Abstract
Severe obesity (BMI ≥ 40 kg/m2) is associated with multiple defects in skeletal muscle which contribute to insulin resistance and a reduction in fatty acid oxidation (FAO) in this tissue. These metabolic derangements are retained in human skeletal muscle cells raised in culture. Together, these findings are indicative of a dysfunctional global metabolic program with severe obesity which is of an epigenetic or genetic origin. Weight loss via gastric bypass surgery can “turn off” and/or correct components of this metabolic program as insulin sensitivity is restored; however, the impairment in FAO in skeletal muscle remains evident. Physical activity can improve FAO and insulin action, indicating that this patient population is not exercise resistant and that exercise offers a pathway to circumvent the abnormal program. Findings presented in this review will hopefully increase the understanding of and aid in preventing and/or treating the severely obese condition.
1. Introduction
Our research group has been studying the intricacies of skeletal muscle metabolism in severely obese patients (BMI ≥ 40 kg/m2) for more than 25 years. These studies were initially possible due to collaborating surgeons providing abdominal muscle (rectus abdominus) biopsies taken during gastric bypass surgery which were then utilized in a muscle strip preparation to study carbohydrate and lipid metabolism. These in vitro incubation studies were complimented with experiments using needle biopsies of a leg muscle (vastus lateralis). Because of the substantial amount of information that we have accumulated, it seemed appropriate to describe and summarize the metabolic profile of the skeletal muscle of these patients and the effects of gastric bypass surgery.
We recently began to examine the characteristics of skeletal muscle cell cultures derived from biopsies obtained from lean and severely obese donors. To our surprise, the metabolic profile of myotubes raised in culture from severely obese individuals displayed the same phenotype as the intact muscle from which they were taken. This finding suggests that the metabolic profile of skeletal muscle observed in severely obese individuals is not solely due to the in vivo environment of the patient, but rather to a constitutive “obesity metabolic program” that is either genetically or epigenetically determined. We believe this represents a paradigm shift in our thinking about metabolic regulation in obesity. This review will focus on our studies that support the concept of a metabolic program in the skeletal muscle of severely obese individuals. Alternative hypotheses on the relationships between lipid oxidation, insulin action, and obesity can be examined in other papers on this topic [1–6].
2. The Metabolic Profile of the Skeletal Muscle of Severely Obese Individuals
2.1. Insulin Action
In the early 1980s we developed a human skeletal muscle strip preparation that was suitable for in vitro incubation experiments to study metabolism [7]. During elective abdominal surgery a biopsy of the rectus abdominus was clamped, excised, and “teased” into 12–20 muscle fiber strips. This preparation was exceptionally versatile as almost any radiolabeled substrate could be utilized in the incubation media to study metabolism and the effects of any hormone could be tested by incubation in its presence and absence.
The first published paper using this preparation [7] reported that glucose transport was stimulated approximately 2.5-fold by insulin in tissue from lean controls, but there was little or no stimulation of glucose transport in muscle from severely obese patients either with or without type 2 diabetes. We subsequently found that glucose transport in the muscle of severely obese patients, both diabetic and nondiabetic, was also resistant to the action of insulin-like growth factor-1 (IGF-1) [8]. Cumulative data from years of similar experiments indicated that for individuals with a BMI ≤ 20 kg/m2 glucose transport was stimulated by approximately 3-4 fold, but there was a progressive decline in insulin responsiveness to a BMI of about 30 kg/m2, after which there was virtually no insulin-induced stimulation [9].
Glucose transport was not the only parameter that demonstrated a reduced response to insulin. Insulin stimulation of glycogen formation, glucose oxidation, and nonoxidized glycolysis were all depressed in muscle of severely obese patients [10]. Interestingly, lactate release was not stimulated by insulin but basal (absence of insulin) lactate release was much higher in obese than nonobese controls suggesting a preferential utilization of carbohydrate rather than lipid as a fuel source.
To investigate the mechanism(s) of insulin resistance with severe obesity we addressed the question of whether a stimulus other than insulin could increase glucose transport in insulin-resistant muscle. In obese Zucker rats we demonstrated that muscle contraction stimulated glucose transport normally, even though there was severe insulin resistance [11]. We were not able to make the human muscle fiber strips contract but we did observe that hypoxia and vanadate, two stimuli that are believed to function through pathways also activated with muscle contraction, stimulated glucose transport normally in muscle strips from severely obese, insulin-resistant individuals [12, 13]. From these data we concluded that the mechanism for the translocation of the insulin-sensitive glucose transporter (GLUT4) was functional and the defect must be upstream and within the signaling pathway leading to insulin-mediated glucose transport. In support of this hypothesis, insulin stimulation of insulin receptor and IRS-1 tyrosine phosphorylation as well as activation of PI-3 kinase and Akt were all substantially reduced with severe obesity [14, 15]. The activities of protein-tyrosine phosphatases (PTPase 1B and LAR) [16], which would be predicted to impair insulin signal transduction, were also increased in muscle fiber strips of severely obese patients compared to nonobese controls.
Partially purified insulin receptors from muscle of severely obese subjects displayed tyrosine kinase activity that was lower than in nonobese controls [17]. We believe this is a result of hyperphosphorylation of serine residues on the insulin receptor, as phosphatase treatment substantially increased tyrosine kinase activity in receptors from the muscle of severely obese subjects [18, 19]. IRS-1 from muscle of severely obese patients was also hyper-phosphorylated, especially on serine 312 [20]. These changes in serine phosphorylation were accompanied by increased kinase activities of PKC and IKK [19, 20]. The involvement of PKC was also implicated by the finding that insulin resistance could be induced by a phorbol ester and insulin sensitivity restored in obese muscle with a PKC inhibitor [21]. Based on these findings our hypothesis is that several kinases are activated in the muscle of severely obese individuals with subsequent serine phosphorylation of the insulin receptor and IRS-1. These modifications depress insulin signal transduction and stimulation of glucose transport, glycogen synthesis, glucose oxidation, and nonoxidized glycolysis.
2.2. Fat Metabolism
Skeletal muscle plays a critical role in controlling whole-body fatty acid oxidation (FAO) due to its mass and metabolic characteristics. At rest FAO is the predominant activity of skeletal muscle [22]; thus any factor which would elicit a decrement in FAO in skeletal muscle could be anticipated to lead to the preferential partitioning of ingested lipid towards ectopic fat accumulation. As an example of FAO influencing body composition, subsequent weight gain was associated with a lower whole-body FAO as determined with indirect calorimetry [23]. A reduction in the activity of an enzyme in skeletal muscle involved with lipid metabolism (β-HAD) was associated with a reduced ability for whole-body FAO, indicating the potentially important role of the characteristics of this tissue in controlling body mass [24].
