On the pass of Mt. Cenis, between France and Italy, is the “Chapelle des Transis,” a refuge dedicated many centuries ago to travelers frozen on their journeys through the Alps. Technological improvements have since reduced the hazards of winter life, but cold injury is still an important medical problem particularly in wartime, where under field conditions disability has often reached epidemic proportions.38
A review of 54 cases of frostbite treated during the past five years at the Colorado General and the Denver Veterans Administration Hospitals has convinced us that cold injury is an important medical problem within the civilian population as well. Hospitalization and rehabilitation constituted a heavy financial burden to the individual, his family and the community. Crippling amputations or late neurovascular complications often resulted.
The cases exhibited a wide spectrum of clinical manifestations ranging from mild erythema to totally destroyed extremities. It was apparent from the lack of uniformity in treatment regimens that no one mode of therapy has been accepted as entirely adequate. This fact emphasizes the lack of general agreement in many facets of the etiology, pathophysiology and proper care of this form of trauma.
Although no new basic information can be gained from a review of cases such as this, it does provide a convenient background to illustrate the complexities of the problem as it now exists in our civilian hospitals. At the same time, many aspects which require further concerted clinical and laboratory investigation under rigidly controlled conditions will become obvious. Various questions will be raised, many of which cannot be answered with certainty at the present time.
NOMENCLATURE AND CLASSIFICATION
What Is Cold Injury?
Cold injury is a composite term applied to a variety of hypothermic traumas which result in similar clinical and pathologic manifestations. The principal environmental factors leading to tissue injury are wetness and cold. Names given to the subdivisions of cold injury are arbitrary and have evolved on the basis of the circumstances of injury. Thus, frostbite is caused by exposure to freezing cold. The combination of nonfreezing cold and wetness produces trench foot, shelter foot and immersion foot.
The extent to which actual tissue freezing occurs in frostbite is controversial,32 except for the special circumstances of “high altitude frostbite”8 where intensely cold dry air freezes tissues within a few seconds. The usual victim of frostbite is not seen by a physician until long after the injured member has been thawed. In the present series, the shortest time between injury and medical examination was 30 minutes, but the average time was five and a half days. Commonly, the history is inadequate to determine whether solidification of the member has occurred. Occasionally, a patient will arrive at the hospital with actual tissue freezing still demonstrable.
Case I (CGH, 164687). A 27 year old man was driving while intoxicated. His car ran out of gas and he walked toward a nearby farmhouse, became tired and lay in a snowdrift to rest. He was found 7 or 8 hours later and brought immediately to the emergency room. Both hands and both feet as well as the ear and nose tips were frozen solid. He was admitted to the ward and allowed to warm in bed at room temperature which is kept at about 72° F. After thawing, which required several hours, the distal extremities were white (Fig. 1). Within 48 hours massive edema developed with proximal hyperemia. Gangrene developed extensively (Fig. 2). Eventually, he lost most of both feet and both hands.
Fig. 1.

(Case I). Hand and foot 24 hours after frostbite.
Fig. 2.

(Case I). Two weeks after injury.
The Gradients of Severity of Cold Injury
In frostbite from whatever cause, the injured member becomes white. Upon thawing, the sequence termed “the triple response” by Sir Thomas Lewis23 is observed. This consists of local skin reddening followed by a wheal at the site of injury, and subsequently by a flare in marginal tissues. In severe exposure, injury to muscles, large vessels, tendons, periosteum, bone and nerves is common. The presence and extent of gangrene is variable.
Since the Korean War, it has been customary to classify frostbite according to the extent of tissue damage.28
1st degree—Erythema and swelling with no blister formation
2nd degree—Blister or bleb formation
3rd degree—Full thickness injury with gangrene but without loss of a part
4th degree—Complete necrosis with loss of a part
Such a classification, which must be made in retrospect, is of limited value in assessing prognosis or planning care of the acute injury.
ETIOPATHOGENESIS
Individual Susceptibility as a Factor
Historically, certain groups of people have been noted to have an increased susceptibility to frostbite. This was recorded by Hippocrates1 in his tract, “On Airs, Waters and Places,” and in detail by Baron Larrey in his memoirs of the Napoleonic campaigns.21 Modern epidemiologic surveys have substantiated the role of psychic and personality factors in frostbite. Neurasthenic, poorly adjusted, badly motivated or excessively sweating soldiers were more prone to cold injury.37 Such factors were especially prominent in the 20 cases treated at the Denver Veterans Administration Hospital. Eleven patients had histories of chronic alcoholism and were inebriated when frozen. Of the combined series of 54 from both hospitals, 21 were intoxicated at the time of exposure. Generally, the patient went to sleep in the snow, in a car, or in an abandoned or unheated garage or house.
