Summary
Strategies for inducing immune tolerance are fundamentally similar across a spectrum of immune-mediated disorders, including allergic disease, autoimmunity, and rejection of allografts. In each case, the objective of establishing an immunoregulatory balance is challenged by variable upswings in effector cell populations and proinflammatory mediators of immunity, requiring careful and innovative therapeutic intervention to restore stability. The Immune Tolerance Network, an international consortium sponsored by the National Institutes of Health, seeks to advance both the scientific understanding and the clinical success of immune therapies for these disorders, through an innovative and collaborative effort involving clinical trials and mechanistic studies. Over the last decade, scientists have evaluated cell-based ablation and deviation strategies in trials using lymphocyte-specific targeting, induction of host-donor hematopoietic chimerism, induction of antigen-specific immune regulation, and a variety of antigen desensitization approaches. In this article, we review some of the highlights of this experience and discuss the potential for progress, utilizing new insights into regulatory mechanisms and biomarker signatures of tolerance.
Keywords: immune-mediated disease, tolerance, immunosuppression, transplantation, allergy, autoimmunity
Therapy for immune-mediated diseases and for transplantation poses a daunting challenge: how best to modulate the immune response for clinical benefit while avoiding long-term immunosuppression, which puts the patient at risk. Fundamental insights into the mechanisms of immune response, developed over the last three decades, have spawned a large number of therapeutic initiatives designed to address this challenge. These efforts to induce immune tolerance represent specific and targeted approaches to reprogram, regulate, or selectively ablate immune cells, eliminate deleterious responses, and restore normal immune homeostasis (Fig. 1).
Fig. 1.
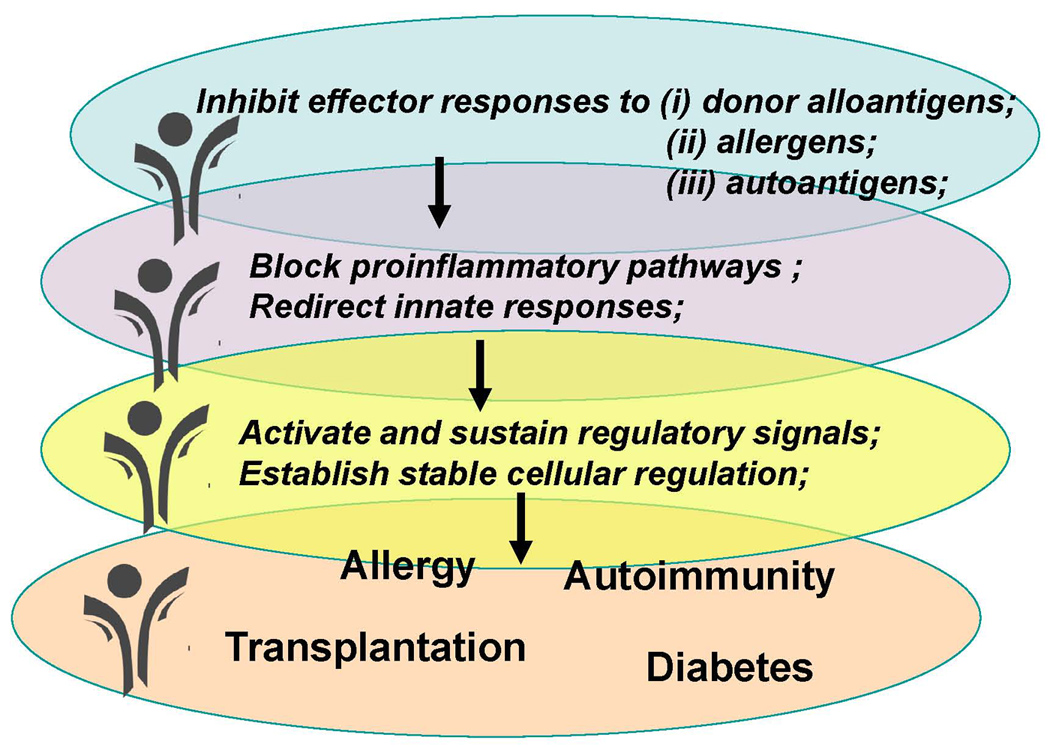
Cross-cutting strategies for the induction of immune tolerance.
The Immune Tolerance Network (ITN) was created to respond to that challenge. The ITN developed as an international consortium, established 10 years ago by the National Institutes of Health in partnership with the Juvenile Diabetes Research Foundation. The ITN exists to advance this field by conducting clinical trials of novel tolerance-inducing therapies and simultaneously studying immunologic mechanisms of the treatment and clinical response. The ITN is a large collaborative venture, involving several hundred basic and clinical immunologists, academic trial centers, and pharmaceutical and biotechnology partners. Centralized data management, regulatory affairs, and core laboratory services are integrated into each trial. Advisory panels and an academic steering committee review and comment on study rationale, protocol design, and mechanistic laboratory studies for each of the three major therapeutic areas of ITN activity: (i) prevent graft rejection after solid organ and tissue transplantation, (ii) achieve long-term tolerance to allergens, and (iii) stop or reverse autoimmune diseases.
Underlying the ITN approach is the premise that strategies and treatments to induce a state of immune tolerance are fundamentally similar across all three of these therapeutic areas (Fig. 2). Successful immune tolerance to allergens, autoantigens, and tissue alloantigens will share similar mechanistic principles and potentially share similar therapies. Under normal homeostatic conditions, peripheral immune tolerance is maintained through a combination of mechanisms that operate simultaneously, creating a redundancy that is essential for a nearly fail-safe system. Pathogenic lymphocytes are inactivated, deleted, deviated, or suppressed, and each of these fates occurs using molecular pathways and cellular interactions that are potential strategies for targeted therapy.
Fig. 2.
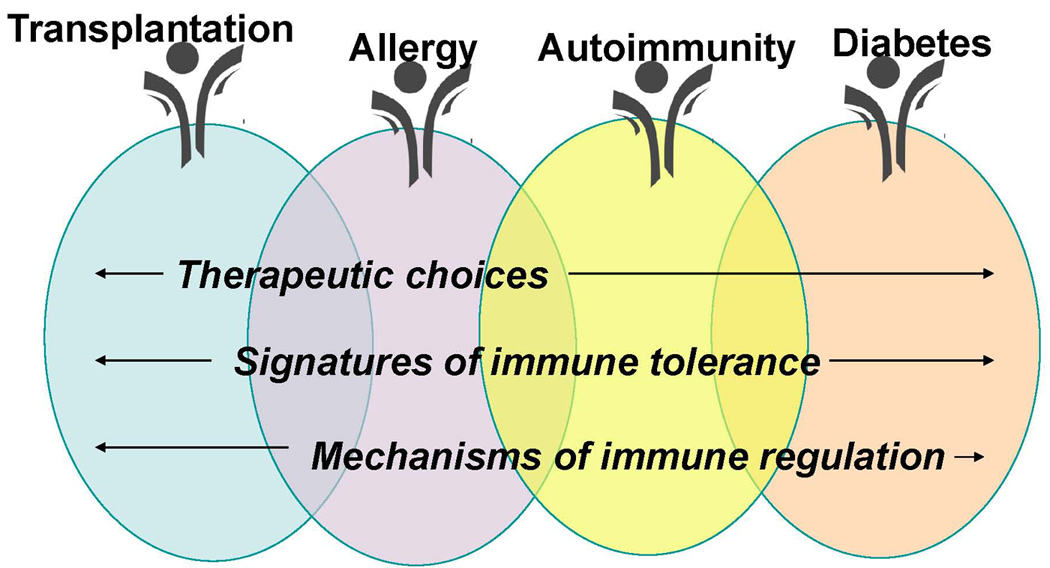
Cross-cutting themes of the Immune Tolerance Network.
In this article, we look back at the rationale and approach for some of the major ITN clinical trials and mechanistic studies of the last decade. We discuss the types of innovative approaches needed to advance our understanding of immune tolerance and to translate this knowledge into safe and effective therapies.
The lymphocyte as a therapeutic target
T lymphocytes have been a major focus of the ITN because of their central role in the pathogenesis of allograft rejection and autoimmune disease. A myriad of drugs, which target T cells and their functions, is now available, including soluble ligands and monoclonal antibodies directed against cell surface receptors. Many of these agents act by depleting T cells (e.g. anti-CD52 monoclonal antibody, CAMPATH-1H) or globally suppressing their function (e.g. calcineurin inhibitors), and consequently are associated with significantly increased risks for toxicity, especially infection. Producing such dramatic shifts in the immune system is indeed risky and may not be necessary to re-establish homeostasis. It is possible that small perturbations, achieved by therapeutic intervention at critical points in the regulatory pathways, may be sufficient to drive the system to a stable state of disease quiescence. Applying this reasoning, the ITN turned to CD3-specific antibodies as potential tolerance-inducing agents, based on their ability to selectively induce T-cell anergy and stimulate regulatory cells in non-obese diabetic (NOD) mice, where their use in established disease has been shown to preserve beta cell function (1, 2). Of the different candidate anti-CD3 antibodies available, the ITN has been studying huOKT3γ1ala-ala, an Fc receptor (FcR), non-binding monoclonal antibody, which now appears, from several clinical studies in type 1 diabetes, to ameliorate an antigen-driven chronic inflammatory response. The goal of the ITN, in this case, has been to induce immunological tolerance and disease remission, with subsequent withdrawal of the treatment.
