Abstract
Monoclonal antibodies (mAbs) are used with increasing success against many tumors, but for brain tumors the blood-brain barrier (BBB) is a special concern. The BBB prevents antibody entry to the normal brain; however, its role in brain tumor therapy is more complex. The BBB is closest to normal at micro-tumor sites; its properties and importance change as the tumor grows. In this review, evolving insight into the role of the BBB is balanced against other factors that affect efficacy or interpretation when mAbs are used against brain tumor targets. As specific examples, glioblastoma multiforme (GBM), primary central nervous system lymphoma (PCNSL) and blood-borne metastases from breast cancer are discussed in the context of treatment, respectively, with the mAbs bevacizumab, rituximab and trastuzumab, each of which is already widely used against tumors outside the brain. It is suggested that success against brain tumors will require getting past the BBB in two senses: physically, to better attack brain tumor targets, and conceptually, to give equal attention to problems that are shared with other tumor sites.
Key words: monoclonal antibody, brain tumor, immunotherapy, glioma, primary central nervous system lymphoma, brain metastases, bevacizumab, rituximab, trastuzumab
Introduction
An early hope for monoclonal antibodies (mAbs) was that they would serve as tumor-specific magic bullets in two ways. As bullets, they would move through the blood to reach and attack tumor targets. The exquisite specificity of a single antibody would provide the magic. Experience with tumors outside the brain has begun to justify this hope. Among the best-studied examples, the mAbs trastuzumab (Herceptin®), rituximab (Rituxan®) and bevacizumab (Avastin®), are now approved as part of the standard therapy for appropriate forms of breast cancer,1–4 B-cell lymphoma5,6 and colorectal cancer, respectively, as well as other types of cancer.7,8
Over time, we have become more sophisticated about both the bullet and its magic. For tumors outside the brain, long-term remissions can indeed be achieved, but not all eligible patients respond, responses may be short-lived and side effects can be limiting.1–8 Many of the evolving insights and adaptations apply very generally to many different therapies or to tumors at many sites. Additional insights apply and new insights are still needed for tumor in the brain.
In applying mAb therapy to brain tumors, both expectations and interpretation are colored by awareness of the blood-brain barrier (BBB). A striking example is seen when tumors in the bodies of breast cancer patients respond to systemic mAb treatment, but then metastases appear in the brain.9,10 The reason most often suggested for this phenomenon is that the BBB must be blocking access to the brain metastases, making the brain a sanctuary site; however, the full explanation must be more complex. Accumulating experience suggests that systemic antibody can be beneficial for patients with brain metastases or with other targets in the brain. How can this be the case if access is blocked by the BBB? If access is not in fact limiting, how is late failure in the brain to be explained, especially when it occurs in parallel with tumor control at other sites?9–11
The questions above set the context for this review. To address them, brain tumors (the target), antibodies (the magic), how antibodies attack tumor (the bullet) and how they reach it (the barrier) are reviewed in turn. With this as background, practical experience with mAbs for brain tumor targets is re-visited (the findings) and ways to go forward are suggested (the future). As will be brought out, the special problems posed by the BBB are balanced by more general concerns. Indeed, one aspect of “getting past the BBB” will be to give greater attention to problems that are shared with other tumor sites.
The Target: Tumor in the Brain
Three tumor types.
Three brain tumor types, each coupled to a mAb that has already been used extensively outside the brain, are discussed below (Table 1). Together, these antibody/target combinations illustrate different challenges to using mAbs and to interpreting their effects against targets in the brain.
Table 1.
Tumor/antibody combinations emphasized in the text
| Brain tumors discussed | Antibodies discussed | Target antigens | |||
| General type | Specific example | Name | How modified | Name | Unique to tumor? |
| glioma | GBMa | bevacizumab (Avastin) | humanized | VEGFc | No |
| lymphoma | PCNSLb | rituximab (Rituxan) | chimeric | CD20d | No |
| metastatic | breast cancer | trastuzumab (Herceptin) | humanized | Her2e | No |
GBM, glioblastoma multiforme
PCNSL, primary central nervous system lymphoma
VEGF, vascular endothelial growth factor
CD20, common B-cell antigen
Her2, human epidermal growth factor receptor 2
Glioma. Among primary brain tumors (those that arise within the brain), the high grade glioma, glioblastoma multiforme (GBM), is the most common and aggressive type in adults. As such, GBM has been the focus of much work with mAbs, as well as other new therapies.12–15
GBM has a complex growth pattern (Fig. 1). There is typically a tumor mass (or more than one) that is easily detected with conventional imaging. The tumor mass does not have a sharp border. Instead, individual tumor cells infiltrate the brain parenchyma and may be widely disseminated at the time of diagnosis. The tumor mass and the infiltrative component present different challenges to mAb therapy.12,15 Experience with bevacizumab draws attention to the many possible effects of a single antibody, especially when coupled to heterogeneity within the tumor itself.
Figure 1.
Two patterns of tumor growth in the brain. Tumor often grows around blood vessels (left), but some tumors can also infiltrate the brain parenchyma (right).
Lymphoma. The second tumor emphasized, primary central nervous system lymphoma (PCNSL), is also considered “primary” because it is normally confined to the central nervous system (CNS); the actual origin is not known.16–18 PCNSL occurs in two very different contexts: in patients with AIDS or other forms of immunosuppression and also in immunocompetent patients.17–19 Although there are important differences between PCNSL in these different contexts, one common feature is that, like other lymphoid cells, normal or neoplastic, PCNSL can infiltrate the brain parenchyma.16–19 A second common feature is that PCNSL is most often derived from B cells.17–19
Rituximab, first used against B-cell lymphomas outside the brain, is now being used in related contexts in the CNS. Its use brings out aspects of antibody specificity that are relevant for any tumor, at any site, as well as practical difficulties in interpretation for targets in the brain.