Case II (Denver VAH, A 5478). A 36 year old man was admitted 2 days after having become intoxicated and sleeping for 12 hours in an abandoned car. Outside temperature was −2° F. Army discharge diagnoses included anxiety neurosis and conversion hysteria. He was a known alcoholic. Gangrene of the tips of all toes developed. Eight months hospitalization was required for debridement and eventual multiple toe amputation.
Eleven of the 54 patients had been previously diagnosed as psychotic, most being chronic alcoholics in addition. The psychiatric diagnoses were either schizophrenia or paranoia. A recurrent theme, both in patients with and without a frank psychiatric disorder, was an unconcern about self-protection, as exemplified in Case III.
Case III (Denver VAH, A 3808). A 46 year old man was admitted on December 6, 1960, for the treatment of frostbite incurred while walking barefoot in the snow 5 days previously. Most of his toes were absent as the result of two prior frostbite incidents in 1958 and 1959. These had resulted from sleeping outdoors and walking in the snow without shoes. He was a known alcoholic with a duodenal ulcer. A previous psychiatric opinion was that he “indulged in willful self-destruction.” After a few hours, he released himself from the hospital. Five days later, he was found dead in the outskirts of a nearby town.
It should not be concluded from the foregoing remarks that all the patients were badly adjusted or inclined to place themselves in danger. In many cases, the exposure was obviously quite unavoidable. One 27 year old man was trapped beneath his car for 13 hours after an accident on a lonely road. Two nurses were frostbitten when forced to walk to safety from stalled cars. Varying degrees of frostbite are common among dedicated outdoor sports enthusiasts.
The importance of racial susceptibility has yet to be clarified. Studies in the Korean War indicate an increased risk of cold injury in Negroes.28,36 Conversely, Eskimos, Arctic fishermen and other inhabitants of northern geographic areas apparently have greater resistance to cold despite the fact that there is no consistently objective measurable difference in their response to reduced temperatures.7,14,15,26 It has been suggested that there is a tissue adaptation at the cellular level in response to the cold environment. Clever experimental proof of the value of cold acclimatization in the prevention of serious frostbite has recently been presented by Shikata, Shumacker and Nash.34 Rabbits kept at 21° F. for 50 days were found to be much less seriously injured by a standard frostbite than control animals which had been maintained in the usual laboratory domicile. Studies on human acclimatization to cold have been inconclusive.26
Environmental Factors
The final determinants of the severity of frostbite, excluding individual sensitivity as mentioned above, are the degree of cold penetrating the tissues and the length of time this cold is applied to the affected part.24 The environmental factors determining final tissue temperature are well known (Fig. 7). The first is the ambient temperature. In rabbits it was found that frostbite occurred where deep digital thermocouples indicated a temperature of less than 22° F.20 This figure is consonant with a study of Korean War injuries in which about 90 per cent of the cold injury cases occurred below 22° F.6 Of collateral importance are factors that increase heat loss by either conduction or convection, i.e., wetness, wind27 or contact with metal.
Fig. 7.

Pathophysiology of frostbite.
Case IV (Denver VAH, A 616). A 52 year old man entered the hospital 6 days after cold exposure of his hands. Without gloves, he had assisted in pushing a stalled car during subzero temperature. Superficial skin slough resulted, not requiring special treatment (Fig. 3).
Fig. 3.

(Case IV). Eight days after cold exposure.
Extensive studies by the armed forces have shown that the most effective clothing consists of layers of wool cloth beneath an outer garment of tightly woven windproof fabric. This makes use of the insulating properties of still air.38 In an analysis of various patients, neglect to cover some discrete area is almost always the chief factor in determining the pattern of injury.
Case V (Denver VAII, A 12676). A 49 year old white man, while under the influence of alcohol, slept in −10° F. weather for several hours in his unheated car. His left shoe and sock were off during this time. He subsequently suffered severe frostbite with gangrene of several toes on the exposed extremity, with no apparent injury to his covered foot. His wife, who occupied the car with him and was likewise inebriated, was adequately protected by clothing; she suffered no injury whatsoever.
Case VI (CGH, Outpatient). A 10 year old Negro boy was seen in the emergency room 5 days after playing outdoors in subzero temperature while wearing poorly fitting trousers. There were rings of frostbite on the legs at the exposed area between his socks and the bottom of the trousers (Fig. 4). Therapy was not required.
Fig. 4.
(Case VI). Seven days after frostbite.
