Abstract
Objectives
The objectives of the study were to: (1) assess the knowledge and awareness of diabetic patients of their risk for systemic and oral diseases as complications associated with diabetes, (2) to assess their attitudes toward sustaining good oral health through proper oral hygiene and regular dental check-ups, and (3) to the extent that they are aware, to determine how they became aware.
Methods
Two hundred self-administered questionnaires were distributed to assess the main objectives of the study. Only completed questionnaires were used in the current study data analysis.
Results
A majority of the participants had Type 2 diabetes (58%). The awareness of diabetic patients of their increased risk for oral diseases is low compared to their awareness of systemic diseases. Their attitude toward maintaining good oral health was also not to desired standard. Of the participants, 50% brushed their teeth once daily and 66% never used dental floss. Regarding participants’ sources of awareness, 37% learned from dentists and 45% through other media sources.
Conclusions
Diabetic patients are found to have little knowledge of their increased risk for oral diseases. In order to promote proper oral health and to reduce the risk of oral diseases, health professionals in both the dental and medical fields need to take the responsibility to develop programs to educate the public about the oral manifestations of diabetes and its complications on oral health.
Keywords: diabetes, oral health, periodontal disease, oral self-care, oral diseases, diabetes complications
Diabetes mellitus has been increasing at such an alarming rate worldwide that recently the World Health Organization (WHO) declared the disease an epidemic. The number of estimated cases of diabetes has increased from 30 million in 1985 to 135 million in 1995, and is projected to increase to 366 million by the year 2030 (1). The prevalence of diabetes mellitus in the United Arab Emirates, the country in which the present study was conducted, was 350,000 cases in 2000 and estimated to increase to 684,000 in 2030 (1).
In addition to the more common complications that arise as a result of this disease, diabetic patients who do not carefully control their blood glucose levels will be at high risk of systemic and oral complications. The most common chronic manifestations are macrovascular diseases and include coronary artery, peripheral vascular, and cerebrovascular diseases. Additionally, microvascular complications manifest as retinopathy, neuropathy, and nephropathy among others. Examples of acute complications are diabetic ketoacidosis, hyperosmolar hyperglycemia, as well as other acute infections (2).
In terms of its oral consequences, diabetes manifests itself in several ways. When diabetes mellitus is left uncontrolled for an extended period, for example, it negatively affects the salivary glands and results in xerostomia or sialosis (3–7). When not enough saliva is produced to wash and cleanse the oral cavity, plaque and debris accumulate at a much faster than normal rate. This could be a factor in the increased risk for dental caries often observed in dental patients (8, 9). Furthermore, peridontitis is perhaps the most widely noted oral manifestation of diabetes mellitus. In fact several researches have advanced the notion that there is a bidirectional relationship between periodontitis and diabetes mellitus (10, 11). In one study, diabetics with uncontrolled blood glucose level were shown to be three times more susceptible to developing severe periodontitis than those with normal blood glucose readings (12).
A recent study by Allen et al. assessed the knowledge of 101 diabetic patients had of their risk for periodontal disease, their attitude toward oral health, and their oral health-related quality of life. The researchers found that only 33% of the participants were aware of their increased risk for periodontal disease (13). Similarly, Eldarrat (14) found that diabetic patients’ awareness of their increased risk for oral diseases was low compared to their awareness of systemic diseases and a significant association was found between glycemic control and oral infections. Furthermore, Moore et al. (15) assessed oral health attitudes, behaviors, and knowledge of participants with Type 1 diabetes and found that most of the participants were unaware of the oral health complications of diabetes mellitus and the need for preventive care.
Despite the worldwide recognition of the dangers of diabetes mellitus, diabetic patients’ awareness of and attitudes toward their heightened risk for oral diseases has not been fully addressed. Thus, the purpose of the current study was to: (1) assess the knowledge and awareness of diabetic patients of their risk for systemic and oral diseases as complications associated with diabetes, (2) to assess their attitudes toward sustaining good oral health through proper oral hygiene and regular dental check-ups, and (3) to the extent that they are aware, to determine how they became aware.
