Abstract
Objective
In 39 US states, people with reduced visual acuity are permitted to drive with a bioptic telescope. Magnification causes a blind area (ring scotoma) around the telescope view, which may impair detection of traffic hazards. We evaluated the ability of the fellow eye to detect stimuli in the area corresponding to the ring scotoma of monocular bioptics in simple conditions (conventional perimetry) and more visually-demanding conditions.
Methods
7 bioptic-users and 7 non-users participated. A computerized dichoptic perimeter enabled separate stimuli to be presented to each eye. The bioptic ring scotoma was mapped by presenting the stimulus to the telescope eye only. Detection tests were then conducted under binocular viewing with stimuli only presented to the fellow eye in a 2×2×2 design: with or without telescope, on uniform gray or patterned (spatial noise) background, with passive (looking at cross) or active (reading letters) fixation task.
Results
There were no significant differences in fellow-eye detection with (86%) and without (87%) a bioptic. Detection rate was significantly reduced on the patterned background and in the active fixation task.
Conclusions
This is the first study to demonstrate fellow-eye detection in the area of the ring scotoma with a monocular bioptic under more realistic and visually-demanding conditions than conventional perimetry. These results should ease the concerns about the monocular ring scotoma causing blindness to traffic outside the field of the telescope.
INTRODUCTION
Monocular bioptic telescopes enable people with reduced visual acuity (VA) to see details of distant objects (Figure 1). Licensure regulations in 39 US states permit driving with a bioptic telescope with widely varying requirements (e.g. minimum VA without the bioptic, and peripheral visual field extent), and an even wider variation in the restrictions imposed (e.g. daylight driving only, no highway driving, requiring side mirrors, and others).1 The majority of bioptic drivers report that the telescope is very helpful, and use it for tasks such as reading road signs and checking the status of traffic light signals.2 Loss of driving privileges greatly impacts economic and emotional well-being,3 while lack of regulation may subject the driver and the general public to undue risk. Unfortunately there has been little scientific basis for allowing or restricting bioptic driving.1 This study attempts to provide rigorous data to inform the debate over the issue of the ring scotoma associated with the use of bioptic telescopes.
Figure 1.
(a) Bioptic users view below the telescope most of the time. (b) Looking intermittently through the telescope with a downward tilt of the head.
Bioptic telescopes are usually mounted on a carrier lens above the primary gaze position tilted upward (Figure 1a). When the wearer wants to examine something more closely, a head tilt of about 10° to 20° and an associated shift of eye position brings the eye, the telescope, and the object of regard into alignment (Figure 1b), offering a magnified view. Normally, only infrequent and brief glances through the telescope are needed.2, 4, 5 Nonetheless, driving is a complex and demanding activity, and even brief vision interruptions may degrade performance. Thus, it is important to understand the hazard detection potential of the fellow (non-telescope) eye when viewing through the telescope.
When viewing through a telescope, the magnified field of view on the retina covers much of the image normally available in the unmagnified view, thus a “ring scotoma” is created around the magnified telescope view (Figure 2). When driving, the ring scotoma could block important traffic features. Some states permit binocular bioptics for driving. With binocular bioptics the ring scotoma is bilateral (and absolute). However, if a monocular bioptic telescope is used, the fellow eye could potentially monitor the scene outside of the telescope view. Some have argued that, due to the available view with the fellow eye, the ring scotoma does not introduce a hazard for a monocular bioptic,6–10 while others have insisted that the driver becomes blind to traffic when viewing through the bioptic.11, 12 Neither point of view has been supported by a systematic investigation.
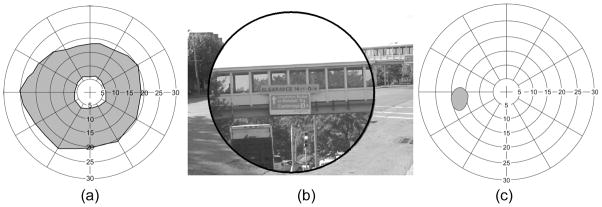
Figure 2.
(a) The ring scotoma when viewing through a 3x Ocutech Mini bioptic telescope. The plotted field of view through the telescope has a diameter of 12 degrees, and the ring scotoma (gray area) has a diameter of 44 degrees with a 75% contrast stimulus (somewhat larger than the computed 36 degrees). (b) A simulated view of a road sign as viewed through a 3x bioptic telescope. The magnified view blocks the view of the intersection. (c) The binocular visual field measured when viewing binocularly through the same telescope. The ring scotoma is no longer apparent as the fellow eye is able to detect the perimetry targets in the ring scotoma area. Only field corresponding to the physiological blind spot of the fellow eye is recorded as not seen, because it overlaps within the ring scotoma.
