Abstract
Background
The primary demonstration of the principle of income-related equity in Canada is the provision of health care services based on need rather than ability to pay. Despite this principle, Canada, along with other OECD countries, exhibits income-related variations in the use of health care services. This paper extends previous analyses to include surgical day care, assesses changes in income-related equity between 1992 and 2002 in British Columbia and tests the feasibility of using administrative data for general equity analyses.
Methods
Data derive from the BC Linked Health Database and from a custom tabulation of income tax filer data provided by Statistics Canada. Cross-sectional analyses measure inequity in the probability and conditional use of services using concentration indices, which summarize health care services use for individuals ranked by income, after standardization for age, sex, region of residence and need for health care services.
Results
Small but systematic relationships were found between income and use of health care services for all types of services, with the exception of visits to general practitioners (GPs). Lower income is associated with greater conditional use of GPs and greater use of acute inpatient care. Higher income is associated with the greater use of specialist and surgical day care services; the latter inequity was found to grow substantially over time.
Conclusions
Deviations from equity deserve further investigation, especially because the use of day care surgery is continually expanding. For example, an understanding of the reasons for differential admission rates to acute and day surgery might provide insight as to whether community-based services could help shift some acute care use among lower income groups to surgical day care. It is possible to use administrative data to monitor income-related equity, and future research should take advantage of this possibility.
Introduction
The primary income-related equity principle underlying medicare in Canada is the provision of hospital and physician services on the basis of on need rather than ability to pay.1 However, van Doorslaer and colleagues2 recently showed that, after controlling for need, many OECD countries including Canada exhibit income-related variations in the use of health care services. Although there is generally little income-related inequity in the use of general practitioner (GP) services, the utilization of specialist services is consistently (and sometimes substantially) greater in higher income groups. (The category “GP” as used here includes both GPs (those with 1 year of general training) and FPs (those with a formal 2-year residency in family medicine.) The opposite is often seen for inpatient hospital services, for which utilization is higher (after needs adjustment) among lower income groups. These findings are broadly consistent with previous Canadian research in this area.3-6
Our study had three objectives. First, we examined the use by income groups of physician, inpatient hospital and surgical day care services; the last of these is an important extension of previous analyses, as surgical day care is a rapidly growing area of health care services.7 Second, we assessed changes in equity between 1992 and 2002 in British Columbia, a decade of many changes in the delivery of health care services. Third, we tested the feasibility of the use of administrative data for general equity analyses, given that previous work has been based almost exclusively on survey data, or has focused on specific diseases or interventions.8-11
Administrative data have some advantages over survey data, which are more commonly the data source for equity analyses. Population-based administrative data permit comparisons over time of publicly funded services such as physician and hospital services. In addition, administrative data pertain to the whole population rather than a sample, which circumvents the problem that surveys may have in representing the tails of the income distribution.12
Methods
Data sources and variable construction
Data were derived from the BC Linked Health Database (BCLHD), a collection of population-based, linkable data covering the use of physician and hospital services,13 and from a custom tabulation of income tax filer data provided by Statistics Canada. The study population included all residents of British Columbia in 1992 and 2002, which in 2002 numbered approximately 4 million.