Mechanism of the Injury
The consequence of frostbite is cell injury or death. The mechanism of this injury has been the subject of important controversy, since it bears on the type and potential efficacy of therapy. If, as Lewis,22 Meryman25 and many others believe, frostbite is essentially a thermal injury, the principal tissue damage has occurred by the time of rewarming and any or all subsequent measures will do little to alter the progression of pathologic events. If, however, vascular or other factors are of fundamental significance in the production of cell damage, there might be more hope for effective treatment. A brief description of the observed phenomena in experimental frostbite may be of interest in evaluating these unsolved questions.
Studies in cooled extremities suggest that a profound reduction in blood flow occurs promptly with cold exposure. When the arms of human volunteers were immersed in water at 55° F. for two hours, blood flow was reduced to approximately 3 per cent of control levels.3 At 32° to 46° F. there is virtually no circulation in the fingers.17 Although cooled tissues require less oxygen, it is reasonable to assume that the reduction in flow is of such extent as to result in ischemia25 and eventual tissue death. Such a mechanism could explain gangrene in nonfreezing cold injury, and it would be an important stage in the development of frostbite at colder temperatures.
Many authors have observed the changes after experimental frostbite, but the well-controlled studies of Kulka19,20 and Bellman4,5 provide the basis for much of the following description. During actual freezing, the tissue becomes opaque as observed by transillumination.11 Upon thawing, appearance is normal for a short time. Edema and rupture of small vessels is then observed, particularly of small venules.5 The role of the protein-rich products of extravasation and transudation are unknown, but it has been suggested that they cause immediate vascular compression and ultimate fibrosis.
Changes in small blood vessels are obvious promptly with thawing. Using microangiography and transillumination techniques, these may evolve for weeks or months.5 There is an immediate, intense arterial vasoconstriction at the junction of uninvolved tissue with frozen tissue. Within a few hours, a demonstrable increase in vascularity occurs in the marginal zone, at the time this area becomes clinically erythematous. Some authors have described the opening of small arteriovenous shunts in this region.20 Flow rate is reduced and intravascular sludging is observed. Within three days multiple small areas of stenosis, or frank, sharply delineated occlusions have been observed microangiographically5 within the previously-frozen area. Tubular filling defects which are thought to be thrombi can be demonstrated in both arteries and veins. By the tenth day these either regress or proceed to stenosis or occlusion of the vessels. During the ensuing weeks, both arteries and veins disappear from the microangiography pattern, presumably due to late thrombosis. The resulting destruction of vascular architecture is partially compensated by the previously mentioned increase in marginal blood supply from which new branches may bud into the formerly frozen area.6 However, in six to twelve weeks such new networks undergo involution and, if the injured area does not undergo necrosis, it is left with a distorted and cross-sectionally reduced vascular pattern.5 Histologic sections at various stages in the above sequence show edema and small-vessel thrombi which are often fibrinoid in character (Fig. 5), and later areas of local arteritis or intimal proliferative thickening (Fig. 6).
Fig. 5.
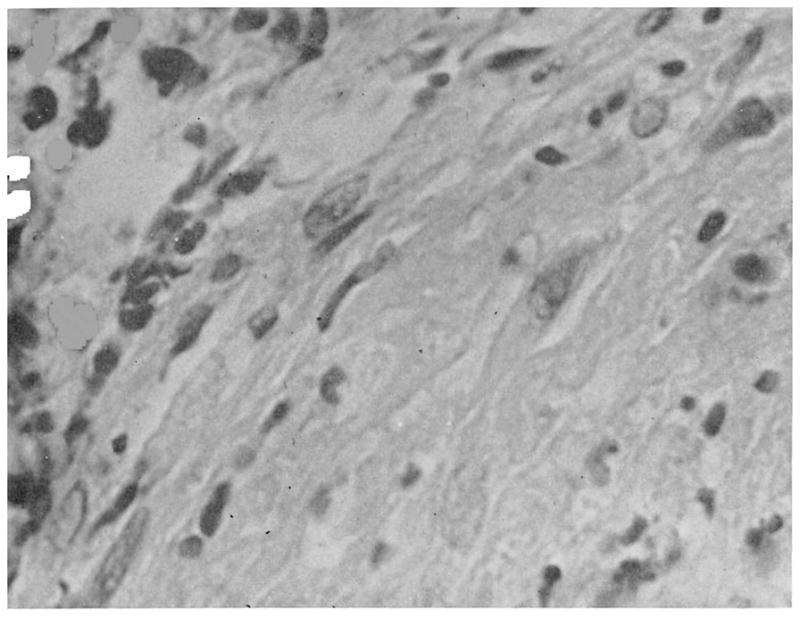
Arterial injury, 1 month after frostbite. Lumen is at upper left. Note intramural edema, disruption of epithelieal lining, and thrombus.