Previous work has shown that in the simple visual conditions of conventional perimetry (e.g., a spot of light on a plain background), the fellow eye can detect targets presented in the area of the ring scotoma when viewing through a monocular bioptic telescope (Figure 2c).5, 10, 13 However, conditions in a conventional perimeter are not representative of the situation during driving; the target is of high contrast and there is no masking background or competing binocular view. Would the target be detected under conditions more akin to real driving? The answer is not obvious. In particular, suppression or rivalry due to the difference in image size between the two eyes may hinder perception.14
Using a bioptic when driving requires active viewing (e.g. reading a road sign). Increasing attentional load has been shown to reduce detection performance when driving;15 therefore the ability of the fellow eye to detect objects in the ring scotoma may be lower in active viewing than in the passive viewing of conventional perimetry.
We evaluated detection performance of the fellow eye in the area of the ring scotoma on both simple (plain gray) and more complex (patterned) backgrounds and in visual conditions of both passive viewing and active viewing (reading letters through the bioptic). We also compared detection performance of participants with and without prior experience of using bioptic telescopes. Our primary hypotheses were that fellow-eye detection rates would be lower: (1) when using the bioptic than not using the bioptic; (2) on the complex than the simple background; (3) in active than passive viewing; and (4) for non-bioptic-users than bioptic-users (as non-users would be more likely to suppress the fellow eye).
METHODS
Participants
We included both younger and older people with reduced visual acuity, both with and without central visual field loss (CFL). Inclusion criteria were: visual acuity (VA) of 20/40 to 20/200 in the better-seeing (telescope) eye; VA of 20/50 to 20/200 in the worse seeing (fellow) eye; no manifest strabismus (evaluated with cover test) and, for participants with CFL, the position and size of central scotoma in the fellow eye had to enable sufficient area for presenting test stimuli.
In total, 28 participants were recruited from local clinics, including 13 bioptic-users (owned and used a bioptic in the last year). Of these 28, 8 failed to meet the inclusion criteria (2 for VA, 1 for scotoma size, 5 for strabismus) and 5 did not complete the study (failed to attend the second visit) due to non-visual reasons. Data for 1 participant was excluded due to unreliable responses. Thus 7 bioptic-users and 7 non-users completed the study. All participants completed the battery of vision tests summarized in Table 1.
TABLE 1.
Vision tests
| Equipment used | Comments | |
|---|---|---|
| Visual Acuity | TestChartPro2000 | Monocular and binocular without bioptic Telescope eye with study bioptic |
| Letter Contrast sensitivity | Custom designed program | Binocular without bioptic |
| Fundus perimetry | Nidek MP-1 microperimeter | Document retinal lesions, and aid in mapping visual fields |
| Monocular visual fields without bioptic | Dichoptic perimeter* without the shutter lenses | Mapped the physiological blind spot and scotoma (if any) of each eye separately Kinetic perimetry on gray background with75% contrast stimulus |
| Monocular visual field with study bioptic | Dichoptic perimeter* without the shutter lenses | Mapped field of view through the bioptic and outer boundary of the ring scotoma Kinetic perimetry on gray background with 75% contrast stimulus |
See online supplementary materials for details
The study was conducted in accordance with the tenets of the Declaration of Helsinki. All participants signed a consent form approved by the Schepens IRB.
Bioptic telescopes
In our previous survey of bioptic drivers2, the two most commonly prescribed monocular bioptics were the Designs for Vision Galilean bioptic telescope (Designs for Vision (DVI), Inc., Ronkonkoma, NY) and the Ocutech Mini Keplerian bioptic telescope (Ocutech Inc., Chapel Hill, NC). We therefore used both types in this study. Emmetropes and participants with contact lenses were fitted with a 3.0× DVI Galilean telescope, while those with spectacle correction were fitted with a 3.0× Ocutech Mini Keplerian telescope that has focus adjustment to compensate for the ametropia. Four bioptic-users and 3 non-users used the DVI telescope in the study; the remaining participants used the Ocutech Mini. For the participants in this study, the measured median field of view of the Ocutech bioptic was 11° with a median ring scotoma of 44° in diameter. The Designs for Vision bioptic had a smaller field of view and ring scotoma (median 8° and 38.5° in diameter). See eBioptic Telescopes for further discussion.