To test the hypothesis that a reduction in FAO in skeletal muscle is evident with obesity, we incubated muscle strips from the rectus abdominus with 14C-labeled palmitate and measured the production of labeled CO2 as the index of FAO [25]. To our surprise, FAO did not differ in the muscle of lean (BMI, 23.8 ± 0.6 kg/m2), and obese (30.2 ± 0.8 kg/m2) individuals but exhibited a significant reduction in the muscle of severely obese (BMI, 53.8 ± 0.4 kg/m2) subjects (−60% compared to lean controls) [25]. In a follow-up study, FAO was determined in needle biopsies from the vastus lateralis using a muscle homogenate preparation to measure labeled CO2; FAO was reduced by ~60% compared to lean controls in individuals approximating severe obesity (BMI, 38.3 ± 3.1 kg/m2) [26]. In a subsequent experiment we confirmed this reduction in FAO and found that the proportion of lipid that remained in the acid-soluble fraction (acid soluble metabolites, ASM), which is an index of incomplete oxidation, was elevated with severe obesity [27]. Together, these findings provide convincing evidence indicating a reduction in FAO in the skeletal muscle of severely obese individuals, as FAO was reduced in two separate muscle groups from different anatomical areas with markedly differing function and recruitment patterns (i.e., postural versus locomotion). This observation is critical as skeletal muscle is a heterogeneous tissue that can vary widely in respect to fiber composition, metabolic characteristics, and neural innervation.
Carnitine palmityoltransferase (CPT-1) regulates the transport of long-chain fatty acids across the mitochondrial membranes and is thus a key regulatory step for the control of FAO. The incubation of needle biopsy samples (vastus lateralis) with several species of fatty acids was utilized to determine if metabolic steps at either the level of CPT-1 or downstream were impaired with severe obesity [26]. The oxidation of palmitoyl carnitine, which enters the mitochondria independently of CPT-1, was depressed indicating that post-CPT-1 mechanisms in either β-oxidation and/or the TCA Cycle contribute to the reduction in FAO with severe obesity. In support of this observation citrate synthase, a TCA cycle enzyme and general indicator of mitochondrial content, was depressed in both the vastus lateralis and rectus abdominus of severely obese subjects [26]. However, CPT-1 activity was also reduced with severe obesity indicating a defect at this level in addition to downstream alterations [26]. Proteome analyses revealed increases in glycolytic enzymes (adenylate kinase, GAPDH, aldolase A, and creatine kinase activity) which was hypothesized to reflect a metabolic drift towards glycolytic energy production with the decrease in FAO in skeletal muscle with severe obesity [28]. This observation is supported by the increased generation of lactate under resting conditions that we have observed in the muscle strips [10]. These findings provide evidence for a metabolic program in the skeletal muscle of severely obese individuals where multiple steps are affected in a manner reflecting a decrement in FAO.
The observation of a reduction in FAO with severe obesity could also be attributed to a reduction in substrate availability, that is reduced fatty acid transport into the muscle of severely obese patients. However, long-chain fatty acid transport rates into giant sarcolemmal vesicles from the muscle of obese individuals were upregulated by ~4-fold compared to lean controls; this elevation in fatty acid transport with obesity was associated with an increased presence of the fatty acid transporter FAT/CD36 at the sarcolemma and an increase in intramuscular triacylglycerol content [29]. Our group has also reported increased intramuscular lipid content with severe obesity which was associated with a preferential partitioning of lipid towards storage rather than oxidation [30]. Such a scenario is metabolically disadvantageous as intramuscular lipid accumulation can be linked with insulin resistance [31]. In addition, intramuscular lipid comprises a relatively small reservoir for whole-body lipid storage as only 1–3% of total muscle area is occupied by lipid droplets [32, 33]. The reduction in FAO could potentially result in an overall partitioning of lipid away from anabolic/catabolic processes in skeletal muscle and towards deposition in adipose tissue which may explain the observation of weight gain in individuals with a depressed whole-body FAO [23].
We have also reported that the skeletal muscle of severely obese individuals, both diabetic and nondiabetic, is comprised of a lower relative percentage of type I muscle fibers (myosin ATPase staining) compared to lean controls [34, 35]. Type I, sometimes known as red, muscle fibers are characterized as being insulin-sensitive and geared towards oxidative metabolism compared to type II (white) muscle fibers; in support, insulin action in rectus abdominus strips was positively related to the relative percentage of type I muscle fibers [34]. This predominance of type II fibers with severe obesity is again suggestive of a general phenotype in the muscle of these patients which favors a low capacity for lipid oxidation and insulin resistance. However, we have observed that muscle fiber type is not altered in severely obese subjects in response to an intervention which improves insulin action such as gastric bypass/weight loss [20, 36, 37]. Such data indicates that contractile (i.e. fiber type) and metabolic characteristics may not always be congruent.
3. Metabolism in Cultured Myotubes from Severely Obese Individuals Is Similar to that in Intact Muscle
Following procedures originally described by Henry et al. [38] we developed methods for culturing cells from human muscle biopsy samples. Briefly, nascent satellite cells are released by trypsin treatment from the muscle and transferred to collagen-coated flasks which provide a matrix for subsequent attachment and proliferation into myoblasts [39]. Proliferation of the myoblasts continues in a serum-rich media in an incubated environment until confluence is obtained, which typically requires 4–6 weeks. Although metabolic studies can be performed in myoblasts, we have elected to examine myotubes as they more closely resemble mature skeletal muscle and express many of the genes that are characteristic of skeletal muscle in vivo [40]. In our experiments the metabolic characteristics of the myotubes are typically studied after 5–8 days of differentiation.
Human skeletal muscle cells (HSkMC) raised in culture offer a unique system for studying metabolism in relation to health and disease. The influence of potential acute adaptive factors such as neural input, hormonal concentrations, and physical activity level on metabolic characteristics in HSkMC are essentially removed due to the length and nature of the proliferation and differentiation phases [38, 41, 42]. Thus, it is believed that characteristics exhibited in HSkMC primarily reflect genetic or epigenetic traits. In addition, the experimental manipulations permitted in cell culture far exceed those possible in vivo. Our findings of remarkably similar metabolic characteristics between HSkMC and skeletal muscle examined in vivo or in vitro from severely obese donors offers an experimental system enabling a more in-depth study of potential mechanisms explaining the obesity-related phenotype.