Fig. 6.
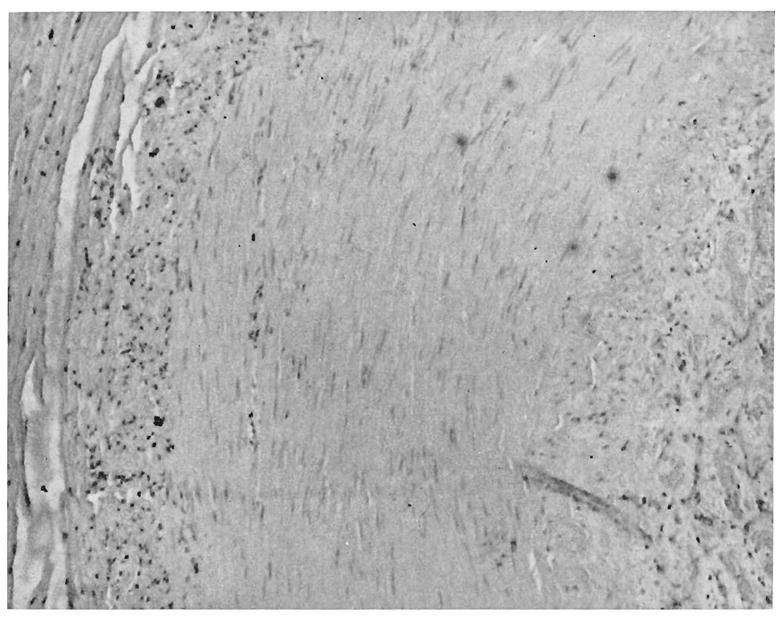
Arterial injury, 11 months following 2° frostbite. Note fibrous intimal proliferation and perivascular lymphocytic infiltration (Case IX). Lumen is on the right.
The ultimate result of various types of cold injury, as evaluated by histologic study, is essentially identical. This does not, of course, prove that all varieties have an identical pathogenesis. Frostbite differs from other cold injuries in that there is the possibility of actual tissue freezing. How often this occurs clinically is difficult to determine, since virtually all patients have been warmed before they are seen by a physician. Some experts believe freezing is uncommon. Others, particularly Meryman,25 believe that this is a common event in frostbite, is a factor of major significance, and justifies the sequestration of frostbite as a separate variety of cold trauma.
It was formerly believed that ice crystal formation within the cells led to their death by simple mechanical rupture of the cell wall. Meryman25 observed that ice crystals develop exclusively from available water in the extracellular compartment rather than within the cell. Under these conditions, a hypertonic environment gradually forms about the cells. Intracellular fluid then enters the interstitial spaces producing, in effect, a local type of intracellular dehydration with ultimate cellular death.
Figure 7 summarizes the probable sequence of events in the pathophysiology of frostbite. As discussed above, there is some experimental evidence that each of these pathways contributes to the degree of injury. Their relative importance is not as yet ascertained, and more research remains to be done in this area.
TREATMENT OF FROSTBITE
Lack of understanding of the pathophysiology of frostbite has made it difficult to recommend or follow rigid principles of therapy. In general, treatment can be divided into measures related to the local care of damaged tissue, and measures designed to diminish secondary vascular damage.
Method of Rewarming the Frozen Part
Until a few years ago, it was thought that rewarming of the frostbitten member should be done slowly. Rubbing the feet with snow, walking, beating the injured part, and plunging the extremity into cold water baths were variants of this approach which were not only passed along from generation to generation among the lay population but actively taught to first aid groups by physicians. A more temperate approach is to allow the patient to warm slowly at room temperature.
Studies with experimental frostbite suggest that the greatest salvage is with rapid warming of the affected part. Decisive information on this point in experimental frostbite has been provided by Lewis22 following earlier work by numerous investigators.2, 10, 11, 13, 31 Unquestionably, the major benefit of rapid warming is due to reduction in total time of cold exposure. In addition, there is some suggestive evidence that rapid rewarming has inherent value quite apart from mere decrease in freezing time.16
The conditions and details of rapid rewarming are explicit.22 The optimum temperature is 104° to 107.5° F. (40° to 42° C). The frozen extremity is placed in a water bath at this temperature. If the water bath is heated to more than 107.5°, harmful rather than beneficial effects occur. If the temperature is less, even by a few degrees, maximum benefit is not obtained. Heavy sedation may be required during the actual rewarming.