Metastatic. Blood-borne metastases from other organs are many-fold more frequent than primary brain tumors; the most common sources are tumors of the lung and breast.9 For many tumors of origin, parenchymal metastases remain (at least initially) in the perivascular space (PVS);20 the infiltrative growth that is characteristic of glial brain tumors or PCNSL is not seen. Another difference from primary brain tumors is that, when patients appear to benefit from systemic mAb, the site of attack can be questioned; efficacy may reflect better control of systemic tumor, rather than of tumor in the brain itself. Interpretation of apparent benefit from systemic trastuzumab, used against human epidermal growth factor receptor 2 (Her2)-overexpressing metastatic breast cancer, suggests this possibility.
Some common features.
Need for new therapies. For each of the tumors described above, new therapies are needed. With current therapy, the median survival after diagnosis of GBM is less than 15 months;12,13,15,21,22 survival can be similar or even shorter after diagnosis of brain metastases,23 or after relapse of PCNSL.19
Micro-tumor targets. Microscopic tumor (or micro-tumor), tumor too small to be readily imaged by conventional methods, is an important component of many brain tumors, including those stressed here. For GBM or other glial brain tumors, infiltrative tumor is known to remain after a main tumor mass has been removed,12,15 PCNSL normally appears as a diffuse B-cell lymphoma17 and blood-borne tumor from other organs first enters the brain as micro-metastases.
For the many cases where it is known that micro-tumor is likely to be present somewhere in the brain, but not exactly where, localized therapies are not appropriate. This increases interest in agents such as mAbs that are less inherently toxic than the conventional therapies,24,25 and so safer for widespread delivery. For tumor outside the brain, a complementary attraction is that most therapies are thought most likely to succeed against micro-tumor, as opposed to larger masses.26 A confounding factor in the brain is that the BBB is closest to normal, and therefore most effective at blocking antibody access, at micro-tumor sites. A related problem is that, although the importance of brain micro-tumor is widely acknowledged, it is rarely targeted explicitly in pre-clinical work.27,28
The challenges of treating brain tumor targets are well illustrated by experience with the mAbs listed in Table 1. Before turning to the clinical findings, it is useful to briefly review properties of the mAbs themselves.
The Magic: What Tumor-Specific Can Mean
Although antibody specificity is indeed exquisite,29 few determinants are limited to tumor cells (Fig. 2).24,30 Fortunately, shared molecules can serve as practical tumor targets and this is true for each molecule targeted by the mAbs in Table 1.
Figure 2.
Distribution of tumor antigens. A tumor cell displays a characteristic combination of components, many of which are also expressed by normal cells. Even though they may not be unique to the tumor, shared antigens can serve as practical tumor targets.
Each B-cell lymphoma expresses a unique idiotype, and this may well be the target of choice in the long term.31 Rituximab, in contrast, recognizes a common B-cell antigen, CD20, that is expressed by both normal and neoplastic B cells. At present, the advantage of rituximab is that it can be used for many different patients, coupled to the fact that the depletion of normal B cells can be tolerated because existing antibody and antibody-forming plasma cells are spared, other protective mechanisms remain active and B cells are eventually replaced.32,33
Although more restricted antigens are known for GBM,34 there has been enormous interest in using bevacizumab to target vascular endothelial growth factor (VEGF), which promotes angiogenesis for tumors, but also in normal wound healing.35 Trastuzumab targets Her2, which is overexpressed in many breast cancers, but also expressed by normal cells.1,24,36 In practice, each of these three mAbs has been used successfully against tumor outside the brain1–8 and, increasingly, is being used against brain tumor targets.
Although targets need not be limited to strict tumor-specific antigens, cross-reactions may cause problems for individual patients. More generally, the problem of resistance is increasingly acknowledged.2,4,12,37,38 For any given mAb, a tumor cell can escape attack at many levels, from its expression of the target determinant, to its susceptibility to the final effector mechanism.12,31,37–39 Probing the basis of resistance is complicated by uncertainty as to which, among many possibilities, are the most important effector mechanisms for a given mAb, tumor and site.
The Bullet: What Antibodies Can Do
Antibodies can lead to death or arrest of a tumor target in a great and growing variety of ways, with new antibody-mediated functions still being identified. Antibodies can directly block activity of a target molecule simply by binding to it, through the antibody variable region,36,40 while additional functions are brought to bear if the constant (Fc) region is engaged. The benefits of Fc binding to elements of the complement cascade or cell-bound Fc receptors are well known.36,40 More recently appreciated is that another kind of Fc receptor, FcRn, binds to an antibody in a way that protects it from degradation. This contributes to the prolonged serum half-life of an antibody, as compared to that of most other proteins.26,41
An antibody need not attack tumor cells themselves. Bevacizumab, which is intended to block development of a tumor's blood supply, is an example.35 Also, the antibody does not necessarily need to attack its target in the brain. Blood-borne tumor or other targets may be attacked before they reach the brain. Complexes between an antibody and its target antigen can stimulate the patient's own immune response or mAbs can modulate an ongoing response.30,38,42 Complementing these spontaneous activities, additional effector mechanisms come into play when mAbs are coupled to agents, such as radionuclides or toxins,24,40 or larger molecules or particles (liposomes, nanoparticles),24,43–45 so that the mAb serves a targeting function and the other component provides (or adds to) the attack mechanism. The sequence of the antibody protein itself may be modified to alter target binding or constant region functions,42 or avoid having the antibody recognized as a foreign protein by the patient's immune system. All three antibodies discussed here were modified to reduce such recognition (Table 1).40 The variety of possible effector mechanisms is multiplied as antibodies are used in combination with other agents or modalities.37 Of particular relevance for brain tumor, radiotherapy is thought to alter the BBB in ways that increase antibody access to tumor sites.23,44
Even where antibody-mediated therapy has been most successful, the key effector mechanisms are not yet known.2,6,32,35,36,38,40 Not only is there a wealth of possibilities, but the balance of effector functions may differ at different tumor sites.12 The frequent use of combination therapies and the potential long-term effects of previous treatments further increase the difficulty of defining the effect of a given antibody. There may also be uncertainty as to where an antibody exerts its effects, for example, whether metastatic tumor is attacked at its source, en route or at its final site. In the brain, interpretation is further impeded by the difficulty of directly analyzing the tumor site. These uncertainties, in turn, complicate interpretation of the role of the BBB.
