Abstract
The Aging in Place Project at the University of Missouri (MU) required legislation in 1999 and 2001 to be fully realized. An innovative home health agency was initiated by the Sinclair School of Nursing specifically to help older adults age in place in the environment of their choice. In 2004, an innovative independent living environment was built and is operated by a private long term care company, as a special facility where residents can truly age in place and never fear being moved to a traditional nursing home unless they choose to do so. With care provided by the home care agency with registered nurse care coordination services, residents receive preventative and early illness recognition assistance that have markedly improved their lives. Evaluation of aging in place reveal registered nurse care coordination improves outcomes of cognition, depression, activities of daily living, incontinence, pain, and shortness of breath as well as delaying or preventing nursing home placement. Links with MU students, faculty, and nearly every school or college on campus enrich the lives of the students and residents of the housing environment. Research projects are encouraged and residents who choose to participate are enjoying helping with developing cutting technology to help other seniors age in place.
Keywords: Aging in place, long term care, assisted living, independence, technology
For those who have experienced traditional nursing homes, assisted living, or senior housing in America, few have been satisfied that the environment or services are ideal for older adults. Those who work in long term care settings struggle with the desire to change their environment and their care delivery systems while meeting the demands and constraints of regulatory oversight. Regulators struggle to meet their obligations to the public for oversight that assures minimum safety and care standards; they see on-going problems that could have solutions, but are constrained by the limitations of the regulations they must enforce.
Setting those constraints aside, an idea was initiated to do things differently. Collaborative relationships were forged with federal and state agencies, university schools and departments, and with a major long term care corporation, Americare, of Sikeston, Missouri. This article recounts a case study of the challenges of pursing and achieving the dream of re-inventing traditional long term care. The results of evaluation research of aging in place conducted throughout this endeavor are discussed.
THE SPARK
A group of nursing faculty and administrators from the University of Missouri-Columbia (MU) undertook the challenge of creating a new model of long term care. This challenge was sparked when several nursing faculty and the dean of the Sinclair School of Nursing (SSON) attended the 1996 American Academy of Nursing meeting where participants were challenged to re-envision care and services for the looming expansion of elders (Rantz et al., 2005). Several at the SSON had experience working in long-term care, had active research programs focused on improving care to older adults, and many had a desire to see things done differently (Rantz, Marek, & Zwygart-Stauffacher, 2000). Older adults and their family members who participated in faculty research projects about aging services consistently related how they wanted to stay at home as long as possible; they feared moving to a nursing home (Rantz et al., 1998, 1999).
In addition to their own research findings and experience, faculty considered lessons learned from several community based service models of nursing case management (Abt 2000; Elkan et al., 2001; Naylor et al, 1999; Collins et al., 1997) and from early demonstrations for nursing home diversion programs (Kemper, 1990; Hughes, 1985). A large interdisciplinary group was convened to discuss ideas that were germinating about a special focus project for the SSON that would re-invent long term care to better meet the needs of elders of the future.
THE VISION
With involvement from many disciplines (health services management, social work, medicine, health professions, environmental design and nursing), the group reached consensus that with the right supportive and restorative services it would be possible to help older adults improve their health and well-being, with most avoiding the need for traditional nursing home care. With that vision, the Aging in Place Project (AIP) began, where seniors would be able to age in place in the home environment of their choice with supportive health care services as needed (Marek & Rantz, 2000).
There was also the concern about rising costs of long term care, particularly nursing home care, so the vision was to create a cost-effective alternative to nursing home care, an alternative responsive to elders’ health care needs and consumer preferences. The foundation of AIP is nurse care coordination (case management) and health care services provided as needed to older adults residing in specially designed senior apartments, other senior private or public congregate housing, or in their own homes in the community (Marek & Rantz, 2000; Rantz, 2003).
Another foundation principle is that people do not have to move from one level of care delivery to another, as their health care needs increase. Frail older adults have the opportunity to ‘age in place,’ in the environment of their choice. Aging in Place is a healthier approach compared to traditional long-term care that forces people to move from one setting to another as needs change. Forced relocation results in mental decline, physical deterioration, and even premature death (Johnson, 1999; Manion & Rantz, 1995; Rantz & Egan, 1987). In the AIP approach, all services a person may eventually need are close and available as needed so there is no need to move to a different place (Marek & Rantz, 2000).
The AIP project has two major complementary parts: an innovative home care agency (Sinclair Home Care) and an innovative independent living environment named after the MU mascot, the Tiger, (TigerPlace). The AIP project required legislation in Missouri to be fully realized.
INNOVATIVE HOME CARE AGENCY
In 1999, an innovative home care agency, Sinclair Home Care, (http://www.homecare.missouri.edu/) was created as a department within the SSON. The agency is a licensed Medicare certified home health agency and an in-home provider of supportive services that is funded through a state community-based long term care program and private pay services. From the outset, Sinclair Home Care was designed to provide community-based care to the residents of TigerPlace (a state of the art senior independent living and care option), and residents of other private congregate senior housing, public senior housing, and private homes of community-dwelling seniors in Boone County, Missouri. The SSON obtained a $2 million grant from the federal Centers for Medicare and Medicaid (CMS) to build the infrastructure for Sinclair Home Care and to evaluate the effectiveness of the aging in place model of care (Marek & Rantz, 2000).