Since most patients with frostbite have already been warmed before seeking medical treatment, the greatest advance in immediate care can be made only in the education of the public and in lay groups trained for first aid duty. It is also necessary within hospitals to adopt a consistent policy applicable to those unusual patients exemplified by Case I, in which instance rewarming could have been performed under the ideal circumstances of a hospital environment.
The Value of Sympathectomy
A consideration of the pathophysiology of frostbite does not provide much hope that sympathectomy will profoundly alter the progression of changes. The acute vasoconstriction that occurs at the time of cooling regresses promptly with thawing, and is replaced with vasomotor dilatation and hyperemia of the marginal zone. Denervation would appear to offer little augmentation of blood supply. Controlled experimental studies provide equivocal or no evidence that sympathectomy is of value. There have been some clinical reports of benefit from sympathectomy. The most extensive clinical study was by De Jong and his associates,9 who described controlled evaluation of sympathectomy in 19 patients with bilateral frostbite of either the hands or feet. These authors performed unilateral sympathectomy and compared the subseqeunt behavior of the treated versus the nontreated limb. They observed more rapid resolution of edema and demarcation of slough of the denervated extremity, providing the sympathectomy was done within ten days of the time of injury.
In two patients in the present series with symmetrical injuries of the feet, sympathectomy was performed on one side. There was no difference in outcome of the treated feet compared with the nontreated feet.
Case VII (Denver VAH, A 12676). A 27 year old schizophrenic male was admitted 12 hours after having walked in the snow without shoes for 4 hours. During the ensuing 6 days, it was clear that the involvement of the feet was absolutely symmetrical. After 6 days, a left lumbar sympathectomy was performed. The development and evolution of gangrene subsequently was exactly the same in the two feet (Fig. 8). The course was not influenced in any demonstrable way. Initially, it was feared that extensive tissue loss was inevitable. After two and a half weeks, a black eschar sloughed bilaterally, revealing pink epithelium.
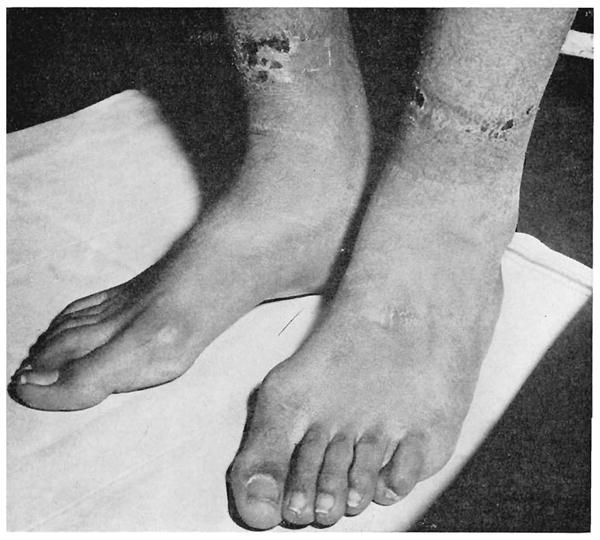
Fig. 8.

(Case VII). Eighteen days after frostbite.
The Value of Intra-arterial Vasodilators and Sympathetic Block
Numerous reports have stressed both the value and the lack of effect of these therapeutic approaches. The conceptual weakness of these forms of therapy would seem to be similar to those of sympathectomy. A specific effect of intra-arterial sympatholytic drugs such as Priscoline in relief of pain has been noted, and will be mentioned again under the section on pain.
The Place of Anticoagulants, Fibrinolysins and Low Molecular Weight Plasma Expanders in Therapy
As mentioned previously, prominent features of the frostbite injury are progression of vascular changes long after the acute injury involving sludging and the formation of agglutinative thrombi. The use of the above agents in the therapy of acute frostbite would appear logical. Heparin has received the greatest trial, with equivocal results, both in this series and elsewhere.18 Low molecular weight plasma expander, which has been shown in other circumstances to prevent blood sludging,12 and fibrinolysin, which might reverse the thrombotic process,33 have not been evaluated.
Local Care
Frostbite injuries have been treated with dressings and by the exposure method. The results appear to be little different, provided the techniques are meticulously executed. In this series, the open technique was used in most cases, with bacterial isolation of the patients. Dry gangrene and slough developed in almost all cases, without the complication of secondary infection.
Exercise of the Afflicted Extremity
During the acute phase of injury, it seems reasonable to immobilize the injured part. As soon as acute inflammation has subsided, exercise should be instituted. This is mentioned in Simeone’s analysis of war cold injuries37 as one of the few measures of undoubted therapeutic efficacy. In the present series it was not unusual to see good motion, and eventually good function, of blackened fingers and toes. Immobilization will result in stiffening and fibrosis in a member which could otherwise achieve functional restoration.