The Barrier: How Entry to the Brain is Controlled
The ability of the BBB to block passive entry of therapeutics into the normal brain is well known; however, understanding of the BBB, even in the normal brain, is still evolving. The BBB is dynamic and can be manipulated; unfortunately, it is not the only impediment.
Entry to normal brain.
What impedes entry. In the brain parenchyma, the anatomical BBB is formed by specialized tight junctions between the endothelial cells of cerebral micro-vessels, together with astrocyte endfeet that abut the endothelium, adjacent pericytes and a characteristic composition of the extracellular matrix (ECM). This anatomical barrier is complemented by a physiological barrier that includes reduced pinocytosis by the endothelial cells (as compared to other tissues), degradative enzymes and transporters that act as efflux pumps to actively return many kinds of molecules, including many drugs, to the blood. Other CNS compartments have variations of these properties, so that the brain environment remains controlled.45–47
What allows entry. As effective as the BBB is in preventing unregulated entry of substances from the blood, it is equally effective at selectively permitting entry of necessary components. Active transporters import nutrients and regulatory molecules.44–47 One approach to delivering agents to the brain is to exploit these transporters.44,45
Of special relevance for antibody therapeutics, FcRn, the Fc receptor that protects antibodies from degradation in serum, is highly expressed on brain vessels.41 In other organs, another function of FcRn is to transport antibody across tissue barriers. For the brain, a role in removal of harmful antibody from the brain has been suggested,41,42 but the actual roles are not yet known. In other tissues, FcRn-mediated transport is bi-directional, and the predominant direction can be modified experimentally.48 It is intriguing to consider whether FcRn might also act to bring antibody into brain tumor sites—or might be exploited for that purpose.
Entry to tumor sites.
Not static. The BBB is dynamic, its properties specified and maintained by reciprocal interactions with adjacent cells. BBB properties change during development and other normal processes, as well as in the context of inflammation or other pathology,45–47,49 including tumor growth.44,50 The BBB may be essentially normal at micro-tumor sites; as the tumor grows, the BBB is progressively disrupted. Ultimately, new vessels may be formed and the tumor itself modulates their properties.50 Indeed, for brain metastases, tumor-adjacent vessels may resemble abnormal versions of vessels in the tissue of origin, rather than brain barrier vessels.44,50
Not the only impediment. When primary or metastatic brain tumor can be imaged by a contrasting-enhancing agent, typically gadolinium, the vessels must be at least leaky enough to permit the agent's extravasation. Unfortunately, this does not necessarily imply effective delivery of mAbs. Even in the normal brain, the distribution of a given molecule will vary with its size, shape, charge, composition (such as lipophilicity) and the extent to which it binds to blood components or tissue.26,45,46 As two examples of the relevance of these factors, antibodies are much larger than gadolinium23 and many drugs bind tightly to serum proteins.50 An important consequence is that the distribution of a contrast-enhancing agent does not necessarily reflect the distribution of therapeutic agents.
Tumor-associated vessels may be leaky, but are also tortuous and chaotic, so that, even if blood-borne molecules do leave the vessel, they may not be evenly distributed within the tumor. Factors such as an unfavorable pressure gradient and the nature of the extracellular matrix can impede the ability of therapeutics, including antibodies, to become well-distributed within a tumor mass, while the center of a large tumor can act as a sink.26,44,50,51 In GBM in particular, blood-borne agents will accumulate in the necrotic center, with its disrupted BBB, rather than at the infiltrative edge, where the BBB is more like that of normal brain.50 Properties of the tumor cell itself can further impede antibody binding or efficacy. Most of these factors are not unique to brain tumors; rather, they can impede the distribution or activity of antibody or other therapy against solid tumor at any site.26,40
In the brain, interpretation of antibody levels is hampered by the difficulty of taking local measurements. Instead, the concentration of therapeutic agents is often followed by measuring levels in cerebrospinal fluid (CSF). This approach does not take into account anatomic and metabolic heterogeneity even within the normal brain, and potential inaccuracy is additionally compounded by heterogeneity among tumor sites.44,46,49,52 Even at a single site, antibody access can change with time. As tumor either responds to therapy or continues to grow, the BBB itself, as well as the other impediments to antibody access, will change accordingly.17,18,53
The Findings: Experience with Three Brain Tumor/Antibody Pairs
The topics discussed so far provide a context for reviewing clinical experience with mAbs in brain tumor therapy. Three of the best-studied antibody/target combinations (Table 1) illustrate specific details.
Bevacizumab and GBM.
The original intention was that bevacizumab would bind VEGF and so attack the highly vascular main tumor mass indirectly, by depriving it of its blood supply.15,35,54 In practice, the antibody does affect tumor blood vessels, reducing their leakiness and other abnormal properties. Benefits of this vessel normalization include reduced edema and intracranial pressure, which permits reduced steroid use,15,54 and perhaps also protection against radiation necrosis.55,56
The effect on tumor growth per se has been hard to interpret. Because it affects blood vessels, bevacizumab also affects extravasation of the contrast agents used to image a tumor mass. In this situation, improvement in the radiographic image can be misleading: It may simply reflect reduced extravasation of the contrast agent rather than tumor control.15
The disseminated components of GBM present complementary challenges. Individual infiltrative cells do not depend on angiogenesis.15 On the contrary, it has been suggested that, in response to bevacizumab, infiltrative growth, as well as other forms of parenchymal invasion, may even be increased.15,22,54,57 The effect of bevacizumab on drug delivery is also complex. Normalizing the vessels may improve distribution of blood-borne agents within a tumor mass,50 but may also impede their extravasation, by restoring the BBB.15
More general factors, not limited to brain tumors, also impede interpretation of an antibody's effects. Many reports of brain tumor findings concern small studies and many depend on historical controls.15,21,22 Moreover, the antibody is normally part of a complex regimen, including surgery, radiation and chemotherapy, and is often given in combination with (further) chemotherapy.15,21,22 All these factors make it hard to define the effect of the antibody itself on tumor growth. Other questions concern response criteria. How to weigh overall survival as opposed to progression-free survival; the possibility that high statistical significance may reflect relatively small quantitative differences in the response and the possibility that a responsive subgroup may go undetected are concerns that apply to all tumors. When there is apparent benefit, the same limitations seen in other contexts apply: as with other tumors, benefits of bevacizumab for GBM patients are transient.22,54 As happens after treatment with other new therapies, GBM normally recurs.22
Rituximab and PCNSL.
