Abstract
There is a need to make medical diagnosis available to critically ill patients on-site, without the necessity of time-consuming and risky transportation to larger reference hospitals. The teleconsultation of medical images is possible with the use of Internet-based TeleDICOM software developed in Krakow, Poland. Interactive consultation between two or more centers offers real-time voice communication, visualization of synchronized Digital Imaging and Communications in Medicine images, and use of interactive pointers and specific calculation tools. If direct interaction between physicians is not needed, the system can also be used in “offline” mode. In 2006, TeleDICOM was successfully deployed in the John Paul II Hospital in Krakow as well as a dozen other cooperating medical centers throughout southeast Poland. It is used for routine referral for cardiosurgical procedures. Aims of the study were to evaluate the image quality, software stability, constant availability, data transmission speed, and quality of real-time synchronized viewing of the images during the TeleDICOM teleconsultation; to evaluate the clinical utility of the TeleDICOM system; and to analyze the compatibility of TeleDICOM with the storage data formats of various imaging machine manufacturers. The analysis of angiographic offline teleconsultations was based on 918 patients referred remotely for coronary artery bypass grafting (CABG). The echocardiographic teleconsultations were performed during 63 live interactive consultations, several of them were presented to live during medical conferences. Measurement tools of the TeleDICOM software were tested against original measurement tools of echocardiographic machines from four different manufacturers. As a result of TeleDICOM consultation, a CABG decision was made in 806 of 918 patients consulted (87.8%). In remaining 12 patients, medical therapy or percutaneous angioplasty was recommended. CABG was performed in 98.6% of the admitted patients. Treatment decisions were changed after admission in 1.4% of patients—however, in all cases, it was not related to analysis of angiography data but rather to the change of clinical condition of the patients. All medical personnel involved in both offline and interactive teleconsultations judged the system positively in all assessed aspects. Lesser scores were observed only in the centers connected by slower networks. Measurements performed in the ECHO-TeleDICOM module were accurate as compared with those performed on a standard echo-machine (correlation r > 0.980, p < 0.001), independently of the echocardiograph model. Conclusion: This study demonstrates that telemedicine can improve patients' management using a clinically effective teleconsultation system. The TeleDICOM system is suited for professional use in the field of cardiovascular disease. It is also prepared for remote live demonstrations of clinical cases during large medical meetings.
Key words: Telemedicine, angiography, cardiac imaging, clinical application, computers in medicine, digital image management, image analysis, ultrasonography
Introduction
Expert consultation has been a key element of medical knowledge development and decision making for ages. In modern times, consultation is frequently needed for interpretation of diagnostic images. This is particularly important when dealing with rare diseases (e.g., congenital anomalies) or complex multidisciplinary conditions that require special management. The Internet has become one of the most important communication tools, and its role in different fields of medicine is increasing.1–49
The Digital Imaging and Communications in Medicine (DICOM) is the international standard for distribution and presentation of medical images acquired from various diagnostic machines. DICOM is widely used in hospitals and is becoming more and more available to smaller medical institutions. There is a need to make diagnostic and therapeutic interventions available to critically ill patients on-site, without the necessity of time-consuming and risky transportation to larger reference hospitals. Nowadays, many small cardiology units perform cardiac catheterization procedures or echocardiographic examinations far from the reference cardiosurgery centers. Experienced cardiologists can solve most of the problems of hospitalized patients locally. In particular cases, however, consultation with a cardiosurgeon is mandatory for optimal decision making. This includes referral for urgent or elective cardiosurgical procedures rather than performing locally high risk or nonoptimal endovascular interventions, dealing with complications requiring surgical backup, etc. The availability of teleconsultation can help to make adequate decisions, which can decrease the time to intervention or avoid unnecessary transportation of inoperable patients. Teleconsultation of medical cases should resemble the face-to-face conversation between physicians looking at the same images, showing each other the important aspects of the examination. Additionally, a group of doctors should be able to participate in the consultation session instead of merely two. Performing detailed measurements of calibrated images should be available to all participants of teleconsultation (Table 1).
Table 1.
The Theoretical Requirements of Optimal Teleconsultation System
| • Sending and receiving of high-resolution DICOM images, from all available medical imaging modalities |
| • Fast, real-time synchronized view of DICOM images and clips in 2 or more teleconsultation centers, avoiding delays during image loading |
| • Live voice interaction of all participants |
| • Availability of mouse-controlled pointers for real-time indication of a region of interest to other teleconsultation partners |
| • Integrated fully automatic calibration of the diagnostic images, measurement tools and calculations for all available imagistic modalities |
| • Secure and authorized access to medical data |
| • Compatibility with standard computers and networks |
| • Intuitive and easy to operate software |
| • 24-h availability and stability of the system |
| • Low cost |
Specialized teleconsultation software has been designed and implemented at the Department of Computer Science of AGH University of Science and Technology in Krakow, Poland. Various telemedical applications have been developed at the department since 2001. TeleDICOM has benefited from the experience gained at AGH and has been designed to meet the requirements listed in Table 1.