The telescopes were mounted centrally in the carrier lenses, not in the bioptic position, so that the experiments could be conducted without the strain of maintaining a head tilt and an eccentric gaze position for long periods. The telescopes were mounted in a custom frame with an adjustable bridge. The bridge was adjusted so that the bioptic was centered at the participant’s pupil. For the bioptic users, the telescope was mounted in front of the same eye as their own bioptics were mounted, and non-users were fitted with the bioptic on the sighting dominant eye (determined using the hole-in-the-card test16). The fellow eye was fitted with a single vision lens with the participant’s habitual distance prescription; including an additional +1D add to focus at the 1m testing distance. When viewing through the telescope, the focus adjustment on the Ocutech and a +1D reading cap on the DVI bioptic enabled clear focus at the 1m testing distance.
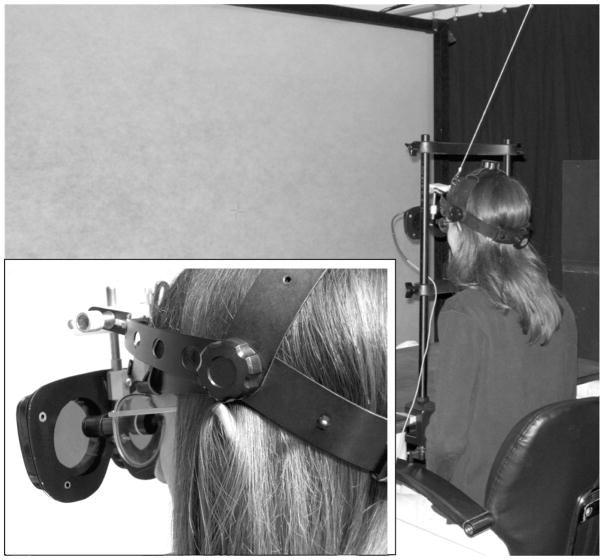
Perimetry apparatus
We used a dichoptic perimetry system17 developed in our lab that enables separate control of the stimuli presented to each eye. Participants wore goggles with ferro-electric liquid crystal shutters (CRS, Rochester, UK) suspended in front of the eyes by a modified indirect ophthalmoscope headband to provide sufficient clearance behind the shutters for the telescope (Figure 3). Because the shutter lens frame restricted field of view, the area of the central visual field that could be seen by each eye was about 25° in diameter and was asymmetric extending further temporally than nasally, especially in participants with narrow inter-pupillary distances (IPD of the shutter lenses was fixed at 68mm). With this system, the fixation mark and an image background can be presented to both eyes, while the perimetry target is presented only to the fellow (non-telescope) eye. Thus, there is no chance that a target intended to be in the ring scotoma would be detected by the telescope eye, even if the scotoma is mis-localized by participant eye or head movements. See ePerimetry Apparatus for further details.
Figure 3.
The apparatus used in this study. Participants wore a modified indirect ophthalmoscope headband with the shutter lenses suspended forward and sat 1m from the screen where the fixation target and stimuli were presented. Inset (lower left) shows details of how the shutter lenses were suspended (the chin rest support bar was removed for the photo of the inset).
Background images
Two different backgrounds were used; a plain light gray background (level 186 of 255) similar to standard perimetry testing, and a patterned spatial noise background (Figure 4) which changed after each trial. The noise background had spatial frequency characteristics similar to those of natural scenes and was thus used to resemble real-world pictures but without the problems of large areas of varying contrast, luminance, and clutter that could alter the difficulty of the detection task (See eBackground Images in online supplemental materials for details). Mean luminance of all backgrounds was 38cd/m2 (8cd/m2 through the shutter lenses).
Figure 4.
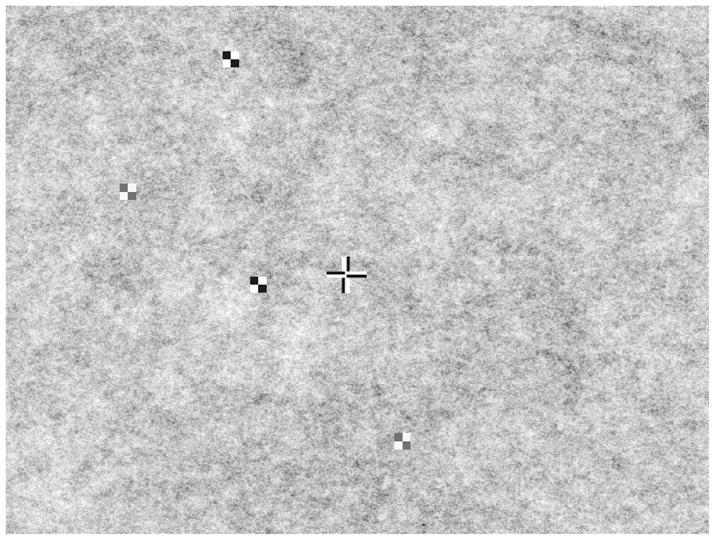
The spatial noise background used in this study with passive fixation cross (2.9° cross) and 75% and 95% contrast stimuli (1°) shown.