Indications for Amputation
One of the characteristic features of frostbite is the surprising salvage that is possible in an apparently badly injured extremity. Final classification of the extent of injury is possible only in retrospect. A blackened and apparently hopelessly traumatized foot may turn out to be almost completely preserved with only superficial skin slough. Extirpation should, therefore, be done with great conservatism and as late as possible. As long as there is movement in the involved area, there is hope for preservation of tissue. In the present series of 54 patients, there were 60 amputations. However, most of these were toes and fingers, almost always preserving more tissue than was expected early in the course. There were also two forearm amputations, two hand amputations, six foot amputations, seven below-knee amputations and two above-knee amputations. The above-knee amputations were in patients with associated occlusive vascular disease.
Pain Control
The control of pain in most patients of this series has not been a serious problem. Generally, aspirin or codeine alone is sufficient. In numerous others, paraldehyde, chloral hydrate and promazine were used, but alcoholism was the underlying indication for these drugs. In an occasional patient with early severe causalgic pain, one of us29 has used intra-arterial Priscoline with apparent relief. The mechanism of this relief is not clear. A similar effect has been noted by Shumacker35 following sympathectomy. It should be re-emphasized, however, that most patients do not require unusual measures for control of pain.
Long-Term Sequelae
Other than obvious loss of portions of limbs or areas of skin from gangrene, frostbite can precipitate a long-term illness with a disabling array of physical findings and symptoms. The following example typifies an all-too-common sequence of events following severe exposure to cold:
Case VIII (CGH, 423145). A 37 year old white man suffered third degree frostbite of both feet and hands 3 years prior to admission. He sought no medical care at the time. He had had progressive circulatory embarrassment since then, with numbness and coldness in all extremities, most marked in winter. Two years following injury, he lost the tips of two toes and the right index finger because of vascular insufficiency. On presentation here, he had impending gangrene of the tip of the right middle finger, his hands and feet were cool and moist, and the skin was shiny. The right third finger and two toes on the left foot showed cyanotic rubor. He underwent a right cervical sympathectomy and bilateral lumbar sympathectomy with good relief of symptoms.
Causalgic-type pain, hyperhydrosis, coldness of extremities and stiff joints were among the most common sequelae noted by Blair6 in a four- year follow-up of Korean War casualties. In general, the degree of long- term disability was related to the severity of the original injury, and discomfort was greater in cold weather than in warm weather. These patients are also much more susceptible to a second cold injury, having once been exposed.
Case IX (CGH, 37387). A 57 year old white man sustained a minor exposure to cold 11 months following a second-degree frostbite of both feet. He suffered increasing causalgic-type symptoms in both feet following the second exposure. There was dependent cyanotic rubor and hyperhydrosis. These symptoms were relieved by lumbar sympathectomy. In addition, the distal phalanx of his fourth toe was amputated because of vascular insufficiency. The arteries in the toe were seen to contain fibrous internal proliferation, with perivascular lymphocytic cuffing as evidence of a long-standing, low-grade vasculitis (Fig. 6).
That these long-term alterations are secondary to the vascular injury sustained at the time of exposure has been well accepted. In addition, physiologic studies by Simeone have shown diminution of the ability of these vessels to react to stress. Blood vessels studied in the skin did not constrict as effectively as the normal ones did when exposed to cold, and did not dilate as effectively when vasoconstriction was blocked.37
Another aspect of long-term frostbite injury was recently reviewed by Ritchie.30 In a study of 13 individuals examined four to 50 years after being frostbitten during childhood, it was noted that frostbite had damaged the epiphyses and resulted in lack of development, deformity and limited use of the fingers. The loss of function was in general related to degree of exposure and age at the time of the episode.
PROPHYLAXIS
Rarely does the well worn maxim, “an ounce of prevention is worth a pound of cure,” have more immediacy and meaning than in the prophylaxis of frostbite. Once the cold injury has taken place, no treatment can save cells already destroyed, and subsequent therapy is essentially supportive.
The realization that frostbite implies a long-term illness with possible economically disastrous consequences should be impressed on all people who live in cold regions. This is most important in outdoor recreational activities. Frostbite is a silent assailant. This fact should be thoroughly appreciated by the public. Lack of pain at the time of injury is part of the natural history of the disease.
A pitfall for the unwary, in Colorado at least, is the lack of feeling of cold despite low ambient temperatures. Rocky Mountain folklore relates this to low humidity, but, as Sir Thomas Lewis has pointed out,24 the humidity of air with freezing temperatures is essentially zero irrespective of geographic location.