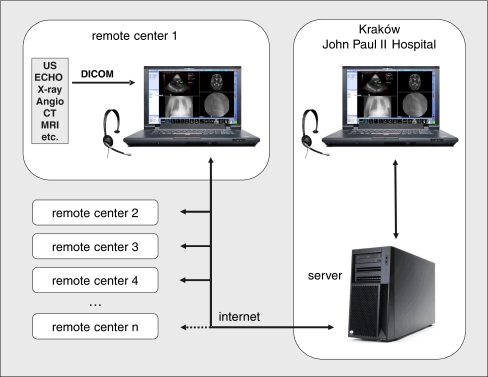
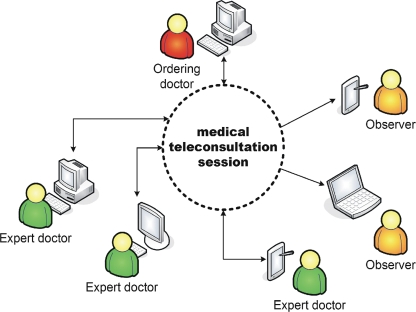
TeleDICOM was implemented using the so-called thick-client architecture. Communication between the noninteractive client and the server is rather simple—the client merely downloads the consultation data and uploads the diagnoses using the data channel. The interactive mode uses three additional channels: voice, session synchronization, and chat. Each channel is a point-to-point link between the client application and a TeleDICOM server (Fig. 1). During the interactive session, when many clients are linked to it concurrently, the architecture transforms to the star topology, as presented in Figure 2. This architecture fits the structure of the contemporary Internet very well, accommodating many private and/or firewalled networks. One of the requirements of TeleDICOM was its efficient operation over public, even low-bandwidth links.
Fig 1.
Structure of the TeleDICOM system used for teleconsultations between John Paul II Hospital and local hospitals throughout southern Poland.
Fig 2.
The logical view multiuser TeleDICOM session.
Each of the communication channels requires a different approach. To be able to handle network errors, data sent via a data channel are fragmented into chunks and reassembled on the both link ends. Therefore, the transfer can be stopped or even aborted at any time, and the application is able to transparently reconnect and resume the transmission later. The channel is cryptographically protected to prevent outside interception or modification of data. To efficiently convey voice data, we used a standard approach based on the H.323 protocol umbrella with RTP/UDP/IP encapsulation. This guarantees optimal voice communication over WAN networks. The voices of the participants of the consultation are mixed and redistributed using an H.323 MCU component. Taking into account the diversity of the clients' link throughputs, each user can select a voice codec best suited to its network link (e.g., G.711 is very fast but needs as much as 64 kpb; iLBC is very CPU-intensive but requires only 15 kbps). The session synchronization and chat channels have been implemented using their own raw-socket protocol for optimal interactivity. Access to the system is restricted and requires a valid account configured by the system administrator. On the server side, image data are stored on the RAID disk (regularly backed up), and the consultation metadata is stored in the database.
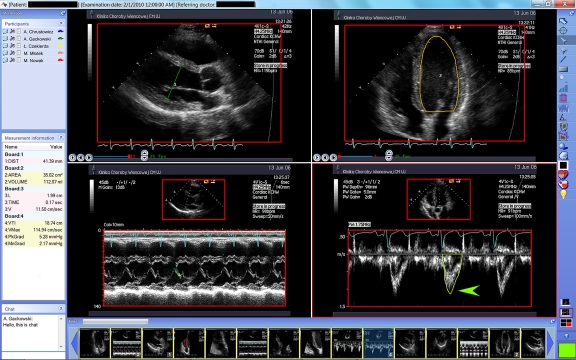
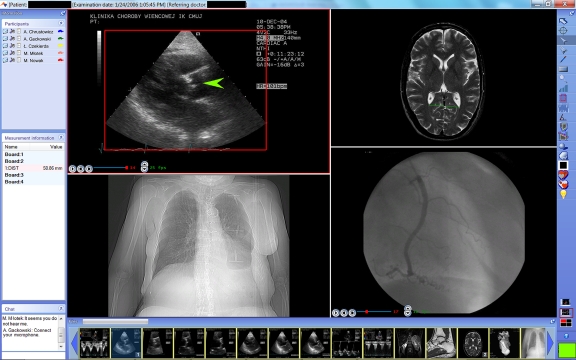
The program can be used for interactive consultation between two or more centers, allowing for real-time voice communication, visualization of synchronized DICOM images, and use of interactive pointers and specific calculation tools (Figs. 3 and 4). If direct interaction between physicians is not needed, the system can also be used in “offline” mode. In such a case, the requested teleconsultation can be done by the consultant on the basis of medical documentation and DICOM images, and the reply can be sent to an ordering physician at a later time. One of the important challenges was to obtain instantaneous synchronization of the high-quality DICOM images and cine-loops on the remote computers. As DICOM files are relatively big, the time-consuming Internet transfer would cause significant delays making the interaction of consulting physicians difficult. To overcome this limitation, the DICOM datasets are transmitted to a central server from which they are automatically downloaded to the workstation in the reference center before the consultation begins. During the teleconsultation, the Internet communication is used only for synchronization of the images, voice communication, and sharing pointers and calculation tools. Therefore, during teleconsultation, the data flow between participating centers is minimized and does not cause significant delays in synchronization of the displayed images. Time spent by teleconsulting physicians is optimized even if the Internet network is relatively slow. The TeleDICOM system is compatible with all DICOM modalities, but we tested it extensively in the clinical areas of angiography and echocardiography.
Fig 3.
Sample teleconsultation screen. Left upper panel: the names of teleconference participants. Right bar: visual and measurement tools. Central panel: echocardiographic images displayed in quad-screen format (single screen format is also available). Upper images are in this case 2D video clips (start, stop, and frame rate controls are visible). Lower images show M-mode and spectral Doppler images. Red rectangles represent automatically calibrated sectors of DICOM images. Physicians can show selected aspects of the study by color arrows and are able to make freehand drawings. All types of echocardiographic measurements can be performed with the results displayed in the left panel. Left lower panel is a chat window. Lower panel shows thumbnails of the available images that can be placed in the main panel.
Fig 4.
Sample multimodality teleconsultation screen showing echocardiographic, computed tomography, x-ray, and angiography images. Size of each window can be adjusted. See Figure 3 legend for explanation of side bars and panels.