Fixation tasks
Two types of fixation tasks were used: passive and active. The fixation target for the passive task was a static black-and-white cross, with legs 8.4 mm (0.5°) thick (4.2 mm white, 4.2 mm black, switching sides at the crossing point, see Figure 4) and overall length and width 50.4 mm (2.9°). For the active task, a single black letter on a white square (1° or 1.4° with bioptic; 2° or 2.7° without bioptic) background was fixated with the letter changing every 2 s. For trials in which the bioptic telescope was used, the letters were 12.6 or 16.8 mm (0.7° or 1.0°) in height, and when the bioptic telescope was not used the letters were 31.5 or 37.8mm (1.8° or 2.2°). In each case, the letter size was selected to enable comfortable reading.
Perimetry target stimuli
The probe stimulus was a 2×2 black-and-white checkerboard 16.8 mm square (1°). The stimulus was presented with internal (Michelson) contrast of either 75% or 95%. See ePerimetry Target Stimuli for details of how the stimulus was chosen. Stimuli were presented for 250 ms, followed by a grace period of 600 ms for accepting a participant button-press response. To avoid onset predictability (and any chance of responding based on timing rather than detection of the stimulus), a randomized delay of 1000 to 1950 ms occurred between stimulus extinction and the next stimulus.
Test condition sequence
The experiment involved 8 test conditions in a 2×2×2 design: with or without telescope, passive or active fixation task, and uniform gray or noise background. Testing was divided into 2 blocks of 4 conditions. Half of the participants used the telescope for the first two conditions of each block and half for the last two conditions of a block. The order of fixation task and background types was counterbalanced within each block and across participants. The total time to complete the 8 test conditions was on average 1 hour.
Procedures
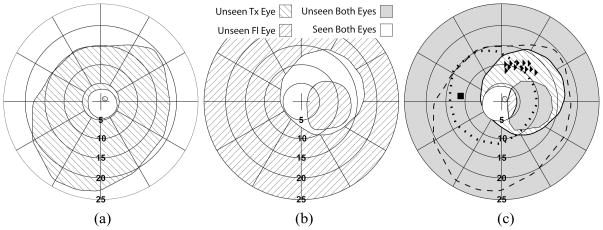
All trials were conducted in dichoptic mode, with the background and fixation targets shown to both eyes. Each condition contained 5 repetitions of 13 stimuli sequentially presented within the area corresponding to the individual’s ring scotoma (Figure 5) and not blocked by the shutter lens or the participant’s fellow eye central scotoma (if any). The order of the 13 stimulus positions was randomly changed for each of the 5 repetitions. See eProcedure for details of control stimuli and how number of stimuli, stimulus location, and eccentricity was chosen.
Figure 5.
An example of the visual field plots obtained for a participant with age-related macular degeneration wearing an Ocutech bioptic on the left side. (a) Monocular viewing without the shutter lenses showing the ring scotoma of the telescope. The participant’s scotoma appears minified through the bioptic. (b) Binocular viewing with the shutter lenses showing the participant’s fellow-eye scotoma and the restriction in visual field size due to the shutter-lens housing. The fixation and background were shown to both eyes and the kinetic stimulus presented to the fellow eye only. (c) Binocular viewing with the shutter lenses; fixation and background shown to both eyes. The kinetic stimulus was presented to the fellow eye only and then to the telescope eye only. The right-facing triangles show the position of the static test stimuli presented to the fellow eye while the participant focused on the fixation target through the telescope. The square shows the position of control static stimuli presented to the telescope eye. The dashed line shows the outer boundary of the ring scotoma as measured in (a). The dotted line indicates the restriction of the telescope-eye shutter lens.
Participants were instructed to fixate on the fixation target and press a hand-held button when a stimulus was detected. For the active fixation trials, they were required to verbally report each letter in the fixation target and press the button when a stimulus was detected. This ensured that they were maintaining fixation and attention.