Rituximab targets the common B-cell marker CD20. Outside the brain, it shows efficacy in patients with different kinds of B-cell lymphoma.5,6 In the brain, its specificity is appropriate for PCNSL, which is typically a B-cell lymphoma. On the other hand, the BBB is likely to block antibody access to sites of infiltrative tumor, and this is also typical of PCNSL. This suggests that full efficacy may require actively delivering antibody across the BBB.44,51,52
In practice, the potential efficacy of rituximab against PCNSL, with or without BBB opening, is not yet known. Although increasing, PCNSL is still rare;18 most reports of rituximab use describe small studies and the antibody is often given as part of a complex therapy, without internal controls.53,58 Given these limitations, work in a related context is relevant.
Systemic rituximab has shown efficacy for patients with autoimmune diseases, especially multiple sclerosis (MS), where B cells are thought to contribute to pathology.32,59 In this case, interpretation is aided by simpler treatments and well-controlled studies. Although rituximab shows efficacy in MS, the mechanism and sites of action are not known. In particular, because autoimmune B cells must enter the brain from the blood, efficacy does not necessarily reflect attack of targets in the brain.59
Trastuzumab and metastastic breast cancer.
The challenge of late brain metastases. As use of trastuzumab for Her2-overexpressing breast cancer became widespread, a troubling finding was an apparent increase in brain metastases.3,10,23,60 The reasons are not known. Brain metastases are typically a late occurrence in breast cancer,10,23,60,61 and so longer survival itself is relevant.3,23,60 The BBB is often assumed to be important;10,23,60,61 however, its role depends upon a point that is often not explicitly discussed: Brain metastases often occur in parallel with tumor control at other sites.9,10 If the patient has responded to antibody therapy in the periphery, what can be the source of the newly-detected brain metastases? Two possibilities imply different roles for the BBB (Fig. 3).
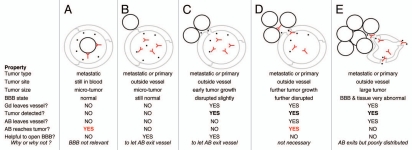
Figure 3.
A varied role for the BBB. Possible relationships among tumor (black circles), gadolinium (Gd, black dots), antibody (AB, Y shapes), blood vessels (grey) and the blood-brain barrier (BBB), under different conditions of tumor growth are depicted.
Model 1. New blood-borne tumor. Late brain metastases may represent new blood-borne tumor from outside the brain, perhaps from known sites of apparently stable disease or from undetected, dormant tumor elsewhere. Eventually, this tumor begins to grow and provides a source of new blood-borne metastases.62 In this case, if systemic mAb therapy is continued even after tumor is no longer detected in the periphery, it may attack the potential brain metastases at their original site or in the blood (Fig. 3A), before the tumor even enters the brain; the BBB need not be involved. Since this tumor has escaped that particular mAb in the periphery, switching to a different therapeutic agent may be preferable. Of course, once the tumor enters the brain, the role of the BBB would change as the tumor grows, just as in Model 2.
Model 2. Dormant tumor in the brain. As an alternative scenario, tumor may have entered the brain long before it is detected and remained, undetected, as micro-metastases3 in a dormant state. As long as the BBB is close to normal, then contrast-enhancing agents, such as gadolinium, would not reveal this tumor and antibody therapeutics would not reach it (Fig. 3B). Once the tumor begins to grow, the BBB might initially be compromised enough for gadolinium, but not antibodies, to extravasate (Fig. 3C). The tumor could thus be detected radiographically, but not treated.
As the tumor continues to grow, the barrier will break down further and antibody may then extravasate (Fig. 3D). Therefore, if the same mAb treatment is continued, it may show efficacy eventually. Actively delivering the antibody across the BBB should allow for an earlier response. If the tumor grows too large before antibody is given, impediments besides the BBB will become increasingly important in blocking distribution of the antibody, even if it does leave the vessel (Fig. 3E).
The ability of systemic antibody to help control brain metastases would thus vary with the tumor's current site (that is, whether or not is was already in the brain) and size, as depicted in Figure 3 as idealized examples. Brain metastases are heterogeneous, even within an individual,20 and may differ in the time of entry to the brain, susceptibility to the antibody in question and BBB status; moreover, each of these factors can change with time. Even with these caveats, the models compared above can help to interpret clinical findings, especially partial or disappointing responses.
In practice. Several authors have suggested that systemic antibody should be continued after brain metastases are detected in breast cancer patients and evidence of benefit has been reported.63–67 Interpretation is complicated by the same factors discussed above: Many studies are small or anecdotal and multiple modalities or agents may be involved. When there is apparent benefit, the key sites are not known. As many authors discuss, benefit from systemic antibody may simply reflect better control of systemic disease; it does not necessarily reflect direct attack of tumor in the brain.63–65,67 In practice, the potential for direct attack is likely to vary among different metastases and to change with time (Fig. 3).
Summary of clinical experience.