In 2006, TeleDICOM was successfully deployed in everyday medical practice at the Department of Cardiovascular Surgery and Transplantology of the John Paul II Hospital in Krakow as well as a dozen other cooperating medical centers throughout southeast Poland. It is used for routine referral for coronary artery bypass grafting (CABG). Simultaneously, a number of advanced tools for echocardiography measurement have been implemented (ECHO-TeleDICOM version of the application). The TeleDICOM server storing the data and mediating in the communication has been installed at John Paul II Hospital in Krakow.
The aims of the study are the following:
To evaluate the image quality, software stability, constant availability, data transmission speed, and quality of real-time synchronized viewing of the images during the TeleDICOM teleconsultation
To compare the results of remote patient consultation versus those of on-site “classic” evaluations once the patient has arrived at the reference center
To evaluate the clinical utility of the TeleDICOM system
To analyze the compatibility of TeleDICOM with the storage data formats of various imaging machine manufacturers
To compare results of the measurements performed by ECHO-TeleDICOM software (two-dimensional [2D], M-mode, Doppler) with those performed during echocardiographic examinations using the built-in measurement tools in the echocardiographic machine
Methods
The main analysis was based on all patients referred by seven cooperating hospitals in southern Poland to CABG via teleconsultation during the period of January 1, 2008 to March 31, 2009. The study group consisted of 918 referred patients (44% women; mean age, 66.2 years; range, 34–87 years). The teleconsultation was elective in 905 of the patients, while 13 patients required urgent attention. DICOM angiographic data were recorded using either the Philips Integris or the Siemens Axiom Artis angiography systems. Travel distance between hospitals and the reference center ranged from 83 to 242 km.
Angiographic teleconsultations were performed in the “offline” mode: patient data and proposals/questions regarding patient management were sent to the reference center via fax. The technician in the referring center transferred the complete angiographic DICOM data from the angiography system (using a CD-ROM) to a standard, Internet-connected PC computer and then loaded into the TeleDICOM system. Based on the patient data and the visualized angiography, the cardiac surgeon in the reference center decided on the optimal management of the patient: CABG, percutaneous coronary intervention (PCI), or conservative treatment. In patients remotely qualified to CABG, the teleconsultation decision was reviewed after admission to the reference center by reviewing their angiography recorded on CD-ROM and once again analyzing the current clinical information. Using the data from the TeleDICOM central server, transmission time of the DICOM datasets to the reference center, errors related to data transmission, and time the that network or server was unavailable were analyzed. The number of program malfunctions reported to the system administrator was also analyzed.
Image quality, software speed, and stability during the consultation were analyzed by cardiac surgeons in the reference center. Software stability, availability, transmission time, and user satisfaction were also analyzed by technicians and physicians from each of the reference centers.
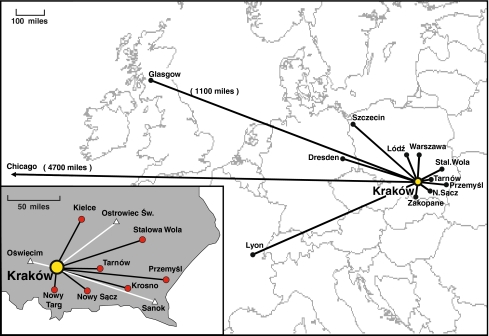
The echocardiographic teleconsultations were performed in the years 2006 to 2010 during 63 live interactive consultations using the ECHO-TeleDICOM system: 4 in the local hospital network of John Paul II Hospital, 17 between John Paul II Hospital and the AGH Department of Computer Science, and 42 teleconsultations (2–7 for individual centers) between John Paul II Hospital and cardiology departments in Krakow, Nowy Sacz, Tarnow, Lodz, Warsaw, Szczecin, Stalowa Wola, Zakopane (Poland), Dresden (Germany), Lyon (France), Chicago (USA), and Glasgow (United Kingdom). Five simultaneous connections between four centers and two simultaneous connections between 13 physicians were realized. The maximum distance between teleconsultation centers was 7,600 km (Krakow-Chicago; Fig. 5).
Fig 5.
Map showing teleconsultations performed with the use of TeleDICOM system. Echocardiography teleconsultations are shown on a map of Europe. Southern Poland angiography teleconsultation network is shown in the inset (black lines with circles represent the connections analyzed in the paper, white lines with the triangles show new connections established recently).
All physicians involved in echocardiography teleconsultations were asked to score quality of images, interactive pointers, and voice transmission as well as assess the system usefulness in clinical practice. Seven echo-teleconsultations were performed during Echocardiography Workshops in Krakow in front of audiences each consisting of more than 200 physicians. The doctors could view and hear the teleconsultation and direct questions to the remote consultant. In 3 of the workshops, 723 questionnaires assessing the quality of this presentation were obtained from participating physicians and subsequently analyzed. Ethics committee approval was obtained before beginning research involving human subjects or clinical information.
To test the measurement tools of the ECHO-TeleDICOM module, DICOM images recorded on the following standard echo-machines were analyzed: SEQUOIA C512 (Siemens Accuson, Malvern, PA, USA), VIVID-7 (GE Vingmed, Pittsburgh, PA, USA), Aplio (Toshiba, Tustin, CA, USA), and SONOS 7500 (Philips, Andover, MA, USA). At least 10 different measurements and calculations were performed in each imaging modality; distance, area, and volume using the Simpson method were recorded in 2D imaging; distance, time, and slope for M-mode; maximal and mean gradient and speed as well as time, velocity time integral, pressure half time, and mitral valve area for both continuous and pulse-wave Doppler. At least 110 measurements were performed on each echocardiograph; recorded datasets were transferred using CD-ROM to computer and sent to ECHO-TeleDICOM. All measurements were repeated using ECHO-TeleDICOM measurement tools. Measurements performed on the echo-machines with the data obtained using ECHO-TeleDICOM measurement tools were then compared, and a correlation coefficient was calculated. Statistica software (Statistica ver. 8, Statsoft, Polska) was used for statistical analysis.