Jeffrey Bluestone, Kevan Herold, and other members of the ITN have been central players in the historic development of CD3-specific antibodies and their clinical application. huOKT3γ1ala-ala was preceded by the mouse monoclonal antibody OKT3 (Ortho Biotech), the first anti-human CD3 monoclonal antibody, and the first monoclonal antibody licensed for clinical use. OKT3 was approved in 1985 for the prevention of acute rejection of major histocompatibility complex (MHC)-mismatched renal allografts, and later it was shown to be useful for the treatment of acute rejection of liver and cardiac allografts. However, OKT3 was lacking in appeal for the treatment of autoimmune disease for many of the same reasons that ultimately led to loss of popularity in transplantation. By virtue of its mouse amino acid sequences, OKT3 induced a vigorous humoral response in humans within 5–7 days after administration, which neutralized the antibody and promoted its clearance. Therefore, OKT3 could not be given repeatedly for the treatment of a chronic process, such as autoimmune disease. OKT3 also triggered a marked cytokine release reaction, owing to its potent mitogenic effects on T cells. These drawbacks were largely overcome in two ways. First, humanizing OKT3 greatly reduced its immunogenicity in vivo. Second, as the ability of CD3-specific antibodies to induce T-cell proliferation and cytokine production is closely tied to their cross-linking ability to bind to FcRs on monocyte/macrophages and natural killer cells (3, 4), the cytokine release reaction was diminished to an acceptable intensity by modifying the Fc region of the antibody to prevent FcR binding.
These changes did not destroy its therapeutic benefits. FcR-non-binding and FcR-binding CD3 antibodies are equivalent in their ability to prolong MHC-mismatched graft survival in animals as well as reverse type 1 diabetes in NOD mice. Initial clinical studies with huOKT3γ1ala-ala to prevent renal allograft rejection confirmed the efficacy of an FcR-non-binding CD3 antibody (5, 6), thereby paving the way for more recent developments in this field.
Three FcR-non-binding CD3-specific antibodies are currently under commercial development: 1. huOKT3γ1ala-ala (teplizumab, Macrogenics/Lilly) is a humanized version of OKT3 containing Fc region mutations at leu234→ala234 and leu235→ala235 (7–9). This FcR-non-binding CD3 antibody has been used in all of the ITN trials. The other non-FcR-binding CD3 monoclonal antibodies in advanced stages of development are otelixizumab (Tolerx/GlaxoSmithKline), also termed ChAglyCD3, and NI-0401 (NovImmune). These CD3-specific antibodies are also genetically engineered as humanized antibodies with minimal FcR-binding ability.
The development of CD3-specific antibodies for the treatment of type 1 diabetes has been reviewed by Chatenoud (10) and Chatenoud and Bluestone (11). To summarize these reviews, the binding of CD3-specific antibodies to T cells has several effects that may account for its tolerance-inducing properties in vivo. Both the FcR-binding and non-binding CD3-specific antibodies have been shown to modulate cell-surface expression of the T-cell receptor (TCR)-CD3 complex (12). In mice, FcR-non-binding CD3 antibodies have been shown to induce functional anergy of T cells, preferentially of activated T cells, as opposed to naive T cells. They do so by delivering a partial agonist signal to the TCR, leading to a reduction in Th1 cells and a boost in Th2 cells (13, 14). This effect is partially blocked by cyclosporine A, consistent with its dependence on an intracellular calcium signal (13). Compared with FcR-binding antibodies, FcR-non-binding antibodies induce similar levels of phosphorylation of CD3ε and p21δ, but less phosphorylation of p23δ and ZAP-70 kinase, with minimal phosphorylation of Cγ1 (14). Work also done in mice shows that administration of FcR-non-binding CD3-specific antibody preserves CD4+ T-regulatory cells, which in NOD mice are found to be more numerous in the pancreatic and mesenteric lymph nodes in the first two weeks of treatment (15). Therefore, non-FcR-binding CD3-specific antibody therapy appears to restore immune tolerance in NOD mice by shifting the balance of effector T cells from a Th1 to a Th2 bias and by inducing CD4+ T-regulatory cells.
In 2002, Herold, Bluestone, and colleagues (16) published their first study of huOKT3γ1ala-ala (teplizumab) for the treatment of new onset type 1 diabetes, which set the stage for the ITN-developed trials. In the first part of this study, 24 eligible patients with type 1 diabetes between the ages of 7½ and 30 years within six weeks of their diagnosis were randomly allocated to receive treatment with a 14-day course of huOKT3γala-ala or usual care. The dosing schedule was derived from the regimen previously used successfully for the prevention of acute renal allograft rejection (5). The antibody was administered intravenously as follows: 1.42 µg/kg of body weight on day 1, 5.67 µg/kg day 2, 11.3 µg/kg on day 3, 22.6 µg/kg on day 4, and 45.4 µg/kg on days 5 through 14. With this dosing regimen, coating of T cells by the anti-CD3 antibody reached 69.2 ± 2.9% at day 12, with peak modulation of the TCR-CD3 complex of 54 ± 3.1% at day 14. After treatment of the first 12 subjects, an additional eight subjects with type 1 diabetes received a modified dosing regimen to increase coating and modulation of the CD3 molecule (17). For this second group, the patients received 450 µg/m2 on day 1, 919 µg/m2 on day 2, and 1,818 µg/m2 on days 3–12. In these subjects with recent-onset type 1 diabetes, the anti-CD3 antibody therapy significantly reduced the loss of stimulated c-peptide measured at 12 months compared with the control arm (16), indicating preservation of residual β cell function. While these benefits were sustained up to 2 years, waning of the c-peptide maintenance after the first year suggested that future studies should consider repeated courses of therapy (18) or addition of synergistic tolerizing strategies. Similar results were obtained in a randomized, placebo-controlled trial involving 80 subjects with new onset type 1 diabetes, in which treatment with another CD3-specific antibody, ChAgylCD3, was also associated with improved maintenance of C-peptide responses for a limited amount of time (19).
Immune monitoring of subjects in these trials did not identify a definitive mechanism responsible for these clinical effects. Studies in vitro and in vivo suggest that huOKT3γ1la-ala has the ability to activate at least some T cells and trigger a mild-to-moderate cytokine release reaction. This reaction, which occurs after the first or second infusion, is characterized by fever, rash, flu-like symptoms, nausea, vomiting, myalgia, arthralgia, and headache. At the same time, there is a rise in the serum levels of tumor necrosis factor α (TNFα), interleukin-5 (IL-5), IL-6, and IL-10, but there is only a slight increase, if any, in serum levels of interferon γ (IFNγ) and IL-2 (17, 20). The outpouring of IL-5 and IL-10 in the absence of very little IFNγ and IL-2 is consistent with the downregulation of Th1 and upregulation of Th2 responses, as shown in mouse studies mentioned earlier (13, 14). The pattern of cytokine release in vivo parallels experiments in vitro, where huOKT3γ1ala-ala in the presence of anti-CD28 monoclonal antibody has been shown to stimulate human peripheral blood mononuclear cells (PBMCs) to produce much more IL-10 than IFNγ (17). This activation signal is associated in vitro with a rise in intracellular calcium and in vivo with an increase in the expression of the activation markers CD25 and CD69 (17).
Since two weeks of therapy led to more than a year of sustained clinical benefit, it is possible that CD3-specific antibodies are exerting their clinical effects by inducing T-cell regulatory mechanisms. T-cell depletion is probably not a significant outcome of CD3-specific antibody therapy, although some depleting effects cannot be completely excluded. It was reported from the initial study in type 1 diabetes that the total circulating lymphocyte count after huOKT3γ1ala-ala therapy reached a nadir of 26.5 ± 9.0% of the baseline count on day 5, recovering by day 30 to reach 123 ± 52% of the pre-treatment levels (16). Originally, this finding was interpreted as a reflection of modest T-cell depletion, but it has been suggested subsequently that the rapid pace of recovery is more consistent with transient margination or trafficking of T cells (20). Interestingly, the clinical responses after treatment with huOKT3γ1ala-ala were found to be associated with a change in the ratio of CD4+ T cells to CD8+ T cells, with an increase in the number of CD8+ T cells predicting a greater likelihood of a maintained c-peptide response (16). Studies in vitro later showed that huOKT3γ1ala-ala induces the proliferation of CD8+ T cells but not CD4+ T cells (17). Moreover, huOKT3γ1ala-ala was found to induce a subset of CD8+CD25+FoxP3+ T cells in PBMC cultures, which was able to downregulate antigen-specific T-cell responses in a cell contact-dependent manner (17). It has also been shown in vitro that peripheral blood CD8+ T cells from four CD3 antibody-treated patients with type 1 diabetes expressed more than threefold higher levels of FoxP3 after drug treatment, as opposed to non-drug treated patients, in which FoxP3 expression changed little over time. This subpopulation of putative CD8+ regulatory T cells persisted up to 10 weeks after treatment.
With these results in hand, the ITN moved forward with its own randomized, controlled, open-label phase IIb trial of huOKT3γ1ala-ala in new onset type 1 diabetes, in which subjects were to receive a second and third course of drug (20). This study used the same dosing scheme as that given to the eight patients in the second part of the original phase II trial. After enrollment of the first six subjects, it became clear that the frequency and severity of side effects were greater in this trial compared with the earlier study. The study was halted at that point, and a biochemical analysis of the new drug lots used in the phase IIb study found a major change in potency due to a different filtering protocol during the antibody manufacturing procedure.