Since its inception, the home care agency has served nearly 3000 clients in its service area of Boone County (where MU is located) and most surrounding counties. The agency serves about a hundred Medicare and private insurance clients each month, about 70 AIP clients in official state recognized AIP settings, as well as in-home and private pay clients. Sinclair Home Care is also a wonderful clinical site for students at MU. All nursing students have community experiences through the agency; nearly 600 nursing students have had clinical experiences with home care clients and staff. Engineering, communication, business, physical therapy, social work, and medical students and residents also have good community based experiences in their courses and practices. Faculty members pursue research agendas that involve the agency and it is a cornerstone for training grants to enhance geriatric education. To date, total grant funding of projects using Sinclair Home Care is over $5 million.
REQUIRED LEGISLATION
Legislation that enabled this project was passed in the Missouri legislature in 1999 and 2001. This legislation was needed to designate four “aging in place” demonstration sites in the state that are regulated by the Missouri Department of Health and Senior Services (MODHSS), but regulated differently from traditional nursing homes or residential care (assisted living). Project sites applied to be accepted as a demonstration site. The MU Sinclair School of Nursing was awarded to be one of those sites.
Two project locations were approved for the SSON, TigerPlace, the innovative independent living cooperative project initiated by the SSON and built by the Americare Corporation of Sikeston, Missouri, and the Maplewood apartments at Lenoir Woods, a traditional continuing care retirement community in Columbia, Missouri. Both locations are just a few miles from the MU campus. Detailed service agreements were executed between Sinclair Home Care with Americare and Lenoir Woods.
Representatives from each of the four sites in the state met with MODHSS staff monthly, then quarterly, to develop draft regulations and share ideas as the projects were developed and implemented. This was new territory for both state staff as well as the providers who embarked on a journey into uncharted areas of long term care. The vision of the legislator who initiated the required legislation was to truly develop a new approach to long term care. He was called upon to articulate that vision to help new state staff and providers stay on track and move outside traditional approaches to regulate the care not just regulate the building where the care takes place. Representatives from the SSON and Americare participated in the state agency convened meetings to guide the legislative initiative, and continue to do so as the project has been implemented. Sites agreed to evaluate the effectiveness of AIP in each innovative approach they pursued so that the model could be replicated if effective.
MODHSS staff conducts required surveys of the AIP locations to assure compliance with the AIP regulations and any other applicable nursing home or residential care regulations. For TigerPlace, the building, housing, and health care services are surveyed annually by MODHSS long term care regulation staff. Additionally, Sinclair Home Care as an agency is surveyed by home care regulators of the MODHSS to assure compliance with home care regulations.
AN INNOVATIVE HOUSING ENVIRONMENT
To fully implement and evaluate the AIP model in an ideal housing development, an innovative independent living facility was designed. In this environment, the expressed goal of AIP is to maximize and promote independence for the older adults who live there. The Americare Corporation of Sikeston, Missouri, in collaboration with the SSON designed TigerPlace. Faculty from many colleges and schools participated in the planning and design. Nurses, physical therapists, occupational therapists, and specialists in environmental design participated in the actual building plan. Faculty from Computer Engineering participated in planning for implementation of technological advances on the horizon so new technology can be readily installed throughout the building. Ongoing research is being conducted and pursued by faculty and students from various schools combining the AIP model and technology enhancements, coined as eldertech. The goal of the research is to promote independent living.
TigerPlace is located just a few miles from the MU campus on about six acres of land adjacent to two other Americare facilities (an Alzheimer’s assisted living and a residential care assisted living). Construction began in spring 2003 for Phase 1 of TigerPlace, a 34,000 square foot development of 33 apartment units. The Phase 1 building was occupied beginning in June 2004. Additional apartment units are planned in additional phase(s) as demand and service use is demonstrated for the project. An additional 24 units are in the construction phase at this time as the current building is fully occupied and many people are on a waiting list.
The building was actually built to skilled nursing facility standards, but it does not in any way look like a traditional nursing home. Each apartment is fully self-contained with separate heating and air-conditioning units with no co-mingling of air handling. Each has its own fully equipped kitchen and washer and dryer. There are two exterior exits for each apartment, one through a private screened porch and the other into a facility corridor that connects each apartment to central services and generous common spaces for all to enjoy. The interior corridors have magnifying light tubes that provide natural light through all the interior spaces, even on cloudy days, helping those with low vision. The links to MU are evident in the decorating, large framed photos of historic views of the campus, and the soft elegant touches of black and gold (the university’s colors). Familiar names of campus features and neighborhoods surrounding the campus are used to name the neighborhoods and common areas of TigerPlace, such as the Bengal Lair, a sports bar that is busy at happy hour and during sports events displayed on a large flat screen television.