Results
The first installation of TeleDICOM software took 2 to 3 h depending on hospital network configuration. Usually, local network firewall settings had to be adjusted in cooperation with the local system administrator. The average learning time for software use by medical personnel was about 10 min.
Mean angiography datasets volume was 159.3 ± 49.3 MB, and the average number of clips per teleconsultation was 9.3. Mean transmission time before teleconsultation was related to referential hospital network capacity and was 7.2 ± 6.8 min at a mean network speed of 6,875 ± 1,225 kb/s and 58.7 ± 25.2 min at mean network speed of 248.4 ± 56.9 kb/s (Table 2). Mean dataset volume of echocardiographic study was 56.0 ± 17.1 MB, and transmission time ranged from 5 to 45 min depending on network speed. All DICOM data from angiography systems and echocardiographs were adequately received and instantaneously available during teleconsultation. There were no malfunctions of the central server reported over the 15 months of study time; however, there was one severe physical network failure lasting approximately 24 h that prohibited John Paul II Hospital from connecting to the Internet.
Table 2.
Transmission Time and Network Speed of the Referential Centers Connections
| Remote center | Teleconsultation number | Network speed (kB/s) | Mean transmission time (min) |
|---|---|---|---|
| Tarnow | 431 | 685.0 ± 381.0 | 29.5 ± 36.0 |
| Przemysl | 79 | 710.2. ± 70.0 | 13 ± 6.6 |
| Nowy Sacz | 141 | 548.7 ± 190.5 | 36.6 ± 10.0 |
| Stalowa Wola | 7 | 451.5 ± 73.0 | 54.1 ± 38.0 |
| Nowy Targ | 61 | 265.3 ± 12.5 | 55.5 ± 36.3 |
| Krosno | 75 | 248.4 ± 56.9 | 58.7 ± 25.2 |
| Kielce | 124 | 6,875.4 ± 1,225.7 | 7.2 ± 6.8 |
| Overall | 918 | 1,397.79 ± 1,709.2 | 37.8 ± 38.7 |
As a result of TeleDICOM consultation, a CABG decision was made in 806 of 918 patients consulted (87.8%). Medical therapy was recommended in 58 cases (6.3%) and 49 patients (5.3%) underwent percutaneous coronary angioplasty at the remote medical center, while 5 patients (0.5%) were admitted to the reference center for left main evaluation by intravascular ultrasound or percutaneous coronary angioplasty requiring on-site cardiac surgery backup. Out of 806 patients qualified for CABG, 770 patients (95.5%) arrived at the department of cardiovascular surgery, while 36 patients (4.5%) did not accept the surgical treatment. CABG was performed in 759 (98.6%) of the admitted patients. Treatment decisions were changed after admission in 11 of 806 patients (1.4%); however, in all cases, it was not related to analysis of angiography data but rather to the clinical condition of the patients or to additional diagnostic test results. In case of urgent teleconsultations, the cardiosurgeon on duty was called at the necessary moment and data transfer ensued immediately. The result of these 13 urgent teleconsultations was received in the referring center 20 to 60 min (41 ± 16 min) after each consultation was ordered. The 905 elective teleconsultations were done each workday morning by consulting cardiosurgeon and cardiologist. The orders sent from the peripheral hospitals during previous 24 h (72 h during weekends) were ready for review by local computers. After the meeting, elective teleconsultation results were sent back to the referring center by 9:00am. Thus, the time that passed between ordering and receiving the results of elective teleconsultation depended not on the TeleDICOM system but on the consultant’s schedules.
All medical personnel involved in teleconsultations judged the system positively in all assessed aspects. The results of this evaluation are presented in Tables 3, 4, and 5. Lesser scores were observed only in the centers connected by slower networks.
Table 3.
Cardiac Surgeons' Opinions on Angiography Teleconsultation Module Based on 918 Teleconsulations
| Surgeon 1 | Surgeon 2 | Surgeon 3 | Mean | |
|---|---|---|---|---|
| Clip loading | 5 | 5 | 5 | 5.0 |
| Clip displaying | 5 | 5 | 5 | 5.0 |
| Image resolution | 5 | 5 | 5 | 5.0 |
| Image contrast | 5 | 5 | 5 | 5.0 |
| System stability | 5 | 4 | 5 | 4.67 |
| Clinical utility | 5 | 5 | 5 | 5.0 |
| Feasibility | 5 | 5 | 5 | 5.0 |
| Mean | 5.0 | 4.86 | 5.0 | 4.95 |
Scoring scale: 1—very poor, 2—poor, 3—fair, 4—good, and 5—excellent. Values in the table are mean (range)
Table 4.
Technicians’ Opinions of the Angiography Teleconsultation Module Based on 918 Teleconsultations
| Tarnow | Przemysl | Nowy Sacz | Stalowa Wola | Nowy Targ | Krosno | Kielce | Overall | |
|---|---|---|---|---|---|---|---|---|
| DICOM file uploading | 5 | 5 | 5 | 5 | 5 | 4 | 5 | 4.86 |
| System stability | 5 | 5 | 5 | 5 | 5 | 4 | 5 | 4.86 |
| Transmission speed | 4 | 5 | 4 | 4 | 4 | 3 | 5 | 4.14 |
| Clinical utility | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5.00 |
| Overall | 4.75 | 5 | 4.75 | 4.75 | 4.75 | 4 | 5 | 4.71 |
Scoring scale: 1—very poor, 2—poor, 3—fair, 4—good, and 5—excellent
Table 5.