Data analysis
Detection performance (number of detections as a fraction of the total number of stimulus presentations) for each test condition was the primary dependent variable. A probit transform was applied to convert the percentile to z-scores to avoid the truncation effect.18, 19 A value of 2.4 was used in cases where 100% of the stimuli were detected and −2.4 in cases where no stimuli were detected. A repeated measures ANOVA was used for analysis as the detection z-scores in each condition did not differ significantly from a normal distribution (Shapiro-Wilk p>0.05). As there was a wide range in participants’ ages, we included age as a covariate in the analysis.20, 21 Fellow-eye detection rates reported in the results are all age adjusted.
RESULTS
Sample characteristics
Participants had a wide variety of diagnoses (Table 2) including 7 with CFL (median fellow-eye and telescope-eye scotoma diameter of 16°(range 6° to 28°). There were no significant differences between bioptic-users and non-users for age, visual acuity in the telescope eye, visual acuity in the fellow eye, and contrast sensitivity (Table 3).
Table 2.
Summary of diagnosis for bioptic-users and non-users
| Bioptic Users | Non-Users | |
|---|---|---|
| CFL | 4 | 3 |
| AMD (with CFL) | 1 | 1 |
| Stargardt’s | 2 | 1 |
| Chorioretinitis | 1 | |
| Doyne dystrophy | 1 | |
| No CFL | 3 | 4 |
| Early AMD (no CFL) | 1 | |
| Nystagmus | 1 | |
| Optic Atrophy | 1 | 2 |
| Rod monochromat | 1 | |
| Diabetic retinopathy | 1 |
Table 3.
Characteristics of enrolled participants
| Bioptic Users (n=7) | Non Bioptic Users (n=7) | Test for differences between groups† | |
|---|---|---|---|
| Male n (%) | 4 (57) | 4 (57) | χ2=0.000 p=1.0 |
| Age, yrs Median (IQR) |
59 (44 to 70) | 53 (35 to 74) | Mann-Whitney U =18.0 p=0.405 |
| Telescope Eye VA* without bioptic Median (IQR) |
20/60 (20/58 to 20/191) | 20/96 (20/76 to 20/126) | Mann-Whitney U =19.0 p=0.481 |
| Fellow Eye VA* Median (IQR) |
20/91 (20/83 to 20/174) | 20/120 (20/115 to 20/126) | Mann-Whitney U =19.0 p=0.480 |
| Contrast sensitivity Median (IQR) |
1.53 (1.38 to 1.60) | 1.33 (1.28 to 1.50) | Mann-Whitney U = 11.5 p=0.096 |
Visual acuity was measured and analyzed in logMAR units, logMAR values were converted to Snellen values for ease of interpretation in this table.
Median time using a bioptic for the bioptic-user group (n=7) was 7 years (range 0.7 to 22 years). Five of them used the bioptic when driving (primarily for reading street names, traffic signs and viewing traffic signals). In addition, 3 participants used the bioptic as spectators at events such as plays, theatre shows or sports. All participants reported the bioptic as helpful on a 5-point scale (1”not at all” to 5”very helpful”) with 86% reporting that it was at least moderately helpful and 29% very helpful. Frequency of bioptic use varied very widely within the bioptic-user group (see eBioptic Telescopes for details).
Fellow-eye detection ability
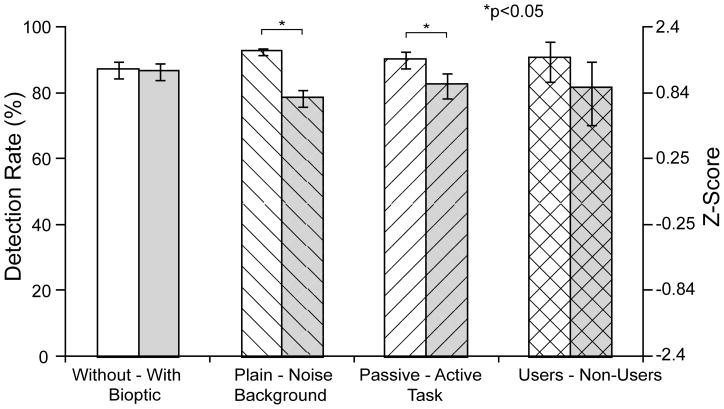
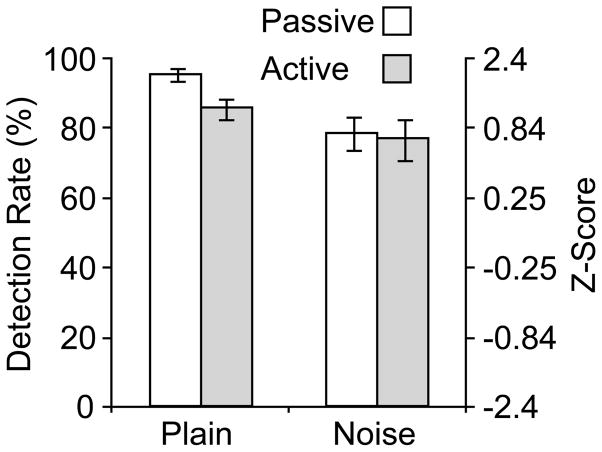
Detection rates under different conditions are shown in Figure 6, and repeated measures ANOVA results are summarized in Table 4. Contrary to our expectations, there was no significant difference between the mean age-adjusted fellow-eye detection rate with the bioptic (86%) and without the bioptic (87%) (means determined from data pooled across both backgrounds and fixation tasks). However, as expected, the detection rate reduced significantly from 92% on the plain background to 78% on the noise background (data pooled across both fixation tasks and with and without bioptic). There was also a significant reduction in detection rate with the active fixation task from 90% in the passive task to 82% in the active task (data pooled across both backgrounds and with and without bioptic). Furthermore, there was a significant interaction of task with background. While both the active task and noise background lowered detection, the difference in detection rates between the passive and active fixation conditions was greater on the plain (96% to 86%) than the noise background (79% to 77%; Figure 7).
