Abstract
Objective
To examine the independent and combined influence of individual and community-level socioeconomic (SES) measures with physical health status outcomes in people with self-reported arthritis.
Methods
From 2004-2005, 968 participants completed a telephone survey assessing health status, chronic conditions, community characteristics, and socio-demographic variables. Individual-level SES measures: homeownership, occupation [professional, or not], educational attainment (< high school (HS), HS degree, and > HS), income (<15, 15-45, >$45K) and community poverty: 2000 U.S. Census block-group “% of individuals living below the poverty line” (low, medium, high) were used. Outcomes were physical functioning (MOS SF-12v2 PCS), functional disability (HAQ) and the CDC HRQOL Healthy Days physical and limited activity days and were analyzed via multivariable regressions.
Results
When entered separately, all individual-level SES variables were significantly (p<0.01) associated with poorer PCS, HAQ, and CDC HRQOL scores. A higher magnitude of effect was seen for household income, specifically <$15,000 in final models with all 4 individual SES measures and community poverty. The magnitude of effect for education is reduced and marginally significant for PCS and number of physically unhealthy days. No effects were seen for occupation, homeownership, and community poverty.
Conclusions
Findings confirm that after adjusting for important covariates, lower individual and community-level SES are associated with poorer physical health outcomes, while household income is the strongest predictor (as measured by both significance and effect) of poorer health status in final models. Studies not having participant-reported income available should make use of other SES measures as they do independently predict physical health.
Keywords: Socioeconomic Status, Health Status
The strong association throughout the developed world between lower levels of individual adult socioeconomic status (SES) and poorer health outcomes from many diseases (1-3), including arthritis (4-6) is well-established and recent data suggest that the socioeconomic environment of an individual's neighborhood may be important in this regard, as well (7-9).
Several published studies from the UK, the US and Canada have examined individual and community measures of SES with outcomes in persons with arthritis (8-13). In the UK, the Early RA Study Group found that greater deprivation measured by the Carstairs Index was associated with a worse clinical score among 869 RA patients in England (8). Another UK study using data from the British RA Outcome Study Group found area of residence deprivation (using a Townsend score) was related to RA severity at recruitment and was a predictor of response in a randomized control clinical trial (9). A third UK study used data from the Norfolk Arthritis Register (NOAR), a large primary care cohort study. They examined the relationship between Inflammatory Polyarthritis and functional outcomes with SES at both the personal and area level, and found that individuals living in more deprived areas had poorer HAQ outcome scores (10).
In the US, a report from the Los Angeles Family and Neighborhood Survey found that having a chronic condition (including arthritis) was associated with substantially poorer self-rated health among participants in a deprived area than those in a more advantaged area (12). Neighborhood SES in the form of concentrated poverty was found to contribute to poorer physical functioning and depression scores in individuals with systemic lupus erythematosus (SLE), independent of individual SES (11). A study using the Canadian Community Health Survey found that living in low-income regions was associated with greater likelihood of reporting arthritis, with this relationship remaining after adjustment for individual SES (13).
Previous work by our group has demonstrated the impact of education and community social determinants on health outcomes in patients with self-reported arthritis (14;15). A correlation was demonstrated between lower SES, specifically educational attainment and community poverty, and poor outcomes in health assessment measures (e.g., MOS SF12v2; CDC HRQOL Health Days Measure). Formal educational attainment is, in part, a marker for behavioral variables (16-20). Community social determinants, through the physical, social and service characteristics of local neighborhoods, can clearly impact residents' health.
Many studies examining the association of both individual and community social determinants with outcomes and mortality have been conducted in primarily urban areas (21;22). Also, most studies usually include only one or two measures of individual SES (11-13), if any (23). This study focuses on a cohort of adults recruited from primary care practices from both rural and urban communities across North Carolina, and expands previous work from our group by examining three other measures of individual SES in addition to educational attainment and community poverty level. We include a dichotomous occupation variable, homeownership, and household income as SES measures and expand our physical health status outcomes to include both general health and arthritis specific assessment measures.
Participants and Methods
Study Design
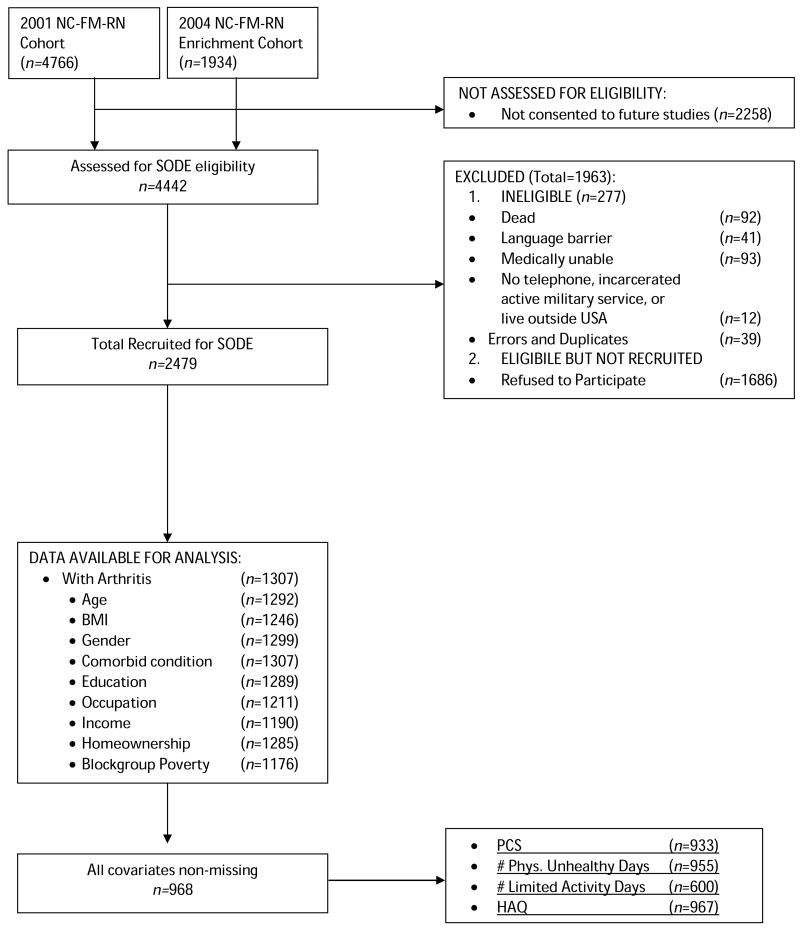
Established in 2001, the North Carolina Family Medicine Research Network (NC-FM-RN) is a practice-based patient cohort for primary care research that is frequently enriched (2004, 2005, 2008). Individuals visiting participating practices who were 18 years of age and older and provided consent to participate in the research study were invited to complete a survey about health conditions and health behaviors (24). This cohort is often used as a population for additional research studies and the current social determinants (SODE) study stems from the NC-FM-RN cohort (Figure 1). In 2004, 4442 NC-FM-RM cohort participants were assessed for eligibility. Of those who had agreed to be contacted for future studies, had a current address and telephone number, and spoke English fluently, 4165 were invited by mailed letter to participate in our study addressing health outcomes. With a 59.5% response rate, 2479 individuals were queried about demographic items, health status, chronic conditions, health attitudes and beliefs and community characteristics in a telephone survey lasting approximately 45 minutes. All study materials and methods were approved by the University of North Carolina at Chapel Hill Biomedical Institutional Review Board.