Income
We used an income variable based on a custom tabulation of 1992 and 2002 tax filer data held at Statistics Canada.1 User-specified analyses conducted within Statistics Canada started with a known number or level of individuals, households and income within geographic areas defined by postal code. For each postal code, a Statistics Canada analyst calculated disposable income per “equivalized” person, ranked the postal codes by this income, and created 1000 income bands, each containing (approximately) 1400 families and 3700 individuals. Equivalization is a means of ensuring comparability14,15; a couple, for example, requires less than two times the income of a single person to achieve the same standard of living. Incomes per equivalized person were derived using the OECD modified scale, counting the first adult as “1”, each subsequent person aged 14 and over as “0.5” and each child under age 14 as “0.3”.16,17
This approach was chosen because it allowed for the creation of a large number of income bands. The resulting variable is ecological – that is, it describes areas rather than individuals – as are income quintiles and deciles commonly used for this sort of analysis.18 But the heterogeneity of income within postal codes as used here will be smaller than the heterogeneity within Statistics Canada dissemination areas, which are the units used to create income quintiles / deciles. The use of ecological measures of income is accepted as valid in health services research8,19 and is common in the analysis of administrative data.20
Health care services use
The BCLHD includes a file of all residents registered with the province of British Columbia for health care insurance. Demographic and location information are available for all individuals regardless of whether they actually use health care services. We obtained age (aggregated into 6 age groups: 0–14, 15–44, 45–64, 65–74, 75–84, and 85 and older), sex, and postal code of residence from this file. Postal codes were used both to assign individuals to 1 of the 1000 income bands described above and to create a variable indicating residence in 1 of 5 geography-based health authorities responsible for health care planning and administration. (Information about these 5 health authorities, from the 2nd edition of the BC Health Atlas, can be found at http://www.chspr.ubc.ca/Research/health-atlas.php?sect=1&sub=5.)
The health care services utilization files of the BCLHD include information on: (1) all hospital separations (discharges and deaths) in British Columbia, as well as all out-of-province (and some out-of-country) hospitalizations for residents of British Columbia; and, (2) services provided by physicians to provincial residents and reimbursed on a fee-for-service basis, as well as out-of-province services provided to residents of British Columbia. Physician expenditures were divided into specialty and general practice services based on whether the specific fee item paid is used predominantly by specialists or by general practitioners. This means that the designations of “specialist” and “general practice” refer to the type of service provided rather than to characteristics of the provider.1
The analyses required the conversion of all health care services utilization into expenditures. Fees paid were included as part of the physician file. Hospital costs were estimated using Resource Intensity Weights and Day Resource Intensity Weights applied to acute inpatient and surgical day care separations, respectively, following procedures used routinely by the BC Ministry of Health.
Need for health care services
Need for health care services was measured using the Adjusted Clinical Group (ACG) system, a validated case-mix grouper for health care services developed at Johns Hopkins University.21 As described by the developers of this system:
The Johns Hopkins ACG Case-Mix System is a statistically valid, diagnosis-based, risk adjustment methodology which allows health care providers, insurers and HMOs to describe or predict a population’s past or future health care utilization and costs. ACGs are also widely used by researchers to compare various patient populations’ prior health resource usage while taking into account the morbidity or “illness burden” of each population.22
The ACG system groups individuals on the basis of the range of diagnoses each receives from physician and hospital encounters over the course of a year. The categories, such as “acute minor” and “chronic major with psychosocial,” characterize the morbidity profile of each individual, and were designed to reflect anticipated use of health care services. Assignment to groups depends on all diagnoses accumulated during a year, and so the analyses were limited to individuals who were resident in British Columbia for a minimum of 9 months of the year. This avoids the potential for misclassification bias, for example counting someone in a lower morbidity group because they had some of their medical encounters while living somewhere else. This exclusion is consistent with other analyses using the ACG system, and previous analyses of data in British Columbia have shown that there is little impact on results.23
The advantage of this approach to measuring need for health care services for this study is that the estimate of need is explicitly based on expected use of services given an identified constellation of medical diagnoses. Two individuals with equal “need” according to this definition will be expected to use approximately the same amount of health care, measured in terms of expenditures.
Statistical analyses
The analyses employ the methods developed by the ECuity group and now widely used in health equity research (including that by van Doorslaer and colleagues2). Within this framework, inequity is measured using concentration curves and concentration indexes, which have the same properties as Lorenz curves and Gini coefficients.
A Lorenz curve is a line that represents the cumulative percentage of the population and the corresponding cumulative percentage of income (measured along the x-axis and y-axis, respectively), where the population is ranked from lowest to highest income (Figure 1). The Lorenz curve representing perfect equality — the case in which every person has the same income — is shown by the diagonal line. In this case, 10% of the population has 10% of total income, 20% of the population has 20% of total income and so on. In reality, the Lorenz curve will lie below the line of equality, since the distribution of income in any population is unequal, and people are ranked from lowest to highest income. The extent of deviation of the actual curve from the diagonal line represents the deviation of the distribution of income from that of perfect equality. A Gini coefficient quantifies this distance, and is mathematically 2 times the shaded area shown in Figure 1.
