Abstract
A 7-year-old girl with progressive ataxia, spasticity, supranuclear ophthalmoplegia, and sea-blue histiocytes in her bone marrow underwent orthotopic liver transplantation for hepatocellular carcinoma. After an initial period of stabilization, she has shown progression of neurologic symptoms with recurrence of storage material in the transplanted liver.
A number of inborn errors of metabolism have now been successfully corrected by organ transplantation, offering new hope for patients suffering from these disorders.1–4 We recently had the opportunity to treat a patient with neurovisceral storage disease with supranuclear ophthalmoplegia, a presumed variant of Niemann-Pick disease with normal lysosomal enzyme activity.5–9 After initial stabilization, the patient has had progressive neurologic deterioration.
CASE REPORT
At 2 months of age the patient T.H. had hepatosplenomegaly. Liver function tests revealed mild hyperbilirubinemia with slight transaminase elevation. Hepatitis B screen, congenital infection antibody titers, α-l-antitrypsin levels, urine metabolic screen, sweat test, and bone marrow and ophthalmologic examinations were negative or normal. Liver biopsy revealed cirrhosis. A celiac angiogram demonstrated esophageal varices.
At 2 years of age a liver-spleen scan suggested either tumor or cirrhosis, but ultrasound showed a homogeneous pattern consistent with cirrhosis. Early growth and development were normal. She walked at 11 months of age, talked in phrases by 2 years of age, and was toilet trained at 2 years of age. At 3½ years of age her gait was said to be wide-based and she had peculiar posturing while running. Clumsiness and a fine tremor developed over the next 18 months. At 5 years of age neurologic examination revealed hypertonicity with ankle clonus and extensor plantar responses, dysmetria, mild ataxia, and difficulty with voluntary upgaze. Intellectual function appeared good, α-fetoprotein and ceruloplasmin values were normal. Kayser-Fleischer rings were not seen. Cranial computed tomographic scan was consistent with mild cerebral atrophy.
Spasticity and ataxia worsened and by 6½ years of age the child was unable to walk independently. At that time an open liver biopsy was performed and an incidental hepatocellular carcinoma was discovered.
Four months later the child was referred to the Children’s Hospital of Pittsburgh for consideration of liver transplantation. Examination at that time revealed a well-nourished child whose liver and spleen were both hard and palpable 5 cm below the costal margins. The child was oriented, sociable, and cooperative with mildly impaired intelligence. Formal IQ testing was not accomplished, but school reports indicated that the child appeared normally sociable, but had difficulty with abstract concepts and was just beginning to learn numbers and the alphabet. Voluntary movements were slow and dysmetric. The lower extremities demonstrated increased tone, clonus, and extensor plantar responses. The child could not walk because of severe ataxia and spasticity. Speech was slow and dysarthric, but intelligible. Sensation and cranial nerve function were intact except for absence of voluntary upgaze. Reflex upgaze was easily elicited. The retinas appeared normal. Bone marrow aspirate showed striking numbers of sea-blue histiocytes. In light of the neurologic deterioration, hepatocellular carcinoma, and the possibility of a reversible storage disorder, at 7 years of age the child underwent liver transplantation using cyclosporine and prednisone.
No changes were noted in the neurologic examination 10 months following transplantation. Verbal subtests of the Wechsler Intelligence Scale for Children-Revised revealed an IQ of 58. The liver was firm and slightly larger than immediately postoperatively, with mildly elevated transaminase values. Liver biopsy revealed storage material in Kupffer cells.
Progressive neurologic deterioration again became evident 18 to 22 months following transplantation when the child developed increasing motor disability, a more aggressive, less cooperative personality, and the onset of grand mal seizures. She was only moderately cooperative for the neurologic examination and had clearly lost many verbal abilities. Speech was exceedingly slow, dysarthric, and often unintelligible. Voluntary movements were also very slow and dysmetric and dystonic posturing of all extremities was noted. The child demonstrated severe pseudobulbar palsy with swallowing difficulty, easy choking, and paucity of facial expression. She now had restriction of voluntary gaze in all directions but reflex eye movements remained intact.
RESULTS
Lysosomal enzyme studies on the open liver biopsy specimen at 5½ years of age (performed at the Children’s Hospital of Philadelphia) were all normal, including sphingomyelinase activity (4.24 nm/h/mg protein; normal = 2.98 ± 0.25). Tissue lipid analysis was normal.