Figure 1. Participant Recruitment and Participation.
Note: NC-FM-RN = North Carolina Family Medicine Research Network; SODE = Current Social Determinants of Health study; PCS= Physical Component Summary; HAQ= Health Assessment Questionnaire
This paper focuses on the 1307 participants self-reporting arthritis according to the 2002 arthritis module of the Behavioral Risk Factor Surveillance System (BRFSS): any type of doctor diagnosed arthritis, including osteoarthritis, rheumatoid arthritis, gout, lupus or fibromyalgia (25).
Measures
Physical Health Status Outcomes were assessed using the following four established measures:
Physical functioning
The Physical Component Summary (PCS) of the standard Medical Outcome Study's (MOS) Short Form survey (SF-12v2) was used to measure physical functioning. It is used in this study as a continuous variable, with a higher score (range: 0-100) indicating better physical health. The scale is strongly correlated with the SF-36 and is reliable in general populations (26).
CDC HRQOL
The Centers for Disease Control and Prevention Health-Related Quality of Life (CDC HRQOL) Healthy Days measures were used to assess outcomes related to physical health and activity limitation (27). Two questions are used in this paper: 1) “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?”, 2) “During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?” Both measures are assessed on a scale from 0-30, with a higher score or more days indicating worse health; these measures are treated as continuous variables in all analyses. The CDC HRQOL questions have been validated and have good construct, acceptable criterion, and known groups validity (28).
Health Assessment Questionnaire (HAQ)
The HAQ measures self-reported disability in daily function by assessing 20 activities of daily living organized around eight domains: dressing and grooming, arising, eating, walking, hygiene, reach, grip, and outside activities. Level of difficulty for each is assessed on a scale from 0 (no difficulty) to 3 (unable to do). Domain scores are summed (range: 0-24) and divided by 8 to provide a continuous, averaged index value from 0 to 3; a higher score indicating greater disability with a 0.22 change indicating clinical relevance (29).
Main Socioeconomic Predictor Variables were assessed using four individual-level SES measures and one community-level SES measure:
Educational attainment was assessed with seven categories and later trichotomized as less than HS degree, HS degree or GED, and greater than a HS degree (referent).
Household income was assessed using a six response-category format in $15,000 increments, ranging from less than $15,000 to greater than $75,000. For use in this paper, household income was trichotmized as less than $15,000 per year, between $15,000 and $45,000 a year, and greater than $45,000 per year (referent).
Occupation was based on a participant description and coded using 2000 US Census occupation classification categories. This variable was further refined into physically demanding/non-professional- (e.g., farming, fishing, service, construction, production, and labor) and non-physically demanding /professional (e.g., management, technical, sales and office) categories for use in this study, with non-physically demanding/professional as referent.
Homeownership was assessed by asking participants “Do you own your home?” (yes, no) with homeowner as the referent.
Community SES was derived by matching each participant's home address to the related 2000 US Census block group, a geographical entity averaging about 1000 residents (30;31) using MapMarker Plus, Version 7.2. Only results with precise geography were used. The 2000 US Census block group poverty rate (% of the population in households with income below the poverty level) was used as a proxy for community level SES (32). In some studies, block group characteristics have been suggested to be better indicators of the immediate SES environment than census tract measures (33). A poverty level category was assigned by dividing the sample into tertiles: low, medium or high without regard to race/ethnicity. The tertile cut-points were 7.5% and 14.1%, meaning that about 1/3 of the sample lived in block groups with a household poverty rate greater than 14.1%. Community poverty is entered in models as indicators for medium, and high household poverty rates, with low as the referent. Residents of a given block group share the same (community) household poverty rate.
Covariates
In this study, covariates included participant socio-demographics (age, race, and gender) as well as health characteristics (body mass index (BMI) and number of comorbid conditions). Age was calculated using the participant's self-reported date of birth and date of telephone survey and used as a continuous measure. Race was self-reported and based on the 2000 US Census race and ethnicity categories and trichotomized into non-Hispanic white (referent), non-Hispanic Black, and Other, where Other includes individuals self-reporting Latino/Hispanic ethnicity or more than one race (American Indian/Alaska Native; Asian; Black or African American; Native Hawaiian or Other Pacific Islander; White; Other). BMI (kg/m2) was calculated from self-reported height and weight, and used as a continuous measure. Existing comorbid conditions were assessed by asking participants if a health professional ever told them they had any of 23 different chronic diseases (e.g. diabetes, heart disease, vision problems). For this paper, number of comorbid conditions is a sum of all self-reported non-arthritis conditions.
Statistical Analysis
Statistical analyses were conducted on 968 participants who self-reported arthritis, after excluding observations missing covariates or main socioeconomic status predictors. Participants with no missing data were not significantly different by demographics or SES (individual and community) variables when compared to people with one or more missing items. However, individuals with missing data tended to report significantly poorer physical health, as they scored 2.3 points lower on PCS, 0.15 points higher on the HAQ, and reported nearly 2 more days of physically unhealthy days, as well as nearly 2 more days of limited activity days. Figure 1 delineates data available for analysis, including the number of observations available for each outcome.
All data were analyzed using STATA version 11.0 (34). Descriptive statistics were computed to describe the sample, and t-tests and chi-squared tests were performed to evaluate statistical differences between non-Hispanic white and non-Hispanic black groups; the 61 participants categorized as ‘other race’ were not included in this examination due to sparse numbers and their being heterogeneous in nature. Correlation analyses examined bivariate associations between individual and community-level SES and physical health status outcomes. Multiple linear regression models, specifically analyses of covariance, were used to examine the associations of the five main SES predictor variables, both separately and together (in block stepwise analyses), with each of the four physical health status outcome measures. All models adjusted for age, gender, BMI, race and comorbid condition count. Since data were collected at 22 family practice sites across North Carolina, we employed the cluster option in STATA regression commands to account for potential intra-site correlation. This option produces Huber-White robust standard errors and provides a more conservative approach to establishing significance of parameter estimates when compared to ordinary linear regressions (35;36).