With this issue corrected, the ITN re-initiated a randomized, two-armed, open-label phase II trial using teplizumab, or huOKT3γala-ala, produced by Macrogenics. Enrollment is now complete for this study, in which 81 participants with new onset type 1 diabetes have been randomly assigned in a 2:1 fashion to receive teplizumab over a 14-day course. After a 12-month interval, eligible patients have received a second course of teplizumab (at month 13). The ITN plans to explore potential mechanisms of action in detail through studies using flow cytometry, measurement of serum autoantibodies, T-cell assays, and whole blood gene expression profiling. Future ITN strategies may focus on combining CD3-specific antibodies with antigen, as suggested by murine studies in which combining anti-CD3 antibodies with antigen has been shown to be more effective than anti-CD3 antibodies or antigen alone (21).
Autoimmune diseases are notable not only for T-cell involvement but also in many cases for a prominent association with autoantibodies. This observation led to the use of anti-B-cell therapeutics, particularly anti-CD20, which were originally developed as anti-B-cell lymphoma drugs but are now used increasingly in autoimmunity. Interestingly, short-term clinical efficacy has now been found for anti-CD20 therapy, even in disease traditionally thought to be T-cell mediated, such as multiple sclerosis and type 1 diabetes. The ITN has conducted a pivotal trial of anti-CD20 in patients with AAV, a debilitating but rare autoimmune disease conventionally treated with the chemotherapeutic drug cyclophosphamide, and has collaborated with NIDDK TrialNet in the conduct of a trial of anti-CD20 in newly diagnosed subjects with type 1 diabetes.
B cells received little attention as a therapeutic target for autoimmune disease until rituximab, a chimeric CD20-specific monoclonal antibody, was shown in the early part of the last decade to improve the signs and symptoms of rheumatoid arthritis (RA) (22). This finding catapulted B-cell-targeted therapy into the limelight and stimulated not only further investigation of rituximab therapy for several autoimmune diseases but also commercial development of other novel agents directed against B cells and their functions. The efficacy and safety of rituximab has now been confirmed for the treatment of RA, and it is approved for this indication. In addition, phase II randomized, placebo-controlled trials have provided evidence for clinical efficacy of rituximab therapy for a variety of indications, including multiple sclerosis (23), type 1 diabetes (24), and pemphigus vulgaris (25). In contrast, two phase II/III randomized, controlled trials of rituximab therapy for lupus nephritis (26) and non-renal lupus (27) failed to meet their primary clinical endpoints. Humanized CD20-specific antibodies, such as ocrelizumab and ofatumumab, have also been developed in an attempt to improve on this approach. Small modular immunopharmaceuticals (e.g. TRU-015), a CD20-related technology, are also in the drug pipeline. Other protein therapeutics directed against the B cell, namely epratuzumab (anti-CD22), belimumab (anti-BAFF), and atacicept (TACI-Fc), are being investigated for the treatment of systemic lupus erythematosus as well as several other indications (28).
The mechanisms by which rituximab improves the clinical manifestations of RA remain poorly understood, even today. It has been long considered that B cells contribute to the mechanisms of many autoimmune diseases through differentiation into short-lived and long-lived plasma cells producing pathogenic autoantibodies. Some autoantibodies display cytopathic properties, such as those to the acetylcholine receptor in myasthenia gravis, while others may form immune complexes that trigger host effector functions or deposit in tissues where they activate complement, and amplify the inflammatory response. Not all autoantibodies are necessarily pathogenic, as evidenced by their occurrence in some healthy individuals and a proportion of healthy siblings of patients with autoimmune disorders. Their appearance may also pre-date the onset of clinical manifestations of autoimmune disease, which is the case for anti-CCP and rheumatoid factor in RA, a multiplicity of autoantibodies in SLE, and anti-insulin, anti-glutamic acid decarboylase, and anti-islet cell antigens in type 1 diabetes. B cells also have several other functions that may play roles in the pathogenesis of autoimmune-mediated diseases, including antigen presentation to T cells, cytokine release, and organization of tertiary lymphoid tissue (28). For example, studies in mice have shown that depletion of B cells by anti-CD20 monoclonal antibodies can downregulate an adaptive immune response by impairing CD4+ T-cell activation (29). Human B cells also secrete pro-inflammatory cytokines, such as IL-6, TNFα, LTα, and IFNγ, in response to Toll-like receptor (TLR) stimulation, which may contribute to disease pathophysiology (30–32). A small subset of B-regulatory cells has also been characterized in mice, termed B10 cells, for their ability to secrete IL-10 (33–35). In mice with EAE, their preferential depletion during disease initiation enhanced EAE pathology (34). It appears that B10 cells are important in the control of disease initiation, while regulatory T cells are more important in inhibiting ongoing disease (34). Regulatory B cells have also been identified in humans with autoimmune disease, but their role in disease pathogenesis remains to be determined (36, 37). Finally, B cells participate in the formation of tertiary lymphoid structures at sites of disease in non-lymphoid organs, such as the synovial tissue in RA and the salivary gland in primary Sjögren’s syndrome. In a severe combined immunodeficiency (SCID) mouse model, ablation of B cells was associated with elimination of tertiary lymphoid tissue, highlighting the importance of B cells in the formation of these structures (38).
Preliminary observations from an open-label clinical study of refractory anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis suggested that rituximab was effective for the treatment of this condition (39;40). The two types of systemic vasculitis predominately associated with serum ANCA are Wegener’s granulomatosis (WG) and microscopic polyangiitis (MPA). ANCA represents a group of autoantibodies, mostly of the IgG isotype, directed against antigens in the cytoplasm of neutrophils and monocytes. The two most relevant target autoantigens are proteinase-3 (PR3) and myeloperoxidase (MPO), which produce cytoplasmic and perinuclear patterns, respectively, by immunofluorescence assays with neutrophils fixed on glass slides. Many studies have shown that MPO-ANCA is mainly targeted by autoantibodies from patients with MPA, while PR3-ANCA predominates in WG; however, these associations are not absolute, as exceptions to this rule are not uncommon. Elimination of ANCA has a therapeutic rationale because of the evidence implicating ANCA in the pathogenesis of WG and MPA (41).
The initial study of rituximab therapy for ANCA-positive systemic vasculitis focused on a study population that was either intolerant or resistant to cyclophosphamide therapy, the standard of care in this setting. Cyclophosphamide, while effective in inducing clinical remission, has been associated with serious toxicity, including hemorrhagic cystitis, leukopenia, serious infections, and malignancy. In addition, most patients with WG or MPA, following successful induction of clinical remission with cyclophosphamide combined with high doses of prednisone, require subsequent long-term treatment to maintain disease quiescence. Therefore, many patients with WG and MPA receive low doses of prednisone and adjunctive immunosuppressive agents, such as azathioprine or methotrexate, for many years and intermittent high doses of prednisone or retreatment with cyclophosphamide to control relapsing disease. As compared with cyclophosphamide, rituximab afforded the possibility of a less toxic therapy, although this hypothesis required further testing in a controlled setting. In the open-label trial of 11 patients with WG and PR3-ANCA, a regimen of rituximab, 375 mg/m2 weekly ×4, was associated with achievement of clinical remission, in all cases, and a substantial drop in ANCA titer (39). Eight of the 11 patients became ANCA negative in this trial, suggesting that this treatment approach might induce immune tolerance. These results were later confirmed in a prospective, open-label trial from the same group (42).
These observations led the ITN to embark on a randomized, double-blind, double-dummy, non-inferiority trial, comparing rituximab with oral cyclophosphamide therapy for ANCA-associated systemic vasculitis (43). To be eligible, subjects must have had active WG or MPA of the severity to warrant therapy with cyclophosphamide. Nine centers enrolled 197 eligible patients, who were randomly allocated to receive treatment with rituximab, 375 mg/m2 weekly × 4, or oral cyclophosphamide, 2 mg/kg/d. All of the subjects were initially treated with the same high doses of corticosteroids, followed by a subsequent taper until they were no longer taking any corticosteroids at month 5. Patients achieving clinical remission between months 3 and 6 were switched to azathioprine, 2 mg/kg/d (cyclophosphamide group), or placebo (rituximab group) for the duration of the study. Treatment failures during this induction phase of the study were switched to the other treatment arms. The primary endpoint was clinical remission, which was defined as a score of 0 on the Birmingham Vasculitis Activity Score for Wegener’s Granulomatosis (BVAS/WG) at 6 months. The study continued until the last patient in the study had returned for his/her 18-month visit. The results, which have been recently published, showed that 63 (64%) of the patients in the rituximab group reached the primary endpoint, as compared with 52 (53%) patients in the comparison group, which met the criterion for non-inferiority (p < 0.001). The rates of adverse events were not significantly different between the two treatment groups. Nearly all of the patients (94%) in the rituximab group showed a drop in peripheral blood CD19+ B cells to a level less than 10 cells/mm3. The study has now been completed through month 18, and further analysis of the clinical results is in progress.