3.1. Insulin Action
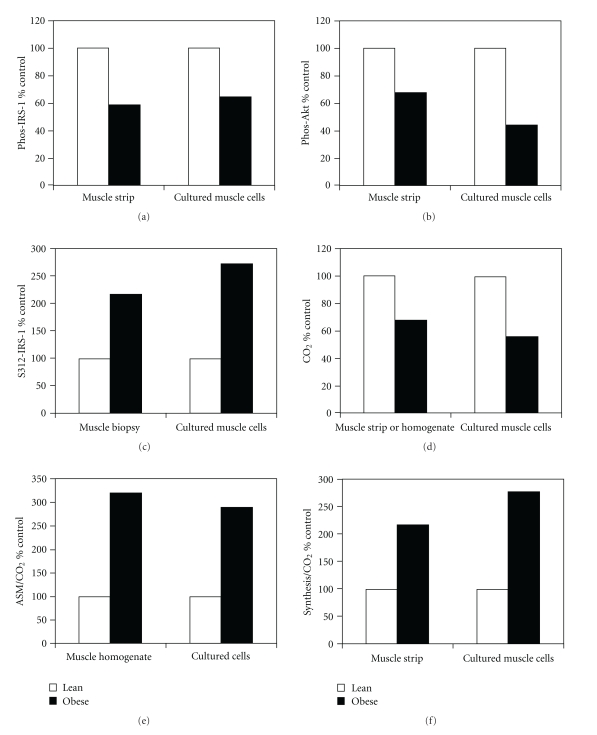
Henry et al. [38] were the first to report that HSkMC from patients with type 2 diabetes retained the insulin resistance exhibited in intact muscle. We extended this finding to obesity by demonstrating that insulin stimulation of IRS-1 tyrosine phosphorylation and Akt phosphorylation was significantly blunted in HSkMC from severely obese patients [43, 44]. In addition, serine 312 of IRS-1 was significantly more phosphorylated in myotubes from severely obese patients than lean controls. Figure 1 shows the comparison of our published data using the muscle strip preparation and HSkMC from lean and severely obese subjects. The degree of stimulation of IRS-1 tyrosine by insulin was approximately 60% in the severely obese muscle compared to lean controls and was essentially reproduced in HSkMC. The degree of blunting of Akt activation and serine 312 IRS-1 phosphorylation were even greater in HSkMC than observed in intact muscle (Figure 1). These data suggest that there are constitutive changes in insulin signaling in the skeletal muscle of severely obese patients that are retained in human skeletal muscle cells raised in culture.
Figure 1.
Comparison of insulin signal transduction and fatty acid oxidation in intact skeletal muscle and human skeletal muscle cells raised in culture (HSkMC) from lean and severely obese donors. Data in the graphs were calculated from mean values in the cited papers and nonobese control values used as 100%. (a) Insulin-stimulated tyrosine phosphorylation of IRS-1 (Phos-IRS-1) [14, 43, 44]. (b) Insulin-stimulated Akt phosporylation (Phos-Akt) [15, 43, 44]. (c) IRS-1 serine 312 phosphorylation (S312-IRS-1) [20, 43, 44]. (d) Complete fatty acid oxidation as determined from labeled CO2 production from 14C labeled palmitate (CO2) [25, 27, 43, 45]. (e) Incomplete fatty acid oxidation from calculating the 14C from labeled palmitate remaining in the acid soluble metabolite fraction divided by labeled CO2 production (ASM/CO2) [27, 43, 45]. (f) Partitioning between lipid synthesis and fatty acid oxidation (synthesis/CO2) [25, 30, 43, 45].
3.2. Fat Metabolism
As already presented in this review, FAO in the skeletal muscle of severely obese individuals is consistently reduced, which likely contributes to the preferential partitioning of lipid towards storage. As presented in Figure 1, the relative magnitude of the reduction in complete (labeled CO2 production) and increase in incomplete (ASM/CO2) FAO are virtually identical in HSkMC compared to intact muscle strips or muscle homogenates [27, 30, 43, 45]. This reduction in FAO does not appear to be due to a reduction in fatty acid uptake as we have reported elevated fatty acid transport into HSkMC from severely obese individuals [43]. Indices of lipid partitioning towards storage are also similar and may even be slightly elevated in HSkMC [27, 30, 43, 45]. These findings indicate that the metabolic signature evident in the skeletal muscle of severely obese individuals in relation to lipid metabolism is essentially retained in HSkMC (Figure 1) and perhaps of a genetic or epigenetic origin.
Gene array and subsequent PCR analyses indicated a 2-fold elevation in stearoyl-CoA desaturase-1 (SCD-1) mRNA in skeletal muscle biopsies from severely obese individuals; this difference was retained in HSkMC [30]. SCD-1 is a lipogenic enzyme which preferentially directs palmitoyl-CoA (C16:0) and stearoyl-CoA (C18:0) towards the synthesis of triacylglycerol, phospholipid, and cholesterol esters within the cell. In knockout mouse models, the absence of SCD-1 protected the animals against both diet-induced and genetic forms of obesity [46]; based on these finding, the increased SCD-1 evident with severe obesity would be anticipated to favor the development of obesity-related conditions. This causal relationship was substantiated when SCD-1 was overexpressed in HSkMC from lean subjects and a reduction in FAO along with increased lipid storage was observed; these alterations resulted in a marked shift of lipid partitioning towards storage and away from oxidation [30]. The fact that both FAO and lipid storages were altered with overexpression suggests that SCD-1 may impart a multitiered level of control by altering the intracellular content of lipid ligands which can function as signaling molecules for gene transcription.
A reduction in mitochondrial content may also contribute to the decrease in FAO evident with severe obesity. In HSkMC, Consitt et al. [45] reported a reduction in FAO, increase in incomplete FAO, increased incorporation into TAG and diacylglycerol (DAG) pools, and an overall preferential partitioning of lipid towards storage rather than oxidation in severely obese subjects. Mitochondrial content, as determined by mitochondrial DNA copy number (mtDNA) and COXIV protein content, was also significantly reduced in the cultures derived from the severely obese donors; however, after correction for mitochondrial content (i.e., FAO/mtDNA; FAO/COXIV) FAO was equivalent in lean and obese subjects. These findings suggest that the mitochondria of severely obese individuals function normally in respect to lipid oxidation and that the overall reduction in FAO can be attributed to a lower mitochondrial content [45]. Overexpression of PGC-1α, a transcriptional coactivator that stimulates mitochondrial biogenesis, increased mitochondrial content and FAO in HSkMC from severely obese individuals [45]. However, FAO remained depressed compared to lean controls, which suggests that the severely obese state limits both mitochondrial biogenesis and oxidative capacity via mechanisms that are independent of PGC-1α abundance. Together, these data obtained in HSkMC [30, 45] demonstrate that lipid oxidation is inherently reduced in the skeletal muscle of severely obese individuals due to decrements in multiple steps of lipid metabolism. We have also observed that HSkMC from severely obese subjects secretes myostatin, a myokine which inhibits protein synthesis, at a high rate; the impact of this alteration on energy metabolism is not yet, however, evident [47].