There is evidence that systemic mAb treatment can benefit patients with brain tumors or other CNS pathology. The nature and site of antibody activity are less clear. The extent to which antibody enters—and acts at—tumor sites within the brain itself is not known. A conservative interpretation is that bevacizumab primarily reduces edema, and rituximab and trastuzumab act primarily on systemic targets. The complexity of tumor therapy, difficulty of direct local measurements, limitations of clinical trials and drawbacks of pre-clinical models all complicate interpretation of clinical results. Regardless of whether the antibody acted in the brain or elsewhere, an increase in overall or progression-free survival, or simply an improved quality of life, are certainly of benefit to brain tumor patients. The goals for the future are, as for all tumors, to increase the benefit and reduce the cost of the therapeutics.
Related topics.
The text has emphasized disseminated tumor within the brain, for which systemic delivery of mAbs is especially relevant. The focus has been on the role of the BBB, rather than specific strategies to overcome it,44,45,51,52 or cases, such as meningeal tumor, where other delivery routes are of special interest.68,69 The points raised should help to interpret findings for a variety of delivery strategies and tumor sites.
The Future
The natural evolution of mAb therapy for any tumor at any site is towards redundancy and refinement. Redundancy, in the sense that alternative targets are identified and alternative antibodies are prepared against promising targets, old or new. Refinement, in the sense that the new antibodies can be designed to solve specific problems: to avoid known cross-reactions or to work by means of alternative effector mechanisms. Refinement of another kind will come from combining therapies in more directed ways, in parallel with growing understanding of the underlying mechanisms of tumor growth, susceptibility and resistance. Combined targeting of a GBM tumor mass plus infiltrative tumor or existing brain metastases plus tumor that has not yet reached the brain are obvious examples. Improved clinical trial design will be important for all tumors,70 as will more predictive pre-clinical models.27,28
As for mAbs themselves, two parallel approaches are each likely to be fruitful. One is to continue to refine the specificity and modifications of the antibody molecule itself. The other is to synthesize novel agents, using knowledge of antibody structure and function as a guide.71 Even as novel agents evolve, the whole antibody molecule still has great value. It has a long half-life and can mediate multiple functions, with new functions and uses still being identified. Indeed, the key mechanisms used by even the most successful antibodies in human patients are not yet established.
For all solid tumors, a complementary evolution of both understanding and technology is needed to improve delivery of therapeutics to larger tumor masses. For the brain, where delivery to micro-tumor is an equal challenge, clearer understanding of the nature and role of the BBB, complemented by improved methods for opening or bypassing it when necessary, have been long-standing goals.44,51 A third approach has received less attention: In other clinical contexts, sustained antibody synthesis occurs within the CNS.32,59 This too should be exploitable for brain tumor patients.72
In the long run, how will mAb therapeutics benefit brain tumor patients? We may depend on antibody itself, a fragment or a synthetic alternative; the agent may be delivered passively or actively made within the brain; it may attack brain tumor directly or “only” targets outside the brain (such as blood-borne metastases or tumor vasculature); or even less directly, it may act to simulate or modify an endogenous response. Most likely, each variation will have its role. In planning and interpreting antibody therapy, the BBB has rightly commanded attention, yet its importance is balanced by that of more general problems of access and resistance. Going forward, a matching focus on challenges that are common to other agents, other tumors and other sites will be a complementary way of getting past the BBB.
Acknowledgements
I thank Cara Tripp for help with Figure 1 and comments on the text.
Abbreviations
- ADCC
antibody-dependent cell-mediated cytotoxicity
- BBB
blood-brain barrier
- CDC
complement-dependent cytotoxicity
- CNS
central nervous system
- CSF
cerebrospinal fluid
- ECM
extracellular matrix
- GBM
glioblastoma multiforme
- MS
multiple sclerosis
- PCNSL
primary central nervous system lymphoma
- PVS
perivascular space
- VEGF
vascular endothelial growth factor
References
- 1.Bria E, Cuppone F, Fornier M, Nistico C, Carlini P, Milella M, et al. Cardiotoxicity and incidence of brain metastases after adjuvant trastuzumab for early breast cancer: the dark side of the moon?? A meta-analysis of the randomized trials. Breast Cancer Res Treat. 2008;109:231–239. doi: 10.1007/s10549-007-9663-z. [DOI] [PubMed] [Google Scholar]