This trial provides a wealth of clinical data as well as samples for mechanistic assays to determine if rituximab therapy has indeed restored immune tolerance. These assays will include flow cytometric analysis of peripheral blood T-cell and B-cell subsets, microarrays for identification of whole blood mRNA signatures, ELISA for measurement of serum ANCA levels, ELISPOT for enumeration of ANCA-positive B cells, and multiplex assays for determination of cytokine and chemokine levels. It is possible that ANCA are largely the product of short-lived plasma cells, which appear to be more sensitive to rituximab-mediated B-cell depletion than long-lived plasma cells (29). In this case, rituximab may produce sustained decreases in serum ANCA titers, which may reduce the rate of relapse despite the absence of continued treatment with immunomodulatory agents. These studies will enable the ITN to examine in addition the effects of B-cell depletion on treatment response and its maintenance, as well as identify potential predictors of relapse that may herald a breakdown in immune tolerance. To this end, McKinney and colleagues (44) have recently identified a CD8+ T-cell signature in patients with active ANCA-associated vasculitis, connected with a higher likelihood of clinical relapse.
While anti-CD3 and anti-CD20 are broadly expressed on most T and B cells, respectively, an alternative set of target molecules are expressed on functionally distinct subclasses of cells or are expressed only after activation. This type of target includes the costimulatory molecules cytotoxic T-lymphocyte antigen 4 (CTLA4) and CD2, and several clinical trials are evaluating safety and efficacy of compounds designed to inhibit their function. CTLA4-Ig, known as abatacept, is now commonly used in treatment of RA, and the ITN has explored additional disease indications based on the premise that this soluble form of CTLA4 inhibits signaling to CD28 through CD80 and CD86, thereby blocking naive T-cell costimulation-dependent activation, and dampening some mature T-cell responses that are enhanced by a second signal received through CD28. The ITN is studying abatacept in multiple sclerosis and systemic lupus erythematosus, and is collaborating with NIDDK TrialNet on a similar trial in type 1 diabetes. A similar concept underlies the current ITN trial of alefacept, a soluble form of LFA3 that acts in part by inhibiting CD2-mediated costimulatory signals.
Chimerism
The goal of tolerance in transplantation is as elusive as it is in autoimmunity. Since the demonstration in 1953 of acquired tolerance to skin grafts by Billingham, Brent, and Medawar, probably the single most famous paper in transplantation immunology (45), many investigators have sought to develop strategies that would be clinically applicable and effective. One of the most promising has been the induction of hematopoietic chimerism. As first described by Ildstad and Sachs over 25 years ago (46), this manipulation involved lethal irradiation of mice and then reconstitution with allogeneic bone marrow. The hematopoietic system of the recipient, in essence, is completely replaced by that of the bone marrow donor, and thus recognizes donor organ and tissue transplants as ‘self’. As a result, donor allografts are tolerated indefinitely without immunosuppression, while third party grafts are rejected. To prevent the development of graft-versus-host disease, either rigorously T-cell-depleted bone marrow or purified stem cells are used.
Since this first description, two major conceptual refinements have occurred, which have facilitated translation to the clinic (reviewed in 47). First, recipients are now infused with a combination of donor and recipient bone marrow, resulting in so-called ‘mixed hematopoietic chimerism’, which is important for full immunocompetence. The rationale is that positive selection of T cells in the thymus occurs on MHC molecules expressed on thymic epithelial cells, i.e. the MHC molecules of the recipient. However, the MHC molecules that will present antigen in the periphery are those found on antigen-presenting cells (APCs), which will be derived from the donor bone marrow. Thus, in the case of a complete hematopoietic chimera, there will be a mismatch between the MHC molecules that select immature T cells and the ones that present antigen to mature T cells, resulting in relative immune incompetence. This mismatch can be prevented by including recipient bone marrow in the transplant innoculum, which means that some APCs will express recipient MHC molecules.
To minimize toxicity, protocols are now lympho-ablative but non-myeloablative, which both spare significant numbers of stem cells in the recipients’ marrow and prevent prolonged periods of neutropenia. In fact, the use of these protocols enables the achievement of mixed chimerism without the need to re-infuse recipients’ bone marrow, as sufficient ‘space’ is created by a non-myeloablative conditioning regimen to enable donor cell engraftment.
Preclinical testing of this approach in mice indicated that mixed chimerism induced tolerance via clonal deletion and that this tolerant state was extremely stable and robust, enabling donor-specific acceptance of skin, the most immunogenic of the known allografts (48, 49). In mice, it was noted that maintenance of tolerance required sustained donor chimerism. If donor hematopoiesis was lost, tolerance was lost as well (reviewed in 50). When mixed chimerism was tested in a highly relevant and predictive non-human primate model (51), it was again shown to induce robust tolerance, an important achievement, since many approaches effective in rodents have not succeeded in primates. Interestingly, however, long-term tolerance in non-human primates was achieved, even though chimerism was only transient (51–53), perhaps indicating a role for regulatory T cells.
With this backdrop, the ITN has conducted two trials using chimerism to induce tolerance in renal transplantation. In the first trial, a single center study led by David Sachs, Megan Sykes, and Ben Cosimi (Massachusetts General Hospital), five patients received kidney allografts from living, related donors matched for one HLA haplotype, and the first three received an induction regimen consisting of thymic irradiation, cyclophosphamide, and anti-CD2 monoclonal antibody, followed by maintenance cyclosporine (54). After the occurrence of acute antibody-mediated rejection in the third patient, the last two patients were given anti-CD20 monoclonal antibody during induction as well. One of the five patients lost his/her graft to irreversible rejection. However, the other four discontinued all immunosuppressive drugs 9–14 months after transplantation, and they have remained stable for 4–7 years after transplantation with excellent renal function. Consistent with non-human primate studies, multi-lineage chimerism was detected in all patients at an early time point (7 days) but rapidly was lost (by day 21). Encouraged by these positive results, albeit in small numbers of patients, the ITN has begun a follow-up trial with a goal of enrolling 15 additional patients in three centers, utilizing the same protocol but expanding it to allow both full HLA-matched and full HLA-mismatched donors.
Whether this approach can be adopted more generally remains to be seen. To date, it has only been carried out at a single center, and the degree of expertise required may make it difficult to adopt widely. Other concerns include potential morbidity of the conditioning regimen (particularly neutropenia and the associated risk of infection), and what the true incidence of rejection and graft loss will be once greater numbers of patients have been transplanted. With current, standard immunotherapy, acute rejection is very uncommon, and one-year graft survival in patients, such as those transplanted in this trial, would approach 95%, a high standard! On the other hand, many patients may be willing to concede a lower rate of early graft survival for the prospect of being immunosuppression free and the possibility of improved long-term graft survival, which many expect will accompany true tolerance.
The ITN continues to be interested in other ways to induce chimerism, in particular, if logistically simpler (e.g. no irradiation of the recipient) and/or induce longer and/or higher levels of chimerism. With respect to the degree of chimerism, a recent study by Tisdale and colleagues (55) is of particular note. These investigators performed a pilot study of HLA-identical patients (family donors, ages 16–45) with bone marrow transplantation for severe sickle cell disease. A non-myeloablative induction regimen was used consisting of alemtuzumab, sirolimus, and total body irradiation (300 cGy). Remarkably high levels of chimerism were achieved, with a mean percentage of donor-derived T cells of 53.3 ± 8.6% and donor myeloid cells of 83.3 ± 10.3% in the circulation at 30 months after transplantation. While it is currently not proven, it stands to reason that sustained high levels of chimerism would be beneficial for donor-specific tolerance, thus making this an attractive protocol for transplantation. Also not known is whether unique aspects of this protocol were important for this level of chimerism. Most notably, of course, would be the use of HLA-identical, donor-recipient combinations. The Tisdale group is currently performing a follow-up study using one haplotype-matched, donor-recipient pairs, and results of this patient population should address that issue. It also is possible that unknown features of the hematopoietic compartment or bone marrow microenvironment in patients with severe sickle cell disease may promote donor marrow engraftment, either directly or by giving it a competitive advantage over recipient cells.
Even if a safe and reliable, tolerance-inducing mixed chimerism protocol is developed, there still remains the problem that these approaches are currently only practical with live donors, and roughly 60% of kidney transplants performed in the United States use deceased donors. The requirement for live donors is based on the need for G-CSF-induced mobilization of donor stem cells, a 5–6 day process before leukapheresis. Extension of mixed chimerism to recipients of deceased donor organs will require a means to obtain sufficient stem cells within the same rapid time frame of organ procurement (typically several hours).
Antigen-directed immunomodulation
Antigen desensitization is an established approach when used in allergy therapy, where it represents a clinically validated proof-of-concept for the use of antigen-targeted immunomodulation in lieu of generalized immunosuppression. Extension of this strategy to achieve long-standing immune tolerance within the ITN portfolio takes two main directions: first, to improve antigen-specific allergen desensitization to make it safer, faster, and more durable; and secondly, to learn from the allergen experience to improve antigen-specific therapeutics in the areas of autoimmune diseases and transplantation.
In a series of clinical trials and parallel mechanistic studies, the concept of augmenting antigen-specific desensitization was evaluated, testing different options for immune intervention. One of the first ITN clinical trials to be completed evaluated the addition of anti-IgE to allergen extract administration, a study led by Thomas Casale, published in 2006 (56). This double-blind, placebo-controlled trial was conducted in 123 patients with at least a two-year history of ragweed allergy, comparing omalizumab (anti-IgE) with placebo in combination with allergen immunotherapy. The major findings of this study showed that fewer moderate and severe adverse reactions to allergen immunotherapy were present in groups receiving omalizumab. In particular, anaphylaxis risk was fivefold less in the group receiving omalizumab.