4. The Effect of Lipid Exposure on Metabolic Programs in Severely Obese Individuals
4.1. Insulin Action
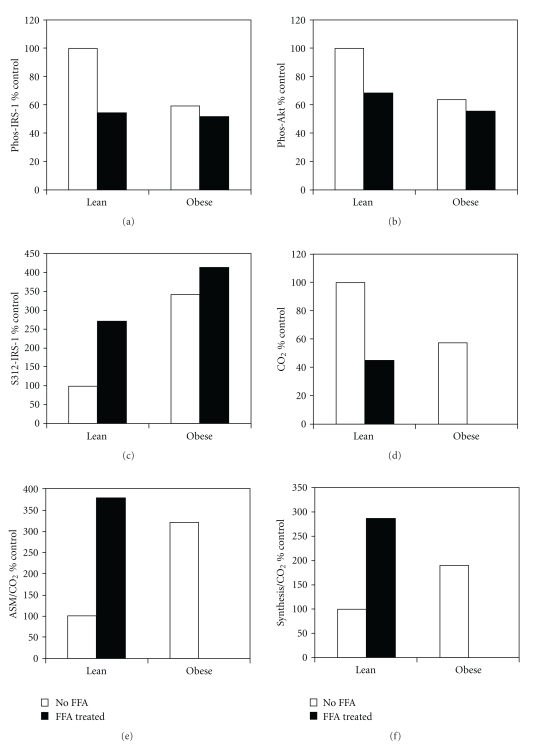
It is well established that a high-fat diet causes insulin resistance in skeletal muscle. Because fatty acids are potent metabolic regulators as well as substrates, we investigated the effects of incubating HSkMC from lean and severely obese subjects in fatty acids for 12 to 48 hours. Consistent with our hypothesis, fatty acids caused insulin resistance in HSkMC from lean controls. Fatty acid exposure decreased values for IRS-1 serine 312 phosphorylation as well as insulin stimulation of IRS-1 and Akt in cells from lean controls to values approximating those in myotubes from severely obese subjects (Figure 2). Since cells from severely obese subjects were already insulin resistant there was no further effect of fatty acid incubation.
Figure 2.
Comparison of insulin signal transduction and fatty acid metabolism in human cultured skeletal muscle cells (HSkMC) from lean and severely obese individuals that were incubated in the presence or absence of free fatty acids for 16 hours. The values shown in the graphs were calculated from mean values in published papers. The values for muscle cells from lean individuals in the absence of fatty acids were used as 100%. (a) Insulin stimulated tyrosine phosphorylation of IRS-1 (Phos-IRS-1) [44]. (b) Insulin stimulated Akt phosporylation (Phos-Akt) [44]. (c) IRS-1 serine 312 phosphorylation (S312-IRS-1) [44]. (d) Complete fatty acid oxidation as determined from labeled CO2 production from 14C labeled palmitate (CO2) [43, 45]. (e) Incomplete fatty acid oxidation from calculating the 14C from labeled palmitate remaining in the acid soluble metabolite fraction divided by labeled CO2 production (ASM/CO2) [43, 45]. (f) Partitioning between lipid synthesis and fatty acid oxidation (synthesis/CO2) [25, 30, 43, 45].
Activation of AMP kinase (AMPK) is known to reverse insulin resistance in many animal models and metformin may increase insulin sensitivity in humans through this mechanism. Therefore, we tested whether activation of AMPK could reverse insulin resistance in HSkMC from severely obese individuals. AICAR (an activator of AMPK) incubation rescued insulin signal transduction in HSkMC from severely obese subjects or cells from lean controls treated with fatty acids [44]. These results suggest that treatment of insulin-sensitive skeletal muscle with fatty acids induces insulin resistance to a degree equivalent to HSkMC from severely obese subjects. Likewise, insulin resistance caused by either fatty acid treatment or severe obesity can be reversed through the activation of AMPK.
4.2. Fat Metabolism
Consumption of a high fat diet is also known to alter lipid metabolism; we therefore hypothesized that treating muscle cells with fatty acids would affect the oxidation and storage of fatty acids. HSkMC from lean and severely obese subjects were treated with fatty acids for 12 to 48 hours and then studied. Consistent with earlier published results [30, 45] we again observed that FAO was initially depressed and fatty acid storage enhanced in HSkMC from severely obese individuals [43]. Interestingly, treatment of HSkMC from lean subjects with fatty acids for 48 hours elicited an elevation in incomplete FAO and increased lipid storage to the point that the phenotype of the lean cells approximated that seen in severely obese individuals. These results led us to the hypothesis that there is a constitutive metabolic program in the skeletal muscle of severely obese patients that can be induced in cells of lean individuals by treatment with fatty acids.
The evidence indicating a relatively global dysfunction in lipid metabolism with severe obesity [25, 26, 43] prompted an investigation of gene regulation in the skeletal muscle of severely obese subjects. In lean individuals we observed that a 5-day high-fat diet (HFD) (65% of total energy from fat) increased the expression of genes which would enhance FAO in skeletal muscle such as PDK4, PPARα, and PGC-1α[48]. This finding is congruent with other data indicating an elevation in FAO as an adaptive response in lean subjects to additional dietary lipid [49, 50]. However, we observed no increases in these genes with the HFD in the muscle of severely obese subjects [48] which is in agreement with the lack of a response to fatty acid incubation in HSkMC [43]. These findings indicate a relatively global dysregulation at the level of gene expression which may be involved with the impaired FAO evident in skeletal muscle with severe obesity.
If our obesity metabolic program hypothesis is correct, a related question is whether the program can be “turned off” and metabolism returned to values similar to lean individuals. Two interventions that were available for us to test this question were weight loss induced by gastric bypass surgery and physical activity.
5. The Metabolic Program in Skeletal Muscle with Severe Obesity Can Be Partially Reversed by Gastric Bypass Surgery
5.1. Insulin Action
To test whether weight loss after gastric bypass could reverse the insulin resistance of severe obesity we studied a group of women who lost approximately 50 kg after surgery and were weight stable for at least 3 months (surgery/weight loss group) [20]. Despite weight loss the subjects still had a BMI of approximately 30 kg/m2 and were classified as obese. Data from the surgery/weight loss group was compared to (1) severely obese women (2) weight- and age-matched women who were never severely obese, and (3) age-matched, but lean (BMI < 25 kg/m2) women. As expected, a whole-body insulin sensitivity index (SI determined from a frequently sampled intravenous glucose tolerance test) demonstrated dramatic insulin resistance in the severely obese compared to the other groups [20]. Interestingly, SI of the surgery/weight loss group was not different than the lean group and was higher than in the weight-matched women. Comparisons of insulin-mediated glucose transport in vitro in muscle fiber strips obtained during surgery generally matched the differences seen in whole body insulin action (SI) [20]. Likewise, muscle IRS-1 serine 312 phosphorylation in the surgery/weight loss group matched that of the lean group and was significantly lower than that of the severely obese or the weight-matched groups [20]. Thus, the weight loss induced by gastric bypass not only reverses insulin resistance, but actually improves insulin sensitivity to a degree that is superior to that seen in weight-matched controls. This improvement in insulin action cannot be attributed to increased physical activity after gastric bypass which is equivalent between previously severely obese surgery patents and weight-matched sedentary controls [51].