- 2.Nielsen DL, Andersson M, Kamby C. HER2-targeted therapy in breast cancer. Monoclonal antibodies and tyrosine kinase inhibitors. Cancer Treat Rev. 2009;35:121–136. doi: 10.1016/j.ctrv.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Viani GA, Afonso SL, Stefano EJ, De Fendi LI, Soares FV. Adjuvant trastuzumab in the treatment of her-2-positive early breast cancer: a meta-analysis of published randomized trials. BMC Cancer. 2007;7:153. doi: 10.1186/1471-2407-7-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Widakowich C, Dinh P, de Azambuja E, Awada A, Piccart-Gebhart M. HER-2 positive breast cancer: what else beyond trastuzumab-based therapy? Anticancer Agents Med Chem. 2008;8:488–496. doi: 10.2174/187152008784533062. [DOI] [PubMed] [Google Scholar]
- 5.Cheung MC, Haynes AE, Meyer RM, Stevens A, Imrie KR. Rituximab in lymphoma: a systematic review and consensus practice guideline from Cancer Care Ontario. Cancer Treat Rev. 2007;33:161–176. doi: 10.1016/j.ctrv.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Racila E, Link BK, Weng WK, Witzig TE, Ansell S, Maurer MJ, et al. A polymorphism in the complement component C1qA correlates with prolonged response following rituximab therapy of follicular lymphoma. Clin Cancer Res. 2008;14:6697–6703. doi: 10.1158/1078-0432.CCR-08-0745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eskens FA, Sleijfer S. The use of bevacizumab in colorectal, lung, breast, renal and ovarian cancer: where does it fit? Eur J Cancer. 2008;44:2350–2356. doi: 10.1016/j.ejca.2008.07.042. [DOI] [PubMed] [Google Scholar]
- 8.Los M, Roodhart JM, Voest EE. Target practice: lessons from phase III trials with bevacizumab and vatalanib in the treatment of advanced colorectal cancer. Oncologist. 2007;12:443–450. doi: 10.1634/theoncologist.12-4-443. [DOI] [PubMed] [Google Scholar]
- 9.Kaal EC, Vecht CJ. CNS complications of breast cancer: current and emerging treatment options. CNS Drugs. 2007;21:559–579. doi: 10.2165/00023210-200721070-00003. [DOI] [PubMed] [Google Scholar]
- 10.Yau T, Swanton C, Chua S, Sue A, Walsh G, Rostom A, et al. Incidence, pattern and timing of brain metastases among patients with advanced breast cancer treated with trastuzumab. Acta Oncol. 2006;45:196–201. doi: 10.1080/02841860500486630. [DOI] [PubMed] [Google Scholar]
- 11.Azar JM, Schneider BP, Einhorn LH. Is the blood-brain barrier relevant in metastatic germ cell tumor? Int J Radiat Oncol Biol Phys. 2007;69:163–166. doi: 10.1016/j.ijrobp.2007.02.042. [DOI] [PubMed] [Google Scholar]
- 12.Lampson LA. Targeted therapy for neuro-oncology: reviewing the menu. Drug Discov Today. 2009;14:185–191. doi: 10.1016/j.drudis.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Minniti G, Muni R, Lanzetta G, Marchetti P, Enrici RM. Chemotherapy for glioblastoma: current treatment and future perspectives for cytotoxic and targeted agents. Anticancer Res. 2009;29:5171–5184. [PubMed] [Google Scholar]
- 14.Omuro AM, Faivre S, Raymond E. Lessons learned in the development of targeted therapy for malignant gliomas. Mol Cancer Ther. 2007;6:1909–1919. doi: 10.1158/1535-7163.MCT-07-0047. [DOI] [PubMed] [Google Scholar]
- 15.Verhoeff JJ, van Tellingen O, Claes A, Stalpers LJ, van Linde ME, Richel DJ, et al. Concerns about anti-angiogenic treatment in patients with glioblastoma multiforme. BMC Cancer. 2009;9:444. doi: 10.1186/1471-2407-9-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aho R, Ekfors T, Haltia M, Kalimo H. Pathogenesis of primary central nervous system lymphoma: invasion of malignant lymphoid cells into and within the brain parenchyme. Acta Neuropathol. 1993;86:71–76. doi: 10.1007/BF00454901. [DOI] [PubMed] [Google Scholar]
- 17.Bessell EM, Hoang-Xuan K, Ferreri AJ, Reni M. Primary central nervous system lymphoma: biological aspects and controversies in management. Eur J Cancer. 2007;43:1141–1152. doi: 10.1016/j.ejca.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Mohile NA, Abrey LE. Primary central nervous system lymphoma. Semin Radiat Oncol. 2007;17:223–229. doi: 10.1016/j.semradonc.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Ferreri AJ, Reni M. Primary central nervous system lymphoma. Crit Rev Oncol Hematol. 2007;63:257–268. doi: 10.1016/j.critrevonc.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 20.Takahashi JA, Llena JF, Hirano A. Pathology of cerebral metastases. Neurosurg Clin N Am. 1996;7:345–367. [PubMed] [Google Scholar]
- 21.Poulsen HS. Grunnet K, Sorensen M, Olsen P, Hasselbalch B, Nelausen K, et al. Bevacizumab plus irinotecan in the treatment patients with progressive recurrent malignant brain tumours. Acta Oncol. 2009;48:52–58. doi: 10.1080/02841860802537924. [DOI] [PubMed] [Google Scholar]
- 22.Zuniga RM, Torcuator R, Jain R, Anderson J, Doyle T, Ellika S, et al. Efficacy, safety and patterns of response and recurrence in patients with recurrent high-grade gliomas treated with bevacizumab plus irinotecan. J Neurooncol. 2009;91:329–336. doi: 10.1007/s11060-008-9718-y. [DOI] [PubMed] [Google Scholar]
- 23.Stemmler HJ, Heinemann V. Central nervous system metastases in HER-2-overexpressing metastatic breast cancer: a treatment challenge. Oncologist. 2008;13:739–750. doi: 10.1634/theoncologist.2008-0052. [DOI] [PubMed] [Google Scholar]
- 24.Siu D. Cancer therapy using tumor-associated antigens to reduce side effects. Clin Exp Med. 2009;9:181–198. doi: 10.1007/s10238-009-0047-z. [DOI] [PubMed] [Google Scholar]
- 25.Chung CH. Managing premedications and the risk for reactions to infusional monoclonal antibody therapy. Oncologist. 2008;13:725–732. doi: 10.1634/theoncologist.2008-0012. [DOI] [PubMed] [Google Scholar]