Figure 1.
Lorenz / concentration curves and Gini coefficients / concentration indexes
The term “Lorenz curve” is generally reserved for measuring inequality in income, but the same principles can be applied to measuring inequalities in other variables such as health care services use. In these cases, we use the terms concentration curves and concentration indexes.24 The measurement of inequality in health care services use is a univariate distribution. It is possible to extend these principles further to measure bivariate distributions, such as income-related inequalities in health care services use. In this case, individuals are still ranked by income along the x-axis, but it is health care services use rather than income that is accumulated on the y-axis. We concentrate on that bivariate distribution in this study because it is these inequalities that might be considered “unfair” and at least potentially amenable to policy review.
Concentration indices can range either from -1 to 0 or from 0 to 1, depending on whether the variable of interest on the y-axis tends to be more concentrated among individuals with lower income (negative concentration index values) or higher income (positive concentration index values).
It is not sufficient merely to rank the population by income and then calculate a concentration index of health care services use, because there will be systematic differences in age, sex and need for health care services by income.20 The ECuity group has shown that it is possible to use linear regression to standardize for these differences. The steps involved are: (1) regress total health care expenditures on a vector of variables that are related to health care services use; (2) use the resulting model to calculate predicted health care services use for each individual; (3) calculate a standardized y (health care services use) for each individual by subtracting predicted from actual expenditures and adding population mean expenditures; and (4) calculate a concentration index for the standardized ys. This approach tests whether differences between actual and expected use of health care services are systematically related to income.
Separate models were run for 4 types of health care services for 1992 and 2002. As is common for health care utilization studies, analyses were conducted using a 2-part estimation model in which utilization was broken into: (1) the decision whether to use any service, estimated via a linear probability model; and (2) conditional on being a user, the amount of services used, estimated by OLS (ordinary least-squares) regression.16 The linear specification is required for the computation of the concentration index. Previous work by the ECuity group has shown that the linear specification of the 2 models does not produce results that are significantly different from the more traditional (but less flexible) logit (part 1) and negative binomial (part 2) specifications.16
Approval for access to de-identified research data was provided through the BC Linked Health Database,25 and ethics approval was provided by the University of British Columbia Behavioural Research Ethics Board.
Results
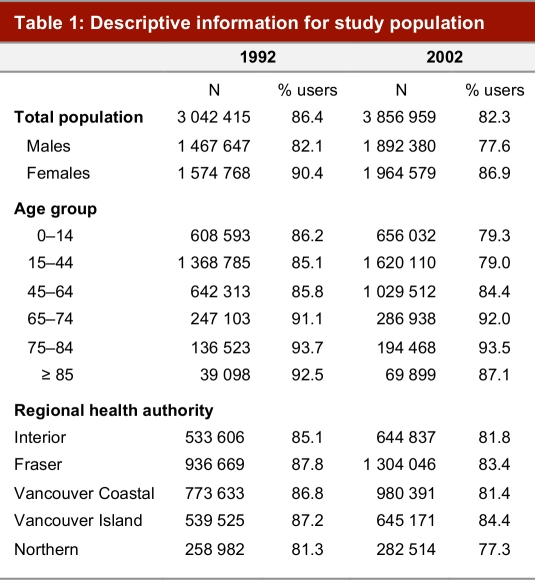
The overall study populations for 1992 and 2002 totalled just over 3 million and 3.8 million individuals, respectively (see Table 1). This is less than the population of British Columbia in these years because of the exclusion of individuals who were resident in the province for fewer than 9 months of the year. The majority of the population used at least 1 type of medicare service, and this was true of both sexes and all age groups. Nine out of 10 females had some contact with medicare services during 1992, as compared to slightly more than 8 out of 10 males. The likelihood of service use tended to rise with age, although it declined slightly in the oldest age group. The proportion of the population who used services was slightly lower in the Northern Health Authority, and proportions for all types of use declined slightly from 1992 to 2002.