Methods
In the current study, a self-administered questionnaire previously used by Eldarrat (14) was utilized to assess the main aims of the study. Questionnaire questions were carefully selected from relevant published reports in international journals. The questionnaire questions were related to participants’ nationality, age and sex, Type and duration of diabetes, and their awareness for systemic and oral diseases as complications associated with diabetes. Also, the questionnaire included questions to assess participant's attitudes toward maintaining good oral health. Various response formats were used in the questionnaire such as ‘yes,’ ‘no,’ ‘I do not know,’ encircling disease name, they were aware of as a complication of diabetes, or filling blank spaces. A pilot study was carried out on 20 diabetic volunteers to assess the response of participants to the questionnaire before conducting the study.
Two hundred questionnaires and consent forms were distributed to the diabetic patients attending the outpatient diabetic clinic in Rashid Hospital, one of the largest governmental hospitals in Dubai, United Arab Emirates. An information sheet explaining the need for the study and the procedure for responding to the questionnaire was enclosed as a cover sheet. Eligible participants were confirmed diabetes mellitus patients who can read and write and were free from any mental disabilities. Data were collected over a period of 8 weeks. None of the participants refused to participate by answering the questionnaire questions. However, questionnaires with uncompleted answers were excluded and a total of 100 completed questionnaires were entered on an Excel spreadsheet and imported into Statistical Package for Social Sciences (SPSS) version 13 (SPSS Inc., Chicago, IL, USA) for data statistical analysis.
Results
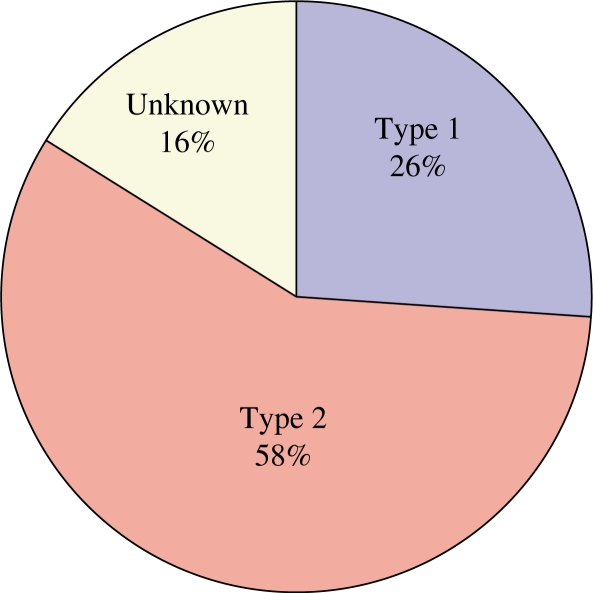
The diabetic patients participating in the current survey were 10% United Arab Emirates (UAE) nationals and 90% non-UAE nationals, of whom 50% were male and 50% were female. The mean of the participants’ age was 47 years. Of the participants, 36% were smokers. Eightyseven percent of the participants were dentulous and 13% were edentulous. Of the edentulous participants, 34% only were wearing complete dentures. The mean of the participants’ diabetes duration was 15 years. The percentage of participants’ knowledge of their diabetes type is shown in Fig. 1. As shown in the figure of the participants, 58% had Type 2 diabetes, 26% had Type 1, and 16% did not know what type of diabetes they had.
Fig. 1.
Participants’ knowledge of their diabetes type (unknown = do not know).
Regarding diabetic patients’ knowledge and awareness of systemic and oral complications associated with diabetes, in this survey the percentage of participants who were aware of their increased risk for eye disease (85%), heart disease (75%), kidney diseases (90%), periodontal disease (60%), dental caries (54%), and oral fungal infections (42%).