- 26.Beckman RA, Weiner LM, Davis HM. Antibody constructs in cancer therapy: protein engineering strategies to improve exposure in solid tumors. Cancer. 2007;109:170–179. doi: 10.1002/cncr.22402. [DOI] [PubMed] [Google Scholar]
- 27.Lampson LA. New animal models to probe brain tumor biology, therapy and immunotherapy: advantages and remaining concerns. J Neurooncol. 2001;53:275–287. doi: 10.1023/a:1012230113527. [DOI] [PubMed] [Google Scholar]
- 28.Lampson LA. Beyond new models: What else we need. In: Martinez R, editor. Animal Models of Brain Tumors. Humana; In press. [Google Scholar]
- 29.Lampson L. Molecular bases of neuronal individuality: Lessons from anatomical and biochemical studies with monoclonal antibodies. In: Kennet R, et al., editors. Monoclonal Antibodies and Functional Cell Lines: Progress and Applications. Plenum Press; 1984. pp. 153–189. [Google Scholar]
- 30.Dougan M, Dranoff G. Immune therapy for cancer. Annu Rev Immunol. 2009;27:83–117. doi: 10.1146/annurev.immunol.021908.132544. [DOI] [PubMed] [Google Scholar]
- 31.Houot R, Levy R. Vaccines for lymphomas: idiotype vaccines and beyond. Blood Rev. 2009;23:137–142. doi: 10.1016/j.blre.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 32.Dalakas MC. Invited article: inhibition of B cell functions: implications for neurology. Neurology. 2008;70:2252–2260. doi: 10.1212/01.wnl.0000313840.27060.bf. [DOI] [PubMed] [Google Scholar]
- 33.Neelapu SS, Kwak LW, Kobrin CB, Reynolds CW, Janik JE, Dunleavy K, et al. Vaccine-induced tumor-specific immunity despite severe B-cell depletion in mantle cell lymphoma. Nat Med. 2005;11:986–991. doi: 10.1038/nm1290. [DOI] [PubMed] [Google Scholar]
- 34.Saikali S, Avril T, Collet B, Hamlat A, Bansard JY, Drenou B, et al. Expression of nine tumour antigens in a series of human glioblastoma multiforme: interest of EGFRvIII, IL-13Ralpha2, gp100 and TRP-2 for immunotherapy. J Neurooncol. 2007;81:139–148. doi: 10.1007/s11060-006-9220-3. [DOI] [PubMed] [Google Scholar]
- 35.Sathornsumetee S, Rich JN. Antiangiogenic therapy in malignant glioma: promise and challenge. Curr Pharm Des. 2007;13:3545–3558. doi: 10.2174/138161207782794130. [DOI] [PubMed] [Google Scholar]
- 36.Spector NL, Blackwell KL. Understanding the mechanisms behind trastuzumab therapy for human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol. 2009;27:5838–5847. doi: 10.1200/JCO.2009.22.1507. [DOI] [PubMed] [Google Scholar]
- 37.Reslan L, Dalle S, Dumontet C. Understanding and circumventing resistance to anticancer monoclonal antibodies. mAbs. 2009;1:222–229. doi: 10.4161/mabs.1.3.8292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bello C, Sotomayor EM. Monoclonal antibodies for B-cell lymphomas: rituximab and beyond. Hematology Am Soc Hematol Educ Program. 2007:233–242. doi: 10.1182/asheducation-2007.1.233. [DOI] [PubMed] [Google Scholar]
- 39.Davis TA, Czerwinski DK, Levy R. Therapy of B-cell lymphoma with anti-CD20 antibodies can result in the loss of CD20 antigen expression. Clin Cancer Res. 1999;5:611–615. [PubMed] [Google Scholar]
- 40.Strome SE, Sausville EA, Mann D. A mechanistic perspective of monoclonal antibodies in cancer therapy beyond target-related effects. Oncologist. 2007;12:1084–1095. doi: 10.1634/theoncologist.12-9-1084. [DOI] [PubMed] [Google Scholar]
- 41.Roopenian DC, Akilesh S. FcRn: the neonatal Fc receptor comes of age. Nat Rev Immunol. 2007;7:715–725. doi: 10.1038/nri2155. [DOI] [PubMed] [Google Scholar]
- 42.Ward ES, Ober RJ. Chapter 4: Multitasking by exploitation of intracellular transport functions the many faces of FcRn. Adv Immunol. 2009;103:77–115. doi: 10.1016/S0065-2776(09)03004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beduneau A, Saulnier P, Benoit JP. Active targeting of brain tumors using nanocarriers. Biomaterials. 2007;28:4947–4967. doi: 10.1016/j.biomaterials.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 44.Deeken JF, Loscher W. The blood-brain barrier and cancer: transporters, treatment and Trojan horses. Clin Cancer Res. 2007;13:1663–1674. doi: 10.1158/1078-0432.CCR-06-2854. [DOI] [PubMed] [Google Scholar]
- 45.Saunders NR, Ek CJ, Habgood MD. Dziegielewska KM, Barriers in the brain: a renaissance? Trends Neurosci. 2008;31:279–286. doi: 10.1016/j.tins.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Eyal S, Hsiao P, Unadkat JD. Drug interactions at the blood-brain barrier: fact or fantasy? Pharmacol Ther. 2009;123:80–104. doi: 10.1016/j.pharmthera.2009.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choi YK, Kim KW. Blood-neural barrier: its diversity and coordinated cell-to-cell communication. BMB Rep. 2008;41:345–352. doi: 10.5483/bmbrep.2008.41.5.345. [DOI] [PubMed] [Google Scholar]
- 48.Kuo TT, de Muinck EJ, Claypool SM, Yoshida M, Nagaishi T, Aveson VG, et al. N-glycan moieties in neonatal Fc receptor determine steady-state membrane distribution and directional transport of IgG. J Biol Chem. 2009;284:8292–8300. doi: 10.1074/jbc.M805877200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hermann DM. Biodistribution processes as underestimated confounders in translational stroke research. Curr Med Chem. 2007;14:3179–3184. doi: 10.2174/092986707782793817. [DOI] [PubMed] [Google Scholar]
- 50.Gerstner ER, Fine RL. Increased permeability of the blood-brain barrier to chemotherapy in metastatic brain tumors: establishing a treatment paradigm. J Clin Oncol. 2007;25:2306–2312. doi: 10.1200/JCO.2006.10.0677. [DOI] [PubMed] [Google Scholar]