Because of the known complex relationships between race and socioeconomic status (e.g., non Hispanic blacks more often have lower income and education), we evaluated for effect measure modification in each physical health status outcomes. Race/SES interaction terms were added to each model separately and then combined. Of all the interaction terms tested, only one parameter estimate showed nominal significance (race & medium poverty, p=0.012), and, under multiple testing, the Bonferroni criterion would not support a finding of effect measure modification. Analyses were, therefore, not stratified by race. However, we do present the characteristics of the study sample as a whole group (N=968), and separately by non-Hispanic white (n=731) and non-Hispanic black (n=176).
For all categorical explanatory variables in this study, the referent was set to what is perceived as the most advantageous class (i.e., professional employment, homeowner, household income>$45,000, greater than HS degree, low community poverty). We anticipate that the less advantageous categories will show outcomes changes that indicate poorer health. Depending on the direction of each variable's scale, a deleterious change from the referent may be negative or positive.
Results
Sociodemographic and outcome characteristics of the 968 participants with arthritis are presented in Table 1. The sample was on average 57 (±13) years old, with an average BMI of 30 kg/m2 (±7), and 2 (±2) comorbid conditions. The majority were female (74%), non-Hispanic white (76%), educated (52% beyond HS), with a household income less than $45,000 (66%). About half of the participants (49%) reported non-professional occupations that typically would be physically demanding (e.g., service industries, farming, manufacturing). Homeownership was reported by 78% of the participants.
Table 1. Participant Sociodemographic and Outcome Characteristics*.
| Variables | Mean (SD) or Percent | p-value | ||
|---|---|---|---|---|
| Whole Group (n=968) |
non-Hispanic White (n=731) |
non-Hispanic Black (n=176)‡ |
||
| Age | 56.86 (13.67) | 56.85 (13.78) | 56.30 (13.85) | 0.631 |
| Body Mass Index | 30.57 (7.37) | 29.82 (6.92) | 33.94 (8.27) | <0.001 |
| Co-Morbid Condition Count | 2.11 (1.58) | 2.07 (1.58) | 2.36 (1.58) | 0.029 |
| Female | 73.55 | 71.14 | 84.09 | 0.001 |
| Homeowner | 78.41 | 82.35 | 61.93 | <0.001 |
| Educational attainment | ||||
| >HS | 52.07 | 55.95 | 34.66 | |
| HS | 30.37 | 29.00 | 36.36 | <0.001 |
| <HS | 17.56 | 15.05 | 28.98 | |
| Physically Demanding Occupation | 49.28 | 45.28 | 71.02 | <0.001 |
| Household Income | ||||
| <$15,000 | 25.83 | 18.74 | 53.98 | |
| $15,000-45,000 | 40.60 | 42.41 | 35.23 | <0.001 |
| >$45,000 | 33.57 | 38.85 | 10.80 | |
| Race | ||||
| non-Hispanic white | 75.52 | n/a | n/a | |
| non-Hispanic black | 18.18 | n/a | n/a | |
| Other | 6.30 | n/a | n/a | |
| Community poverty rate | 12.18 (8.59) | 11.28 (7.73) | 15.94 (10.91) | <0.001 |
| Community poverty | ||||
| Low (<7.5%) | 33.47 | 36.25 | 21.02 | |
| Med (7.5-14.1%) | 33.57 | 34.47 | 31.82 | <0.001 |
| High (>14.1%) | 32.95 | 29.27 | 47.16 | |
| Physical Health Status Outcomes† | ||||
| PCS (SF12v2) | 40.74 (12.12) | 41.08 (12.37) | 39.38 (10.99) | 0.099 |
| Unhealthy days- Physical | 8.66 (10.65) | 8.66 (10.86) | 8.59 (9.95) | 0.941 |
| Limited activity days | 9.21 (10.32) | 9.09 (10.53) | 9.87 (9.58) | 0.489 |
| HAQ | 0.67 (0.73) | 0.63 (0.71) | 0.84 (0.82) | <0.001 |
Values are the percentage unless otherwise indicated
Note N varies for outcomes: PCS, N=933; Unhealthy Days - Physical, N=955; Limited Activity Days, N=600; HAQ, N=967.
Other, N=61
For each physical health status outcome assessed, the participants reported a mean PCS score of 40.74 (±12.12) and mean HAQ score of 0.67 (±0.73). On average, they reported an average of 8.6 (±10.65) unhealthy physical days and 9.2 (±10.32) limited activity days per month on the CDC HRQOL healthy days scale.
Also presented in Table 1 are the sociodemographic characteristics stratified by non-Hispanic white (white) and non-Hispanic black (black) racial subgroups, with p-values reported for each test to indicate substantial differences by race. Results show that blacks are more likely than whites to have lower education, to be non-homeowners, to have a non-professional, physically demanding occupation, to have lower household income, and to live in a community with high poverty rate. Blacks had greater disability than their white counterparts as noted with higher HAQ scores. While there were no significant differences by race for PCS, number of physically unhealthy days or number of limited activity days, there was a trend toward lower PCS scores for blacks.
Correlation analyses (not shown) revealed that individual and community SES variables were weakly correlated with each other (ranging from 0.10 to 0.40, p<0.01), and also weakly correlated with the physical health outcomes (ranging from 0.06 to 0.36, p<0.01). Correlation analyses between the physical health outcomes indicates that they are moderately correlated with each other (ranging from 0.55 to 0.73, p<0.001).
We examined the independent effect of each SES variable alone or in concert, on the physical health status outcomes. A staged set of models was developed to allow for in-depth examination, with results of these analyses presented in Tables 2, 3, and 4. Since the referent is conceptualized as the most advantaged class in all cases, the PCS (higher score implies better health) tends to have negative parameter estimates for the SES variables, while the other outcomes (higher scores imply poorer health) tend to have positive estimates.