Results of Questionnaire Filled by Physicians Evaluating ECHO-TeleDICOM System
| Physicians performing teleconsultation (n = 21) | Physicians observing teleconsultation (n = 723) | |
|---|---|---|
| Image quality | 4.9 (4–5) | 4.7 (4–5) |
| Clip loading speed | 4.8 (4–5) | 4.6 (4–5) |
| Clip displaying | 4.9 (4–5) | 4.7 (4–5) |
| Interactive pointers | 4.9 (4–5) | 4.9 (4–5) |
| Voice quality | 3.9 (2–5) | 3.9 (3–5) |
| Mean | 4.68 | 4.56 |
| Clinical usefulness | 4.5 (4–5) | 4.5 (4–5) |
| Educational usefulness | 4.4 (4–5) | 4.4 (4–5) |
| Mean | 4.45 | 4.45 |
Scoring scale: 1—very poor, 2—poor, 3—fair, 4—good, and 5—very good. Values in the table are mean (range)
Measurements performed in the ECHO-TeleDICOM module were accurate as compared with those performed on a standard echo-machine (correlation r > 0.980, p < 0.001), independently of the echocardiograph model (Table 6).
Table 6.
Correlation Coefficients (r Value) of Measurements Performed on Standard Echocardiographs Compared With Those Performed With Echo-TeleDICOM
| Type of echo-machine | 2D | M-Mode | Doppler | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Distance | Left ventricular volume | Area | Distance | Time | Slope | Velocity | VTI | Pressure half-time | Time | |
| Toshiba Aplio | 1.000 | 0.999 | 0.999 | 0.996 | 0.946 | 1.000 | 0.987 | 0.999 | 0.991 | 0.999 |
| Philips Sonos 7500 | 1.000 | 0.999 | 0.999 | 0.999 | 1.000 | 1.000 | 0.998 | 0.999 | 0.979 | 0.999 |
| Siemens Sequoia C512 | 1.000 | 1.000 | 0.999 | 1.000 | 0.985 | 1.000 | 0.978 | 0.979 | 0.978 | 0.999 |
| GE Vivid 7 | 1.000 | 0.999 | 0.993 | 1.000 | 0.995 | 1.000 | 0.974 | 0.994 | 0.999 | 0.999 |
p value for all measurements was highly significant (p < 0.001)
VTI velocity time integral
Discussion
The presented teleconsultation system is composed of a DICOM viewer and the Internet-based platform allowing for fully interactive, real-time teleconsultation, thus bringing together geographically distant physicians. The software also includes accurate measurements and calculations tools for standard echocardiographic examinations.
Transmission time is related to data volume and network parameters. Due to the fact that the program allows data transmission before consultation, network speed is not essential for elective consultations; however, a high-speed network is required for emergency consultations. The real-life connection speed was relatively low in several remote centers; this illustrates the difficulties that can be experienced when implementing telemedicine systems in countries with a relatively poor Internet infrastructure (like in central and eastern Europe). Nevertheless, this problem did not cause difficulties in TeleDICOM system performance (the interactive mode requires at least 100 kb/s, but the noninteractive mode has no minimum threshold). Anyway, this problem will soon be resolved as Internet systems consistently evolve.
At the time the system was developed and tested, the only way to load the DICOM data to the system was to a copy a CD-ROM previously burned by the angiographic or echocardiographic systems. The source DICOM machines were not equipped with network connectivity—this option required additional costs, which were not justifiable to many hospitals in Poland (as no network infrastructure existed at that time). Today’s systems allow data transfer without the use of CD media.
DICOM image quality and program stability help to enable therapeutic decisions. The software is intuitive, is easy to install, and can be used without significant costs. It can optimize a patient’s management without the need to transport the patient for consultation at the reference center. The system is also able to display current and old images of all DICOM modalities from the same patient, increasing the amount of data available to physicians.
During the testing phase, signed documents containing clinical data had to be transmitted between hospitals via fax due to legal restrictions. The TeleDICOM system provides the option of uploading and transferring clinical data so paper documents are technically not necessary.
Positive opinions from physicians who have used the system support the thesis that teleconsultation in cardiology has unlimited potential. The number of TeleDICOM teleconsultations is increasing; by the end of 2009, over 1,500 referral cases had been consulted in this fashion. Moreover, many new medical centers have joined the network since our survey was taken (Fig. 5). In addition, the system allows the sharing of medical experience not only between individuals but also on a collective basis (e.g., large medical conferences). Interactive remote case analysis was successfully presented many times to audiences consisting of several hundred physicians. The system is being improved by further optimizing the graphic interface and adding reporting tools.
Conclusion
This study demonstrates that telemedicine can improve patients’ management using a clinically effective teleconsultation system. The TeleDICOM system is suited for professional use in the field of cardiovascular disease. It is also prepared for remote live demonstrations of clinical cases during large medical meetings.