The patients recorded their symptom severity scores twice a day during 12 weeks of treatment in the allergy season, and the study also measured serum levels of allergen-specific IgG and IgE via ELISA. The results showed a 10-fold increase in specific IgG compared with baseline in the blood of patients treated with both omalizumab and immunotherapy, similar to the immunotherapy-only group, indicating that omalizumab did not interfere with the predicted induction of IgG by immunotherapy. The daily allergy severity scores were lower in the group receiving both immunotherapy and omalizumab than all other groups as well. Since induction of IgG4 is thought to be a primary mechanism underlying allergen desensitization, a follow-up study evaluated the ability of IgG4 from subjects to compete with IgE and inhibit the binding and presentation of the allergen-IgE complex (57). The total IgE-allergen complexes bound to B cells were measured via cell staining with anti-IgE FITC antibody. The results showed a significant decrease of binding in the group receiving immunotherapy only, no decrease in the placebo group, and complete inhibition of binding in groups receiving omalizumab. The latter sustained response after cessation of allergen administration suggests the possibility of induction of a tolerogenic response, but whether this is due to specific IgG4 directly or whether the persistent inhibition of allergen-IgE complexes binding to APCs caused a sustained downregulation of the Th2 response, resulting in decreased local allergen-specific IgE production, or yet another mechanism remains to be clarified.
A more direct test of the immune deviation concept for augmenting allergen desensitization was evaluated in an ITN trial led by Peter Creticos, which explored the concept of enhancing immune deviation as a tolerogenic approach (58). In this trial, subjects received a ragweed antigen, Amp a 1, coupled to DNA with a CpG motif designed to bind to TLR9. Signaling through TLR9, expressed in plasmacytoid dendritic cells, was intended to deviate antigen-specific T-cell responses and potentially inhibit the Th2 responses associated with active allergy. Fifteen subjects with seasonal ragweed allergy were enrolled in this randomized, double-blind, placebo-controlled trial, and the primary outcome measures associated with clinical symptoms were significantly improved in the active treatment group. Symptomatic indices maintained improvement after ragweed season, even though no further treatment was given, and less relief medication was needed. Although a number of cytokine and transcription profiling assays were performed in this study, no clear mechanism was confirmed, and there did not appear to be increased allergen-specific IgG.
This question of the relationship between cytokine deviation and allergen-specific IgG was also addressed by a study led by Stephen Durham and Steven Till investigating the role that IL-10 plays in allergen desensitization (59). Eighteen study participants received 12 months of grass pollen immunotherapy or placebo in a double-blinded and randomized study, and cytokines, antibodies, and intradermal allergen challenge were evaluated. As expected, serum levels of allergen-specific IgG4 and IgA were higher in the immunotherapy group, and this correlated with increased IL-10 production by PBMCs stimulated with grass antigen, particularly early in treatment. If there is a direct causal link between an early rise in IL-10 with allergen immunotherapy and subsequent IgG4 production with the development of tolerance, then such a response pattern could help in the design of therapies that specifically augment this proposed mechanism.
The above trials represent a key experimental strategy relevant to many different types of antigen-specific tolerization, in which antigen is presented in a context that will elicit a non-pathogenic response, while at the same time fostering a regulated immune response that will be dominant and durable. Deviation of a predominant Th2 response to a Th1-type response is somewhat unique to allergy, but other approaches, such as eliciting an IL-10 TR1-type response, are more generalizable to other immune-mediated disorders. Efforts to boost tolerance through TR1 and other regulatory T-cell pathways, such as natural Tregs, have also been a part of the ITN approach focused on autoimmune diseases. However, one key difference from the allergy trials is that in autoimmune diseases there are multiple autoantigenic targets of the immune response. Although we know a large number of tissue proteins that are recognized as autoantigens, it is not yet clear whether induced antigen-specific regulation needs to be targeted to specific dominant proteins or whether regulation directed to one protein will successfully modulate responses to all.
For example, in the commonly used animal model of type 1 diabetes, the non-obese diabetic (NOD) mouse, multiple autoantigens are targeted during the progression of the immune destruction of islet cells. Immunomodulation or genetic manipulation that tolerizes the animal to a single autoantigen can successfully prevent diabetes, and this tolerization prevents sensitization to additional islet antigens (60, 61). A very similar sequence of events occurs in an induced murine model of autoimmune encephalomyelitis, in that tolerization to the initiating autoantigen prevents the spreading of autoimmune targeting to other myelin-associated autoantigens and blocks progression of disease (62). In the hope that these animal models would recapitulate some of the key features of human autoimmunity, the ITN evaluated an insulin ‘vaccination’ protocol, which had shown efficacy in the NOD model. In this trial, led by Tihamer Orban, metabolically inactive insulin B-chain fragment was administered with incomplete Freund’s adjuvant to 12 subjects in a double-blind, randomized, 1:1 placebo-controlled clinical trial focused on evaluation of safety and mechanistic studies (63).
While both groups of subjects showed increased insulin-specific autoantibodies during the trial, the increase was much higher in the vaccine groups, indicating a specific humoral response to insulin. No differences were found between the groups for other diabetes-associated autoantibodies. This humoral response peaked at three months but reverted to the level of the placebo group by one year. In contrast, T-cell proliferation measured by antigen stimulation also markedly increased, peaked at six months, and remained positive throughout the study. Invariant natural killer T (iNKT) cell frequency was measured by flow cytometry and found to be increased in the vaccine group. Since the immune sensitization seen in this trial elicited biomarkers associated with pathogenic responses, such as robust T-cell proliferation and autoantibodies, any follow-up studies will need to focus on a more directed regulatory phenotype. Nevertheless, the trial demonstrated that modulation of established immune responses to autoantigens, such as insulin, is readily achieved in a clinical trial setting, bringing autoimmune diseases, such as type 1 diabetes, conceptually closer to the approach currently taken in allergy trials.
Two innovative strategies that combine regulatory signaling with antigen delivery are currently under development in the ITN portfolio. The first, based on the work of Andrew Saxon, is designed to present allergen in a desensitization protocol, co-administered with signaling through inhibitory Fc receptors (64). The second, based on the work of Steven Miller and others, is to present autoantigens, co-presented with apoptotic syngeneic cells, designed for uptake into normal, regulated scavenger pathways that may lead to tolerogenic antigen presentation (65), an approach currently in a phase I study in Germany led by Roland Martin (66). These types of antigen delivery are challenging, due to the potential for enhancing, rather than reducing, pro-inflammatory immunity associated with disease exacerbations and uncertainties regarding the appropriate autoantigenic proteins or peptides. A cautious approach is required, but recent advances in measuring regulatory T cells will be very helpful for designing the next generation of trials informed by biomarkers of regulated phenotypes.
Administration of antigen requires some thoughtful consideration of the patient population and disease process under study. Different conditions are required to elicit an immune response dominated by a particular type of T cell (e.g. Th1, Th2, Th17, TR1, or Treg) when considering a naive T-cell population or one that is already committed to a particular differentiation pathway, and this has several important implications for trial design. First, in a relapsing-remitting autoimmune disease, the cytokine and tissue microenvironment during antigen dosing is likely to be quite different during the remission phase compared with the relapse phase, and on theoretical grounds it could very well lead to different outcomes. For example, the presence of proinflammatory cytokines, such as IL-1 or IL-6, is predicted to bias naive responses to antigen toward a Th17 lineage, away from a Treg program. Second, effector memory autoreactive T cells are relatively refractory to deletion or regulation (67–69) and may require directed therapy prior to administration of antigen. This has recently been found in the context of type 1 diabetes, in patients who had recurrence of their autoimmune disease after pancreas transplantation, with expansion of the pre-existing memory autoreactive T-cell population. Third, some forms of regulatory T cells are known to display an ability to be reprogrammed into effector cells, a phenotype known as ‘plasticity’ (70, 71), or to lose the epigenetic markers associated with persistent FOXP3 expression (72). Thus, administration of regulatory T cells in vivo may require simultaneous management of the recipient environment to assure maintenance of regulatory function.
These concerns have led the ITN toward several new strategies for combining antigen tolerization with additional systemic therapies. For example, dampening pro-inflammatory cytokine environments may be a useful adjunct therapeutic for most types of tolerance induction. Current prospects for consideration include the anti-IL-1 and anti-IL-6R antagonists or antibodies already in clinical use, or a ‘re-purposing’ of an established drug, such as α-1 antitrypsin. The latter is now being evaluated as a monotherapy in an ITN trial in a type 1 diabetes population. Additional combination therapeutics are also under consideration, including the use of monoclonal antibodies that may target the effector T-cell populations (e.g. alefacept, alemtuzimab) or the use of antigen delivery technologies that preferentially invoke presentation by regulatory or tolerogenic DC populations. Another example involves the direct stimulation of a Treg population, through expansion either in vitro or in vivo. In vitro expansion, followed by syngeneic adoptive transfer, represents a form of cell-based therapy currently being evaluated in the context of graft versus host disease (ClinicalTrials.gov Identifier NCT00725062). The ITN, in partnership with the Juvenile Diabetes Research Foundation, will conduct a similar study in the context of type 1 diabetes patients. This trial follows on the heels of a current ITN phase I study of in vivo Treg expansion, in which IL-2 is combined with rapamycin, a potent stimulator of natural Treg lineages in prior animal studies (73). Whether either of these Treg expansion strategies can be adapted successfully to antigen-specific T-cell populations poses a technical challenge, although precedent for detection of the rare antigen-specific Treg cells in peripheral blood has been reported (74;75).