Table 1.
Descriptive information for study population
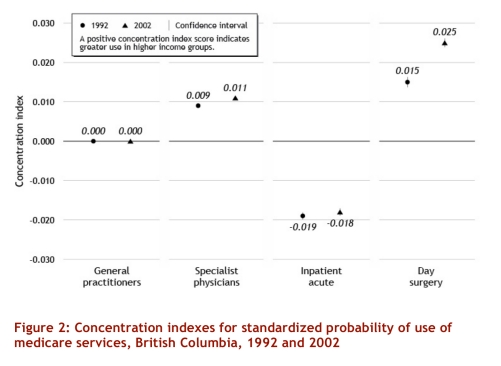
There was no income-related difference in the probability of visiting a general practitioner (GP) after adjusting for age, sex, region of residence and need for health care services (see Figure 2). The probability of specialist visits, however, was more heavily concentrated in higher income groups, and this inequity increased slightly over time (see Figure 2; error bars indicate 95% confidence intervals but tend to be narrow and so are not apparent for all outcomes). There was a greater probability of admission to acute inpatient care among lower income groups, while use of surgical day care showed the opposite – i.e., a greater likelihood with higher income. In addition, the concentration index for probability of use of surgical day care increased substantially over time.
Figure 2.
Concentration indexes for standardized probability of use of medicare services, British Columbia, 1992 and 2002
The conditional use of services, after standardization for age, sex, region of residence and need, showed slightly different patterns for GP services (Figure 3). Given some contact with GPs, there was a greater use of services among individuals in lower income groups, and this increased (meaning it became more heavily concentrated) over time. The other service types showed the same relationships as seen for the probability of use: greater conditional use of specialist services and surgical day care among higher income groups, and greater use of inpatient acute care among lower income groups. There is some suggestion that inequities may be decreasing in the conditional use of specialist services and may be increasing in acute inpatient care, but the changes are smaller in magnitude than that seen for the probability of use of surgical day care. Sensitivity analyses excluding residents of the Northern Health Authority, where there is a greater reliance on non-fee-for-service payments, and of rural areas, where it is expected that there is more heterogeneity in the ecological income measure, had marginal effects on these results, and no impact on overall trends (data not shown).
Figure 3.
Concentration indexes for standardized conditional use of medicare services, British Columbia, 1992 and 2002
Discussion
This study shows that with the development of variables for income and need, administrative data can be used to measure income-related equity in the use of health care services. The use of administrative data means it is possible to analyze equity in the use of surgical day care, a service type that is not directly queried in Canadian household surveys on health and health care use.* Our results suggest that this is an important development: higher income groups are greater users of day care surgery, and this inequity is increasing over time.
One of the research questions following from the implementation of medicare in Canada was whether removing financial barriers created socio-economic or income-based equity in the use of health care services.5,26 The general result of early studies was that inequities in access were reduced but not eliminated. More recent research is generally consistent in showing that higher income individuals are more likely to visit specialists2,4,27,28, while lower income individuals are more likely to receive more inpatient acute care.2,27 Some of these studies also show that higher income individuals are more likely to visit a GP, but this finding is not universal (e.g., Dunlop et al.4), and was not the case in the present study. One previous study3 linked survey and administrative data and found no relationship between income and total physician or specialist physician use after controlling for health status. It is not clear how generalizable those results are, however, because they were limited to a small population (n ~ 2000) in a single province (Ontario) in the mid 1990s.
A direct comparison with the study by van Doorslaer and colleagues2 is useful because the method of analysis was the same, although the sources of data were different. Compared to that earlier study, the results reported here for British Columbia with respect to the probability of seeing a GP, forexample, are lower in magnitude, but generally would lead to similar conclusions about Canada in international comparisons. Results for other comparisons between the 2 studies are similar.