Acknowledgement
Members of the TeleDICOM multicenter validation group:
Jarosław D. Kasprzak (II Department of Cardiology, University of Medicine, Lodz, Poland), Dariusz Dudek (II Department of Cardiology, Jagiellonian University, Krakow, Poland), Tomasz Masternak (Department of Computer Science, AGH University of Science and Technology, Krakow, Poland), Marcin Młotek (Service de Rythmologie, Hôpital Louis Pradel, Lyon, France), Piotr Sonecki (Western Infirmary, Glasgow, United Kingdom), Marek Konka (Department of Congenital Heart Disease, Institute of Cardiology, Warsaw, Poland), Piotr Szymański (Department of Congenital Heart Disease, Institute of Cardiology, Warsaw, Poland), Krzysztof Mokrzycki (Department of Cardiac Surgery, Pomeranian Medical University, Szczecin, Poland), Maciej Żabówka (Kardiomed Medical Center, Tarnów, Poland), Bogdan Kapelak (Department of Cardiovascular Surgery and Transplantology, Institute of Cardiology, Jagiellonian University, Krakow, Poland; John Paul II Hospital, Krakow, Poland), Jerzy Samitowski (Department of Cardiovascular Surgery and Transplantology, Institute of Cardiology, Jagiellonian University, Krakow, Poland; John Paul II Hospital, Krakow, Poland), Roman Pfitzner (Department of Cardiovascular Surgery and Transplantology, Institute of Cardiology, Jagiellonian University, Krakow, Poland; John Paul II Hospital, Krakow, Poland), Roman Rogóż (John Paul II Hospital, Krakow, Poland), Bogdan Januś (Hemodynamics Department, Szczeklik Hospital, Tarnow, Poland), Mariusz Kędzierski (Hemodynamics Department, District Hospital, Przemyśl, Poland), Marcin Dołemski (Hemodynamics Department, District Hospital, Przemyśl, Poland), Jacek Dragan (Department of Invasive Cardiology, Electrotherapy and Angiology, Nowy Scz, Poland), Wojciech Dobrowolski (Department of Invasive Cardiology, Electrotherapy and Angiology, Nowy Scz, Poland), Marek Ujda (Department of Cardiology, Specialist Hospital, Stalowa Wola, Poland), Jacek Legutko (Department of Invasive Cardiology, Electrotherapy and Angiology, Nowy Targ, Poland), Janusz Szczupak (Department of Invasive Cardiology, Electrotherapy and Angiology, Krosno, Poland), Wojciech Gutkowski (Hemodynamics Department, Cardiology Center, Kielce, Poland), Jacek Kołcz (Department of Pediatric Cardiosugery, Polish-American Pediatric Institute, Krakow, Poland), Wiktoria Wojciechowska (Ist Department of Cardiology and Arterial Hypertension, Krakow, Poland), Adam Koprowski (IT Department, Institute of Cardiology, Warsaw, Poland)
References
- 1.Arnold CW, Bui AA, Morioka C, El-Saden S, Kangarloo H. Informatics in radiology: a prototype Web-based reporting system for onsite-offsite clinician communication. Radiographics. 2007;27(4):1201–1211. doi: 10.1148/rg.274065124. [DOI] [PubMed] [Google Scholar]
- 2.Audebert HJ, Boy S, Jankovits R, Pilz P, Klucken J, Fehm NP, Schenkel J. Is mobile teleconsulting equivalent to hospital-based telestroke services? Stroke. 2008;39(12):3427–3430. doi: 10.1161/STROKEAHA.108.520478. [DOI] [PubMed] [Google Scholar]
- 3.Balasingham I, Ihlen H, Leister W, Røe P, Samset E. Communication of medical images, text, and messages in inter-enterprise systems: a case study in Norway. IEEE Trans Inf Technol Biomed. 2007;11(1):7–13. doi: 10.1109/TITB.2006.879597. [DOI] [PubMed] [Google Scholar]
- 4.Banitsas KA, Georgiadis P, Tachakra S, Cavouras D. Using handheld devices for real-time wireless teleconsultation. Conf Proc IEEE Eng Med Biol Soc. 2004;4:3105–3108. doi: 10.1109/IEMBS.2004.1403877. [DOI] [PubMed] [Google Scholar]
- 5.Barry N, Campbell P, Reed N, Reid ME, Bower DJ, Norrie J, Currie GD. Implementation of videoconferencing to support a managed clinical network in Scotland: lessons learned during the first 18 months. J Telemed Telecare. 2003;9(Suppl 2):S7–S9. doi: 10.1258/135763303322596110. [DOI] [PubMed] [Google Scholar]
- 6.Bergh B, Schlaefke A, Pietsch M, García I, Vogl TJ. Evaluation of a "no-cost" Internet technology-based system for teleradiology and co-operative work. Eur Radiol. 2003;13(2):425–434. doi: 10.1007/s00330-002-1488-x. [DOI] [PubMed] [Google Scholar]
- 7.Boman K, Olofsson M, Forsberg J, Boström SA. Remote-controlled robotic arm for real-time echocardiography: the diagnostic future for patients in rural areas? Telemed J E Health. 2009;15(2):142–147. doi: 10.1089/tmj.2008.0079. [DOI] [PubMed] [Google Scholar]
- 8.Bonvini RF, Caoduro L, Menafoglio A, Calanca L, Segesser L, Gallino A. Telemedicine for cardiac surgery candidates. Eur J Cardiothorac Surg. 2002;22(3):377–380. doi: 10.1016/S1010-7940(02)00364-0. [DOI] [PubMed] [Google Scholar]
- 9.Cała J, Czekierda Ł, Gackowski A, Zieliński K: Współczesne systemy telekonsultacyjne w diagnostyce medycznej. W: Technologie informacyjne w medycynie. Pod red. Zygmunta Wróbla. Wydawnictwo Uniwersytetu Ślskiego, Katowice 2008
- 10.Cała J, Czekierda Ł, Nowak M, Zieliński K: The practical experiences with deployment of advanced medical teleconsultation system over public IT infrastructure. Proceedings of the 21st IEEE International Symposium on Computer-Based Medical Systems, University of Jyväskylä, Finland, 2008.