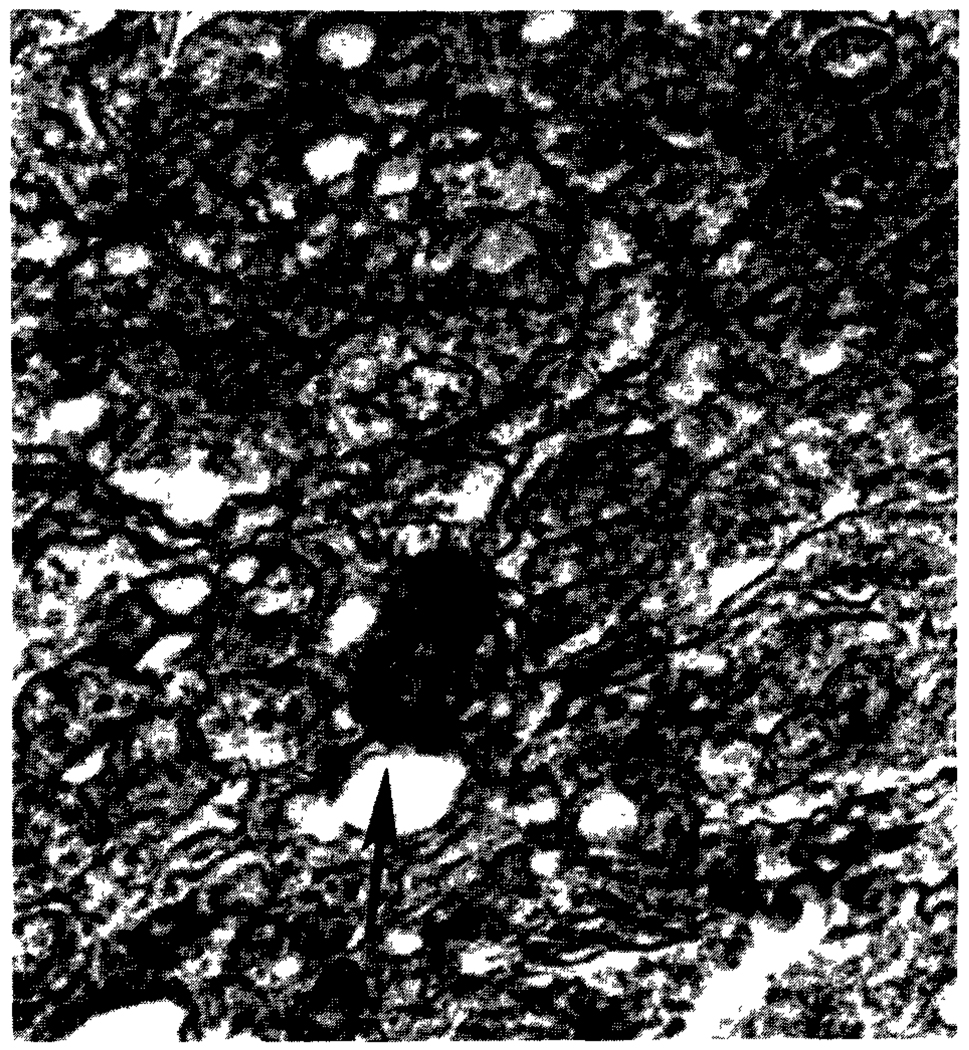
Hepatectomy specimen demonstrated cirrhosis and an incidental hepatoma. The Kupffer cells were quite prominent by virtue of having abundant cytoplasm. These cells, stained lightly with periodic acid-Schiff stain even after diastase digestion, were Sudan black positive and autofluorescent. This lipochrome material was also found in sympathetic ganglion cells of an adrenal gland removed at the time of transplantation. The Kupffer cells in the liver biopsy done 10 months after transplantation contained this same storage substance (see Figure). Although it is not unusual to find some lipochrome in Kupffer cells of transplanted livers, the fine dispersion, giving the effect of a large granular cell, is unique. Bone marrow aspirate, both before and 10 months after transplantation, demonstrated large histiocytes with peculiar “sea-blue” staining characteristics.
Figure 1.
Allograft liver biopsy 10 months after transplantation (Sudan black stain) shows presence of ceroid storage material in Kupffer cell (arrow).
DISCUSSION
Although sea-blue histiocytes have been seen in the bone marrow of patients with a variety of hematologic disorders,10 a neurovisceral storage disorder with vertical supranuclear ophthalmoplegia and similarities to Niemann-Pick disease seems to be a specific entity.5–9 In 1973 Neville et al7 described nine new patients with reference to four earlier ones.7 The clinical manifestations of our patient are similar to those previously reported. In most of the cases sphingomyelinase and other lysosomal enzyme activities were normal, though exceptions may occur as described in the report of Wenger et al.8 Onset of signs may be noted as early as 2 months of age (present case and patient 4 of Neville et al) but more frequently begin later in the first or second decade. Slow, inexorable progression of symptoms occurs over a period of many years.