The building is licensed as an intermediate care facility. This facilitates using private long term care insurance benefits to offset the costs of living at TigerPlace, when a resident has needs that would meet the qualifying criteria of a particular insurance plan. Some long term care insurance plans also cover home care services, which are available from Sinclair Home Care when needs arise for any resident. A most important feature of TigerPlace is that residents are allowed to age in place and live in their own apartment for the rest of their life, never being forced to move to a nursing home, unless that is their choice. Because TigerPlace is part of the AIP Missouri Demonstration Project, because the building was built to nursing home standards, and because care can be provided as needed by Sinclair Home Care, residents may live in their apartments as long as they wish. To date, several residents have died since moving to TigerPlace with family, friends, hospice, and home care services to help them to a peaceful death. For more information on Tigerplace please visit the following website: http://nursing.missouri.edu/practice/tigerplace.php
AN INNOVATIVE CARE DELIVERY MODEL
Care coordination by a registered nurse is central to the success of AIP. Care delivery is organized around a wellness center strategically placed near the dining room and sports bar. Labeled TigerCare, the wellness center is staffed by a registered nurse care coordinator who is on the staff of Sinclair Home Care. At the TigerCare wellness center, there is on-going assessment of resident needs and health promotion activities including exercise and health classes to help residents remain active and vital. Residents have a comprehensive health assessment upon moving to TigerPlace and then every six months by the care coordinator. The TigerCare wellness center is open three mornings each week and residents have easy access to the registered nurse during these hours. After hours, residents may call the Sinclair Home Care registered nurse on call with questions or concerns. All residents have access to a registered nurse 24 hours a day.
Residents also have four private home visits per year and exercise classes five days per week included with their base health care package as a part of living at TigerPlace. Recently, a personal care assistant has been added to routine morning and evening staffing of TigerPlace by Sinclair Home Care to assist residents with activities of daily living in the morning and evening times. Sinclair Home Care provides an array of home care services such as medication management, assistance with activities of daily living, and care coordination of health conditions with residents’ physicians and other health care providers. Medicare home health care is provided by Sinclair Home Care when residents need and qualify for that service.
SPECIAL PET PROGRAM
Pets are welcome at TigerPlace. Several residents brought their family pets when they moved into TigerPlace and others have adopted since moving in. The building is designed to be “pet friendly.” For example, each apartment has an exterior door for easy outdoor access, screened porches, and wide windowsills for cats to enjoy. Furthermore, as one part of the TigerPlace Pet Initiative (TiPPI), the building has a veterinary exam room where pets have regular health care and treatment by students and faculty of the MU College of Veterinary Medicine. Services are also available for individuals who require pet sitters, or who would like help in finding an animal to adopt. An endowment fund enables foster care for pets who outlive their owners, or for pets whose owners are no longer able to take care of them. Another component of TiPPI is the feeding program in which residents can purchase excellent pet food at a low cost. The most recent addition to TiPPI is a weekly program called PAWSitive Visits which brings interesting animals and birds to TigerPlace. The program has included chinchillas, rabbits, cats, dogs, a horse, a giant horned owl, a screech owl, a pot-bellied pig. Perhaps the most successful visit was the private appearance of the MU College of Veterinary Medicine mascot Mule Team, a special team of two mules that appear at major MU events and maintained by MU veterinary students.
OVERALL COLLABORATION
Americare staff are responsible for operation of the housing and hospitality services for TigerPlace. These include dining, housekeeping, maintenance of the apartments and building, billing for services, transportation, social and recreational activities. MU staff are responsible for the health care services, planning care, daily exercise programs, veterinary services, and linking the MU community of faculty and students with TigerPlace residents as well as social, recreational and educational activity planning linked to MU.
STUDENT EXPERIENCES AT TIGERPLACE
A major value of undertaking a collaborative project such as TigerPlace is for students to enrich the lives of residents and for residents to enrich the lives of students. From an educational point of view, faculty members want to better prepare students for the future with the growing aging population. If students have positive experiences with older adults, they may be interested in pursing career paths in gerontology.
There is no limit to possible student experiences at TigerPlace, creative ideas are sought from faculty, staff and students as each semester is planned. Since opening in June 2004, well over 300 students from many schools and colleges have enriched the lives of TigerPlace residents and had their lives enriched by the residents. For example, nursing students have interviewed most of the residents to assess their activity interests to help plan recreational and social activities. Occupational therapy students have applied massage therapy skills, which residents really enjoy. Horticulture students have planned individual gardens for residents outside their screened porches. Veterinary medicine students provided annual exams and care of dogs and cats of TigerPlace. Graduate students have pursued their master’s projects that have included an evaluation of universal design principles at TigerPlace and life histories. Undergraduate business and engineering students are working together to plan and produce new products to meet special needs of older adults such as a specially designed walker with automatic brakes.
PRELIMINARY RESULTS OF AGING IN PLACE EVALUATIONS
There are two evaluations of the Aging in Place concept at MU underway. A federally funded evaluation (Centers for Medicaid and Medicare (CMS) funded, Marek PI, 1999–2003) and a state mandated evaluation of legislation piloting AIP in four pilot sites in Missouri, including the one for which the SSON is responsible at TigerPlace and Lenior Woods.