- 11.Carey LS. Teleradiology: part of a comprehensive telehealth system. Radiol Clin North Am. 1985;23(2):357–362. [PubMed] [Google Scholar]
- 12.Carrino JA, Unkel PJ, Miller ID, Bowser CL, Freckleton MW, Johnson TG. Large-scale PACS implementation. J Digit Imaging. 1998;11(3 Suppl 1):3–7. doi: 10.1007/BF03168246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casey F, Brown D, Corrigan N, Craig BG, Quinn M, McCord B, Rogers J, Mulholland HC. Value of a low-cost telemedicine link in the remote echocardiographic diagnosis of congenital heart defects. J Telemed Telecare. 1998;4(Suppl 1):46–48. doi: 10.1258/1357633981931416. [DOI] [PubMed] [Google Scholar]
- 14.Chen RS, Chen SK. Teledentistry using videoconferencing and a DICOM image management system. J Telemed Telecare. 2002;8(4):244–246. doi: 10.1258/135763302320272248. [DOI] [PubMed] [Google Scholar]
- 15.Clark RA, Eckert KA, Stewart S, Phillips SM, Yallop JJ, Tonkin AM, Krum H. Rural and urban differentials in primary care management of chronic heart failure: new data from the CASE study. Med J Aust. 2007;186(9):441–445. doi: 10.5694/j.1326-5377.2007.tb00993.x. [DOI] [PubMed] [Google Scholar]
- 16.Cotton JL, Gallaher KJ, Henry GW. Accuracy of interpretation of full-length pediatric echocardiograms transmitted over an integrated services digital network telemedicine link. South Med J. 2002;95(9):1012–1016. [PubMed] [Google Scholar]
- 17.Dańda J, Juszkiewicz K, Leszczuk M, Loziak K, Papir Z, Sikora M, Watza R. Medical video server construction. Pol J Pathol. 2003;54(3):197–204. [PubMed] [Google Scholar]
- 18.Falk V, Mourgues F, Vieville T, Jacobs S, Holzhey D, Walther T, Mohr FW, Coste-Manière E. Augmented reality for intraoperative guidance in endoscopic coronary artery bypass grafting. Surg Technol Int. 2005;14:231–235. [PubMed] [Google Scholar]
- 19.Firstenberg MS, Greenberg NL, Garcia MJ, Morehead AJ, Cardon LA, Klein AL, Thomas JD. Internet-based transfer of cardiac ultrasound images. J Telemed Telecare. 2000;6(3):168–171. doi: 10.1258/1357633001935275. [DOI] [PubMed] [Google Scholar]
- 20.Gackowski A, Cała J, Czekierda Ł, Zieliński K, Nowak M, Powroźnik P, Wolański M, Kruszyński M, Podolec P. Digital archiving and teleconsultation of echocardiographic exam: practical echocardiography. Ed. Podolec P, Tracz W, Hoffman P, Gackowski A. Medycyna Praktyczna Kraków, 2006.
- 21.Geoffroy O, Acar P, Caillet D, Edmar A, Crepin D, Salvodelli M, Dulac Y, Paranon S. Videoconference pediatric and congenital cardiology consultations: a new application in telemedicine. Arch Cardiovasc Dis. 2008;101(2):89–93. doi: 10.1016/S1875-2136(08)70264-X. [DOI] [PubMed] [Google Scholar]
- 22.Georgiadis P, Cavouras D, Daskalakis A, Sifaki K, Malamas M, Nikiforidis G, Solomou E. PDA-based system with teleradiology and image analysis capabilities. Conf Proc Eng Med Biol Soc. 2007;2007:3090–3093. doi: 10.1109/IEMBS.2007.4352981. [DOI] [PubMed] [Google Scholar]
- 23.Gómez EJ, Pozo F, Quiles JA, Arredondo MT, Rahms H, Sanz M, Cano P. A telemedicine system for remote cooperative medical imaging diagnosis. Comput Methods Programs Biomed. 1996;49(1):37–48. doi: 10.1016/0169-2607(95)01706-2. [DOI] [PubMed] [Google Scholar]
- 24.Gray WP, Somers J, Buckley TF. Report of a national neurosurgical emergency teleconsulting system. Neurosurgery. 1998;42(1):103–107. doi: 10.1097/00006123-199801000-00020. [DOI] [PubMed] [Google Scholar]
- 25.Hands LJ, Clarke M, Mahaffey W, Francis H, Jones RW. An e-Health approach to managing vascular surgical patients. Telemed J E Health. 2006;12(6):672–680. doi: 10.1089/tmj.2006.12.672. [DOI] [PubMed] [Google Scholar]
- 26.Hooper GS, Yellowlees P, Marwick TH, Currie PJ, Bidstrup BP. Telehealth and the diagnosis and management of cardiac disease. J Telemed Telecare. 2001;7(5):249–256. doi: 10.1258/1357633011936471. [DOI] [PubMed] [Google Scholar]
- 27.Huffer LL, Bauch TD, Furgerson JL, Bulgrin J, Boyd SY. Feasibility of remote echocardiography with satellite transmission and real-time interpretation to support medical activities in the austere medical environment. J Am Soc Echocardiogr. 2004;17(6):670–674. doi: 10.1016/j.echo.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 28.Lamminen H, Ruohonen K. Fundus imaging and the telemedical management of diabetes. J Telemed Telecare. 2002;8(5):255–258. doi: 10.1258/135763302760314207. [DOI] [PubMed] [Google Scholar]
- 29.Löfgren C, Boman K, Olofsson M, Lindholm L. Is cardiac consultation with remote-controlled real-time echocardiography a wise use of resources? Telemed J E Health. 2009;15(5):431–438. doi: 10.1089/tmj.2008.0148. [DOI] [PubMed] [Google Scholar]
- 30.Luccichenti G, Cademartiri F, Pichiecchio A, Bontempi E, Sabatini U, Bastianello S: User interface of a teleradiology system for the MR assessment of multiple sclerosis. J Digit Imaging. 2009. [DOI] [PMC free article] [PubMed]