It is likely that the main reason for the lower magnitude of results, and a limitation of the present study, is that the income variable used here is ecological; even at a very fine-grained level of aggregation, this still means that these analyses very likely underestimate the true relationship between income and health care services use. If anything, the present analyses are likely to present a conservative estimate of equity.
Another limitation is that the physician data do not include any detailed information for services provided by physicians paid by non-fee-for-service methods (e.g., contracts, salary, sessional payments). These alternative payment arrangements have traditionally represented less than 10% of total payments to physicians, but the proportion has been rising in recent years.29 Sensitivity analyses, however, suggest that these missing data do not have a large impact on results.
The measure of need for health care services, the ACG system, also has some limitations, the most important of which is that it cannot assess the health care needs of people who do not access the health care system. This issue, and the relationship between self-reported health status and “need” as measured by systems such as the ACG case-mix grouper, are important areas for future research.
Finally, our analyses were limited to sectors of the health care system that are part of medicare and thus covered by (essentially) full public payment. Analyses of other health care sectors in which users make out-of-pocket payments would surely indicate higher inequities in use.
The concentration indexes reported in Figure 2 and Figure 3 are all close to zero, indicating small but systematic relationships between income and use after adjusting for need. Lower income individuals have a higher conditional use of GP services, and both a greater probability and a higher conditional use of acute inpatient services, whereas higher income individuals tend to receive more specialist and surgical day care services.
In fact, it is only with respect to the likelihood of visits with GPs that no income-based inequity was found in the use of services. In other words, inequities in use are found for physician-referred rather than patient-initiated services, suggesting that income-based inequities in the system are more likely the result of the way patients are cared for rather than the result of patient behaviours and decisions about presenting for care. Ultimately, however, it is difficult to disentangle patient effects from physician effects, since higher income patients might be more likely to request specific services or referrals4 and physicians often find it difficult to “say no” once patients make direct requests.30
The results suggest that there may be a trade-off between GP and specialist services and between acute and surgical day care services. For example, because of geography and the uneven distribution of specialty services, individuals in areas that are under-served by specialists (who also tend to have lower average income) might make more use of GP services. However, we did adjust for region of residence in the analyses. A trade-off might also occur if there is an imperfect adjustment for health status, leaving a remaining relationship between income and severity of disease unaccounted for in the analyses. However, this also does not seem plausible, because the results for hospital services would suggest that the (unmeasured) severity of illness is greater for lower income groups (which receive more acute care services), while physician services suggest the opposite (lower income groups receive fewer specialist services).
Some inequities became more pronounced between 1992 and 2002, in particular the likelihood of referral for surgical day care services (which was greater for higher income groups) and expenditures on total hospital care, including both acute inpatient and surgical day care (which were greater for lower income groups). These differences deserve further study, especially as the use of day care surgery continues to expand. A better understanding of the reasons for differential admission rates to acute care and day surgery might offer some guidance as to whether relatively inexpensive community-based services could help shift some acute care use among lower income groups to surgical day care.
The general picture of equity in physician and hospital services use in British Columbia is that the system is delivering services largely according to need. The differences by income group in the use of physician and hospital services are relatively small, but there is always room for improvement. Future research should take advantage of the breadth of coverage of administrative data to analyze trends at provincial and sub-provincial levels, and in more precise categories such as medical versus surgical care within acute care hospitals. Certainly, there is a need to monitor equity as health care reforms continue.
Acknowledgments
This work was completed in partial fulfillment of the requirements for a PhD in the Department of Health Care and Epidemiology at the University of British Columbia. Comments on earlier versions of these analyses were provided by my thesis committee members, Morris Barer, Robert Evans and Clyde Hertzman. I am also grateful to Jerry Hurley for comments on an earlier draft of this paper, and to Dawn Mooney for creating the figures used here.
Biography
Kimberlyn M. McGrail is an Assistant Professor in the School of Population and Public Health at UBC and Faculty of the Centre for Health Services and Policy Research at the University of British Columbia, Vancouver, B.C.