Biomarker discovery
The ITN is important for its dual mandate, not only to conduct clinical trials of new therapies aimed at producing stable, long-term immune tolerance, but also to explore the underlying mechanisms of tolerance induction, including biomarker discovery and validation. Biomarkers of disease activity and/or therapeutic success are valuable for at least two reasons. First, they may give important insights into the underlying biological mechanisms of the primary disease, which can, in turn, lead to new treatment strategies. Of course, biomarkers may not be causally related to a disease but may simply reflect an association (i.e. a marker). However, even the latter markers can be extraordinarily useful by enabling one to predict which group(s) of patients are appropriate for what type of therapy or providing a surrogate endpoint for a clinical trial, which otherwise might take years to reach its conclusion.
There is an official NIH definition of the term biomarker: ‘a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacological responses to therapeutic intervention’ (76). Therefore, many indicators are potential biomarkers; however, most that have been studied to date in the context of immune-mediated illnesses have poor predictive accuracy. For example, in the case of renal transplantation, serum creatinine, a measure of renal function, could be considered a biomarker of the immune response (or lack thereof) to the transplant. It provides no insight into mechanisms of rejection or tolerance, and, similarly, has little to no predictive accuracy for the future status of a patient.
All ITN-conducted trials include mechanistic assays aimed at biomarker discovery/validation. The ITN also has been actively engaged in non-interventional biomarker discovery studies, most prominently in transplantation.
Renal transplantation
The kidney is by far the most commonly transplanted organ, and virtually all patients are maintained on lifelong immunosuppression to prevent graft rejection. Sometimes, however, because of either medical non-compliance or life threatening complications of immunosuppression (e.g. severe opportunistic infections), patients discontinue their medications. In the vast majority of instances, this action leads to graft rejection, but occasionally, albeit rarely, patients retain stable transplant function and are said to be tolerant.
In an effort to define biomarkers of tolerance in renal transplantation, the ITN recently conducted a registry study led by Kenneth Newell, in which tolerant patients were identified, and analysis was performed on their PBMC phenotype and gene expression patterns in comparison with stable patients maintained on immunosuppressive drugs and healthy controls (77). Such studies have been attempted in the past; however, limitations in patient numbers have significantly hampered the ability to perform statistically meaningful analyses.
The 25 tolerant patients in the ITN study represent the largest single series ever reported and enabled us to divide the group into a training set and a validation (test) set. This study found that PBMCs from tolerant patients, compared with stable patients on standard immunosuppression, exhibited a B-cell signature characterized by increased numbers of total B cells, naive B cells, and transitional B cells. Over 30 genes were found to be overexpressed in the blood of tolerant recipients (again compared with patients on immunosuppression), and the majority of these were B-cell-associated transcripts. By analyzing a training set of 19 tolerant patients, plus 24 drug-treated recipients, we found that the expression of three B-cell genes alone, IGKV4-1, IGLL1, and IGKV1D-13, was sufficient to discriminate between tolerant and non-tolerant (i.e. still on immunosuppression) recipients. This finding was further validated in a test set of 12 patients (six tolerant, six on immunosuppression), where all of the tolerant patients were accurately predicted, as were five of the six still on medication. The core findings of a B-cell tolerance signature were confirmed in a concurrent study by a European group of investigators in an independently gathered cohort of patients (78), and elevated circulating B cells and CD20 transcripts had previously been noted in a smaller study as well (79).
No significant gene expression differences were found between tolerant patients and healthy controls, suggesting that tolerance may look similar to ‘health’. Thus, it is possible that the ITN signature is a marker for drug therapy, rather than a specific tolerant state per se. Of note, however, four of the 30 patients on drug therapy had the ‘tolerance signature’. While this may merely indicate a lack of specificity for the transcript analysis, a more optimistic interpretation is that a sizable minority of patients on drug therapy may be tolerant. The ITN has just started a follow-up study to determine the prevalence (and stability over time) of the tolerance signature in 250 stable renal allograft recipients (1–3 years post-transplantation). If the signature is found in an appreciable percentage and is consistent over time, it may form the basis for a future drug withdrawal trial.
Liver transplantation
Liver transplantation is an extremely attractive setting for discovery and validation of transplantation biomarkers. Liver transplant rejection is relatively easy to arrest, and, importantly, the liver has substantial regenerative capacity, unique among commonly transplanted organs. This means that drug withdrawal trials to validate defined signatures are relatively safer to conduct in liver transplant patients than in recipients of other organs.
These attractive features have spawned a number of studies. One of the most prominent was reported by Sánchez-Fueyo and colleagues in Barcelona (80). Studying 17 tolerant and 21 drug-treated liver transplant recipients, they developed a peripheral blood gene expression signature associated with tolerance, which was validated in a test set of 11 tolerant and 12 non-tolerant recipients. Interestingly, this signature was characterized by genes preferentially expressed in NK, NKT, and γδ T cells, thus differing significantly from the one found in the renal transplantation studies, suggesting that all ‘tolerance’ may not look alike, varying perhaps with disease, organ, etc.
Based in part on these interesting results, a number of studies are either ongoing or in development. The Barcelona group is conducting supervised drug withdrawal to investigate whether patients who are successfully weaned are more likely to have the signature than those who are drug dependent. Future studies are likely to include presence or absence of the signature as a primary inclusion/exclusion criterion for drug withdrawal, although randomization has been considered as well. The ITN is collaborating with this group in a related study to determine if, in liver transplant recipients identified as non-tolerant, discontinuation of calcineurin inhibitors, followed by six-month treatment with rapamycin, modifies the pattern of expression of the set of genes associated with tolerance.
A recently completed ITN pilot study in a selected group of 20 pediatric, living, related donor, liver transplant recipients, conducted by Sandy Feng (UCSF), has shown that over half of the patients could successfully undergo immunosuppresive drug discontinuation. While the size of the patient group was too small to allow validation of the Barcelona transcript biomarkers, let alone discovery of new ones, the clinical results are extremely encouraging and suggest that a larger study with appropriate statistical power is justified.
Open questions and future directions
While most will agree that gene expression profiling for biomarkers has tremendous potential, the field is still young. Among the most vexing questions are where to look and how to look. Where? Blood is obviously the compartment of choice to sample, but many different types of cells are present. How? Looking at gene expression in whole blood would seem to be the most appropriate in terms of not excluding an important cell population but also potentially the least sensitive, since the signal-to-noise ratio will be the lowest. Indeed, a recent study from Kenneth Smith’s group at Cambridge (44) reports a prognostically predictive transcriptional signature in CD8+ T cells of patients with vasculitis and lupus. This signature, however, was observed only when purified CD8+ T cells were studied and was not observed in unfractionated mononuclear cells. Clearly, assays that do not require cell fractionation are easier to perform and can be more widely adopted. Once target genes are identified, more directed and sensitive assays can be utilized, which do not require isolation of specific cell sub-populations.
The ‘how’ is probably as important as the ‘where’. Evolving technologies present a myriad of platforms for array-based and quantitative gene expression. While these approaches are increasingly sensitive and specific (as well as less expensive), biomarker profiles seen with one platform cannot assume to hold true on newer ones, unless they are revalidated, necessitating time, expense, and a set of ‘gold standard’ samples.
Achieving reconstitution of immune tolerance in clinical medicine is a daunting challenge, with complexities of multiple interacting immunological mechanisms overlaid on a background of variation in patterns of disease. A growing number of potential therapies provide a rich opportunity for matching selected interventions to appropriate patients, requiring new insights into clinical stratification through use of biomarkers. The ITN brings a strategic focus to this task, built upon the philosophy that diverse immune-mediated diseases, studied as a whole, will light the path toward immune tolerance.