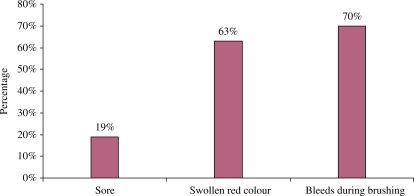
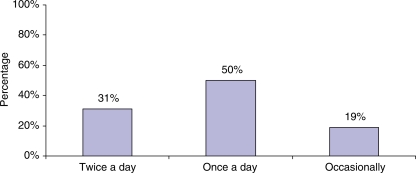
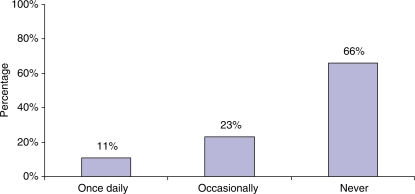
Seventy-seven percent of participants were suffering from dry mouth. Of these, 60% were unaware of the serious consequences of dry mouth on their oral health. Participants’ knowledge of periodontal disease signs is shown in Fig. 2. As can be seen in Fig. 2, the majority of the participants (70%) were aware that bleeding during brushing is a sign of gingival disease, while 63% were aware that swollen red-colored gingiva is a sign of gum disease, and 19% were aware that soreness of the gingiva is a sign of periodontal disease. Figure 3 shows the diabetic patients’ attitude toward using a toothbrush for oral self-care. As the graph indicates, 19% of the respondents did not use a brush on a daily basis, 31% brushed twice a day, and a significantly higher number of respondents (50%) brushed once a day. Figure 4 is a breakdown of the respondents’ attitude toward using dental floss as part of their oral self-care. A significant proportion (66%) never used dental floss, 11% reported using dental floss once a day, and 23% did not use on a daily basis. The questionnaire also revealed that there is a relatively low percentage (40%) of yearly visits to a dental clinic. Only 14% reported they visited for a regular dental check-up. In response to the question about whether they would wish to save a mobile tooth, 24% of participants said they would prefer extraction and 16% would consent to extraction of an anterior tooth. The decision made by a dentist in considering whether to extract a loose front tooth was favored by 70% of respondents. In decisions whether to have extraction of the mobile tooth, 34.2% favored the dentist's decision. Time and cost factors were less likely to influence the consent for extraction of either anterior or posterior tooth (4.2 and 7.1%, respectively). As for the sources of participants’ knowledge and awareness of their increased risk for oral diseases, 37% of the participants had received this information from dentists, 4% from dental hygienists, and 45% from other sources such as television programs, the Internet, magazines, and friends.
Fig. 2.
Respondents' awareness of signs of periodontal disease.
Fig. 3.
Respondents' frequency of using a toothbrush.
Fig. 4.
Respondents' frequency of using dental floss.
Discussion
The recent rise in diabetes is not a genetic shift only but also an environmental shift as a result of lifestyle habits. The prevalence of diabetes worldwide has been increasing epidemically. It was declared by WHO that 366 million people are expected to suffer from diabetes mellitus by 2030. In the current study, more than half of the participants (58%) had Type 2 diabetes, 26% suffered from Type 1 and, unexpectedly, 16% of participants did not know what type of diabetes they had.
The data presented in this study reveals an important finding: it clearly demonstrates that diabetics have more knowledge about their increased risk for systemic complications associated with diabetes than they do for oral and dental complications. The percentage of participants who were aware of their increased risk for eye disease was 85%, heart disease 75%, kidney diseases 90%, periodontal disease 60%, dental caries 54%, and oral fungal infections 42%. Similar findings were reported by several researchers, who assessed the knowledge diabetic patients had of their risk for periodontal disease, their attitude toward oral health and their oral health-related quality of life. Researchers found that 98% of the participants were aware of their increased risk for eye disease, 84% for heart disease, 94% for kidney disease, and 33% for periodontal disease (13).
Another important finding of the present study is that the knowledge of diabetic patients of their increased risk for oral diseases such as periodontal disease, tooth caries, and fungal infections as result of mouth dryness was very inadequate. More than 70% of the participants were suffering from dry mouth and were unaware of the harmful effect of xerostomia on their oral health. It is well known that a significant reduction of salivary flow leading to xerostomia is the most common oral manifestation of diabetes. It is of paramount importance to inform and make diabetics aware of the beneficial properties of saliva. Saliva's function of washing and cleansing the oral cavity is known to prevent the accumulation of plaque and debris, which could be a contributing factor in diabetics’ increased risk for periodontal disease and dental caries (8, 9). In addition, saliva has antimicrobial actions, which when impaired and the blood and saliva glucose concentrations are high, allows for the growth of Candida organisms (16). Moreover, diabetics should be informed and educated about the importance for keeping the oral cavity moist by stimulating salivary flow and frequent sips of water.