Liver transplantation has offered new hope to many patients with primary hepatic-based inborn errors of metabolism such as tyrosinemia, α-l-antitrypsin deficiency, Wilson’s disease, type I glycogen storage disease, and, more recently, homozygous familial hypercholesterolemia.1–4 The results with lipidoses are far less clear, but Daloze et al11 reported near normalization of graft liver, serum, and cerebrospinal fluid sphingomyelinase activity in a patient with Niemann-Pick disease type A after liver replacement. Our goal was to cure our patient of both the hepatocellular carcinoma and the neurovisceral storage disease by using liver transplantation. Unfortunately, recurrence of storage material and clinical progression of neurologic disease indicates that the variant of Niemann-Pick disease which affected our patient is not a primary hepatic-based disorder. Bone marrow transplantation, which has recently been used to treat several lipidoses and mucopolysaccharidoses, might also be considered for patients with this disorder.12–14 Identification of a specific enzymatic deficiency in cells of bone marrow origin would provide a firm theoretical basis for this approach and make documentation of biochemical improvement possible.
ACKNOWLEDGMENT
Tissue lipid analysis was performed by Dr David Wenger, University of Colorado.
REFERENCES
- 1.Hood JM, Koep LJ, Peters RL, et al. Liver transplantation for advanced liver disease with alpha 1 antitrypsin deficiency. N Engl J Med. 1980;302:272–275. doi: 10.1056/NEJM198001313020505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malatack JJ, Finegold DN, Iwatsuki S, et al. Liver transplantation for type 1 glycogen storage disease. Lancet. 1983;1:1073–1074. doi: 10.1016/s0140-6736(83)91910-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zitelli BJ, Malatack JJ, Gartner JC, et al. Orthotopic liver transplantation in children with hepatic-based metabolic disease. Transplant Proc. 1983;15:1284–1287. [PMC free article] [PubMed] [Google Scholar]
- 4.Starzl TE, Bilheimer DW, Bahnson HT, et al. Heart-liver transplantation in a patient with familial hypercholesterolemia. Lancet. 1984;1:1382–1383. doi: 10.1016/s0140-6736(84)91876-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silverstein MN, Ellefson RD, Dhern EJ. The syndrome of the sea-blue histiocyte. N Engl J Med. 1970;282:1–4. doi: 10.1056/NEJM197001012820101. [DOI] [PubMed] [Google Scholar]
- 6.Grover WD, Naiman JC. Progressive paresis of vertical gaze-in lipid storage disease. Neurology. 1971;21:896–899. doi: 10.1212/wnl.21.9.896. [DOI] [PubMed] [Google Scholar]
- 7.Neville BGR, Lake BD, Stephen R, et al. A neurovisceral storage disease with vertical supranuclear ophthalmoplegia and its relationship to Niemann-Pick disease. Brain. 1973;96:97–120. doi: 10.1093/brain/96.1.97. [DOI] [PubMed] [Google Scholar]
- 8.Wenger DA, Barth G, Githens JH. Nine cases of sphingomyelin lipidosis: A new variant in Spanish-American children. Am J Dis Child. 1977;131:955–961. doi: 10.1001/archpedi.1977.02120220021002. [DOI] [PubMed] [Google Scholar]
- 9.Yan-go FL, Takehiko Y, Pierre RU, et al. A progressive neurologic disorder with supranuclear vertical gaze paresis and distinctive bone marrow cells. Mayo Chn Proc. 1984;59:404–410. doi: 10.1016/s0025-6196(12)61464-5. [DOI] [PubMed] [Google Scholar]
- 10.Rywlin AM, Hernandez JA, Chastain DE, et al. Ceroid histiocytosis of spleen and bone marrow in idiopathic thrombocytopenic purpura: A contribution to the understanding of the sea-blue histiocyte. Blood. 1971;37:587–593. [PubMed] [Google Scholar]
- 11.Daloze P, Delvin EE, Glorieux JH, et al. Replacement therapy for inherited enzyme deficiency: Liver replacement in Niemann-Pick Disease type A. Am J Med Genet. 1977;1:229–239. doi: 10.1002/ajmg.1320010209. [DOI] [PubMed] [Google Scholar]
- 12.Hobbs JR, Hugh-Jones K, Barrett AJ, et al. Reversal of clinical features of Hurler’s disease and biochemical improvement after treatment by bone-marrow transplantation. Lancet. 1981;2:709–712. doi: 10.1016/s0140-6736(81)91046-1. [DOI] [PubMed] [Google Scholar]
- 13.Hobbs JR. Bone marrow transplantation for inborn errors. Lancet. 1981;2:735–739. doi: 10.1016/s0140-6736(81)91059-x. [DOI] [PubMed] [Google Scholar]
- 14.Krivit W, Pierpont ME, Ayaz K, et al. Bone marrow transplantation in the Maroteaux-Lamy Syndrome (mucopolysaccharidosis type VI). Biochemical and clinical status 24 months after transplantation. N Engl J Med. 1984;311:1606–1611. doi: 10.1056/NEJM198412203112504. [DOI] [PubMed] [Google Scholar]