With the CMS funded evaluation of AIP, an extensive data collection and evaluation was conducted of the clinical and cost outcomes of older adults helped with a nursing care coordination intervention. Participants included seniors living in their private homes, senior congregate housing (non-licensed), and public congregate housing. Comparison groups included seniors in the community receiving traditional state-funded in-home services and a cohort (acuity, age, cognitive and activity of daily living matched) who entered skilled nursing homes.
The outcome analyses of the CMS funded evaluation revealed that AIP intervention clients had significantly better outcomes in cognition, depression, activities of daily living, and incontinence than a matched cohort of nursing home residents at 6, 12, 18, and 24 months (Marek et al., 2005). In the comparison of the AIP clients with traditional state-funded in-home services, at 12 months, the AIP nurse care coordination clients had significantly better outcomes of pain, shortness of breath, and activities of daily living (Marek et al, 2006). Results suggest that community based care with registered nurse care coordination enhances clinical outcomes of long term care clients. In another analysis of 700 clients served in the AIP CMS funded evaluation, nurse care coordination delayed or prevented nursing home placement for 250 clients served in the beginning years of the operation of Sinclair Home Care (Unpublished data, Marek & Rantz, 2004). Most of these clients were using Medicaid in-home services to help with activities of daily living while they lived independently in subsidized public congregate housing or private homes. With the help of a registered nurse care coordinator and sometimes an electronic medication dispensing machine in their home, these frail elders could remain at home, where they wanted to live.
Cost effectiveness analyses are underway at this time. It is anticipated that the total costs of AIP registered nurse care coordination in the community are at least no greater than the costs of nursing home care, is far preferred by older adults, and improves their functional outcomes of care. If costs of delaying or preventing nursing home placement are considered, the cost savings of community based nurse care coordination are considerable.
For those AIP clients living in public congregate housing, their improvements and stability of chronic physical and mental illnesses using the RN care coordination model was quite remarkable. Public housing officials were so pleased with reductions in resident conflicts (related to mental illnesses), police calls to the apartments, emergency room visits for acute illnesses or acute exacerbations of chronic illnesses, and better social interactions among residents, that they applied and obtained grant funding to continue the AIP care coordination program and on-site wellness center for two years after the CMS grant ended.
For the state evaluation of AIP, a research team in the SSON with collaborators from the School of Medicine and other MU schools and colleges is guiding the data collection and analysis. Data collection has been underway at TigerPlace and Lenior Woods since mid-2004. Data about functional status, hospitalization, emergency room use, and medication use are to be evaluated across all state sites as a part of the legislatively mandated state evaluation. Preliminary analyses are anticipated soon. Anecdotal evidence of high resident satisfaction, early illness recognition, and health promotion activity acceptance indicate preliminary positive results.
RESEARCH ACTIVITIES AT TIGERPLACE
It was envisioned that research activities would bring together diverse researchers across the MU campus to propose new approaches to common, persistent problems that older adults face. Such problems include detecting adverse health events such as falls, or other situations that may require immediate assistance. Much deterioration can be prevented if problems like these can be detected in seconds or minutes, not hours or days. The team is working on predicting that adverse health events are about to happen. This predictive approach can address problems that have plagued long-term community-based care and facility-based care for decades. With early impending illness recognition and quick detection of adverse events like falls, resident outcomes can be improved through health promotion interventions such as strength training or early illness treatment.
TigerPlace provides researchers with a unique opportunity in which to develop and evaluate technology in a collaborative setting that is affiliated with the SSON. At MU, faculty from Electrical and Computer Engineering, Health Informatics, Health Professions, Schools of Social Work, Medicine and Nursing have come together to conduct interdisciplinary research projects to improve the quality of life and care of seniors (Rantz et al., 2005). With interdisciplinary expertise, research is underway that will not only improve the lives of the residents at TigerPlace, but plans are to deploy and test the technologies developed so that seniors in other settings can benefit from this work.
The major focus of the collaborative research underway at TigerPlace (funded by the National Science Foundation, Skubic, PI, and the Administration on Aging, Rantz, PI) is to investigate the use of sensors to monitor and assess potential problems in mobility and cognition of elders in their home. The aims are to develop and deploy technology to sense alert conditions such as falls, and changes in daily patterns that may indicate impending health problems. The components of the system include an in-home monitoring system, an event-driven anonymized video-sensor network, and a component for automated activity analysis and behavior reasoning.
The In-Home Monitoring System (IMS) (Alwan et al., 2003) consists of a set of wireless infrared motion sensors and pressure switch pads (sensor mats) that can be used to infer specific activities. Faculty members at MU collaborated with colleagues at the Medical Automation Research Center (MARC) at the University of Virginia to test the IMS in apartments at TigerPlace. A stove temperature sensor and sensors on cabinet doors are also being used. The system is augmented with a bed sensor capable of detecting presence, respiration (normal or abnormal), pulse (low, normal or high) and movement in the bed (Alwan et al., 2003a).