Proper clothing, which means multiple layers of light woolen material and a windproof outer garment, are basic equipment. Proper head gear and foot wear are extremely important. Gloves should be worn at all times, particularly when the hands must come in contact with metallic objects.
Unfortunately, a sound educational and public health program will have little meaning for the majority of our patients. Their sociopathic and often frankly psychotic backgrounds preclude any worthwhile value in this area.
SUMMARY
Frostbite is a serious illness with potentially disastrous consequences which are often not apparent immediately after injury. Factors contributing to the severity of the injury have been enumerated.
The pathologic physiology of the injured member following exposure has been intensively studied in laboratory animals with subsequent extrapolation to human cold injury. That much still remains to be understood is evident by the diverse modes of treatment, each with its proponents. Certain aspects of therapy have, however, become generally accepted. If thawing of the frostbitten extremities has not taken place at the time the patient is first seen, the affected parts should be warmed rapidly at a temperature of 104° to 107.5° F. (40° to 42° C). Open treatment is as effective as dressings. Ambulation should be started as early as possible.
In the absence of infection, amputation should be delayed until definitive demarcation has occurred. This may and usually does take several months.
In a civilian population living in cold climates, a public health education program would be of some benefit. However, because of the emotionally disturbed condition of the patient in almost half of our cases, the value of this form of prophylaxis is limited.
Acknowledgments
Aided by Grant A-3176 from the U.S. Public Health Service, Bethesda, Maryland.
References
- 1.Adams F. The Genuine Works of Hippocrates. London: The Sydenham Society; 1886. [Google Scholar]
- 2.Allen FM, Safford FK., Jr Experiments on local hypothermia for treatment of burns and frostbite. Arch Surg. 1950;61:515. doi: 10.1001/archsurg.1950.01250020520011. [DOI] [PubMed]
- 3.Bancroft H, Edholm OG. Effect of temperature on blood flow and deep temperature in the human forearm. J Physiol. 1943;102:5. doi: 10.1113/jphysiol.1943.sp004009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellman S, Adams-Ray J. Vascular reactions after experimental cold injury. A microangiographic study on rabbit ears. Angiology. 1956;7:339. doi: 10.1177/000331975600700404. [DOI] [PubMed] [Google Scholar]
- 5.Bellman S, Strombeck JO. Transformation of the vascular system in cold-injured tissue of the rabbit’s ear. Angiology. 1960;11:108. doi: 10.1177/000331976001100204. [DOI] [PubMed] [Google Scholar]
- 6.Blair JR. Follow-up on cold injury cases from the Korean War. In: Ferrer MI, editor. Fourth Conference on Cold Injury. Josiah Macy Jr. Foundation; New York City: 1955. p. 9. [Google Scholar]
- 7.Coffey MF. A comparative study of young Eskimos and Indian males with acclimatized white males. In: Ferrer MI, editor. Third Conference on Cold Injuries. Josiah Macy Jr. Foundation; New York City: 1953. p. 100. [Google Scholar]
- 8.Davis L, Scarff JE, Rogers N, Dickinson M. High altitude frostbite. Surg Gynec Obst. 1943;77:561. [Google Scholar]
- 9.DeJong O, Golding MR, Sawyer PN, Wesolowski SA. Recent observations in the therapy of frostbite. S Forum. 1961;12:444. [PubMed] [Google Scholar]
- 10.Finneran JC, Shumacker HB., Jr Studies in experimental frostbite: Further evaluation of early treatment. Surg Gynec & Obst. 1950;90:430. [Google Scholar]
- 11.Fuhrman FA, Crismon JM. Studies on gangrene following cold injury: Treatment of cold injury by immediate rapid warming. J Clin Invest. 1947;26:476. [PubMed] [Google Scholar]
- 12.Gelin LE. Supravascular aggregation and capillary flow. Acta chir scandinav. 1957;113:463. [PubMed] [Google Scholar]
