Abstract
The annual death numbers of influenza and pneumonia in Norway were studied for the time period 1980–2000. No direct relationships were found with the variations of the annual UVB fluences, probably due to the fact that these variations did not exceed 30%. However, there was a very pronounced seasonal variation of both influenza deaths and pneumonia deaths, the vast majority occurring during the winter. Vitamin D levels were also estimated from several publications. The data support the hypothesis that a high vitamin D level, as that found in the summer, acts in a protective manner with respect to influenza as well as pneumonia. The findings are discussed and compared with data from tropical and subtropical areas.
Key words: vitamin D, influenza, pneumonia, solar radiation, UVB radiation
Introduction
Nearly all human diseases related to respiratory pathogens exhibit seasonal variations.1,2 The reasons for the seasonality, however, are still not known. Among the poorly tested hypothesis are: Seasonality of low temperatures, of dry air, of crowding together indoor in the winter, travelling patterns, vacations, seasonality of ultraviolet (UV) radiation from the sun that might kill pathogens, circannual rhythms of hormones like the “dark hormone” melatonin, etc.3 Additionally, the question of whether it is the host or the vira/bacteria that exhibit seasonality arises. In the present work we have compared the seasonality of deaths of influenza and pneumonia in Norway with those of vitamin D photosynthesis and vitamin D serum levels.
Results and Discussion
Figure 1 shows the seasonal variation of vitamin D formation in human skin calculated from the known, 1990–2000 average levels of UV as earlier described,8 using the action spectrum of Galkin and Terenetskaya.9 The small dip in the curve in June is related to the cloud cover, which is taken into account. In agreement with earlier work, the vitamin D level is maximal about one month after the time of maximal formation, which occurs close to midsummer. This is due to the fact that the vitamin D level is here determined as the concentration of 25-hydroxyvitamin D [25(OH)D or calcidiol] in serum and that the formation of this metabolite from previtamin D, via vitamin D (mainly in the liver), takes some time. The fact that many have their vacation in July may also play a role. The observed delay is in agreement with earlier findings11–14 and has been discussed in these papers. In fact, the lowest vitamin D level is found in February, and average levels as low as 25 nmol/l have been observed among women avoiding direct sun exposure.
Figure 1.
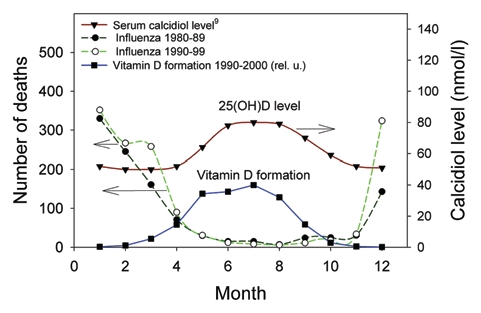
Seasonal variations of serum levels of vitamin D (▼) in the Nordic countries, given as averages from three reports in ref. 9. Photosynthesis of vitamin D for Southern Norway (■) is calculated by use of the action spectrum in ref. 7, UV measurements in Oslo and radiative transfer calculations using a cylinder model as described in the text. The results are presented in relative units (rel. u.). Influenza deaths in two periods (●, ◯) in Norway are also given.
In both periods studied (1980–1989 and 1990–1999, Fig. 1), the death rates are very small in the season when the vitamin D status is best. The agreement between the death numbers in the two periods is good. This argues, although only weakly, for the common assumption that the seasonal variation of influenza is host related rather than caused by differences in the viral strains from year to year. This is also in agreement with recent observations that the same virus strain seems to be present in the hosts over longer periods, two years or more, but leading to manifest disease only under favourable conditions, mainly related to host immune weakening.1,15,16 One might expect variations in the immune system to play major roles. Vitamin D interacts with the immune system, essentially strengthening it, in several ways as reviewed elsewhere.17–19 Other pathways of interaction, like via circannual rhythms, cannot yet be ruled out.20 The preventive effect of vitamin D supplementation has been demonstrated also in intervention studies.21 Furthermore, Ginde et al. found that the serum levels of vitamin D were inversely associated with upper respiratory tract infections,22 and it seems that exposure to artificial UVB radiation has a protective effect.23 We, therefore, propose that the seasonal variation of influenza death numbers is related to the seasonal variation of vitamin D status.