Prospective studies have confirmed that gastric bypass surgery dramatically enhances insulin action in severely obese patients [36, 37, 52]. In these experiments, we obtain measurements at approximately one year after surgery, as patients are weight stable by the time [53]; data are thus not confounded by responses evident with negative energy balance. In terms of possible mechanisms explaining this improvement, we observed that there was no change in the concentration of the insulin-sensitive glucose transporter (GLUT4) [52]. Insulin receptor concentration, however, doubled with weight loss which may contribute to the improvement in insulin action seen with the intervention [54]. Gene array and RT-PCR analyses indicated that growth factor receptor-bound protein 14, glycerol-3-phosphate dehydrogenase, and myostatin were elevated with severe obesity but significantly reduced with weight loss [55]. Pathway analyses indicated the involvement of these and other genes in weight-loss responsive networks which would be expected to improve insulin signaling, decrease triglyceride synthesis, and increase muscle mass with gastric bypass/weight loss [55]. However, the predominance of insulin-resistant, glycolytic muscle fibers evident with severe obesity [35] was not altered with gastric bypass surgery/weight loss [36], although a higher initial percentage of type I fibers was associated with increased weight loss [35]. In contrast, intramuscular TAG and long-chain fatty acyl-CoA concentrations (palmityl, stearate, and linoleate CoA) were dramatically reduced with gastric bypass/weight loss [36, 37]. This reduction in intramuscular lipid content could contribute to the improvement in insulin action seen with gastric bypass surgery as intracellular lipids can induce insulin resistance [44].
5.2. Fat Metabolism
An impaired capacity for FAO has been linked with insulin resistance through the accumulation of lipid-related metabolites which impede insulin signal transduction or other mechanisms [56]. Conversely, a high capacity for FAO in skeletal muscle has been positively associated with insulin sensitivity independent of intramuscular lipid content [57]. An increase in FAO in skeletal muscle with gastric bypass/weight loss could thus explain both the improvement in insulin action and reduction in intracellular lipid content evident at one year after the intervention [36, 37, 52]. However, our studies indicate that the depressed FAO evident with severe obesity is not altered with gastric bypass surgery/weight loss.
Using needle biopsies from the vastus lateralis Berggren et al. [27] compared FAO in severely obese women after gastric bypass surgery/weight loss to (1) lean controls and (2) severely obese individuals. FAO was virtually equivalent in the muscle from the gastric bypass surgery/weight loss and severely obese groups and depressed compared to the lean women. Incomplete lipid oxidation (ASM/CO2) was also elevated compared to lean controls in both the gastric bypass/weight loss and severely obese groups. With a prospective study design, we again observed no effect of gastric bypass surgery/weight loss on complete and incomplete FAO in the skeletal muscle of women who lost 55 kg to achieve a mean BMI of 30.5 ± 2.3 kg/m2 [27]. These findings in skeletal muscle were supported by studies that utilized whole-body indices of FAO. Infusion of labeled tracers (13C palmitate and 14C acetate) indicated that FAO remained equivalent in gastric bypass surgery/weight loss and severely obese women and depressed compared to lean controls [58]. A comparison of fat utilization during submaximal exercise (indirect calorimetry) also indicated that whole-body lipid oxidation was depressed in women who had lost weight via gastric bypass surgery compared to weight-matched controls [51].
In summary, insulin action is improved with gastric bypass surgery/weight loss to the extent that previously severely obese subjects are even more insulin sensitive than weight-matched controls. Gastric bypass surgery/weight loss does not, however, rescue the reduction in FAO in skeletal muscle evident with severe obesity. If an impaired FAO is linked with weight gain [23], the inability to alter FAO with weight loss intervention may explain why some individuals are predisposed to severe obesity and weight regain after dietary-induced weight loss. The mechanical limitations imposed on energy intake by the gastric bypass procedure may be the only practical and effective intervention to insure long-term weight loss in this patient population. The data gathered from our work also suggests that the optimal treatment strategy for the metabolic aberrations evident with severe obesity would consist of weight loss coupled with an intervention that would increase FAO in skeletal muscle.
6. The Obesity Metabolic Program Can Be Reversed by Exercise
6.1. Insulin Action and Fat Metabolism
The effects of exercise training on skeletal muscle are well documented and include improving insulin action and increasing FAO. It thus seems intuitive that exercise would be effective in alleviating the insulin resistance and reduction in FAO in skeletal muscle evident with severe obesity. However, there are reports of an “exercise resistance” in obese/diabetic patients in terms of eliciting mitochondrial biogenesis [59, 60] which could also be evident in severely obese individuals as both populations share the common traits of insulin resistance and a reduction in FAO [56]. In relation to insulin action, we examined the effects of 7 consecutive days of exercise (60 min/day, ~65% VO2peak) on severely obese men [61]. This relatively acute training prescription was utilized as body mass is not altered; thus any changes can be primarily attributed to the effects of contractile activity alone. Exercise training reduced fasting and two-hour insulin concentrations and also reduced the insulin area under the curve during an oral glucose tolerance test, indicating improved insulin action.
A similar acute training prescription (10 consecutive days, 60 min/day, ~70% VO2 Peak) was utilized to determine the impact of physical activity on FAO [27]. Three groups of subjects were examined: (1) lean (BMI < 25 kg/m2); (2) obese but not severely obese and (3) previously severely obese subjects who had lost weight through gastric bypass surgery. Complete FAO (labeled CO2) in skeletal muscle biopsies was initially reduced and incomplete FAO (ASM/CO2) elevated in the gastric bypass/weight loss compared to the lean and obese groups. Exercise training increased complete FAO by ~2-fold in the lean and obese groups and, despite the initial decrement, also increased FAO in the gastric bypass/weight loss group to the degree that it did not differ between the lean, obese, and weight loss groups after the intervention. Incomplete oxidation was also normalized after exercise training in the skeletal muscle of the gastric bypass/weight loss group [27]. No differences in the responses of PDK4, CPT-1, and PGC-1α mRNA to training were evident between the groups. These findings [27, 61] indicate that exercise training can be used to alleviate the phenotype/metabolic program of insulin resistance and reduced FAO evident with severe obesity, although the cellular mechanism(s) remain to be defined.
7. Conclusions
Severe obesity (BMI ≥ 40 kg/m2) is associated with insulin resistance in skeletal muscle due to impairments in multiple steps of the insulin signaling pathway. Increased intramuscular lipid content and a reduction in FAO, both conditions linked with insulin resistance, are also evident in the skeletal muscle of severely obese individuals. The deficit in FAO in skeletal muscle with severe obesity may also help explain a propensity towards the development of obesity/severe obesity and weight gain in these individuals as lipid is partitioned towards storage rather than oxidation.