Table 2. Parameter estimates for each of five SES variables singly with four Physical Health Outcomesa, B (95% Confidence Interval), p-value.
| SES Variable | Outcomes | |||
|---|---|---|---|---|
| SF-12v2 PCS 0-100 |
Physical Unhealthy Days 0-30 |
Limited Activity Days 0-30 |
Disability Status HAQ 0-3 |
|
| 1. Educational Attainment | ||||
| HS degree | -2.72 (-4.13, -1.32) p≤0.001 |
2.18 (0.57, 3.78) p=0.010 |
1.21 (-0.70, 3.13) p=0.202 |
0.08 (-0.01, 0.16) p=0.067 |
| Less than HS | -4.83 (-6.74, -2.92) p≤0.001 |
3.56 (1.83, 5.28) p≤0.001 |
3.51 (0.39, 6.64) p=0.029 |
0.24 (0.08, 0.40) p=0.005 |
| 2. Physically Demanding Occupation | ||||
| -2.19 (-3.44, -0.94) p=0.002 |
1.67 (0.08, 3.26) p=0.041 |
1.84 (-0.07, 3.75) p=0.058 |
0.12 (0.03, 0.22) p=0.010 |
|
| 3. Non-Homeowner | ||||
| -2.74 (-4.18, -1.31) p≤0.001 |
2.01 (0.28, 3.73) p=0.025 |
2.20 (0.28, 4.13) p=0.027 |
0.15 (0.07, 0.23) p≤0.001 |
|
| 4. Household Income | ||||
| $15,000-45,000 | -3.97 (-5.72, -2.22) p≤0.001 |
1.87 (0.65, 3.10) p=0.005 |
3.25 (1.45, 5.06) p≤0.001 |
0.14 (0.02, 0.25) p=0.020 |
| <$15,000 | -8.51 (-10.43, -6.58) p≤0.001 |
5.86 (4.39, 7.33) p≤0.001 |
7.41 (5.38, 9.44) p≤0.001 |
0.48 (0.36, 0.61) p≤0.001 |
| 5. Community Poverty | ||||
| Medium (7.5 - 14.1%) | -0.32 (-2.35, 1.71) p=0.750 |
0.65 (-0.76, 2.06) p=0.347 |
0.68 (-1.19, 2.54) p=0.459 |
0.01 (-0.14, 0.15) p=0.919 |
| High (>14.1%) | -1.20 (-2.89, 0.49) p=0.153 |
1.36 (0.28, 2.43) p=0.016 |
2.10 (-0.27, 4.47) p=0.080 |
0.10 (0.03, 0.17) p=0.008 |
Five separate models are run for each Physical Health Outcome. All models are adjusted for age, gender, BMI, race, comorbid condition count
Table 3. Parameter estimates for single of four individual SES paired with Community SES with four Physical Health Outcomesa, B (95% Confidence Interval), p-value.
| SES Variable | Outcomes | |||
|---|---|---|---|---|
| SF-12v2 PCS 0-100 |
Physical Unhealthy Days 0-30 |
Limited Activity Days 0-30 |
Disability Status HAQ 0-3 |
|
| 1. Educational | ||||
| Attainment | ||||
| HS degree | -2.72 (-4.13, -1.31) p≤0.001 |
2.12 (0.47, 3.77) p=0.014 |
1.11 (-0.85, 3.07) p=0.252 |
0.08 (-0.01, 0.16) p=0.088 |
| Less than HS | -4.89 (-6.79, -2.99) p≤0.001 |
3.53 (1.75, 5.32) p≤0.001 |
3.50 (0.26, 6.73) p=0.036 |
0.25 (0.08, 0.41) p=0.005 |
| Community Poverty | ||||
| Medium (7.5 - 14.1%) | 0.32 (-1.53, 2.17) p=0.721 |
0.21 (-1.13, 1.55) p=0.744 |
0.32 (-1.69, 2.33) p=0.743 |
-0.02 (-0.16, 0.12) p=0.770 |
| High (>14.1%) | -0.86 (-2.40, 0.68) p=0.258 |
1.10 (-0.03, 2.23) p=0.055 |
1.93 (-0.51, 4.38) p=0.115 |
0.08 (0.01, 0.16) p=0.029 |
| 2. Income | ||||
| $15,000-45,000 | -4.04 (-5.80, -2.27) p≤0.001 |
1.84 (0.62, 3.07) p=0.005 |
3.22 (1.44, 5.00) p≤0.001 |
0.14 (0.02, 0.26) p=0.021 |
| <$15000 | -8.56 (-10.52, -6.60) p≤0.001 |
5.78 (4.28, 7.28) p≤0.001 |
7.24 (4.93, 9.55) p≤0.001 |
0.48 (0.34, 0.62) p≤0.001 |
| Community Poverty | ||||
| Medium (7.5 - 14.1%) | 0.63 (-1.29, 2.56) p=0.502 |
0.06 (-1.30, 1.42) p=0.930 |
-0.03 (-1.99, 1.93) p=0.973 |
-0.04 (-0.18, 0.10) p=0.536 |
| High (>14.1%) | 0.05 (-1.48, 1.57) p=0.949 |
0.42 (-0.78, 1.61) p=0.477 |
0.94 (-1.53, 3.40) p=0.439 |
0.02 (-0.05, 0.10) p=0.562 |
| 3. Physically Demanding Occupation | ||||
| -2.17 (-3.42, -0.92) p=0.002 |
1.61 (-0.01, 3.24) p=0.052 |
1.80 (-0.11, 3.72) p=0.064 |
0.12 (0.04, 0.21) p=0.008 |
|
| Community Poverty | ||||
| Medium (7.5 - 14.1%) | -0.03 (-2.04, 1.99) p=0.979 |
0.44 (-1.03, 1.90) p=0.541 |
0.47 (-1.59, 2.53) p=0.640 |
-0.01 (-0.15, 0.13) p=0.905 |
| High (>14.1%) | -1.02 (-2.69, 0.65) p=0.216 |
1.22 (0.17, 2.27) p=0.025 |
1.99 (-0.52, 4.50) p=0.114 |
0.09 (0.02, 0.16) p=0.016 |
| 4. Non-Homeowner | -2.69 (-4.16, -1.22) p≤0.001 |
1.92 (0.16, 3.69) p=0.034 |
2.13 (0.14, 4.12) p=0.037 |
0.15 (0.07, 0.22) p≤0.001 |
| Community Poverty | ||||
| Medium (7.5 - 14.1%) | -0.07 (-2.20, 2.07) p=0.948 |
0.49 (-0.99, 1.96) p=0.499 |
0.40 (-1.59, 2.39) p=0.679 |
-0.01 (-0.15, 0.14) p=0.938 |
| High (>14.1%) | -0.98 (-2.69, 0.72) p=0.245 |
1.22 (0.11, 2.33) p=0.033 |
1.93 (-0.47, 4.33) p=0.110 |
0.09 (0.02, 0.15) p=0.016 |
Four separate models are run for each Physical Health Outcome. All models adjusted for age, gender, BMI, race, comorbid condition count
Table 4. Parameter estimates for all five SES variables cumulatively in blocks arranged according to level of influence, B (95% Confidence Interval), p-value.