An argument against this proposal from our data might be that the influenza death rates start to increase almost two months after the vitamin D levels have reached their minimum (Fig. 1).
However, one should remember that our register gives time-points for death, not for disease initiation. A delay of weeks is quite likely. Similarly, the death numbers start to decrease several months before the vitamin D level starts to increase significantly. This is likely to be related to induction of better immunity. Thus, influenza pandemies, starting outside the classical winter influenza season, have a duration of not more than a few months, but also in the case of classical pandemies, like the Spanish flu, 1918–1919, there came a winter wave after the initial wave.24 The first wave peaked in 1918, in October 19th in Baltimore, in October 26th in Augusta and in November 5th in San Francisco (an east-west wave), while the secondary wave came January 1919.
In future work other factors than vitamin D, essentially those mentioned in the introduction, should be taken into account. Out of these temperature and humidity may be the most important ones.25–28
Variation of summer UVB levels over the two decades, from 1980 to 2000, as shown in Figure 2, upper panel, are significant. For instance, from 1997 to 1998 there was a 20% decrease in the level. Annual numbers of influenza deaths do not reflect the variations of the UVB levels. This may be due to that the UVB variations are too small, notably in view of the fact that summer levels of vitamin D are not more than 30–50% higher than winter levels. Thus, a 20% decrease in summer UVB level would result in only a small overall decrease in vitamin D level, probably too small to influence the immunity next winter significantly.
Figure 2.

Upper: The UVB levels in Norway in the period 1980–2000.29 In this case the UVB fluences were determined for a horizontal plane with the CIE erythema spectrum, which is UVB weighted and very close to the vitamin D spectrum used in the rest of this work. Lower: The average number of influenza and pneumonia deaths per year in Norway in the same period.
Norway is localized from 58 to 70 degrees north, vitamin D being synthesized in skin exclusively in the summer months. It is, therefore, of interest to compare our data with data from tropical and subtropical regions. Generally, there is no distinct seasonal pattern in the tropics.30–32 In Singapore small peaks were found in June–July and in November–January, coinciding with the winter in the Southern and northern hemisphere, respectively.30 At latitudes between 20 and 30 degrees north, clear winter seasons of influenza are found.15,33 This is at first sight surprising. However, we have calculated by the methods described above, that at 25 degrees north the rate of vitamin D synthesis in human skin is about five times larger in late June than in late December. Sometimes secondary peaks are observed in June–August.15,33 These peaks may be caused by other climatic factors than those directly related solar elevation.34 Thus, cloud cover is likely to be involved since it will influence both humidity and UV penetration through the atmosphere. It seems that that many respiratory syncytial virus epidemics begin in coastal areas.35
Variations of the ambient UVB level have sometimes been proposed as factors related to influenza periods.36–38 However, we have earlier shown that influence of variations of cloud cover on the annual UVB fluence is more than three times as large as that of variations of ozone levels.39,40 Furthermore, during a sunspot cycle (about 11 years) the UVB fluence varies less than 1%.39,41,42
In conclusion, our data are in agreement with the assumption that the high numbers of winter influenza and pneumonia deaths in Norway are related to low vitamin D levels in this season.
Materials and Methods
Influenza and pneumonia deaths.
The numbers of monthly influenza and pneumonia deaths were calculated by Prof. Øystein Kravdal from individual data provided by Statistics Norway. The numbers are averaged over the years 1980–1989 and 1990–1999. It may be difficult know if the influenza deaths are caused directly by influenza or by secondary diseases.