Acknowledgements
We thank the many colleagues and collaborators who have assisted in ITN research studies over the last decade. The ITN is supported by the National Institutes of Health, National Institute of Allergy and Infectious Diseases, with additional support from National Institute of Diabetes and Digestive and Kidney Diseases and the Juvenile Diabetes Research Foundation.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Chatenoud L, Thervet E, Primo J, Bach JF. Anti-CD3 antibody induces long-term remission of overt autoimmunity in nonobese diabetic mice. Proc Natl Acad Sci USA. 1994;91:123–127. doi: 10.1073/pnas.91.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chatenoud L, Primo J, Bach JF. CD3 antibody-induced dominant self tolerance in overtly diabetic NOD mice. J Immunol. 1997;158:2947–2954. [PubMed] [Google Scholar]
- 3.Hirsch R, Gress RE, Pluznik DH, Eckhaus M, Bluestone JA. Effects of in vivo administration of anti-CD3 monoclonal antibody on T cell function in mice. II. In vivo activation of T cells. J Immunol. 1989;142:737–743. [PubMed] [Google Scholar]
- 4.Ferran C, et al. Anti-tumor necrosis factor modulates anti-CD3-triggered T cell cytokine gene expression in vivo. J Clin Invest. 1994;93:2189–2196. doi: 10.1172/JCI117215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Woodle ES, et al. Humanized, nonmitogenic OKT3 antibody, huOKT3 gamma(Ala-Ala): initial clinical experience. Transplant Proc. 1998;30:1369–1370. doi: 10.1016/s0041-1345(98)00278-4. [DOI] [PubMed] [Google Scholar]
- 6.Woodle ES, et al. Phase I trial of a humanized, Fc receptor nonbinding OKT3 antibody, huOKT3gamma1(Ala-Ala) in the treatment of acute renal allograft rejection. Transplantation. 1999;68:608–616. doi: 10.1097/00007890-199909150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Alegre ML, et al. Effect of a single amino acid mutation on the activating and immunosuppressive properties of a "humanized" OKT3 monoclonal antibody. J Immunol. 1992;148:3461–3468. [PubMed] [Google Scholar]
- 8.Alegre ML, et al. A non-activating "humanized" anti-CD3 monoclonal antibody retains immunosuppressive properties in vivo. Transplantation. 1994;57:1537–1543. [PubMed] [Google Scholar]
- 9.Woodle ES, et al. Humanized OKT3 antibodies: successful transfer of immune modulating properties and idiotype expression. J Immunol. 1992;148:2756–2763. [PubMed] [Google Scholar]
- 10.Chatenoud L. CD3-specific antibody-induced active tolerance: from bench to bedside. Nat Rev Immunol. 2003;3:123–132. doi: 10.1038/nri1000. [DOI] [PubMed] [Google Scholar]
- 11.Chatenoud L, Bluestone JA. CD3-specific antibodies: a portal to the treatment of autoimmunity. Nat Rev Immunol. 2007;7:622–632. doi: 10.1038/nri2134. [DOI] [PubMed] [Google Scholar]
- 12.Chatenoud L, Baudrihaye MF, Kreis H, Goldstein G, Schindler J, Bach JF. Human in vivo antigenic modulation induced by the anti-T cell OKT3 monoclonal antibody. Eur J Immunol. 1982;12:979–982. doi: 10.1002/eji.1830121116. [DOI] [PubMed] [Google Scholar]
- 13.Smith JA, Tso JY, Clark MR, Cole MS, Bluestone JA. Nonmitogenic anti-CD3 monoclonal antibodies deliver a partial T cell receptor signal and induce clonal anergy. J Exp Med. 1997;185:1413–1422. doi: 10.1084/jem.185.8.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith JA, Tang Q, Bluestone JA. Partial TCR signals delivered by FcR-nonbinding anti-CD3 monoclonal antibodies differentially regulate individual Th subsets. J Immunol. 1998;160:4841–4849. [PubMed] [Google Scholar]
- 15.Belghith M, Bluestone JA, Barriot S, Megret J, Bach JF, Chatenoud L. TGF-beta-dependent mechanisms mediate restoration of self-tolerance induced by antibodies to CD3 in overt autoimmune diabetes. Nat Med. 2003;9:1202–1208. doi: 10.1038/nm924. [DOI] [PubMed] [Google Scholar]
- 16.Herold KC, et al. Anti-CD3 monoclonal antibody in new-onset type 1 diabetes mellitus. N Engl J Med. 2002;346:1692–1698. doi: 10.1056/NEJMoa012864. [DOI] [PubMed] [Google Scholar]
- 17.Herold KC, Burton JB, Francois F, Poumian-Ruiz E, Glandt M, Bluestone JA. Activation of human T cells by FcR nonbinding anti-CD3 mAb, hOKT3gamma1(Ala-Ala) J Clin Invest. 2003;111:409–418. doi: 10.1172/JCI16090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herold KC, et al. A single course of anti-CD3 monoclonal antibody hOKT3gamma1(Ala-Ala) results in improvement in C-peptide responses and clinical parameters for at least 2 years after onset of type 1 diabetes. Diabetes. 2005;54:1763–1769. doi: 10.2337/diabetes.54.6.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keymeulen B, et al. Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. N Engl J Med. 2005;352:2598–2608. doi: 10.1056/NEJMoa043980. [DOI] [PubMed] [Google Scholar]
- 20.Herold KC, et al. Treatment of patients with new onset Type 1 diabetes with a single course of anti-CD3 mAb Teplizumab preserves insulin production for up to 5 years. Clin Immunol. 2009;132:166–173. doi: 10.1016/j.clim.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bresson D, et al. Anti-CD3 and nasal proinsulin combination therapy enhances remission from recent-onset autoimmune diabetes by inducing Tregs. J Clin Invest. 2006;116:1371–1381. doi: 10.1172/JCI27191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edwards JC, Szczepanski L, Szechinski J, Filipowicz-Sosnowska A, Emery P, Close DR, et al. Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med. 2004;350:2572–2581. doi: 10.1056/NEJMoa032534. [DOI] [PubMed] [Google Scholar]
- 23.Hauser SL, et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med. 2008;358:676–688. doi: 10.1056/NEJMoa0706383. [DOI] [PubMed] [Google Scholar]
- 24.Pescovitz MD, et al. Rituximab, B-lymphocyte depletion, and preservation of beta-cell function. N Engl J Med. 2009;361:2143–2152. doi: 10.1056/NEJMoa0904452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joly P, et al. A single cycle of rituximab for the treatment of severe pemphigus. N Engl J Med. 2007;357:545–552. doi: 10.1056/NEJMoa067752. [DOI] [PubMed] [Google Scholar]
- 26.Furie R, et al. Efficacy and safety of rituximab in subjects with active proliferative lupus nephritis (LN): results from the randomized, double-blind phase III LUNAR study; ACR/ARHP 2009 Annual Scientific Meeting; Philadelphia, PA. 2009. [Google Scholar]
- 27.Merrill JT, et al. Efficacy and safety of rituximab in moderately-to-severely active systemic lupus erythematosus: the randomized, double-blind, phase II/III systemic lupus erythematosus evaluation of rituximab trial. Arthritis Rheum. 2010;62:222–233. doi: 10.1002/art.27233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Townsend MJ, Monroe JG, Chan AC. B-cell targeted therapies in human autoimmune diseases: an updated perspective. Immunol Rev. 2010;237:264–283. doi: 10.1111/j.1600-065X.2010.00945.x. [DOI] [PubMed] [Google Scholar]
- 29.Bouaziz JD, et al. Therapeutic B cell depletion impairs adaptive and autoreactive CD4+ T cell activation in mice. Proc Natl Acad Sci USA. 2007;104:20878–20883. doi: 10.1073/pnas.0709205105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cognasse F, et al. Identification of two subpopulations of purified human blood B cells. Immunology. 2008;125:430–437. doi: 10.1111/j.1365-2567.2008.02844.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agrawal S, Aggarwal A, Dabadghao S, Naik S, Misra R. Compound heterozygosity of HLA-DR4 and DR1 antigens in Asian Indians increases the risk of extra-articular features in rheumatoid arthritis. Br J Rheumatol. 1995;34:41–44. doi: 10.1093/rheumatology/34.1.41. [DOI] [PubMed] [Google Scholar]
- 32.Bar-Or A, et al. Abnormal B-cell cytokine responses a trigger of T-cell-mediated disease in MS? Ann Neurol. 2010;67:452–461. doi: 10.1002/ana.21939. [DOI] [PubMed] [Google Scholar]
- 33.Matsushita T, Yanaba K, Bouaziz JD, Fujimoto M, Tedder TF. Regulatory B cells inhibit EAE initiation in mice while other B cells promote disease progression. J Clin Invest. 2008;118:3420–3430. doi: 10.1172/JCI36030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matsushita T, Horikawa M, Iwata Y, Tedder TF. Regulatory B cells (B10 cells) and regulatory T cells have independent roles in controlling experimental autoimmune encephalomyelitis initiation and late-phase immunopathogenesis. J Immunol. 2010;185:2240–2252. doi: 10.4049/jimmunol.1001307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Watanabe R, et al. Regulatory B cells (B10 cells) have a suppressive role in murine lupus: CD19 and B10 cell deficiency exacerbates systemic autoimmunity. J Immunol. 2010;184:4801–4809. doi: 10.4049/jimmunol.0902385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Blair PA, et al. CD19(+)CD24(hi)CD38(hi) B cells exhibit regulatory capacity in healthy individuals but are functionally impaired in systemic Lupus Erythematosus patients. Immunity. 2010;32:129–140. doi: 10.1016/j.immuni.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 37.Iwata Y, et al. Characterization of a rare IL-10-competent B-cell subset in man that parallels mouse regulatory B10 cells. Blood. 2010 doi: 10.1182/blood-2010-07-294249. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Takemura S, Klimiuk PA, Braun A, Goronzy JJ, Weyand CM. T cell activation in rheumatoid synovium is B cell dependent. J Immunol. 2001;167:4710–4718. doi: 10.4049/jimmunol.167.8.4710. [DOI] [PubMed] [Google Scholar]