- 13.Harkins HN, Harmon PH. Thermal injuries: Effects of freezing. J Clin Invest. 1937;16:213. doi: 10.1172/JCI100850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hellstrom B, Anderson KL. Heat output in the cold from the hands of Arctic fishermen. J Appl Physiol. 1960;15:771. doi: 10.1152/jappl.1960.15.5.771. [DOI] [PubMed] [Google Scholar]
- 15.Hildes JA, Irving L, Hart JS. Estimation of heat flow from hands of Eskimos by calorimetry. J Appl Physiol. 1961;16:617. doi: 10.1152/jappl.1961.16.4.617. [DOI] [PubMed] [Google Scholar]
- 16.Hurley LA. Proj. N. M. 007081.14. Naval Med. Res. Inst; Bethesda, Md: 1956. [Google Scholar]
- 17.Kramerk K, Schulze W. Die kaltedilatation der hautgefase. Arch fd ges Physiol. 1948;250:141. [PubMed] [Google Scholar]
- 18.Kreyberg L. Development of acute tissue damage due to cold. Physiol Rev. 1949;29:156. doi: 10.1152/physrev.1949.29.2.156. [DOI] [PubMed] [Google Scholar]
- 19.Kulka PJ. Vasomotor microcirculatory insufficiency: Observations on non-freezing cold injury of the mouse ear. Angiology. 1961;12:491. doi: 10.1177/000331976101201011. [DOI] [PubMed] [Google Scholar]
- 20.Kulka PJ. Histopathologic studies in frostbitten rabbits. In: Ferrer MI, editor. Fourth Conference on Cold Injury. Josiah Macy Jr. Foundation; New York City: 1955. p. 97. [Google Scholar]
- 21.Larrey DJ. Memoires de chirurgie militaire et campagnes. Paris: J. Smith; 1817. [Google Scholar]
- 22.Lewis RB. The Wellcome prize essay for 1951: Local cold injury; frostbite. Milit Surgeon. 1952;110:25. [PubMed] [Google Scholar]
- 23.Lewis T. Observations on some normal and injurious effects of cold upon the skin and underlying tissues. Brit M J. 1941;2:795. doi: 10.1136/bmj.2.4222.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis T. Effects of cold upon skin and underlying tissues. Brit M J. 1941;2:869. doi: 10.1136/bmj.2.4224.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meryman HT. Tissue freezing and local cold injury. Physiol Rev. 1957;37:233. doi: 10.1152/physrev.1957.37.2.233. [DOI] [PubMed] [Google Scholar]
- 26.Milan FA, Eisner RW, Rodabl K. Thermal and metabolic responses of men in the Antarctic to a standard cold stress. J Appl Physiol. 1961;16:401. doi: 10.1152/jappl.1961.16.3.401. [DOI] [PubMed] [Google Scholar]
- 27.Molnar GW. Sixth Conference on Cold Injury. Josiah Macy Jr. Foundation; New York City: 1958. An evaluation of wind chill; p. 175. [Google Scholar]
- 28.Orr KD, Fainer DC. Cold injuries in Korea during the winter of 1950–1951. Medicine. 1952;31:177. doi: 10.1097/00005792-195205000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Owens JC. Causalgia. Ann Surg. 1957;23:636. [PubMed] [Google Scholar]
- 30.Ritchie GW. Abstract Modern Medicine. Mar, 1962. p. 54. [Google Scholar]
- 31.Rosenfeld L, Langohr JL, Owen CR, Cope O. Circulation of the blood and lymph in frostbite and influence of therapeutic cold and warmth. Arch Surg. 1949;59:1045. doi: 10.1001/archsurg.1949.01240041055006. [DOI] [PubMed] [Google Scholar]
- 32.Ferrer MI, editor. Second Conference on Cold Injury. Josiah Macy Jr. Foundation; New York City: 1952. pp. 203–216. [Google Scholar]
- 33.Sherry S, Fletcher AP, Alkjaersig N. Developments in fibrinolytic therapy for thromboembolic disease. Ann Int Med. 1959;50:560. doi: 10.7326/0003-4819-50-3-560. [DOI] [PubMed] [Google Scholar]
- 34.Shikata JI, Shumacker HB, Jr, Nash FD. Studies in experimental frostbite: Effect of cold acclimatization upon resistance to local cold injury. AMA Arch Surg. 1960;81:817. [Google Scholar]
- 35.Shumacker HB., Jr Sympathectomy in the treatment of frostbite. Surg Gynec Obst. 1951;93:727. [PubMed] [Google Scholar]
- 36.Schuman LM. Epidemiology of cold injury in man. In: Ferrer MI, editor. Second Conference on Cold Injury. Josiah Macy Jr. Foundation; New York City: 1952. p. 11. [Google Scholar]
- 37.Simeone FA. The surgical volumes of the history of the United States Army Medical Department in World War II, Cold Injury. AMA Arch Surg. 1960;80:396. doi: 10.1001/archsurg.1960.01290200040007. [DOI] [PubMed] [Google Scholar]
- 38.Whayne TF. In: Preventive Medicine in World War II. Coates JB Jr, editor. Office of Surgeon General; Washington, D. C: 1955. p. 63. [Google Scholar]