Figure 6.
Mean age-adjusted fellow-eye detection rates for the primary factors in the repeated measures ANOVA. Fellow-eye detection performance was: not significantly different with and without a bioptic telescope; higher on the plain background than the noise background; higher in the passive fixation task than the active fixation task; and not significantly different between bioptic-users and non-users. Error bars are the within-subjects 95% confidence interval of the mean for all comparisons24, 25 except bioptic users vs. non-users, where between-subjects 95% confidence intervals are given.
Table 4.
ANOVA results (n=14)
| Bioptic | Background | Task | User | Age | |
|---|---|---|---|---|---|
| Bioptic (with/without) | F(1,11)=0.06, p=0.812 | F(1,11)=0.41, p=0.537 | F(1,11)=0.09, p=0.773 | F(1,11)=1.93, p=0.193 | F(1,11)=0.00, p=0.992 |
| Background (plain/noise) | F(1,11)=85.13, p<0.001 | F(1,11)=21.46, p=0.001 | F(1,11)=0.53, p=0.481 | F(1,11)=5.54, p=0.038 | |
| Task (passive/active) | F(1,11)=8.70, p=0.013 | F(1,11)=1.78, p=0.209 | F(1,11)=1.66, p=0.224 | ||
| User (User/non-user) | F(1,11)=3.41, p=0.092 | ||||
| Age (covariate) | F(1,11)=8.38, p=0.015 |
Shaded grey boxes show main effects. The others show interactions.
Bold text indicates a significant effect p<0.05.
Figure 7.
Mean age-adjusted fellow-eye detection rates for the passive and active fixation tasks on the plain and noise backgrounds. While both the active task and noise background lowered detection, the impact of the active fixation task was less on the more complex noise background. Error bars are the within-subjects 95% confidence interval of the mean.24, 25
There was a trend for the bioptic-user group to have better fellow-eye detection performance than the non-user group (on average 91% vs. 81%); however, this did not reach statistical significance. The interaction between user-group, task, and viewing with/without a bioptic was significant (F(1,11)= 4.89, p=0.049). Post hoc tests found that in the active task when using the bioptic, bioptic-users had higher detection rates than non-users, approaching significance (91% vs. 67%, p=0.06).
Finally (as might be expected) the covariate age had a significant effect: fellow-eye detection rates decreased with increasing age, and age had a stronger effect on the noise background than the plain background. However, there were no significant interactions between age and task or viewing with/without a bioptic.
DISCUSSION
Both bioptic-users and non-users were able to detect the majority of stimuli in the ring scotoma area with the fellow eye on complex backgrounds while engaged in an active viewing task through a monocular bioptic. Furthermore, fellow-eye detection rates were similar with and without the bioptic (86% and 87%, respectively). This suggests that the use of the monocular bioptic (and thus the different magnification in each eye) did not cause a reduction in fellow-eye detection performance and the fellow eye was not suppressed to any extent when using the bioptic in our test conditions. Suppression of one eye during binocular viewing is a common sensory adaptation in strabismus. Strabismus is not rare among low vision patients (we found 5 among the 28 we screened for this study). Suppression could affect fellow-eye detection in the area of the ring scotoma. Strabismus might also affect the eccentricity of the field area in the fellow eye overlapping the ring scotoma and thus also affect detection. We, therefore, are currently investigating fellow eye detection performance with monocular bioptics in people with strabismus.