Footnotes
Competing interests: None declared.
Funding source: Financial support for this work was provided by a Canadian Institutes of Health Research doctoral research award and by the Centre for Health Services and Policy Research at the University of British Columbia.
The Canadian Community Health Survey (CCHS) asks about contacts with specialist physicians other than while patients are in hospital overnight, and so it is possible that some day surgery contacts are embedded in this response. The only direct question about day surgery is with reference to the most recent contact with a physician, and so there is no possibility of teasing apart these different types of use. See, for example, the questionnaire from CCHS Cycle 1.1.
References
- 1.McGrail KM. Equity in health, health care services use and health care financing in British Columbia, 1992 and 2002 [dissertation] 2006.
- 2.van Doorslaer Eddy, Masseria Cristina, Koolman Xander OECD Health Equity Research Group. Inequalities in access to medical care by income in developed countries. CMAJ. 2006;174(2):177–83. doi: 10.1503/cmaj.050584. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=16415462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkelstein M M. Do factors other than need determine utilization of physicians' services in Ontario? CMAJ. 2001;165(5):565–70. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=11563208. [PMC free article] [PubMed] [Google Scholar]
- 4.Dunlop S, Coyte PC, McIsaac W. Socio-economic status and the utilisation of physicians' services: results from the Canadian National Population Health Survey. Soc Sci Med. 2000;51(1):123–33. doi: 10.1016/s0277-9536(99)00424-4. [DOI] [PubMed] [Google Scholar]
- 5.Birch S, Abelson J. Is reasonable access what we want — implications of, and challenges to, current Canadian policy on equity in health-care. Int J Health Serv. 1993;23(4):629–53. doi: 10.2190/K18V-T33F-1VC4-14RM. [DOI] [PubMed] [Google Scholar]
- 6.Newbold KB, Eyles J, Birch S. Equity in health care: methodological contributions to the analysis of hospital utilization within Canada. Soc Sci Med. 1995;40(9):1181–92. doi: 10.1016/0277-9536(94)00229-m. [DOI] [PubMed] [Google Scholar]
- 7.Canadian Institute for Health Information. Trends in acute inpatient hospitalizations and day surgery visits in Canada, 1995–1996 to 2005–2006. Ottawa: 2007. http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=bl_hmdb_3jan2007_e. [Google Scholar]
- 8.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999;341(18):1359–67. doi: 10.1056/NEJM199910283411806. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=10536129&promo=ONFLNS19. [DOI] [PubMed] [Google Scholar]
- 9.Pilote L, Joseph L, Belisle P, Penrod J. Universal health insurance coverage does not eliminate inequities in access to cardiac procedures after acute myocardial infarction. Am Heart J. 2003;146(6):1030–7. doi: 10.1016/S0002-8703(03)00448-4. [DOI] [PubMed] [Google Scholar]
- 10.Rabi D, Edwards AL, Southern DA, Svenson LW, Sargious PM, Norton P. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health Serv Res. 2006;6:124. doi: 10.1186/1472-6963-6-124. http://www.biomedcentral.com/1472-6963/6/124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Booth GL, Hux JE. Relationship between avoidable hospitalizations for diabetes mellitus and income level. Arch Intern Med. 2003;163(1):101–6. doi: 10.1001/archinte.163.1.101. http://archinte.ama-assn.org/cgi/pmidlookup?view=long&pmid=12523923. [DOI] [PubMed] [Google Scholar]
- 12.Frenette M, Green DA, Picot G. Rising income inequality in the 1990s: an exploration of three data sources. Ottawa: Statistics Canada; Cat. no 11F0019MIE2004219 http://www.statcan.ca/bsolc/english/bsolc?catno=11F0019MIE2004219. [Google Scholar]