- 39.Specks U, Fervenza FC, McDonald TJ, Hogan MC. Response of Wegener's granulomatosis to anti-CD20 chimeric monoclonal antibody therapy. Arthritis Rheum. 2001;44:2836–2840. doi: 10.1002/1529-0131(200112)44:12<2836::aid-art471>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 40.Keogh KA, Wylam ME, Stone JH, Specks U. Induction of remission by B lymphocyte depletion in eleven patients with refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2005;52:262–268. doi: 10.1002/art.20718. [DOI] [PubMed] [Google Scholar]
- 41.Gomez-Puerta JA, Bosch X. Anti-neutrophil cytoplasmic antibody pathogenesis in small-vessel vasculitis: an update. Am J Pathol. 2009;175:1790–1798. doi: 10.2353/ajpath.2009.090533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keogh KA, Ytterberg SR, Fervenza FC, Carlson KA, Schroeder DR, Specks U. Rituximab for refractory Wegener's granulomatosis: report of a prospective, open-label pilot trial. Am J Respir Crit Care Med. 2006;173:180–187. doi: 10.1164/rccm.200507-1144OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stone JH, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221–232. doi: 10.1056/NEJMoa0909905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McKinney EF, et al. A CD8+ T cell transcription signature predicts prognosis in autoimmune disease. Nat Med. 2010;16:586–591. doi: 10.1038/nm.2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Billingham RE, Brent L, Medawar PB. Actively acquired tolerance of foreign cells. Nature. 1953;172:603–606. doi: 10.1038/172603a0. [DOI] [PubMed] [Google Scholar]
- 46.Ildstad ST, Sachs DH. Reconstitution with syngeneic plus allogeneic or xenogeneic bone marrow leads to specific acceptance of allografts or xenografts. Nature. 1984;307:168–170. doi: 10.1038/307168a0. [DOI] [PubMed] [Google Scholar]
- 47.Sykes M. Mixed chimerism and transplant tolerance. Immunity. 2001;14:417–424. doi: 10.1016/s1074-7613(01)00122-4. [DOI] [PubMed] [Google Scholar]
- 48.Sharabi Y, Sachs DH. Mixed chimerism and permanent specific transplantation tolerance induced by a nonlethal preparative regimen. J Exp Med. 1989;169:493–502. doi: 10.1084/jem.169.2.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fuchimoto Y, et al. Mixed chimerism and tolerance without whole body irradiation in a large animal model. J Clin Invest. 2000;105:1779–1789. doi: 10.1172/JCI8721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wekerle T, Sykes M. Mixed chimerism as an approach for the induction of transplantation tolerance. Transplantation. 1999;68:459–467. doi: 10.1097/00007890-199908270-00001. [DOI] [PubMed] [Google Scholar]
- 51.Kawai T, et al. Mixed allogeneic chimerism and renal allograft tolerance in cynomolgus monkeys. Transplantation. 1995;59:256–262. [PubMed] [Google Scholar]
- 52.Kawai T, et al. Long-term outcome and alloantibody production in a non-myeloablative regimen for induction of renal allograft tolerance. Transplantation. 1999;68:1767–1775. doi: 10.1097/00007890-199912150-00022. [DOI] [PubMed] [Google Scholar]
- 53.Kawai T, et al. CD154 blockade for induction of mixed chimerism and prolonged renal allograft survival in nonhuman primates. Am J Transplant. 2004;4:1391–1398. doi: 10.1111/j.1600-6143.2004.00523.x. [DOI] [PubMed] [Google Scholar]
- 54.Kawai T, et al. HLA-mismatched renal transplantation without maintenance immunosuppression. N Engl J Med. 2008;358:353–361. doi: 10.1056/NEJMoa071074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hsieh MM, et al. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med. 2009;361:2309–2317. doi: 10.1056/NEJMoa0904971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Casale TB, et al. Omalizumab pretreatment decreases acute reactions after rush immunotherapy for ragweed-induced seasonal allergic rhinitis. J Allergy Clin Immunol. 2006;117:134–140. doi: 10.1016/j.jaci.2005.09.036. [DOI] [PubMed] [Google Scholar]
- 57.Klunker S, et al. Combination treatment with omalizumab and rush immunotherapy for ragweed-induced allergic rhinitis: Inhibition of IgE-facilitated allergen binding. J Allergy Clin Immunol. 2007;120:688–695. doi: 10.1016/j.jaci.2007.05.034. [DOI] [PubMed] [Google Scholar]
- 58.Creticos PS, et al. Immunotherapy with a ragweed-toll-like receptor 9 agonist vaccine for allergic rhinitis. N Engl J Med. 2006;355:1445–1455. doi: 10.1056/NEJMoa052916. [DOI] [PubMed] [Google Scholar]
- 59.Francis JN, et al. Grass pollen immunotherapy: IL-10 induction and suppression of late responses precedes IgG4 inhibitory antibody activity. J Allergy Clin Immunol. 2008;121:1120–1125. doi: 10.1016/j.jaci.2008.01.072. [DOI] [PubMed] [Google Scholar]
- 60.Nakayama M, et al. Prime role for an insulin epitope in the development of type 1 diabetes in NOD mice. Nature. 2005;435:220–223. doi: 10.1038/nature03523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tarbell KV, Yamazaki S, Olson K, Toy P, Steinman RM. CD25+ CD4+ T cells, expanded with dendritic cells presenting a single autoantigenic peptide, suppress autoimmune diabetes. J Exp Med. 2004;199:1467–1477. doi: 10.1084/jem.20040180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Smith CE, Miller SD. Multi-peptide coupled-cell tolerance ameliorates ongoing relapsing EAE associated with multiple pathogenic autoreactivities. J Autoimmun. 2006;27:218–231. doi: 10.1016/j.jaut.2006.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Orban T, et al. Autoantigen-specific regulatory T cells induced in patients with type 1 diabetes mellitus by insulin B-chain immunotherapy. J Autoimmun. 2010;34:408–415. doi: 10.1016/j.jaut.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang K, Zhu D, Kepley C, Terada T, Saxon A. Chimeric human fcgamma-allergen fusion proteins in the prevention of allergy. Immunol Allergy Clin North Am. 2007;27:93–103. doi: 10.1016/j.iac.2006.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Miller SD, Turley DM, Podojil JR. Antigen-specific tolerance strategies for the prevention and treatment of autoimmune disease. Nat Rev Immunol. 2007;7:665–677. doi: 10.1038/nri2153. [DOI] [PubMed] [Google Scholar]
- 66.Lutterotti A, Sospedra M, Martin R. Antigen-specific therapies in MS - Current concepts and novel approaches. J Neurol Sci. 2008;274:18–22. doi: 10.1016/j.jns.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 67.Laughlin E, Burke G, Pugliese A, Falk B, Nepom G. Recurrence of autoreactive antigen-specific CD4+ T cells in autoimmune diabetes after pancreas transplantation. Clin Immunol. 2008;128:23–30. doi: 10.1016/j.clim.2008.03.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schneider A, Rieck M, Sanda S, Pihoker C, Greenbaum C, Buckner JH. The effector T cells of diabetic subjects are resistant to regulation via CD4+ FOXP3+ regulatory T cells. J Immunol. 2008;181:7350–7355. doi: 10.4049/jimmunol.181.10.7350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vendrame F, et al. Recurrence of type 1 diabetes after simultaneous pancreas-kidney transplantation, despite immunosuppression, is associated with autoantibodies and pathogenic autoreactive CD4 T-cells. Diabetes. 2010;59:947–957. doi: 10.2337/db09-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hori S. Developmental plasticity of Foxp3(+) regulatory T cells. Curr Opin Immunol. 2010 doi: 10.1016/j.coi.2010.08.004. in press. [DOI] [PubMed] [Google Scholar]
- 71.Rubtsov YP, et al. Stability of the regulatory T cell lineage in vivo. Science. 2010;329:1667–1671. doi: 10.1126/science.1191996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lal G, Bromberg JS. Epigenetic mechanisms of regulation of Foxp3 expression. Blood. 2009;114:3727–3735. doi: 10.1182/blood-2009-05-219584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Battaglia M, Stabilini A, Migliavacca B, Horejs-Hoeck J, Kaupper T, Roncarolo MG. Rapamycin promotes expansion of functional CD4+CD25+FOXP3+ regulatory T cells of both healthy subjects and type 1 diabetic patients. J Immunol. 2006;177:8338–8347. doi: 10.4049/jimmunol.177.12.8338. [DOI] [PubMed] [Google Scholar]
- 74.Walker MR, Carson BD, Nepom GT, Ziegler SF, Buckner JH. De novo generation of antigen-specific CD4+CD25+ regulatory T cells from human CD4+ Proc Natl Acad Sci USA. 2005;102:4103–4108. doi: 10.1073/pnas.0407691102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Long SA, Walker MR, Rieck M, James E, Kwok WW, Sanda S, et al. Functional islet-specific Treg can be generated from CD4+ Eur J Immunol. 2009;39:612–620. doi: 10.1002/eji.200838819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- 77.Newell KA, et al. Identification of a B cell signature associated with renal transplant tolerance in humans. J Clin Invest. 2010;120:1836–1847. doi: 10.1172/JCI39933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sagoo P, et al. Development of a cross-platform biomarker signature to detect renal transplant tolerance in humans. J Clin Invest. 2010;120:1848–1861. doi: 10.1172/JCI39922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brouard S, et al. Identification of a peripheral blood transcriptional biomarker panel associated with operational renal allograft tolerance. Proc Natl Acad Sci USA. 2007;104:15448–15453. doi: 10.1073/pnas.0705834104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Martinez-Llordella M, et al. Using transcriptional profiling to develop a diagnostic test of operational tolerance in liver transplant recipients. J Clin Invest. 2008;118:2845–2857. doi: 10.1172/JCI35342. [DOI] [PMC free article] [PubMed] [Google Scholar]