- 51.Bellavance MA, Blanchette M, Fortin D. Recent advances in blood-brain barrier disruption as a CNS delivery strategy. AAPS J. 2008;10:166–177. doi: 10.1208/s12248-008-9018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Doolittle ND, Jahnke K, Belanger R, Ryan DA, Nance RW, Jr, Lacy CA, et al. Potential of chemo-immunotherapy and radioimmunotherapy in relapsed primary central nervous system (CNS) lymphoma. Leuk Lymphoma. 2007;48:1712–1720. doi: 10.1080/10428190701493902. [DOI] [PubMed] [Google Scholar]
- 53.Yilmaz M, Erkutlu I, Kilciksiz S, Pehlivan M, Okan V, Alptekin M, et al. Modified IDARAM chemotherapy regimen for primary central nervous system lymphoma: experience of three cases. Hematology. 2008;13:107–113. doi: 10.1179/102453308X315870. [DOI] [PubMed] [Google Scholar]
- 54.Kim WY, Lee HY. Brain angiogenesis in developmental and pathological processes: mechanism and therapeutic intervention in brain tumors. FEBS J. 2009;276:4653–4664. doi: 10.1111/j.1742-4658.2009.07177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu AK, Macy ME, Foreman NK. Bevacizumab as therapy for radiation necrosis in four children with pontine gliomas. Int J Radiat Oncol Biol Phys. 2009;75:1148–1154. doi: 10.1016/j.ijrobp.2008.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Torcuator R, Zuniga R, Mohan YS, Rock J, Doyle T, Anderson J, et al. Initial experience with bevacizumab treatment for biopsy confirmed cerebral radiation necrosis. J Neurooncol. 2009;94:63–68. doi: 10.1007/s11060-009-9801-z. [DOI] [PubMed] [Google Scholar]
- 57.Rubenstein JL, Kim J, Ozawa T, Zhang M, Westphal M, Deen DF, et al. Anti-VEGF antibody treatment of glioblastoma prolongs survival but results in increased vascular cooption. Neoplasia. 2000;2:306–314. doi: 10.1038/sj.neo.7900102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shah GD, Yahalom J, Correa DD, Lai RK, Raizer JJ, Schiff D, et al. Combined immunochemotherapy with reduced whole-brain radiotherapy for newly diagnosed primary CNS lymphoma. J Clin Oncol. 2007;25:4730–4735. doi: 10.1200/JCO.2007.12.5062. [DOI] [PubMed] [Google Scholar]
- 59.Hauser SL, Waubant E, Arnold DL, Vollmer T, Antel J, Fox RJ, et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med. 2008;358:676–688. doi: 10.1056/NEJMoa0706383. [DOI] [PubMed] [Google Scholar]
- 60.Cheng X, Hung MC. Breast cancer brain metastases. Cancer Metastasis Rev. 2007;26:635–643. doi: 10.1007/s10555-007-9083-x. [DOI] [PubMed] [Google Scholar]
- 61.Bos PD, Zhang XH, Nadal C, Shu W, Gomis RR, Nguyen DX, et al. Genes that mediate breast cancer metastasis to the brain. Nature. 2009;459:1005–1009. doi: 10.1038/nature08021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goss P, Allan AL, Rodenhiser DI, Foster PJ, Chambers AF. New clinical and experimental approaches for studying tumor dormancy: does tumor dormancy offer a therapeutic target? APMIS. 2008;116:552–568. doi: 10.1111/j.1600-0463.2008.001059.x. [DOI] [PubMed] [Google Scholar]
- 63.Bartsch R, Rottenfusser A, Wenzel C, Dieckmann K, Pluschnig U, Altorjai G, et al. Trastuzumab prolongs overall survival in patients with brain metastases from Her2 positive breast cancer. J Neurooncol. 2007;85:311–317. doi: 10.1007/s11060-007-9420-5. [DOI] [PubMed] [Google Scholar]
- 64.Bravo Marques JM. Treatment of brain metastases in patients with HER2+ breast cancer. Adv Ther. 2009;26:18–26. doi: 10.1007/s12325-009-0047-0. [DOI] [PubMed] [Google Scholar]
- 65.Church DN, Bahl A, Jones A, Price CG. HER2-positive breast cancer brain metastases: multiple responses to systemic chemotherapy and trastuzumab—a case report. J Neurooncol. 2006;79:289–292. doi: 10.1007/s11060-006-9139-8. [DOI] [PubMed] [Google Scholar]
- 66.Metro G, Sperduti I, Russillo M, Milella M, Cognetti F, Fabi A. Clinical utility of continuing trastuzumab beyond brain progression in HER-2 positive metastatic breast cancer. Oncologist. 2007;12:1467–1469. doi: 10.1634/theoncologist.12-12-1467. [DOI] [PubMed] [Google Scholar]
- 67.Park IH, Ro J, Lee KS, Nam BH, Kwon Y, Shin KH. Trastuzumab treatment beyond brain progression in HER2-positive metastatic breast cancer. Ann Oncol. 2009;20:56–62. doi: 10.1093/annonc/mdn539. [DOI] [PubMed] [Google Scholar]
- 68.Hong SJ, Kim JS, Chang JH, Kim KM, Kim SJ, Lee HW, et al. A successful treatment of relapsed primary CNS lymphoma patient with intraventricular rituximab followed by high-dose chemotherapy with autologous stem cell rescue. Yonsei Med J. 2009;50:280–283. doi: 10.3349/ymj.2009.50.2.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rubenstein JL, Combs D, Rosenberg J, Levy A, McDermott M, Damon L, et al. Rituximab therapy for CNS lymphomas: targeting the leptomeningeal compartment. Blood. 2003;101:466–468. doi: 10.1182/blood-2002-06-1636. [DOI] [PubMed] [Google Scholar]
- 70.Chow SC, Chang M. Adaptive design methods in clinical trials—a review. Orphanet J Rare Dis. 2008;3:11. doi: 10.1186/1750-1172-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dimitrov DS. Engineered CH2 domains (nanoantibodies) mAbs. 2009;1:26–28. doi: 10.4161/mabs.1.1.7480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lampson L, Tripp C. Antibody-secreting cells to deliver antibody against brain metastases. J Clinical Oncology. 2007;25:3047. [Google Scholar]