This study also revealed the additional important finding that diabetic patients have limited knowledge of the associations between oral health and overall health. In the current study only 34% of edentulous participants were wearing complete dentures. Moreover, the majority of the participants were without dentures and ate selected soft foods that were easy to chew and swallow. These participants are deprived of the benefits of eating healthy food. This has negative consequences on their glycemic control, general health, and health-related quality of life. A recent study showed a significant association between dentate status of diabetics and their metabolic control scores, as a higher proportion of patients in the dentate group were found to have lower metabolic control scores (13).
In terms of their oral self-care, maintaining good oral hygiene was also poor among the participants. Half of the participants brushed their teeth once daily, 31% of the participants brushed their teeth twice daily, and 19% did not brush on a daily basis. In addition, more than half of the participants never used dental floss to clean between their teeth. Similar results were reported by several investigators who found that of 299 participants, only 29% brushed their teeth on a twice-daily basis (17).
The data of the present study showed that about 40% of the participants had not visited a dental clinic within the last year. The main reason to visit a dental clinic within the last year was to receive treatment for pain and/ or discomfort. Only 14% visited for regular check-ups. This showed that participants’ attitude toward their oral health was poor in comparison with the findings of other surveys. Only 14% of participants in this survey visited regularly for dental check-ups compared with 37, 47, and 59% in a survey done in the UK (13, 17, 18). The results of this survey showed that the information regarding participants increased risk for oral diseases associated with diabetes came from dentists (37%), dental hygienists (4%), and 45% from other sources such as television programs, the Internet, magazines, and friends.
It is of paramount importance for dental professionals to raise the awareness of diabetic patients of their increased risk for oral diseases and the impact of oral health on their general health. Research projects to determine awareness for diabetic patients of their increased risk for oral and dental diseases and their attitude to maintaining good oral health will significantly and positively impact their oral health-related quality of life. Early detection and treatment of tooth caries, periodontal disease, and other oral diseases would be of enormous benefit to protect diabetic patients from the harmful oral complications associated with diabetes. In fact, one of the US national health objectives to be achieved by 2010 was to increase to 71% the proportion of people with diabetes who have an annual dental checkup (19). Furthermore, it is necessary for dental professionals and related government agencies to promote awareness of the relationship between diabetes and oral heath in order to prevent harmful dental complications and expensive treatment.
Conclusion
Within the limitations of the current study, the data presented in this study clearly demonstrated that diabetics have more knowledge about their increased risk for systemic complications associated with diabetes than they do for oral and dental complications. In order to promote proper oral health and to reduce the risk of oral diseases, health professionals in both the dental and medical fields need to take the responsibility to develop programs to educate the public about the oral manifestations of diabetes and its complications on oral health.
Acknowledgements
The author wishes to express her gratitude to Dr Stephen Palubiski at English Language College, University of Sharjah, for his careful reading and editing of this article, and to Dr Mohamed Bataineh at University General Requirements Unit, UAE University, Al Ain, UAE for his useful advice and help in data analysis.