An event-driven anonymized video sensor network complements the IMS, as the visual information helps reduce false alarms generated by the motion sensors or fall detector. In order to preserve the privacy of the residents, algorithms are developed to find a moving person in the image and extract a silhouette (Chen et al., 2006; Wang et al., 2003). Important feature variables are then extracted from the silhouette to characterize the person’s movement and used for statistical activity analysis. Analysis of short term activities, such as falls, is accomplished using a hidden Markov model (HMM) (Anderson et al., 2006).
The final component of the system is the behavioral reasoning system that captures typical patterns of activities for an individual and recognizes deviation from the normal pattern. We are investigating different techniques for this component, including a fuzzy logic rule base (Wang, 2006) and a hierarchical HMM. Fuzzy rules are advantageous in that a linguistic description can be used to represent the rules so they are easily understood by health care staff. In addition, new rules based on geriatric expertise can readily be incorporated into the system. This is especially useful for cases not in the training data (because they are statistically unlikely to occur) but important nonetheless because of potential safety concerns.
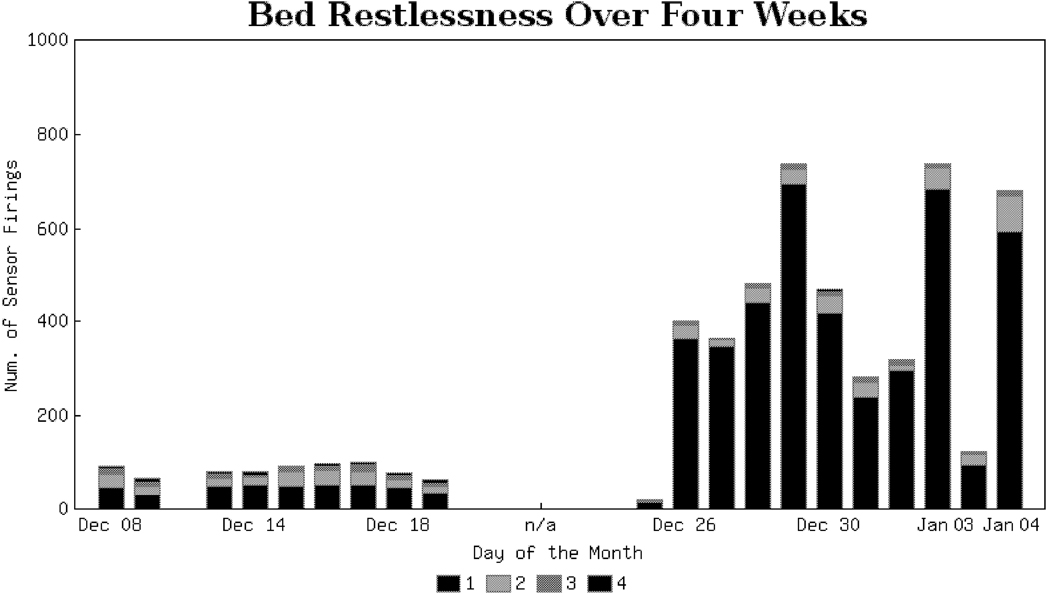
An example of the use of these systems begins with the acquisition of the bed sensor data that is analyzed and displayed in a restlessness histogram that is a count of the frequency of resident’s motion over time (see Figure 1). The bars on the display are color coded to show four levels of restlessness from level 1 (least restless) to level 4 (most restless). Longitudinal comparisons give an indication of changes in sleep patterns, which can be interpreted by health care staff as potential changes in the resident’s health status that require assessment of the resident and further investigation for early illness recognition. Using computational intelligence techniques described above, sensor data are modeled to develop expected patterns of activities. When deviations from those patterns are detected this may indicate a change in the resident’s health status or activity behaviors for some health-related reason.
FIGURE 1.
Bed Restlessness Data Graph, showing different levels of restlessness from level 1 (least restless) to level 4 (most restless)
The research team is also concerned about willingness of older adults to accept technology in their apartments or homes. Before deployment of the sensors in any apartments, a series of focus groups were conducted to evaluate the older adults’ attitudes and perceptions of smart home technologies in general, asking subjects to identify what activities of daily living could be enhanced by technology; what types of technologies they were familiar with; and what technologies they would be willing to accept (Demiris et al., 2004). This work indicated that older adults were concerned about falls and that they perceived technologies that monitor activity levels and sleep patterns as useful. The older adults emphasized the need for non-obtrusive systems. This work informed the design of specific technologies that were chosen to be installed in the TigerPlace apartments.
Initial follow-up focus groups and interviews have been conducted, and additional are planned to investigate older adults’ perceptions of the specific smart home technologies employed by the TigerPlace project (i.e., a bed sensor, gait monitor, stove sensor, motion sensor, and video sensor); perceived advantages and concerns associated with these types of technology; willingness to adopt such technologies in their own residence; and preferences about recipients of sensor-generated information pertaining to their activity levels, sleep patterns and potential emergencies. This follow-up work provides insight into older adults’ attitudes towards specific sensor technologies and captures the level of willingness to allow installation of such technologies and to share associated personal data with other stakeholders (Demiris et al., 2006).