| SES Variable | Outcomes | |||
|---|---|---|---|---|
| SF-12v2 PCS 0-100 |
Physical Unhealthy Days 0-30 |
Limited Activity Days 0-30 |
Disability Status HAQ 0-3 |
|
| Block 1 | ||||
| Occupation | -2.03 (-3.29, -0.76) p=0.003 |
1.54 (-0.03, 3.11) p=0.054 |
1.66 (-0.13, 3.46) p=0.068 |
0.12 (0.02, 0.21) p=0.018 |
| Non-Homeowner | -2.55 (-3.95, -1.16) p≤0.001 |
1.85 (0.12, 3.58) p=0.037 |
2.01 (0.17, 3.85) p=0.034 |
0.14 (0.06, 0.22) p=0.002 |
| Block 2 | ||||
| Occupation | -2.03 (-3.29, -0.78) p=0.003 |
1.50 (-0.10, 3.10) p=0.064 |
1.65 (-0.16, 3.46) p=0.072 |
0.12 (0.03, 0.20) p=0.013 |
| Non-Homeowner | -2.53 (-3.96, -1.10) p≤0.001 |
1.79 (0.04, 3.54) p=0.046 |
1.97 (0.05, 3.88) p=0.044 |
0.14 (0.05, 0.22) p=0.003 |
| Community Poverty | ||||
| Medium (7.5 - 14.1%) | 0.19 (-1.93, 2.30) p=0.855 |
0.30 (-1.22, 1.82) p=0.687 |
0.23 (-1.93, 2.39) p=0.824 |
-0.02 (-0.16, 0.12) p=0.784 |
| High (>14.1%) | -0.83 (-2.51, 0.86) p=0.319 |
1.09 (0.02, 2.18) p=0.046 |
1.84 (-0.69, 4.37) p=0.145 |
0.08 (0.01, 0.14) p=0.027 |
| Block 3 | ||||
| Occupation | -0.83 (-2.04, 0.38) p=0.169 |
0.63 (-0.81, 2.06) p=0.374 |
0.99 (-0.43, 2.40) p=0.163 |
0.06 (-0.02, 0.15) p=0.138 |
| Non-Homeowner | -2.25 (-3.84, -0.67) p=0.007 |
1.61 (-0.14, 3.36) p=0.069 |
1.85 (0.17, 3.52) p=0.032 |
0.12 (0.03, 0.22) p=0.014 |
| Community Poverty | ||||
| Medium (7.5 - 14.1%) | 0.56 (-1.39, 2.51) p=0.556 |
0.05 (-1.37, 1.47) p=0.946 |
0.03 (-2.15, 2.21) p=0.976 |
-0.03 (-0.17, 0.11) p=0.624 |
| High (>14.1%) | -0.64 (-2.19, 0.91) p=0.400 |
0.96 (-0.17, 2.08) p=0.092 |
1.75 (-0.77, 4.27) p=0.163 |
0.07 (0.01, 0.14) p=0.048 |
| Education | ||||
| HS | -2.54 (-4.00, -1.09) p=0.002 |
1.98 (0.36, 3.60) p=0.019 |
0.96 (-0.95, 2.87) p=0.306 |
0.06 (-0.03, 0.15) p=0.160 |
| <HS | -4.16 (-6.19, -2.14) p≤0.001 |
3.00 (1.36, 4.64) p≤0.001 |
2.87 (0.09, 5.65) p=0.044 |
0.20 (0.02, 0.37) p=0.027 |
| Block 4 | ||||
| Occupation | 0.15 (-1.05, 1.35) p=0.800 |
0.07 (-1.27, 1.42) p=0.912 |
0.35 (-0.98, 1.67) p=0.592 |
0.01 (-0.06, 0.09) p=0.723 |
| Non-Homeowner | -0.75 (-2.19, 0.69) p=0.290 |
0.58 (-1.30, 2.46) p=0.530 |
0.36 (-1.61, 2.33) p=0.706 |
0.03 (-0.08, 0.14) p=0.585 |
| Community Poverty | ||||
| Medium (7.5 - 14.1%) | 0.87 (-1.02, 2.76) p=0.350 |
-0.12 (-1.50, 1.26) p=0.857 |
-0.17 (-2.24, 1.90) p=0.867 |
-0.05 (-0.18, 0.09) p=0.462 |
| High (>14.1%) | 0.11 (-1.40, 1.62) p=0.880 |
0.38 (-0.85, 1.60) p=0.528 |
0.95 (-1.54, 3.44) p=0.436 |
0.02 (-0.06, 0.10) p=0.568 |
| Education | ||||
| HS | -1.58 (-3.00, -0.15) p=0.031 |
1.42 (-0.22, 3.06) p=0.086 |
0.05 (-2.06, 2.16) p=0.960 |
0.01 (-0.08, 0.10) p=0.814 |
| <HS | -2.19 (-4.41, 0.03) p=0.053 |
1.67 (-0.24, 3.58) p=0.083 |
1.07 (-1.93, 4.06) p=0.467 |
0.08 (-0.12, 0.27) p=0.418 |
| Income | ||||
| $15,000-45,000 | -3.52 (-5.17, -1.86) p≤0.001 |
1.36 (0.09, 2.63) p=0.037 |
3.01 (0.92, 5.11) p=0.007 |
0.13 (-0.01, 0.26) p=0.056 |
| <$15,000 | -7.43 (-9.54, -5.32) p≤0.001 |
4.79 (2.81, 6.78) p≤0.001 |
6.65 (3.71, 9.59) p≤0.001 |
0.44 (0.27, 0.61) p≤0.001 |
All models in Blocks 1-4 are adjusted for age, gender, BMI, race, comorbid condition count
Each of the five individual-level SES variables was entered singly into models for each of the four outcomes, adjusting for age, gender, BMI, race and comorbid condition count. Most of the resulting estimates (Table 2) are significantly different from zero, with most being p<0.01. The effect of education on each of the physical health outcomes is shown in Table 2. People with less than a high school education scored about 4.8 points lower on the PCS compared to those with education beyond high school. They also reported about 3.6 more days per month of poor physical health and 3.5 more days of limited activity related to health. Finally, participants with less than a high school education scored 0.24 higher on the HAQ scale of disability, indicating greater disability.