The impaired insulin signal transduction and depressed FAO from intact skeletal muscle remained apparent in human skeletal muscle cells (HSkMCs) raised in culture from severely obese donors. It is believed that characteristics exhibited in HSkMC primarily reflect genetic or epigenetic traits. These data have led us to believe that the skeletal muscle of severely obese individuals displays a global metabolic program which results in insulin resistance and impaired FAO. We believe this concept represents a paradigm shift in our concepts about metabolic regulation in obesity.
This metabolic program can be induced with fatty acid exposure in HSkMC. In contrast, weight loss via gastric bypass surgery can “turn off” components of this metabolic program as insulin sensitivity is restored or even enhanced compared to weight-matched controls with the intervention. However, gastric bypass/weight loss does not rescue the decrement in FAO in skeletal muscle evident with severe obesity. This consistent retention of a reduced FAO may explain why severely obese individuals are prone to weight gain and weight-regain after diet-induced weight loss and why the mechanical limitations imposed on energy intake by the gastric bypass procedure provides an effective intervention. Physical activity can improve FAO and insulin action in severely obese individuals, indicating that this patient population is not “exercise resistant”; physical activity should thus be considered as an adjunct to weight loss intervention. In conclusion, it is hoped that the research summarized in this review can aid in preventing and/or treating the severely obese condition.
Acknowledgments
This work was supported by NIH Grants RO1DK46121 (GLD) and RO1DK56112 (JAH).
References
- 1.Turner N, Heilbronn LK. Is mitochondrial dysfunction a cause of insulin resistance? Trends in Endocrinology and Metabolism. 2008;19(9):324–330. doi: 10.1016/j.tem.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Dumas JF, Simard G, Flamment M, Ducluzeau PH, Ritz P. Is skeletal muscle mitochondrial dysfunction a cause or an indirect consequence of insulin resistance in humans? Diabetes and Metabolism. 2009;35(3):159–167. doi: 10.1016/j.diabet.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Phielix E, Mensink M. Type 2 diabetes mellitus and skeletal muscle metabolic function. Physiology and Behavior. 2008;94(2):252–258. doi: 10.1016/j.physbeh.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 4.Holloszy JO. Skeletal muscle “mitochondrial deficiency” does not mediate insulin resistance. American Journal of Clinical Nutrition. 2009;89(1):463S–466S. doi: 10.3945/ajcn.2008.26717C. [DOI] [PubMed] [Google Scholar]
- 5.Abdul-Ghani MA, DeFronzo RA. Mitochondrial dysfunction, insulin resistance, and type 2 diabetes mellitus. Current Diabetes Reports. 2008;8(3):173–178. doi: 10.1007/s11892-008-0030-1. [DOI] [PubMed] [Google Scholar]
- 6.Abdul-Ghani MA, Muller FL, Liu Y, et al. Deleterious action of FA metabolites on ATP synthesis: possible link between lipotoxicity, mitochondrial dysfunction, and insulin resistance. American Journal of Physiology. 2008;295(3):E678–E685. doi: 10.1152/ajpendo.90287.2008. [DOI] [PubMed] [Google Scholar]
- 7.Dohm GL, Tapscott EB, Pories WJ, et al. An in vitro human muscle preparation suitable for metabolic studies. Decreased insulin stimulation of glucose transport in muscle from morbidly obese and diabetic subjects. Journal of Clinical Investigation. 1988;82(2):486–494. doi: 10.1172/JCI113622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dohm GL, Elton CW, Raju MS, et al. IGF-I-stimulated glucose transport in human skeletal muscle and IGF-I resistance in obesity and NIDDM. Diabetes. 1990;39(9):1028–1032. doi: 10.2337/diab.39.9.1028. [DOI] [PubMed] [Google Scholar]
- 9.Elton CW, Tapscott EB, Pories WJ, Dohm GL. Effect of moderate obesity on glucose transport in human muscle. Hormone and Metabolic Research. 1994;26(4):181–183. doi: 10.1055/s-2007-1000807. [DOI] [PubMed] [Google Scholar]
- 10.Friedman JE, Caro JF, Pories WJ, Azevedo JL, Dohm GL. Glucose metabolism in incubated human muscle: effect of obesity and non- insulin-dependent diabetes mellitus. Metabolism. 1994;43(8):1047–1054. doi: 10.1016/0026-0495(94)90188-0. [DOI] [PubMed] [Google Scholar]
- 11.Dolan PL, Tapscott EB, Dorton PJ, Dohm GL. Contractile activity restores insulin responsiveness in skeletal muscle of obese Zucker rats. Biochemical Journal. 1993;289(2):423–426. doi: 10.1042/bj2890423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azevedo JL, Jr., Carey JO, Pories WJ, Morris PG, Dohm GL. Hypoxia stimulates glucose transport in insulin-resistant human skeletal muscle. Diabetes. 1995;44(6):695–698. doi: 10.2337/diab.44.6.695. [DOI] [PubMed] [Google Scholar]
- 13.Carey JO, Azevedo JL, Morris PG, Pories WJ, Dohm GL. Okadaic acid, vanadate, and phenylarsine oxide stimulate 2-deoxyglucose transport in insulin-resistant human skeletal muscle. Diabetes. 1995;44(6):682–688. doi: 10.2337/diab.44.6.682. [DOI] [PubMed] [Google Scholar]
- 14.Goodyear LJ, Giorgino F, Sherman LA, Carey J, Smith RJ, Dohm GL. Insulin receptor phosphorylation, insulin receptor substrate-1 phosphorylation, and phosphatidylinositol 3-kinase activity are decreased in intact skeletal muscle strips from obese subjects. Journal of Clinical Investigation. 1995;95(5):2195–2204. doi: 10.1172/JCI117909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brozinick JT, Roberts BR, Dohm GL. Defective signaling through Akt-2 and -3 but not Akt-1 in insulin-resistant human skeletal muscle: potential role in insulin resistance. Diabetes. 2003;52(4):935–941. doi: 10.2337/diabetes.52.4.935. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad F, Azevedo JL, Cortright R, Dohm GL, Goldstein BJ. Alterations in skeletal muscle protein-tyrosine phosphatase activity and expression in insulin-resistant human obesity and diabetes. Journal of Clinical Investigation. 1997;100(2):449–458. doi: 10.1172/JCI119552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caro JF, Sinha MK, Raju SM. Insulin receptor kinase in human skeletal muscle from obese subjects with and without noninsulin dependent diabetes. Journal of Clinical Investigation. 1987;79(5):1330–1337. doi: 10.1172/JCI112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou Q, Dolan PL, Dohm GL. Dephosphorylation increases insulin-stimulated receptor kinase activity in skeletal muscle of obese Zucker rats. Molecular and Cellular Biochemistry. 1999;194(1-2):209–216. doi: 10.1023/a:1006942831223. [DOI] [PubMed] [Google Scholar]