Other research projects are possible and encouraged at TigerPlace as well as at Sinclair Home Care. For example, a current team at Sinclair Home Care is developing approaches to use the information system to evaluate outcomes of care and efficacy of care using advanced informatics methods. Since TigerPlace has been built, almost $4 million in grant funding as been successfully obtained for research to develop and deploy sensor networks of technology to enhance aging in place. To date, total research and training grant dollars involving Sinclair Home Care and/or TigerPlace total over $8 million; this is viewed as a successful academic research venture for a very high research activity university (Carnegie RU/VH, University).
LESSONS LEARNED: THREE YEARS OF COLLABORATION BETWEEN PUBLIC, STATE, AND PRIVATE PARTNERS
Following through with the implementation of a new model of care delivery has been an incredible journey. First, developing a sound working relationship between the partners of the SSON and Americare staff who were responsible for building the innovative environment was, and still is, essential to success. Additionally, a solid working relationship and commitment to piloting AIP from the Missouri Department of Health and Senior Services staff responsible for surveying this special project is critical. From the outset, all partners, faculty of SSON, staff of Americare, and state agency staff agreed to be true to the principles of AIP: maximizing independence, dignity, and health promotion. The men and women who live at TigerPlace are the number one priority, so with that common ground, dealing with the logistics of day-to-day operations becomes possible. Communication and team work is essential. Resident satisfaction with living at TigerPlace is high. All apartments were occupied quickly, within a few months of opening, and continue to be fully occupied with a waiting list of those who want to move in.
From the outset, cooperative operations meetings with Sinclair Home Care staff, SSON faculty, and Americare staff were planned, first more frequently than monthly, and then monthly. Between those official face-to-face times, almost daily contact between the nurse care coordinator responsible for TigerPlace, the administrator, and other staff at TigerPlace is common. Two key nurse faculty from SSON are on-site at least weekly, involved in activities, student experiences, and health care issues. Other faculty from MU are on-site for weekly technology research meetings to implement the funded research projects and develop new research projects for the future. Representatives from both the SSON and Americare attend state sponsored meetings held for the project sites.
The electronic information system of Sinclair Home Care has been critical to implementing the model of AIP. Since a nurse is not on-site 24 hours a day, seven days a week, a reliable communication network of nurse response is essential. This has been accomplished by keeping all health information in the Sinclair Home Care database that is accessible by laptop by all the registered nurse care coordinators who work for the agency. When there is a call after hours from a resident at TigerPlace, the home care nurse on call takes the call, accesses the needed up-to-date health information so that the concern can be handled by an informed nurse. The average number of calls per month after hours from TigerPlace residents is about five per month. Although that is not a high number, it is critical that the nurse be informed so the concern can be handled accurately and needless trips to the emergency room avoided. Using a traditional paper chart would make using an on-call system with the home care nurse impossible to achieve with accuracy.
Having a school of nursing undertake a project like this has real advantages for practice, research, and educational experiences for students. Beyond nursing students, students from many schools and colleges can and are benefiting from the special relationship between MU and TigerPlace. Many of the residents thoroughly enjoy helping the students gain valuable insights from them and helping young people understand the issues and joys of aging. They enjoy participating in the learning activities of the students and see those as enhancements to their lives at TigerPlace.
From a practice and research perspective, faculty members are challenged to develop new ways of thinking about care delivery and actually participate in the development and testing of new ideas. The practice setting is fertile ground for new research questions and challenges. Interdisciplinary research activities are perceived as relevant to researchers because many have experienced problems with older family members and they are excited about the possibility of actually solving a problem they experienced first hand. For example, most researchers of the TigerPlace technology research team have experienced family members who have fallen at home and have not been discovered for hours or even a day or more, or family members whose acute illnesses went undetected for days. Researchers see potential solutions to helping people live more independently, safely, and longer in the privacy of one’s own home or apartment through the use of technologies to detect and alert staff of potentially adverse health events.
With successful health promotion activities and encouragement, residents of TigerPlace are enjoying their better health and abilities to remain active. With those abilities comes a desire to continue to find meaning and purpose in living and involvement with peers, family, and friends. One successful program that both residents and students enjoy is the Senior Teacher Education Partnership (STEP) program in the School of Medicine at MU. Each medical student is connected with an older adult in the community who is living independently and develops a long term relationship with the senior throughout their medical school experience. These relationships are very important to both the senior and the student; many become friends who keep in touch for many years. Both developing new relationships and maintaining old ones are keys to have continuing purpose in life. Staying connected with friends and family in the community and community activities can help with developing and maintaining relationships. Staff at TigerPlace are very committed to facilitating community connections by providing transportation as requested by residents, available every day. Faculty members at MU are committed to making connections with faculty, staff, and students to TigerPlace and helping residents get involved with events at the MU campus.