While the significant role of educational attainment, occupation, and homeownership is observed for all physical health outcomes, household income of <$15,000 has the largest negative effects on PCS and physically unhealthy days outcomes. The role of community poverty is not as strongly associated with worse physical functioning (PCS) as are the individual-level SES markers, however high community poverty is significantly associated with greater number of physically unhealthy days and HAQ disability, with a trend for greater limited activity days.
The relationship between each of the four individual SES measures (education, household income, occupation, and homeownership) and physical health outcomes was then examined in the context of community poverty, adjusting for covariates (Table 3). The first set of models examined educational attainment as the individual level SES measure and community poverty level on physical health outcomes. Individuals with less than a high school degree had significantly poorer scores on all four health status outcomes compared to individuals with greater than a high school degree for physical functioning (β=-4.89, p=≤0.001), physically unhealthy days (β =3.53, p=≤0.001), limited activity days (β =3.50, p=0.036), and HAQ disability (β =0.25, p=0.005). Individuals with a high school degree had significantly poorer PCS and physically unhealthy days, as well as a trend for poorer HAQ score compared to those with greater than a high school degree. In two models, living in the poorest communities (i.e., highest community poverty rate) was associated with poorer health status outcomes independent of education level. The high poverty group had a statistically significant negative impact on HAQ disability scores (β =0.08, p=0.029) and a trend for greater physically unhealthy days (β =1.10, p=0.055). Comparing these results to those in Table 2, we observed a similar educational attainment effect, but a reduced community poverty effect. Educational attainment appears to more strongly explain all physical health outcomes, although both remain significant for HAQ disability.
This dynamic is observed in the occupation and homeownership sets of regression models as well. When compared to the referent groups, having a physically demanding job and not owning a home both were associated with poorer physical health outcomes. As before, when these groups were individually adjusted for community level poverty, poorer HAQ disability scores and greater numbers of physically unhealthy days were seen in the highest level poverty groups. Comparing to results shown in Table 2, we see that the effects of occupation and homeownership seem to remain independent and decrease only slightly.
Most striking are those models including both household income and community poverty (Table 3). The effects for household income approximate those given in Table 2 and remain significant, while the significant effects for community poverty are eliminated. The information provided by community poverty is apparently subsumed by the individual income and no independent association with any physical health outcome remains. When compared to those making more than $45,000, participants earning less than $15,000 had lower PCS scores by 8.56 points (p=≤0.001) and higher HAQ disability scores by nearly half a point (β =0.48, p=≤0.001). Additionally, those with lowest household income had increased number of physically unhealthy days, 5.78 days more per month (p=≤0.001) and increased limited activity days, 7.24 days more per month (p=≤0.001). Lesser, but significant (p<0.01) results were seen for results comparing participants from households earning $15,000-$45,000 to the over $45,000 income group.
Finally, a series of models successively adds SES variables until all five SES variables are in each model (see Table 4). Considering both the relative sizes of parameter estimates and their p-values for each outcome in Tables 2 and 3, the order of the introduction of SES variables has been arranged so the variables that tended to be less influential are entered first (i.e., occupation, homeownership), community poverty next, and then education; the final variable entered is household income.
The Block 1 models have occupation and homeownership entered together and they are independently significant for PCS and HAQ. Community poverty was added in the second set of models (Block 2), and living in the poorest community is associated with greater number of physically unhealthy days (β =1.09, p=0.046) and greater HAQ disability score (β =0.08, p=0.027). Moreover, significant independent effects are maintained in occupation and homeownership. In Block 3, educational status is included in the models. While the effects for less than high school are significant, homeownership and high community poverty also show independent significance for some of the outcomes. However the significant independent effect of occupation is eliminated with the addition of education into this model.
Block 4 adds household income to the other variables to create models that contain all the SES variables. Income is significant at both levels (<$15,000 and $15,000-$45,000) relative to the >$45000 level, while all other SES variables lose significance, with the exception of HS education on PCS, where it remains a significant individual-level SES variable.
Discussion
Previous research has revealed that individual and community-level SES independently influence health outcomes, with lower SES (particularly educational attainment, income, and area-level deprivation) being associated with greater risk of rheumatic conditions (13;14;37-39) and worse health outcomes for people with arthritis (8-11;15;40). In addition, low occupational status was found to be associated with poorer health and chronic disease, including arthritis (41). Yet there remained a need to go beyond these known relationships to better understand to what extent household income influences physical health outcomes given multiple measures of individual-level SES factors (e.g., occupation, homeownership and education).
This study identified the importance of individual SES, particularly household income (at both levels, <$15,000 and $15,000-$45,000) relative to the >$45000 level, while most other SES variables lose significance. One observed exception was educational attainment, where those with less than a HS education had worse physical functioning and education remained a significant individual-level SES variable. It is important to consider that even while small differences in outcomes may be statistically significant if the sample size is large as in our case, this statistical significance may not constitute what an individual with arthritis would report as an important difference in physical health outcome, such as physical functioning or disability. Previous research has proposed that a minimally important difference (MID) that a patient would report is a universal value of effect size (ES)=0.5 (Norman, 2003) but is likely to be dependent on the particular instruments reported and the anchors used to elicit MID responses from patients (Hays, 2005). HAQ changes of about 0.20 have been reported as clinically important (Pope, 2009; Redelmeier, 1993), corresponding to ES=0.27. The PCS (SF-36) MID corresponds to ES=0.49 (Farivar, 2004). Given this, we consider that the parameter estimates may be interpreted as changes in the physical health measures resulting from a treatment consisting of the condition expressed by the SES variable relative to its referent class and we calculated quasi ES (qES) for all outcomes under this paradigm. For example, the PCS parameter estimate for lowest income (<$15,000) is -7.43, meaning that people with low income would have an average PCS that is 7.43 units less than those in the highest income group (greater than $45,000). Using the sample standard deviation of PCS (12.12) from Table 1, a quasi effect size (qES) would be 7.43/12.12 = 0.61. Likewise the qES's for physical unhealthy days, limited activity days, and HAQ are 0.45, 0.64, and 0.60, respectively. Because expert opinion varies widely on what constitutes a meaningful difference and how this should be assessed, qES's are one ad hoc way to capture the magnitude of the effects, standardizing the parameter estimates by corresponding standard deviations. Our findings represent substantial effects judged against other estimates of MID.