The finding that fellow-eye detection rates were similar with and without the bioptic appears promising for easing the concerns about the ring scotoma causing blindness to traffic outside the field of the telescope.11, 12 Peli22 describes the ability to use both the fellow eye and telescope eye as bi-ocular multiplexing. The high resolution image (seen through the bioptic) is multiplexed with the available wide field of view (of the fellow eye) in a way that permits the visual system to separate them and use them in a natural way. While no mechanism for such multiplexing is apparent, it appears that such bi-ocular multiplexing is indeed possible, at least for the detection task tested here.
Use of the noise background with spatial frequency characteristics similar to those of natural scenes caused an overall reduction in detection from 92% on the plain background to 78% on the noise background, confirming our concern that standard perimetric evaluation (as previously performed10) is not sufficient to determine the impact of the ring scotoma on detection. Real-world scenes are more complex and change dynamically. Therefore we are conducting further studies to investigate the impact of a real-world moving background.
Our active viewing task more closely simulated the attention required when using a bioptic for tasks such as reading signs than the typical passive fixation in conventional perimetry. Monocular bioptic use is a type of dual-tasking (divided attention) situation. Users must attend to the information seen through the telescope while also being aware of the information seen with the fellow eye, where both usually fall on corresponding retinal areas. We found an overall reduction in detection from 90% in the passive fixation task to 82% in the active fixation task to be consistent with the literature showing reduced performance with increased attentional load.15, 23 However, there was no significant interaction of fixation task with viewing with/without a bioptic; overall the active fixation task had a similar impact on fellow-eye detection with and without a bioptic.
Interestingly, while both the noise background and active fixation task significantly reduced fellow-eye detection performance, the impact of the active task was lower on the more complex noise background than the simple plain background (Figure 7). In other words, even with the combination of active viewing and complex background, participants still achieved 77% detection, and the active task did not reduce detection as much as might have been expected when combining the 2 most difficult conditions. Attentional load is probably higher in real driving than in our experimental set up, as users have to see the object of regard quickly, and also deal with other driving activities such as controlling the steering, gas, brake etc. By comparison, in this study, observers looked through the bioptic continuously for several minutes at a time.
We hypothesized that participants who had not used bioptics would be more likely to suppress the fellow eye than bioptic-users. While the bioptic-users did have higher overall detection than non-users (91% vs. 81%), the difference was not significant (p=0.092 However, consistent with our hypothesis, bioptic users had higher detection rates than non-users (91% vs. 67%) in the most demanding condition (active task, viewing through bioptic) and the difference approached significance (p=0.06).
In summary, this is the first study to demonstrate fellow-eye detection in the area of the ring scotoma when viewing through a monocular bioptic in more visually complex conditions than those of conventional perimetry. Our finding of no difference in fellow-eye detection with and without a bioptic provides preliminary but strong evidence against the opinion that a driver becomes blind to traffic when viewing through a monocular bioptic,11, 12 but needs to be further confirmed in test conditions that even more closely simulate real-world use of a bioptic. We plan to conduct future studies to evaluate bi-ocular multiplexing ability in conditions involving more natural bioptic use including dynamic motion backgrounds (real traffic videos), viewing through the bioptic for brief glances when detail is needed, and testing the fellow eye over a larger area of the ring scotoma.