Solar exposure and seasonal vitamin D formation.
The main factors influencing the UV irradiances at ground level are solar zenith angle (variable with season, latitude and time of day), cloud and snow cover and the thickness of the ozone layer.4
In this study, the solar UV exposures were calculated using a radiative transfer model.5,6 Total ozone amounts used in this model were measured by the Total Ozone Mapping Spectrometer (TOMS) satellite instruments. The daily cloud cover was derived from measured reflectivities by TOMS instruments and ground-based UV measurements in Oslo. A cylinder geometry of the human body was used. The arguments for this choice have been presented earlier.7,8
The results are presented as vitamin D forming UV doses. The efficiency spectrum for vitamin D production gives the relative effectiveness of solar radiation at different wavelengths in converting 7-dehydrocholesterol to previtamin D.9 Briefly, an efficiency spectrum is calculated by multiplying the intensity of the solar radiation (wavelength by wavelength) with the action spectrum for the vitamin D production for the corresponding wavelength. The vitamin D action spectrum was taken from the publication of Galkin and Terenetskaya9 which is similar to that measured by MacLaughlin et al. in ex vivo skin specimens.10
The vitamin D levels in different seasons are taken from an earlier publication11 and are averages from three different experimental Nordic series described there.
Acknowledgements
We want to thank Øystein Kravdal from the Institute of Economy (Oslo University, Norway) for calculating the number of deaths of influenza and pneumonia. Direct overpass TOMS data were provided by NASA/GSFC.
Abbreviations
- 25(OH)D
25-hydroxyvitamin D
- TOMS
total ozone mapping spectrometer
- UV
ultraviolet
Footnotes
Previously published online: www.landesbioscience.com/journals/dermatoendocrinology/article/11357
References
- 1.Dowell SF, Ho MS. Seasonality of infectious diseases and severe acute respiratory syndrome-what we don't know can hurt us. Lancet Infect Dis. 2004;4:704–708. doi: 10.1016/S1473-3099(04)01177-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eccles R. An explanation for the seasonality of acute upper respiratory tract viral infections. Acta Otolaryngol. 2002;122:183–191. doi: 10.1080/00016480252814207. [DOI] [PubMed] [Google Scholar]
- 3.Monto AS. Global burden of influenza: what we know and what we need to know. Int Congr Ser. 2004;1263:3–11. [Google Scholar]
- 4.Madronich S, McKenzie RL, Bjorn LO, Caldwell MM. Changes in biologically active ultraviolet radiation reaching the Earth's surface. J Photochem Photobiol B. 1998;46:5–19. doi: 10.1016/s1011-1344(98)00182-1. [DOI] [PubMed] [Google Scholar]
- 5.Stamnes K, Tsay SC, Wiscombe WJ, Jayaweera K. Numerically stable algorithm for discrete-ordinate-method radiative transfer in multiple scattering and emitting layered media. Appl Opt. 1988:2509–2527. doi: 10.1364/AO.27.002502. [DOI] [PubMed] [Google Scholar]
- 6.Dahlback A, Stamnes K. A new spherical model for computing the radiation field available for photolysis and heating rate at twilight. Planet Space Sci. 1991;39:671–683. [Google Scholar]
- 7.Moan J, Dahlback A, Porojnicu AC. At what time should one go out in the sun? Adv Exp Med Biol. 2008;624:86–88. doi: 10.1007/978-0-387-77574-6_7. [DOI] [PubMed] [Google Scholar]
- 8.Moan J, Dahlback A, Lagunova Z, Cicarma E, Porojnicu AC. Solar radiation, vitamin D and cancer incidence and mortality in Norway. Anticancer Res. 2009;29:3501–3509. [PubMed] [Google Scholar]