Results from this study suggest that while household income does indeed play a dominant role, the other individual-level measures of SES do independently predict physical health measures when examined in their own right. We propose that occupation, homeownership, and educational attainment remain important and good measures to include in further research examining the relationship between SES and arthritis-related outcomes. We believe that perhaps household income not only captures the objective number of dollars available to the individual and household, but also contains elements of occupational status, knowledge and literacy, as well as the availability, level, and extent of resources and social capital contained in the other SES measures. At the very least, study findings suggest that having household income above $45,000 provides an individual with arthritis the financial means to seek out goods and services, either within or outside their community, necessary for better general and arthritis-specific health outcomes.
This study uniquely illustrates both the separate and combined effect of individual and community socioeconomic factors on a variety of physical health outcome measures, including general health outcomes (e.g., SF-12v2 PCS, the CDC HRQOL measures) and an arthritis specific outcome (e.g., HAQ). This study also used four measures of individual-level SES (occupation, homeownership, educational attainment, and household income) which has previously not been found in the arthritis literature to date. Additionally, this study has a moderately large number of participants (N=968), who, as a group, are racially and geographically diverse. Though sampling procedures preclude complete generalizability of results to the general population, we do believe that the racial and geographic diversity increases the generalizability more than would be expected in a homogeneous sample.
Despite these strengths, there are a few limitations worthy of note as with any large telephone survey study. First, this is a cross sectional study which does not allow for examination and determination of a causal pathway of individual and/or community SES influence on physical health outcomes. We caution that poor health may cause individuals to have access to fewer resources and place them in a lower SES condition. Second, this study may have been unintentionally influenced by two sources of bias: reporting bias and recall bias. Potential for reporting bias may come from our attempt to obtain information about household income. While participants are told at the beginning of the study that their participation and all information provided to the research study staff will be kept confidential, many participants of all income levels may remain uncomfortable with income disclosure (42). Reliance upon telephone survey data may introduce some level of participant recall bias. Third, this study did not ask participants to self-report health behaviors (e.g., smoking or level of physical activity), health insurance status or disease duration (i.e., time since arthritis diagnosis). These factors are known to be unequally distributed by SES and could also be influentially associated with physical health among individuals with arthritis. Additionally, we do not have information about how long individuals have lived with arthritis. Finally, the use of aggregate US Census data to proxy community SES can be considered a crude measure of community given that it does not account for contextual community life details (e.g., neighborhood safety and publically available opportunities for physical activity).
In conclusion, our study findings suggest SES measures, particularly household income, play an important role in physical health outcomes among people with arthritis. Our study sheds light into the complex interplay between common markers of SES - occupation, homeownership, education and income, as well as community poverty. Because the national health care agenda places a priority on reducing health disparities caused by inequalities in SES and race, our findings may be of particular interest to clinicians and/or public health practitioners seeking to reduce poorer health outcomes due to these social factors. Furthermore, additional research is needed to examine the influence of individual and community SES over the life course as it relates to general physical health status in people with arthritis.
Acknowledgments
This project was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases Multidisciplinary Clinical Research Center, Rheumatic Diseases: P60-AR49465-01 and manuscript preparation was supported by the Thurston Arthritis Research Center Training Grant 5T32-AR007416.
We thank the following participating family practices in the North Carolina Family Medicine Research Network (NC-FM-RN) for their assistance: Black River Health Services, Burgaw; Bladen Medical Associates, Elizabethtown; Blair Family Medicine, Wallace; Cabarrus Family Medicine, Concord; Cabarrus Family Medicine, Harrisburg; Cabarrus Family Medicine, Kannapolis; Cabarrus Family Medicine, Mt. Pleasant; Chatham Primary Care, Siler City; CMC-Biddle Point, Charlotte; CMC-North Park, Charlotte; Community Family Practice, Asheville; Cornerstone Medical Center, Burlington; Dayspring Family Medicine, Eden; Family Practice of Summerfield, Summerfield; Goldsboro Family Physicians, Goldsboro; Henderson Family Health Center, Henderson; Orange Family Medical Group, Hillsborough; Person Family Medical Center, Roxboro; Pittsboro Family Medicine, Pittsboro; Prospect Hill Community Health Center, Prospect Hill; Robbins Family Practice, Robbins; and Village Family Medicine, Chapel Hill. Finally, we thank the individuals who willingly participated in the study.
Grant Support: This project was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Disease Multidisciplinary Clinical Research Center Rheumatic Diseases: P60-AR49465-01.
Reference List
- 1.Berkman LF, Kawachi I. Social Epidemiology. Oxford: Oxford University Press; 2000. [Google Scholar]
- 2.Evans T, Whitehead M, Diderichsen F, Bhuiya A, Wirth M. Challenging Inequities in Health: From Ethics to Action. Oxford: Oxford University Press; 2001. [Google Scholar]
- 3.Wilkinson RG. Unhealthy Societies: the Afflictions of Inequality. New York: Routledge; 1996. [Google Scholar]
- 4.Callahan LF. Socioeconomic status and rheumatoid arthritis. In: Wolfe F, Pincus T, editors. Rheumatoid Arthritis: Pathogenesis, assessment, outcome, and treatment. New York: Marcel Dekker, Inc.; 1994. pp. 297–316. [Google Scholar]
- 5.Karlson EW, Daltroy LH, Lew RA, Wright EA, Partridge AJ, Roberts WN, et al. The independence and stability of socioeconomic predictors of morbidity in systemic lupus erythematosus. Arthritis Rheum. 1995;38:267–73. doi: 10.1002/art.1780380217. [DOI] [PubMed] [Google Scholar]
- 6.Ward MM. Examining health disparities in systemic lupus erythematosus. Arthritis Rheum. 2001;44(12):2711–4. doi: 10.1002/1529-0131(200112)44:12<2711::aid-art457>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 7.Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 8.Young A, Wilkinson P, Talamo J, Dixey J, Cox N, Davies P, et al. Socioeconomic deprivation and rheumatoid disease: what lessons for the health service? ERAS Study Group. Early Rheumatoid Arthritis Study. Ann Rheum Dis. 2000;59(10):794–9. doi: 10.1136/ard.59.10.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harrison MJ, Tricker KJ, Davies L, Hassell A, Dawes P, Scott DL, et al. The relationship between social deprivation, disease outcome measures, and response to treatment in patients with stable, long-standing rheumatoid arthritis. J Rheumatol. 2005;32(12):2330–6. [PubMed] [Google Scholar]