- 13.Chamberlayne R, Green B, Barer ML, Hertzman C, Lawrence WJ, Sheps SB. Creating a population-based linked health database: a new resource for health services research. Can J Public Health. 1998;89(4):270–3. doi: 10.1007/BF03403934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ebert U. Using equivalent income of equivalent adults to rank income distributions. Soc Choice Welfare. 1999:233–58. doi: 10.1007/s003550050142. [DOI] [Google Scholar]
- 15.Ebert U. Social welfare when needs differ: An axiomatic approach. Economica. 1997;64(254):233–44. [Google Scholar]
- 16.van Doorslaer E, Masseria C OECD Health Equity Research Group Members. Income-related inequality in the use of medical care in 21 OECD countries. OECD Health Working Paper No. 14. Paris: OECD; 2004. pp. 1–44. [Google Scholar]
- 17.van Doorslaer Eddy, Koolman Xander, Jones Andrew M. Explaining income-related inequalities in doctor utilisation in Europe. Health Econ. 2004;13(7):629–47. doi: 10.1002/hec.919. [DOI] [PubMed] [Google Scholar]
- 18.Wilkins R. PCCF+ Version 3G User’s Guide [Geocodes/PCCF): Automated geographic coding based on the Statistics Canada Postal Code Conversion Files including postal codes to June 2001. Ottawa: Statistics Canada; 2001. pp. 1–61. Cat. no. 82F0086-XDB. [Google Scholar]
- 19.Southern D, McLaren L, Hawe P, Knudtson ML, Ghali WA. Individual-level and neighborhood-level income measures: agreement and association with outcomes in a cardiac disease cohort. Med Care. 2004;43(11):1116–22. doi: 10.1097/01.mlr.0000182517.57235.6d. [DOI] [PubMed] [Google Scholar]
- 20.Roos NP, Mustard CA. Variation in health and health care use by socioeconomic status in Winnipeg, Canada: Does the system work well? Yes and no. Milbank Q. 1997;75(1):89–111. doi: 10.1111/1468-0009.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reid RJ, MacWilliam L, Verhulst L, Roos N, Atkinson M. Performance of the ACG case-mix system in two Canadian provinces. Med Care. 2001;39(1):86–99. doi: 10.1097/00005650-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 22.The Hopkins ACG case-mix system. 2003. [accessed 2004 Nov 10]. http://www.acg.jhsph.edu/
- 23.Broemeling AM, Watson D, Black C. Chronic conditions and co-morbidity among residents of British Columbia. Vancouver: Centre for Health Services and Policy Research. Vancouver: Centre for Health Services and Policy Research; 2005. http://www.chspr.ubc.ca/files/publications/2005/chspr05-08.pdf. [Google Scholar]
- 24.Wolfson M, Rowe G. On measuring inequalities in health. Bull World Health Organ. 2001;79(6):553–60. http://www.who.int/bulletin/pdf/2001/issue6/vol.79.no.6.553-560.pdf. [PMC free article] [PubMed] [Google Scholar]
- 25.British Columbia Ministry of Health, Centre for Health Services and Policy Research (UBC) Access policy for research uses of linked health data. Victoria: British Columbia Ministry of Health; 1996. pp. 1–21. [Google Scholar]
- 26.Beck RG, Horne JM. Economic-class and risk avoidance — experience under public medical-care insurance. J Risk Insur. 1976:73–86. [Google Scholar]
- 27.Asada Y, Kephart G. Equity in health services use and intensity of use in Canada. BMC Health Serv Res. 2007;7:41. doi: 10.1186/1472-6963-7-41. http://www.biomedcentral.com/1472-6963/7/41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nabalamba A, Millar WJ. Going to the doctor. Health Rep. 2006;18(1):23–35. [PubMed] [Google Scholar]
- 29.Canadian Institute for Health Information. The status of alternative payment programs for physicians in Canada. Ottawa: The Institute; 2005. [Google Scholar]
- 30.Carlsen B, Norheim OF. BMC Health Serv Res. 2005;5:70. doi: 10.1186/1472-6963-5-70. http://www.biomedcentral.com/1472-6963/5/70. [DOI] [PMC free article] [PubMed] [Google Scholar]