- 31.Mantero A, Catena E, Tarelli G, Torta D, Barbier P, Pedroncelli E, Begnis R, Tappia D, Lombardi F, Vitali E. Teleconsulting in echocardiography using a standard cable on HDSL. G Ital Cardiol. 2007;8(3):168–175. [PubMed] [Google Scholar]
- 32.Martinelli T, Bosson JL, Bressollette L, Pelissier F, Boidard E, Troccaz J, Cinquin P. Robot-based tele-echography: clinical evaluation of the TER system in abdominal aortic exploration. J Ultrasound Med. 2007;26(11):1611–1616. doi: 10.7863/jum.2007.26.11.1611. [DOI] [PubMed] [Google Scholar]
- 33.McConnell ME, Steed RD, Tichenor JM, Hannon DW. Interactive telecardiology for the evaluation of heart murmurs in children. Telemed J. 1999;5(2):157–161. doi: 10.1089/107830299312113. [DOI] [PubMed] [Google Scholar]
- 34.Munir JA, Soh EK, Hoffmann TN, Stewart JP. A novel approach to tele-echocardiography across the Pacific. Hawaii Med J. 2004;63(10):310–313. [PubMed] [Google Scholar]
- 35.Napoli M, Nanni M, Cimarra S, Crisafulli L, Campioni P, Marano P. Picture archiving and communication in radiology. Rays. 2003;28(1):73–81. [PubMed] [Google Scholar]
- 36.Neri E, Thiran JP, Caramella D, Petri C, Bartolozzi C, Piscaglia B, Macq B, Duprez T, Cosnard G, Maldague B, Pauw J. Interactive DICOM image transmission and telediagnosis over the European ATM network. IEEE Trans Inf Technol Biomed. 1998;2(1):35–38. doi: 10.1109/4233.678534. [DOI] [PubMed] [Google Scholar]
- 37.Nitzkin JL, Zhu N, Marier RL. Reliability of telemedicine examination. Telemed J. 1997;3(2):141–157. doi: 10.1089/tmj.1.1997.3.141. [DOI] [PubMed] [Google Scholar]
- 38.Sable CA, Cummings SD, Pearson GD, Schratz LM, Cross RC, Quivers ES, Rudra H, Martin GR. Impact of telemedicine on the practice of pediatric cardiology in community hospitals. Pediatrics. 2002;109(1):E3. doi: 10.1542/peds.109.1.e3. [DOI] [PubMed] [Google Scholar]
- 39.Sekar P, Vilvanathan V. Telecardiology: effective means of delivering cardiac care to rural children. Asian Cardiovasc Thorac Ann. 2007;15(4):320–323. doi: 10.1177/021849230701500411. [DOI] [PubMed] [Google Scholar]
- 40.Smith AC, Williams M, Justo R. The multidisciplinary management of a paediatric cardiac emergency. J Telemed Telecare. 2002;8(2):112–114. doi: 10.1258/1357633021937578. [DOI] [PubMed] [Google Scholar]
- 41.Stahl JN, Zhang J, Zellner C, Pomerantsev EV, Chou TN, Huang HK. A new approach to teleconferencing with intravascular US and cardiac angiography in a low-bandwidth environment. Radiographics. 2000;20(5):1495–1503. doi: 10.1148/radiographics.20.5.g00se151495. [DOI] [PubMed] [Google Scholar]
- 42.Tsai CL, Madore B, Leotta MJ, Sofka M, Yang G, Majerovics A, Tanenbaum HL, Stewart CV, Roysam B. Automated retinal image analysis over the Internet. Trans Inf Technol Biomed. 2008;12(4):480–487. doi: 10.1109/TITB.2007.908790. [DOI] [PubMed] [Google Scholar]
- 43.Umans V, Kok W, Spruijt HJ, Bronzwaer J. Clinical feasibility of remote angiographic teleconsultation using a ISDN-30 communication network. Telemed J. 1999;5(4):391–394. doi: 10.1089/107830299311961. [DOI] [PubMed] [Google Scholar]
- 44.Umeda A, Iwata Y, Okada Y, Shimada M, Baba A, Minatogawa Y, Yamada T, Chino M, Watanabe T, Akaishi M. A low-cost digital filing system for echocardiography data with MPEG4 compression and its application to remote diagnosis. J Am Soc Echocardiogr. 2004;17(12):1297–1303. doi: 10.1016/j.echo.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 45.Walsh C, Cosgrave J, Crean P, Murray D, Walsh R, Kennedy J, Buckley M, O'Hare N. Synchronized, interactive teleconferencing with digital cardiac images. J Digit Imaging. 2006;19(1):85–91. doi: 10.1007/s10278-005-8147-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wei Z, Wu Y, Deng RH, Yu S, Yao H, Zhao Z, Ngoh LH, Han LT, Poh EW. A secure and synthesis tele-ophthalmology system. Telemed J E Health. 2008;14(8):833–845. doi: 10.1089/tmj.2008.0086. [DOI] [PubMed] [Google Scholar]
- 47.Weisser G, Engelmann U, Ruggiero S, Runa A, Schröter A, Baur S, Walz M. Teleradiology applications with DICOM-e-mail. Eur Radiol. 2007;17(5):1331–1340. doi: 10.1007/s00330-006-0450-8. [DOI] [PubMed] [Google Scholar]
- 48.Widmer S, Ghisla R, Ramelli GP, Taminelli F, Widmer B, Caoduro L, Gallino A. Tele-echocardiography in paediatrics. Eur J Pediatr. 2003;162(4):271–275. doi: 10.1007/s00431-003-1170-6. [DOI] [PubMed] [Google Scholar]
- 49.Woodson KE, Sable CA, Cross RR, Pearson GD, Martin GR. Forward and store telemedicine using Motion Pictures Expert Group: a novel approach to pediatric tele-echocardiography. J Am Soc Echocardiogr. 2004;17(11):1197–1200. doi: 10.1016/j.echo.2004.06.032. [DOI] [PubMed] [Google Scholar]