopkins W, Des Jarlais DC. Knowledge about and behaviors affecting the spread of AIDS. International Journal of the Addictions. 1990;25:345–361. doi: 10.3109/10826089009053164. [DOI] [PubMed] [Google Scholar]
- Lightfoot M, Comulada WS, Stover G. Computerized HIV preventive intervention for adolescents: Indications of efficacy. American Journal of Public Health. 2007;97(6):1027–1030. doi: 10.2105/AJPH.2005.072652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malow RM, Dévieux JG, Jennings T, Lucenko BA, Kalichman SC. Substance-abusing adolescents at varying levels of HIV risk: Psychosocial characteristics, drug use, and sexual behavior. Journal of Substance Abuse. 2001;13:103–117. doi: 10.1016/s0899-3289(01)00069-4. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK, Grabinski MJ. Application of interactive, computer technology to adolescent substance abuse prevention and treatment. In: Cohall AT, Rickert V, Ryan O, editors. Harnessing technology for adolescent health promotion. Elk Grove Village, IL: American Academy of Pediatrics; 2007. pp. 342–356. [PubMed] [Google Scholar]
- Marsch LA, Bickel WK, Grabinski MJ, Badger GJ. Applying Computer technology to substance abuse prevention science: Results of a preliminary examination. Journal of Child and Adolescent Substance Abuse. 2007;16:69–94. [Google Scholar]
- Mensinger JL, Diamond GS, Kaminer Y, Wintersteen MB. Adolescent and therapist perception of barriers to outpatient substance abuse treatment. The American Journal on Addictions. 2006;15:16–25. doi: 10.1080/10550490601003631. [DOI] [PubMed] [Google Scholar]
- Milner-Fenwick Stopping the spread of HIV and AIDS. 1996 Retrieved from http://www.milner-fenwick.com. [Google Scholar]
- Morrison-Beedy D, Carey MP, Seibold-Simpson SM, Xia Y, Tu X. Preliminary efficacy of a comprehensive HIV prevention intervention for abstinent adolescent girls: Pilot study findings. Research in Nursing and Health, 2009. 2009;32:569–581. doi: 10.1002/nur.20357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muck R, Zempolich KA, Titus JC, Fishman M, Godley MD, Schwebel R. An overview of the effectiveness of adolescent substance abuse treatment models. Youth & Society. 2001;33:143–168. [Google Scholar]
- National Institute on Drug Abuse. Monitoring the future. Rockville, MD: National Institutes of Health; 2001. [Google Scholar]
- Otto-Salaj LL, Heckman TG, Stevenson LY, Kelley JA. Patterns, predictors, and gender differences in HIV/AIDS risk among severely mentally ill men and women. Community Mental Health Journal. 1998;34:175–190. doi: 10.1023/a:1018745119578. [DOI] [PubMed] [Google Scholar]
- Roberto AJ, Zimmerman RS, Carlyle KE, Abner EL. A computer-based approach to preventing pregnancy, STD, and HIV in rural adolescents. Journal of Health Communication. 2007;12:53–76. doi: 10.1080/10810730601096622. [DOI] [PubMed] [Google Scholar]
- Roker D, Coleman J. Education and advice about illegal drugs: What do young people want? Drugs: Education, Prevention, and Policy. 1997;4:53–64. [Google Scholar]
- Rotheram-Borus MJ, Ingram BK, Swendeman D, Flannery D. Common principles embedded in effective adolescent HIV prevention programs. AIDS Behavior. 2009;13(3):387–398. doi: 10.1007/s10461-009-9531-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorenson JL, London J, Morales E. Group counseling to prevent AIDS. In: Sorenson JL, Wermuth DR, Gibson KH, Choi J, Guydish S, Batki S, editors. Preventing AIDS in drug users and their sexual partners. New York: Guilford; 1991. pp. 99–115. [Google Scholar]
- UNAIDS. 2008 Report on the Global AIDS Epidemic. Geneva: UNAIDS; 2008. Status of the global HIV epidemic. [Google Scholar]