Conflict of interest and funding
The author has not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Smyth S, Heron A. Diabetes and obesity: the twin epidemics. Nat Med. 2006;12:75–80. doi: 10.1038/nm0106-75. [DOI] [PubMed] [Google Scholar]
- 2.Skamagas M, Breen TL, LeRoith D. Update on diabetes mellitus: prevention, treatment, and association with oral diseases. Oral Dis. 2008;14:105–14. doi: 10.1111/j.1601-0825.2007.01425.x. [DOI] [PubMed] [Google Scholar]
- 3.Sheppard IM. Oral manifestation of diabetes mellitus: a study of one hundred cases. J Am Dent Assoc. 1942;29:1188–92. [Google Scholar]
- 4.Lamey PJ, Darwazeh AM, Frier BM. Oral disorders associated with diabetes mellitus. Diabet Med. 1992;9:410–6. doi: 10.1111/j.1464-5491.1992.tb01809.x. [DOI] [PubMed] [Google Scholar]
- 5.Russotto SB. Asymptomatic parotid gland enlargement in diabetes mellitus. Oral Surg Oral Med Oral Pathol. 1981;52:594–8. doi: 10.1016/0030-4220(81)90075-x. [DOI] [PubMed] [Google Scholar]
- 6.Murrah VA. Diabetes mellitus and associated oral manifestations: a review. J Oral Pathol. 1985;14:271–81. doi: 10.1111/j.1600-0714.1985.tb00494.x. [DOI] [PubMed] [Google Scholar]
- 7.Greenspan D. Xerostomia: diagnosis and management. Oncology. 1996;10:7–11. [PubMed] [Google Scholar]
- 8.Rees TD. The diabetic dental patient. Dent Clin North Am. 1994;38:447–63. [PubMed] [Google Scholar]
- 9.Finney LS, Finney MO, Gonzalez-Campoy JM. What the mouth has to say about diabetes. Careful examinations can avert serious complications. Postgrad Med. 1997;102:117–26. doi: 10.3810/pgm.1997.12.384. [DOI] [PubMed] [Google Scholar]
- 10.Bartolucci EG, Parkes RB. Accelerated periodontal breakdown in uncontrolled diabetes. Pathogenesis and treatment. Oral Surg Oral Med Oral Pathol. 1981;52:387–90. doi: 10.1016/0030-4220(81)90336-4. [DOI] [PubMed] [Google Scholar]
- 11.Ureles SD. Case report: a patient with severe periodontitis in conjunction with adult-onset diabetes. Compend Contin Educ Dent. 1983;4:522–8. [PubMed] [Google Scholar]
- 12.Li CL, Tsai ST, Chou P. Comparison of metabolic risk profiles between subjects with fasting and 2-hour plasma glucose impairment: the Kinmen Study. J Clin Epidemiol. 2002;55:19–24. doi: 10.1016/s0895-4356(01)00410-3. [DOI] [PubMed] [Google Scholar]
- 13.Allen EM, Ziada HM, O'Halloran D, Clerehugh V, Allen PF. Attitudes, awareness and oral health-related quality of life in patients with diabetes. J Oral Rehabil. 2008;35:218–23. doi: 10.1111/j.1365-2842.2007.01760.x. [DOI] [PubMed] [Google Scholar]
- 14.Eldarrat A. Oral Health Prev Dent; Awareness and attitude of diabetic patients towards their increased risk for oral diseases. (in-press) [PubMed] [Google Scholar]
- 15.Moore PA, Orchard T, Guggenheimer J, Weyant RJ. Diabetes and oral health promotion: a survey of disease prevention behaviors. JADA. 2000;131:1333–41. doi: 10.14219/jada.archive.2000.0388. [DOI] [PubMed] [Google Scholar]
- 16.Manfredi M, McCullough MJ, Vescovi P, Al-Kaarawi ZM, Porter SR. Update on diabetes mellitus and related oral diseases. Oral Dis. 2004;10:187–20. doi: 10.1111/j.1601-0825.2004.01019.x. [DOI] [PubMed] [Google Scholar]
- 17.Bakhshandeh S, Murtomaa H, Vehkalahti MM, Mofid R, Suomalainen K. Oral self-care and use of dental services among adults with diabetes mellitus. Oral Health Prev Dent. 2008;6:279–86. [PubMed] [Google Scholar]
- 18.Kelly M, Steele J, Nuttall N, Bradnock G, Morris J, Nunn J. Adult dental health survey: oral health in the United Kingdom. London: TSO; 1998. p. 2000. [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) Dental visits among dentate adults with diabetes – United States, 1999 and 2004. MMWR Morb Mortal Wkly Rep. 2005;54:1181–83. [PubMed] [Google Scholar]