Some extremely valued activities by residents include a twice monthly “Poker Night,” an event full of fun and laughter started by a husband of SSON faculty. “Happy Feet” is a group activity (segregated, one for women and one for men, at their initiative) started by a volunteer nurse in the community who enjoys foot care; student nurses now participate when they are in their gerontological clinical class and are enjoying it, too. A retired nurse alumni of the SSON has joined residents in “Afternoon tea,” so enjoyed by many women at TigerPlace. “Talk and Sew,” initiated by a SSON faculty, is popular with the women who are interested in quilting or other sewing activities, or just talking while others do “show and tell” with projects they are working on or completed years ago.
Another valued activity that developed is a support group for some of the nurse daughters who have a parent or parents who have moved to TigerPlace. This started as a “let’s go to dinner and talk” activity that the nurses have found helpful and fun. They meet at a local restaurant for a meal and conversation. Many new ideas have been generated by this talented group such as helping to identify appropriate learning opportunities for students that would be meaningful for their parents and volunteer opportunities for their parents to enrich the lives of TigerPlace residents who want to contribute to the Columbia community. Two residents are weekly volunteers for a community-based organization helping those with developmental disabilities in the Columbia area; another resident is now volunteering at the University Hospital, directing visitors to locations throughout the complex of buildings.
Some ideas for improvement of the model include locating the housing building within walking distance of campus. This has also been recommended by others building university-based retirement communities (Larkin, 2007). This was not possible in Columbia due to land issues near MU, but if others pursue this idea and can find a location on which to build where walking to the campus is possible, that should be pursued. This has not been an insurmountable problem since transportation is provided for those who want to go to MU events. However, walking access would likely be valued by the residents and make it easier for student participation.
Another idea is to revisit what we learned applying the AIP model in public congregate housing. With public financing for building, a low-income version of TigerPlace could be developed with health care supplemented by our current state funded Medicaid In-Home Services Program. It would be necessary to obtain other funding for the necessary RN care coordination, as in Missouri and many other states, there are no Medicaid funds for this critical nurse service. With a creative solution to the issue of funding RN care coordination, developing a low income TigerPlace AIP project is quite feasible.
As the project matures, there will likely be more lessons learned. At this stage, all who are connected with TigerPlace, the students, faculty, staff of Americare, residents and families are pleased to have an aging in place option for them to pursue. Researchers will continue to advance the state of technology to help people age in place. Students will have new experiences that teach them important life skills with older people. Staff have an exciting cutting edge place to work. Families and residents have a wonderful option that encourages maximizing independence, dignity, and health promotion with the assurance that if they choose, they will never have to move to a traditional nursing home.
Acknowledgments
The authors wish to acknowledge the organizations and staff who made the AIP project possible: Americare of Sikeston, MO; TigerPlace staff; Sinclair Home Care staff; MU Sinclair School of Nursing faculty and deans; MU administration; Missouri Department of Health and Senior Services staff; Missouri state legislature (in particular, Tim Harlan of Columbia, MO); and all the friends and families who have supported those who implemented this pioneering effort.
REFERENCES
- Abt Associates Inc. Evaluation of the Community Nursing Organization Demonstration Final Report. Cambridge, MA: 2000. Apr, [Google Scholar]
- Alwan M, Kell S, Dalal S, Turner B, Mack D, Felder R. In-Home Monitoring System and Objective ADL Assessment: Validation Study. Intl. Conf. on Independence, Aging and Disability; Washington, DC. 2003. [Google Scholar]
- Alwan M, Dalal S, Kell S, Felder R. Derivation of Basic Human Gait Characteristics from Floor Vibrations. 2003 Summer Bioengineering Conference; Sonesta Beach Resort in Key Biscayne; Florida. 2003a. Jun 25–29, [Google Scholar]
- Anderson D, Keller J, Skubic M, Chen X, He Z. Recognizing Falls From Silhouettes. Proceedings, IEEE 2006 International Conference of the Engineering in Medicine and Biology Society; New York, NY. 2006. August 30–September 3, pp. 6388–6391. [DOI] [PubMed] [Google Scholar]