- 19.Itani SI, Zhou Q, Pories WJ, MacDonald KG, Dohm GL. Involvement of protein kinase C in human skeletal muscle insulin resistance and obesity. Diabetes. 2000;49(8):1353–1358. doi: 10.2337/diabetes.49.8.1353. [DOI] [PubMed] [Google Scholar]
- 20.Bikman BT, Zheng D, Pories WJ, et al. Mechanism for improved insulin sensitivity after gastric bypass surgery. Journal of Clinical Endocrinology and Metabolism. 2008;93(12):4656–4663. doi: 10.1210/jc.2008-1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cortright RN, Azevedo JL, Zhou Q, et al. Protein kinase C modulates insulin action in human skeletal muscle. American Journal of Physiology. 2000;278(3):E553–E562. doi: 10.1152/ajpendo.2000.278.3.E553. [DOI] [PubMed] [Google Scholar]
- 22.Dagenais GR, Tancredi RG, Zierler KL. Free fatty acid oxidation by forearm muscle at rest, and evidence for an intramuscular lipid pool in the human forearm. Journal of Clinical Investigation. 1976;58(2):421–431. doi: 10.1172/JCI108486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zurlo F, Lillioja S, Puente AED, et al. Low ratio of fat to carbohydrate oxidation as predictor of weight gain: study of 24-h RQ. American Journal of Physiology. 1990;259(5):E650–E657. doi: 10.1152/ajpendo.1990.259.5.E650. [DOI] [PubMed] [Google Scholar]
- 24.Zurlo F, Nemeth PM, Choksi RM, Sesodia S, Ravussin E. Whole-body energy metabolism and skeletal muscle biochemical characteristics. Metabolism. 1994;43(4):481–486. doi: 10.1016/0026-0495(94)90081-7. [DOI] [PubMed] [Google Scholar]
- 25.Hulver MW, Berggren JR, Cortright RN, et al. Skeletal muscle lipid metabolism with obesity. American Journal of Physiology. 2003;284(4):E741–E747. doi: 10.1152/ajpendo.00514.2002. [DOI] [PubMed] [Google Scholar]
- 26.Kim JY, Hickner RC, Cortright RL, Dohm GL, Houmard JA. Lipid oxidation is reduced in obese human skeletal muscle. American Journal of Physiology. 2000;279(5):E1039–E1044. doi: 10.1152/ajpendo.2000.279.5.E1039. [DOI] [PubMed] [Google Scholar]
- 27.Berggren JR, Boyle KE, Chapman WH, Houmard JA. Skeletal muscle lipid oxidation and obesity: influence of weight loss and exercise. American Journal of Physiology. 2008;294(4):E726–E732. doi: 10.1152/ajpendo.00354.2007. [DOI] [PubMed] [Google Scholar]
- 28.Hittel DS, Hathout Y, Huffman EP, Houmard JA. Proteome analysis of skeletal muscle from obese and morbidly obese women. Diabetes. 2005;54(5):1283–1288. doi: 10.2337/diabetes.54.5.1283. [DOI] [PubMed] [Google Scholar]
- 29.Bonen A, Parolin ML, Steinberg GR, et al. Triacylglycerol accumulation in human obesity and type 2 diabetes is associated with increased rates of skeletal muscle fatty acid transport increased sarcolemmal FAT/CD36. FASEB Journal. 2004;18(10):1144–1146. doi: 10.1096/fj.03-1065fje. [DOI] [PubMed] [Google Scholar]
- 30.Hulver MW, Berggren JR, Carper MJ, et al. Elevated stearoyl-CoA desaturase-1 expression in skeletal muscle contributes to abnormal fatty acid partitioning in obese humans. Cell Metabolism. 2005;2(4):251–261. doi: 10.1016/j.cmet.2005.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shulman GI. Cellular mechanisms of insulin resistance. Journal of Clinical Investigation. 2000;106(2):171–176. doi: 10.1172/JCI10583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goodpaster BH, He J, Watkins S, Kelley DE. Skeletal muscle lipid content and insulin resistance: evidence for a paradox in endurance-trained athletes. Journal of Clinical Endocrinology and Metabolism. 2001;86(12):5755–5761. doi: 10.1210/jcem.86.12.8075. [DOI] [PubMed] [Google Scholar]
- 33.Goodpaster BH, Theriault R, Watkins SC, Kelley DE. Intramuscular lipid content is increased in obesity and decreased by weight loss. Metabolism. 2000;49(4):467–472. doi: 10.1016/s0026-0495(00)80010-4. [DOI] [PubMed] [Google Scholar]
- 34.Hickey MS, Carey JO, Azevedo JL, et al. Skeletal muscle fiber composition is related to adiposity and in vitro glucose transport rate in humans. American Journal of Physiology. 1995;268(3):E453–E457. doi: 10.1152/ajpendo.1995.268.3.E453. [DOI] [PubMed] [Google Scholar]
- 35.Tanner CJ, Barakat HA, Lynis Dohm G, et al. Muscle fiber type is associated with obesity and weight loss. American Journal of Physiology. 2002;282(6):E1191–E1196. doi: 10.1152/ajpendo.00416.2001. [DOI] [PubMed] [Google Scholar]
- 36.Gray RE, Tanner CJ, Pories WJ, MacDonald KG, Houmard JA. Effect of weight loss on muscle lipid content in morbidly obese subjects. American Journal of Physiology. 2003;284(4):E726–E732. doi: 10.1152/ajpendo.00371.2002. [DOI] [PubMed] [Google Scholar]
- 37.Houmard JA, Tanner CJ, Yu C, et al. Effect of weight loss on insulin sensitivity and intramuscular long-chain fatty acyl-CoAs in morbidly obese subjects. Diabetes. 2002;51(10):2959–2963. doi: 10.2337/diabetes.51.10.2959. [DOI] [PubMed] [Google Scholar]
- 38.Henry RR, Ciaraldi TP, Abrams-Carter L, Mudaliar S, Park KS, Nikoulina SE. Glycogen synthase activity is reduced in cultured skeletal muscle cells of non-insulin-dependent diabetes mellitus subjects: biochemical and molecular mechanisms. Journal of Clinical Investigation. 1996;98(5):1231–1236. doi: 10.1172/JCI118906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berggren JR, Tanner CJ, Houmard JA. Primary cell cultures in the study of human muscle metabolism. Exercise and Sport Sciences Reviews. 2007;35(2):56–61. doi: 10.1249/JES.0b013e31803eae63. [DOI] [PubMed] [Google Scholar]