- 10.Harrison MJ, Farragher TM, Clarke AM, Manning SC, Bunn DK, Symmons DP. Association of functional outcome with both personal- and area-level socioeconomic inequalities in patients with inflammatory polyarthritis. Arthritis Rheum. 2009;61(10):1297–304. doi: 10.1002/art.24830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trupin LS, Tonner MC, Yazdany J, Julian LJ, Criswell LA, Katz PP, et al. The role of neighborhood and individual socioeconomic status in outcomes of systemic lupus erythematosus. J Rheumatol. 2008;35(9):1782–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Brown AF, Ang A, Pebley AR. The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. Am J Public Health. 2007;97(5):926–32. doi: 10.2105/AJPH.2005.069443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canizares M, Power JD, Perruccio AV, Badley EM. Association of regional racial/cultural context and socioeconomic status with arthritis in the population: a multilevel analysis. Arthritis Rheum. 2008;59(3):399–407. doi: 10.1002/art.23316. [DOI] [PubMed] [Google Scholar]
- 14.Callahan LF, Shreffler J, Mielenz T, Schoster B, Kaufman JS, Xiao C, et al. Arthritis in the Family Practice Setting: Associations with Education and Community Poverty. Arthritis Care Res. 2008;59(7):1002–8. doi: 10.1002/art.23834. [DOI] [PubMed] [Google Scholar]
- 15.Callahan LF, Shreffler J, Mielenz T, Kaufman J, Schoster B, Randolph R, et al. Health-Related Quality of Life in Adults from 17 Family Practice Clinics in North Carolina. Preventing Chronic Disease. 2009;6(1) [PMC free article] [PubMed] [Google Scholar]
- 16.Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87–121. doi: 10.1093/oxfordjournals.epirev.a036030. [DOI] [PubMed] [Google Scholar]
- 17.Pincus T, Callahan LF. Associations of low formal education level and poor health status: behavioral, in addition to demographic and medical, explanations? J Clin Epidemiol. 1994;47(4):355–61. doi: 10.1016/0895-4356(94)90156-2. [DOI] [PubMed] [Google Scholar]
- 18.Callahan LF, Cordray DS, Wells G, Pincus T. Formal education and five-year mortality in rheumatoid arthritis: mediation by helplessness scale score. Arthritis Care Res. 1996;9(6):463–72. doi: 10.1002/art.1790090608. [DOI] [PubMed] [Google Scholar]
- 19.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816–20. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pincus T, Callahan LF. Are mind-body variables a central factor linking socioeconomic status and health? (Invited responses to comments of Adler NE, Fries JF, Hurowitz JC, Kaplan GA, Mishra SI, Waitzkin H, Ruberman W, Williams RG, Winkleby M concerning: What explains the association between socioeconomic status and health: Primarily access to medical care of mind-body variables? Advances. 1995;11:4–36. [Google Scholar]; Advances. 1995;11:6–39. [Google Scholar]
- 21.Yen IH, Yelin EH, Katz P, Eisner MD, Blanc PD. Perceived neighborhood problems and quality of life, physical functioning, and depressive symptoms among adults with asthma. Am J Public Health. 2006;96(5):873–9. doi: 10.2105/AJPH.2004.059253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda county study. Am J Epidemiol. 1999;149:898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- 23.Sturm R, Gresenz CR. Relations of income inequality and family income to chronic medical conditions and mental health disorders: national survey. BMJ. 2002;324(7328):20. doi: 10.1136/bmj.324.7328.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sloane PD, Callahan L, Kahwati L, Mitchell CM. Development of a Practice-based Patient Cohort for Primary Care Research. Fam Med. 2006;38(1):50–7. [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; BRFSS Arthritis Questions 1996–2010. [cited 2010 July 27]; URL: http://www.cdc.gov/arthritis/data_statistics/brfss_questions.htm. [Google Scholar]
- 26.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention . Measuring Healthy Days: Population assessment of health-related quality of life. Atlanta: CDC; 2000. [Google Scholar]
- 28.Mielenz T, Jackson E, Currey S, DeVellis R, Callahan LF. Psychometric properties of the Centers for Disease Control and Prevention Health-Related Quality of Life (CDC HRQOL) items in adults with arthritis. Health Qual Life Outcomes. 2006;4:66. doi: 10.1186/1477-7525-4-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23(2):137–45. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 30.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–10. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krieger N. Women and social class: a methodological study comparing individual, household, and census measures as predictors of black/white differences in reproductive history. J Epidemiol Community Health. 1991;45:35–42. doi: 10.1136/jech.45.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bureau of the Census U . Census of Population and Housing, Census 2000 Summary File 3. Washington, DC: Department of Commerce; 2002. [Google Scholar]
- 33.Diez-Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighborhood of residence and incidence of coronary heart disese. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 34.Stata statistical software. College Station, TX: Stata Corporation; 2005. [Google Scholar]
- 35.Williams RL. A Note on Robust Variance Estimation for Cluster-Correlated Data. Biometrics. 2000;56:645–6. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 36.Hubbard AE, Ahern J, Fleischer NL, Laan MVd, Lippman SA, Jewell N, et al. To GEE or Not to GEE: Comparing Population Average and Mixed Models for Estimating the Associations Between Neighborhood Risk Factors and Health. Epidemiology. 2010;21(4):467–74. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- 37.Schneider S, Schmitt G, Richter W. Prevalence and correlates of inflammatory arthritis in Germany: data from the First National Health Survey. Rheumatol Int. 2006;27(1):29–38. doi: 10.1007/s00296-006-0153-0. [DOI] [PubMed] [Google Scholar]
- 38.Bengtsson C, Nordmark B, Klareskog L, Lundberg I, Alfredsson L. Socioeconomic status and the risk of developing rheumatoid arthritis: results from the Swedish EIRA study. Ann Rheum Dis. 2005;64(11):1588–94. doi: 10.1136/ard.2004.031666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pedersen M, Jacobsen S, Klarlund M, Frisch M. Socioeconomic status and risk of rheumatoid arthritis: a Danish case-control study. J Rheumatol. 2006;33(6):1069–74. [PubMed] [Google Scholar]
- 40.Jordan KP, Thomas E, Peat G, Wilkie R, Croft P. Social risks for disabling pain in older people: a prospective study of individual and area characteristics. Pain. 2008;137(3):652–61. doi: 10.1016/j.pain.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 41.Volkers AC, Westert GP, Schellevis FG. Health disparities by occupation, modified by education: a cross-sectional population study. BMC Public Health. 2007;7:196. doi: 10.1186/1471-2458-7-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Turrell G. Income non-reporting: implications for health inequalities research. J Epidemiol Community Health. 2000;54:207–14. doi: 10.1136/jech.54.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]