Supplementary Material
Acknowledgments
The authors thank Dr Russell Woods and Henry Apfelbaum for advice and helpful comments when preparing the manuscript. This research was supported in part by NIH grants EY12890 (EP), EY05957(EP), EY018680 (ARB) and AG034553 (GL). The NIH had no role in study design, data collection, data analysis or report writing. The first author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Peli E, Peli D. Driving With Confidence: A Practical Guide to Driving With Low Vision. Singapore: World Scientific; 2002. [Google Scholar]
- 2.Bowers AR, Apfelbaum DH, Peli E. Bioptic telescopes meet the needs of drivers with moderate visual acuity loss. Invest Ophthalmol Vis Sci. 2005;46:66–74. doi: 10.1167/iovs.04-0271. [DOI] [PubMed] [Google Scholar]
- 3.Ragland DR, Satariano WA, MacLeod KE. Driving cessation and increased depressive symptoms. J Gerontol Series A Biol Sci Med Sci. 2005;60:399–403. doi: 10.1093/gerona/60.3.399. [DOI] [PubMed] [Google Scholar]
- 4.Luo G, Fu X, Peli E. A recording and analysis system of bioptic driving behaviors. Proceedings of the 5th International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design; Driving Assessment, Big Sky, MT; 2009. pp. 460–467. [Google Scholar]
- 5.Peli E. Functional fields of bioptic telescopes: Implications for driving (abstract). International BiOptic Driving Conference; London, UK. 2004. [Google Scholar]
- 6.Feinbloom W. Driving with bioptic telescopic spectacles. Am J Optom Physiol Opt. 1977;54(1):35–42. [PubMed] [Google Scholar]
- 7.Jose R, Ousley BA. The visually handicapped, driving with bioptics - some new facts. Rehabil Optom. 1984;2:2–5. [Google Scholar]
- 8.Kelleher DK, Mehr EB, Hirsch MJ. Motor vehicle operation by a patient with low vision: a case report. Am J Optom Arch Am Acad Optom. 1971;48:773–776. doi: 10.1097/00006324-197109000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Korb DR. Preparing the visually handicapped person for motor vehicle operation. Am J Optom Arch Am Acad Optom. 1970;47:619–628. [PubMed] [Google Scholar]
- 10.Lippmann O, Corn AL, Lewis MC. Bioptic telescopic spectacles and driving performance: A study in Texas. J Vis Impair Blind. 1988;82:182–187. [Google Scholar]
- 11.Fonda G. Bioptic telescopic spectacle is a hazard for operating a motor vehicle. Arch Ophthalmol. 1983;101:1907–1908. doi: 10.1001/archopht.1983.01040020909015. [DOI] [PubMed] [Google Scholar]
- 12.Keeney AH. Field Loss vs. Central Magnification. Arch Ophthalmol. 1974;92:273. doi: 10.1001/archopht.1974.01010010283001. [DOI] [PubMed] [Google Scholar]
- 13.Fetchenheuer I, Peli E, Woods RL. Functional visual fields of monocular bioptic telescopes (abstract). The 7th International Conference on Low Vision: Activity and Participation; 2002. p. 81. [Google Scholar]
- 14.Blake R. A primer on binocular rivalry, including current controversies. Brain and Mind. 2001;2:5–38. [Google Scholar]
- 15.Chaparro A, Wood JM, Carberry T. Effects of age and auditory and visual dual tasks on closed-road driving performance. Optom Vis Sci. 2005;82:747–754. doi: 10.1097/01.opx.0000174724.74957.45. [DOI] [PubMed] [Google Scholar]
- 16.Seijas O, Gomez de Liano P, Gomez de Liano R, Roberts CJ, Piedrahita E, Diaz E. Ocular dominance diagnosis and its influence in monovision. Am J Ophthalmol. 2007;144:209–216. doi: 10.1016/j.ajo.2007.03.053. [DOI] [PubMed] [Google Scholar]
- 17.Woods RL, Apfelbaum HL, Peli E. DLP-based dichoptic vision test system. J Biomed Optics. 2010;15:1–13. doi: 10.1117/1.3292015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pearson K. On the Theory of Contingency and Its Relation to Association and Normal Correlation. Cambridge University Press; London: 1904. [Google Scholar]
- 19.Winer BJ, Brown DR, Michels KM. Statistical Principles in Experimental Design. McGraw-Hill; New York: 1991. [Google Scholar]
- 20.Aligna J. Remarks on the analysis of covariance in repeated measures designs. Multivariate Behav Res. 1982;17:117–130. [Google Scholar]
- 21.Delaney HD, Maxwell SE. On using analysis of covariance in repeated measures designs. Multivariate Behav Res. 1981;16:105–123. doi: 10.1207/s15327906mbr1601_6. [DOI] [PubMed] [Google Scholar]
- 22.Peli E. Vision multiplexing: An engineering approach to vision rehabilitation device development. Optom Vis Sci. 2001;78:304–315. doi: 10.1097/00006324-200105000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Strayer DL, Johnston WA. Driven to distraction: dual-Task studies of simulated driving and conversing on a cellular telephone. Psychol Sci. 2001;12:462–466. doi: 10.1111/1467-9280.00386. [DOI] [PubMed] [Google Scholar]
- 24.Loftus GR, Masson MEJ. Using confidence intervals in within-subject designs. Psychon Bull Rev. 1994;1:476–490. doi: 10.3758/BF03210951. [DOI] [PubMed] [Google Scholar]
- 25.Wright DB. Graphing within-subjects confidence intervals using SPSS and S-Plus. Behav Res Methods. 2007;39:82–85. doi: 10.3758/bf03192846. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.