- 9.Galkin ON, Terenetskaya IP. ‘Vitamin D’ biodosimeter: basic characteristics and potential applications. J Photochem Photobiol B. 1999;53:12–19. doi: 10.1016/s1011-1344(99)00115-3. [DOI] [PubMed] [Google Scholar]
- 10.MacLaughlin JA, Anderson RR, Holick MF. Spectral character of sunlight modulates photosynthesis of previtamin D3 and its photoisomers in human skin. Science. 1982;216:1001–1003. doi: 10.1126/science.6281884. [DOI] [PubMed] [Google Scholar]
- 11.Moan J, Porojnicu AC, Robsahm TE, Dahlback A, Juzeniene A, Tretli S, Grant W. Solar radiation, vitamin D and survival rate of colon cancer in Norway. J Photochem Photobiol B. 2005;78:189–193. doi: 10.1016/j.jphotobiol.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Beadle PC, Burton JL, Leach JF. Correlation of seasonal variation of 25-hydroxycalciferol with UV radiation dose. Br J Dermatol. 1980;103:289–293. doi: 10.1111/j.1365-2133.1980.tb07246.x. [DOI] [PubMed] [Google Scholar]
- 13.Brot C, Vestergaard P, Kolthoff N, Gram J, Hermann AP, Sorensen OH. Vitamin D status and its adequacy in healthy Danish perimenopausal women: relationships to dietary intake, sun exposure and serum parathyroid hormone. Br J Nutr. 2001;86:97–103. doi: 10.1079/bjn2001345. [DOI] [PubMed] [Google Scholar]
- 14.Moan J, Porojnicu A, Lagunova Z, Berg JP, Dahlback A. Colon cancer: prognosis for different latitudes, age groups and seasons in Norway. J Photochem Photobiol B. 2007;89:148–155. doi: 10.1016/j.jphotobiol.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Shih SR, Chen GW, Yang CC, Yang WZ, Liu DP, Lin JH, et al. Laboratory-based surveillance and molecular epidemiology of influenza virus in Taiwan. J Clin Microbiol. 2005;43:1651–1661. doi: 10.1128/JCM.43.4.1651-1661.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang JW, Ngai KL, Lam WY, Chan PK. Seasonality of influenza A(H3N2) virus: a Hong Kong perspective (1997–2006) PLoS One. 2008;3:2768. doi: 10.1371/journal.pone.0002768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, Madronich S, et al. Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134:1129–1140. doi: 10.1017/S0950268806007175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cannell JJ, Zasloff M, Garland CF, Scragg R, Giovannucci E. On the epidemiology of influenza. Virol J. 2008;5:29. doi: 10.1186/1743-422X-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grant WB, Giovannucci E. The possible roles of solar ultraviolet-B radiation and vitamin D in reducing casefatality rates from the 1918–1919 influenza pandemic in the United States. Dermato-Endocrinology. 2009;1:215–219. doi: 10.4161/derm.1.4.9063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dowell SF. Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis. 2001;7:369–374. doi: 10.3201/eid0703.010301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aloia JF, Li-Ng M. Re: epidemic influenza and vitamin D. Epidemiol Infect. 2007;135:1095–1096. doi: 10.1017/S0950268807008308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ginde AA, Mansbach JM, Camargo C., Jr Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2009;169:384–390. doi: 10.1001/archinternmed.2008.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fleming DM, Elliot AJ. Epidemic influenza and vitamin D. Epidemiol Infect. 2007;135:1091–1092. doi: 10.1017/S0950268807008291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Britten RH. The incidence of epidemic influenza, 1918–1919. Pub Healht Rep. 1932;47:303–339. [Google Scholar]