- Chen X, He Z, Keller J, Anderson D, Skubic M. Adaptive Silouette Extraction In Dynamic Environments Using Fuzzy Logic. Proceedings, 15th IEEE International Conference on Fuzzy Systems; Vancouver, Canada. 2006. Jul, pp. 832–839. [Google Scholar]
- Chen X, He Z, Anderson D, Keller J, Skubic M. Adaptive Silhouette Extraction and Human Tracking in Complex and Dynamic Environments. Proceedings, International Conference on Image Processing; Atlanta. 2006. Oct, pp. 561–564. [Google Scholar]
- Colins C, Butler FR, Gueldner SH, Palmer MH. Models for Community-base long-term care for the elderly in a changing health system. Nursing Outlook. 1997;45:59–63. doi: 10.1016/s0029-6554(97)90080-4. [DOI] [PubMed] [Google Scholar]
- Dermis G, Skubic M, Rantz M, Hensel B. Smart home sensors for aging in place: Older adults’ attitudes and willingness to adopt. The Gerontologist. 2006;46(Special Issue 1):430. [Google Scholar]
- Demiris G, Rantz MJ, Aud MA, Marek KD, Tyrer HW, Skubic M, Hussam AA. Older adults’ attitudes towards and perceptions of “smart house” technologies. Medical Informatics and the Internet in Medicine. 2004;29(2):87–94. doi: 10.1080/14639230410001684387. [DOI] [PubMed] [Google Scholar]
- Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, Blair M, Williams D, Brummell K. Effectiveness of home based support for older people: systematic review and meta-analysis. British Medical Journal. 2001;323:1–9. doi: 10.1136/bmj.323.7315.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes SL. Apples and Oranges? A review of evaluation of community-based long-term care. Health Services Research. 1985;20(4):461–488. [PMC free article] [PubMed] [Google Scholar]
- Johnson RA. Helping older adults adjust to relocation: Nursing interventions and issues. In: Swanson L, Tripp-Riemer T, editors. Transitions in the Older Adult. New York: Springer; 1999. pp. 52–72. [Google Scholar]
- Kemper P. Case management agency systems of administering long-term care: Evidence form the channeling demonstration. The Gerontologist. 1990;30(6):817–824. doi: 10.1093/geront/30.6.817. [DOI] [PubMed] [Google Scholar]
- Larkin M. University-based retirement communities on the rise. The Journal on Active Aging. 2007;6(2):52–59. [Google Scholar]
- Manion PS, Rantz MJ. Relocation stress syndrome: A comprehensive plan for long-term care admissions. Geriatric Nursing. 1995;16(3):108–112. doi: 10.1016/s0197-4572(05)80039-4. [DOI] [PubMed] [Google Scholar]
- Marek K, Popejoy L, Petroski G, Mehr D, Rantz MJ, Lin W. Clinical outcomes of aging in place. Nursing Research. 2005;54(3):202–211. doi: 10.1097/00006199-200505000-00008. [DOI] [PubMed] [Google Scholar]
- Marek KD, Popejoy L, Petroski G, Rantz MJ. Nurse care coordination in community-based long-term care. Journal of Nursing Scholarship. 2006;38(1):80–86. doi: 10.1111/j.1547-5069.2006.00081.x. [DOI] [PubMed] [Google Scholar]
- Marek KD, Rantz MJ. Aging in place: A new model for long term are. Nursing Administration Quarterly. 2000;24(3):1–11. doi: 10.1097/00006216-200004000-00003. [DOI] [PubMed] [Google Scholar]
- Marek, Rantz . Sinclair School of Nursing. University of Missouri-Columbia; 2004. Unpublished data. [Google Scholar]
- Naylor M, Brooten D, Campbell R, Jacobsen BS, Mezey M, Pauley, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized controlled trial. Journal of the American Medical Association. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Egan K. Reducing death from translocation syndrome. American Journal of Nursing. 1987;87(10):1351–1352. [PubMed] [Google Scholar]
- Rantz MJ, Marek KD, Aud MA, Tyrer HW, Skubic M, Demiris G, Hussam AA. Technology and nursing collaboration to help older adults age in place. Nursing Outlook. 2005;53(1):40–45. doi: 10.1016/j.outlook.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Marek KD, Zwygart-Stauffacher M. The future of long-term care for the chronically ill. Nursing Administration Quarterly. 2000;25(1):51–58. doi: 10.1097/00006216-200010000-00015. [DOI] [PubMed] [Google Scholar]
- Rantz MJ. Aging in place. Nurseweek. (Midwest/Heartland Edition) 2003;4(2):7. [Google Scholar]
- Rantz MJ, Mehr D, Popejoy L, Zwygart-Stauffacher M, Hicks L, Grando V, Conn V, Porter R, Scott J, Maas M. Nursing home care quality: A multidimensional theoretical model. Journal of Nursing Care Quality. 1998;12(3):30–46. doi: 10.1097/00001786-199802000-00007. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Zwygart-Stauffacher M, Popejoy L, Grando V, Mehr D, Hicks L, Conn V, Wipke-Tevis D, Porter R, Bostick J, Maas M. Nursing home care quality: A multidimensional theoretical model integrating the views of consumers and providers. Journal of Nursing Care Quality. 1999;14(1):16–37. doi: 10.1097/00001786-199910000-00004. [DOI] [PubMed] [Google Scholar]
- Wang S, Keller J, Burks K, Skubic M, Tyrer H. Assessing Physical Performance of Elders Using Fuzzy Logic. Proceedings, 15th IEEE International Conference on Fuzzy Systems; Vancouver, Canada. 2006. Jul, pp. 2998–3003. [Google Scholar]
- Wang L, Tan T, Ning H, Hu W. Silhouette analysis-based gait recognition for human identification. IEEE Trans. Pattern Analysis and Machine Intelligence. 2003;25(12):1505–1518. [Google Scholar]