- 40.Muoio DM, Way JM, Tanner CJ, et al. Peroxisome proliferator-activated receptor-α regulates fatty acid utilization in primary human skeletal muscle cells. Diabetes. 2002;51(4):901–909. doi: 10.2337/diabetes.51.4.901. [DOI] [PubMed] [Google Scholar]
- 41.Gaster M. Insulin resistance and the mitochondrial link. Lessons from cultured human myotubes. Biochimica et Biophysica Acta - Molecular Basis of Disease. 2007;1772(7):755–765. doi: 10.1016/j.bbadis.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 42.Gaster M, Rustan AC, Aas V, Beck-Nielsen H. Reduced lipid oxidation in skeletal muscle from type 2 diabetic subjects may be of genetic origin: evidence from cultured myotubes. Diabetes. 2004;53(3):542–548. doi: 10.2337/diabetes.53.3.542. [DOI] [PubMed] [Google Scholar]
- 43.Bell JA. Lipid partitioning, incomplete fatty acid oxidation, and insulin signal transduction in primary human muscle cells: effects of severe obesity, fatty acid incubation, and fatty acid translocase/CD36 overexpression. American Journal of Physiology. 2010;95(7):3400–3410. doi: 10.1210/jc.2009-1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bikman BT, Zheng D, Reed MA, Hickner RC, Houmard JA, Dohm GL. Lipid-induced insulin resistance is prevented in lean and obese myotubes by AICAR treatment. American Journal of Physiology. 2010;298(6):R1692–R1699. doi: 10.1152/ajpregu.00190.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Consitt LA, Bell JA, Koves TR, et al. Peroxisome proliferator-activated receptor-γ coactivator-1α overexpression increases lipid oxidation in myocytes from extremely obese individuals. Diabetes. 2010;59(6):1407–1415. doi: 10.2337/db09-1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cohen P, Miyazaki M, Socci ND, et al. Role for stearoyl-CoA desaturase-1 in leptin-mediated weight loss. Science. 2002;297(5579):240–243. doi: 10.1126/science.1071527. [DOI] [PubMed] [Google Scholar]
- 47.Hittel DS, Berggren JR, Shearer J, Boyle K, Houmard JA. Increased secretion and expression of myostatin in skeletal muscle from extremely obese women. Diabetes. 2009;58(1):30–38. doi: 10.2337/db08-0943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boyle KE, Canham JP, Consitt LA, et al. A high-fat diet elicits differential responses in genes coordinating oxidative metabolism in skeletal muscle of lean and obese individuals. Journal of Clinical Endocrinology and Metabolism. 2011;96(3):775–781. doi: 10.1210/jc.2010-2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Astrup A, Buemann B, Christensen NJ, Toubro S. Failure to increase lipid oxidation in response to increasing dietary fat content in formerly obese women. American Journal of Physiology. 1994;266(4):E592–E599. doi: 10.1152/ajpendo.1994.266.4.E592. [DOI] [PubMed] [Google Scholar]
- 50.Schrauwen P, Van Marken Lichtenbelt WD, Saris WHM, Westerterp KR. Changes in fat oxidation in response to a high-fat diet. American Journal of Clinical Nutrition. 1997;66(2):276–282. doi: 10.1093/ajcn/66.2.276. [DOI] [PubMed] [Google Scholar]
- 51.Guesbeck NR, Hickey MS, MacDonald KG, et al. Substrate utilization during exercise in formerly morbidly obese women. Journal of Applied Physiology. 2001;90(3):1007–1012. doi: 10.1152/jappl.2001.90.3.1007. [DOI] [PubMed] [Google Scholar]
- 52.Friedman JE, Dohm GL, Leggett-Frazier N, et al. Restoration of insulin responsiveness in skeletal muscle of morbidly obese patients after weight loss: effect on muscle glucose transport and glucose transporter GLUT4. Journal of Clinical Investigation. 1992;89(2):701–705. doi: 10.1172/JCI115638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pories WJ, MacDonald Jr. KG, Morgan EJ, et al. Surgical treatment of obesity and its effect on diabetes: 10-y follow-up. American Journal of Clinical Nutrition. 1992;55(2):582S–585S. doi: 10.1093/ajcn/55.2.582s. [DOI] [PubMed] [Google Scholar]
- 54.Pender C, et al. Muscle insulin receptor concentrations in obese patients post bariatric surgery: relationship to hyperinsulinemia. International Journal of Obesity and Related Metabolic Disorders. 2004;28(3):363–369. doi: 10.1038/sj.ijo.0802565. [DOI] [PubMed] [Google Scholar]
- 55.Park JJ, Berggren JR, Hulver MW, Houmard JA, Hoffman EP. GRB14, GPD1, and GDF8 as potential network collaborators in weight loss-induced improvements in insulin action in human skeletal muscle. Physiological Genomics. 2006;27(2):114–121. doi: 10.1152/physiolgenomics.00045.2006. [DOI] [PubMed] [Google Scholar]
- 56.Befroy DE, Petersen KF, Dufour S, et al. Impaired mitochondrial substrate oxidation in muscle of insulin-resistant offspring of type 2 diabetic patients. Diabetes. 2007;56(5):1376–1381. doi: 10.2337/db06-0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bruce CR, Anderson MJ, Carey AL, et al. Muscle oxidative capacity is a better predictor of insulin sensitivity than lipid status. Journal of Clinical Endocrinology and Metabolism. 2003;88(11):5444–5451. doi: 10.1210/jc.2003-030791. [DOI] [PubMed] [Google Scholar]
- 58.Thyfault JP, Kraus RM, Hickner RC, Howell AW, Wolfe RR, Dohm GL. Impaired plasma fatty acid oxidation in extremely obese women. American Journal of Physiology. 2004;287(6):E1076–E1081. doi: 10.1152/ajpendo.00177.2004. [DOI] [PubMed] [Google Scholar]
- 59.De Filippis E, Alvarez G, Berria R, et al. Insulin-resistant muscle is exercise resistant: evidence for reduced response of nuclear-encoded mitochondrial genes to exercise. American Journal of Physiology. 2008;294(3):E607–E614. doi: 10.1152/ajpendo.00729.2007. [DOI] [PubMed] [Google Scholar]
- 60.Herńandez-Alvarez MI, Thabit H, Burns N, et al. Subjects with early-onset type 2 diabetes show defective activation of the skeletal muscle PGC-1α/mitofusin-2 regulatory pathway in response to physical activity. Diabetes Care. 2010;33(3):645–651. doi: 10.2337/dc09-1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hickey MS, Gavingan KE, McCammon MR, et al. Effects of 7 days of exercise training on insulin action in morbidly obese men. Clinical Exercise Physiology. 1999;1:24–28. [Google Scholar]