- 25.Liao CM, Chang SY, Chen SC, Chio CP. Influenza-associated morbidity in subtropical Taiwan. Int J Infect Dis. 2009;13:589–599. doi: 10.1016/j.ijid.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 26.Nafstad P, Skrondal A, Bjertness E. Mortality and temperature in Oslo, Norway, 1990–1995. Eur J Epidemiol. 2001;17:621–627. doi: 10.1023/a:1015547012242. [DOI] [PubMed] [Google Scholar]
- 27.Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lowen A, Palese P. Transmission of influenza virus in temperate zones is predominantly by aerosol, in the tropics by contact: A hypothesis. PLoS Curr Influenza. 2009 doi: 10.1371/currents.RRN1002. Aug 17:RRN1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moan J, Porojnicu AC, Dahlback A. Epidemiology of cutaneous malignant melanoma. In: Ringborg U, Brandberg Y, Breitbart EW, Greinert R, editors. Skin cancer prevention. New York: Informa Healthcare; 2007. pp. 179–201. [Google Scholar]
- 30.Shek LP, Lee BW. Epidemiology and seasonality of respiratory tract virus infections in the tropics. Paediatr Respir Rev. 2003;4:105–111. doi: 10.1016/s1526-0542(03)00024-1. [DOI] [PubMed] [Google Scholar]
- 31.Chew FT, Doraisingham S, Ling AE, Kumarasinghe G, Lee BW. Seasonal trends of viral respiratory tract infections in the tropics. Epidemiol Infect. 1998;121:121–128. doi: 10.1017/s0950268898008905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doraisingham S, Goh KT, Ling AE, Yu M. Influenza surveillance in Singapore: 1972–86. Bull World Health Organ. 1988;66:57–63. [PMC free article] [PubMed] [Google Scholar]
- 33.Suzuki Y, Taira K, Saito R, Nidaira M, Okano S, Zaraket H, et al. Epidemiologic study of influenza infection in Okinawa, Japan, from 2001 to 2007: changing patterns of seasonality and prevalence of amantadine-resistant influenza A virus. J Clin Microbiol. 2009;47:623–629. doi: 10.1128/JCM.01760-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Viboud C, Pakdaman K, Boelle PY, Wilson ML, Myers MF, Valleron AJ, et al. Association of influenza epidemics with global climate variability. Eur J Epidemiol. 2004;19:1055–1059. doi: 10.1007/s10654-004-2450-9. [DOI] [PubMed] [Google Scholar]
- 35.Stensballe LG, Devasundaram JK, Simoes EA. Respiratory syncytial virus epidemics: the ups and downs of a seasonal virus. Pediatr Infect Dis J. 2003;22:21–32. doi: 10.1097/01.inf.0000053882.70365.c9. [DOI] [PubMed] [Google Scholar]
- 36.Ertel S. Influenza pandemics and sunspots—easing the controversy. Naturwissenschaften. 1994;81:308–311. doi: 10.1007/BF01131945. [DOI] [PubMed] [Google Scholar]
- 37.Vaquero JM, Gallego MC. Sunspot numbers can detect pandemic influenza A: the use of different sunspot numbers. Med Hypotheses. 2007;68:1189–1190. doi: 10.1016/j.mehy.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 38.Hayes DP. Influenza pandemics, solar activity cycles and vitamin D. Med Hypotheses. 2009 doi: 10.1016/j.mehy.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 39.Moan J. Visible Light and UV radiation. In: Brune D, Hellborg R, Persson BRR, Paakkonen R, editors. Radiation at Home, Outdoors and in the Workplace. Oslo: Scandinavian Publisher; 2001. pp. 69–85. [Google Scholar]
- 40.Moan J, Dahlback A. Ultraviolet Radiation and Skin Cancer: Epidemiological Data from Scandinavia. In: Young AR, Bjorn LO, Moan J, Nultsch W, editors. Enviromental UV Photobiology. New York and London: Plenum Press; 1993. pp. 255–293. [Google Scholar]
- 41.Lean J. Solar ultraviolet irradiance variations. J Geophys. 1987;92:839–868. [Google Scholar]
- 42.Rottman G, Woods T, Snow M, DeToma G. The solar cycle variation in ultraviolet irradiance. Adv Space Res. 2001;27:1927–1932. [Google Scholar]


