Abstract
Introduction:
The obesity epidemic has become a health crisis in the United States, particularly for minorities. This article reports on the health status and sociodemographic characteristics of morbidly obese American Indians living in rural areas of California.
Methods:
A cross-sectional randomized household study of 457 American Indian adults was implemented at 13 rural reservation sites throughout California. Data collected included sociodemographics, body mass index (BMI), health status, and health problems. Chisquare tests were used to assess statistical differences among categorical data and ANOVA methods were used for normally distributed continuous variables.
Results:
Nearly a majority of females were morbidly obese (11.6%) or obese (37.3%), while males were significantly represented in the overweight (38%) group (P=.0007). The prevalence of morbid obesity was twice the general population (13% vs. 5.9% respectively); average age was 47 years; 35% spoke their tribal language; 87% were enrolled in a tribe; 46% had 50% or more Indian blood; 42% were married; 29% had less than 12th grade education; and the average monthly household income was $2,126. The average weight of participants was 266 pounds (P<.0001). Morbidly obese adults reported more health problems and physical limitations (P=.003) than adults in other BMI categories. Obesity status and health conditions were significant for those with type 2 diabetes (P=.003), arthritis (P=.04) and hypertension (P=.03).
Discussion:
The obesity epidemic in the American Indian population is a severe and a multifactorial problem. The high rate of poor health status among this population should be addressed, possibly by programs designed to increase physical activity.
Keywords: Morbid Obesity, Health Status, Characteristics, Sociodemographics, Rural, American Indians
Introduction
The obesity epidemic is a growing public health crisis in the United States. The prevalence of American adults who are at least 100 pounds overweight has risen dramatically in the past decade.1 For instance, 31% of those aged 20–74 years in the general population were categorized as obese in 1999–2004, as compared to just 14% in 1976–1980.2 Indeed, rates of obesity have been steadily increasing over the past 30 years, a trend largely attributed to Americans consuming diets high in fat and calories and living sedentary lifestyles.3 Among American Indians, the age-adjusted percentage of adults who were obese was 34%, 1.6 times higher than that reported for non-Hispanic Whites.4 American Indian obesity rates are not only higher than those for the general US population, they are also now higher than any other ethnic group, except for black females whose obesity rates are similarly in the 30–37% range.5,6 At one time morbid obesity was thought to be an uncommon and rare condition found only among a few individuals, however, research is showing an increased trend towards morbid obesity across all sectors of the American public. Factors associated with morbid obesity include genetics, as well as metabolic, environmental, behavioral and socioeconomic influences, yet there may be other complex factors attributed to the increased prevalence of morbid obesity, particularly among minority groups.7 Exploration into areas of culture, sociodemographic characteristics and health status need to be examined to identify potential contributors to morbid obesity.
Research has revealed that the association between income level and obesity is strong. In developed countries like the United States, obesity is most common among those with low socioeconomic status.8 Age and education levels are demographic factors found to be related to body weight; additionally, weight gain increases with age and decreases with educational attainment. Studies also show living in an urban area is positively related to higher overweight and obesity prevalence.9,10 This may be because of easy access to high-fat foods, as well as increasingly more sedentary lifestyles due to access to transportation capabilities and less physically demanding jobs.
Most studies use body mass index (BMI) as the primary assessment of overweight status. The BMI, which is calculated from reported height and weight, combined with waist circumference and additional risk factors may be used to make an initial assessment of a person’s risk for developing obesity-associated diseases. Morbid obesity (or severe obesity), defined as a BMI >40 or weight gain over 100 pounds, is associated with a myriad of health conditions posing serious health risks and contributing to premature death.11,12 These morbid obesity related conditions (ie, high blood pressure, stroke, heart disease, high cholesterol, diabetes, gallbladder disease, and osteoarthritis) negatively impact individuals’ quality of life.13 Morbid obesity is particularly troubling to communities as with massive weight gain individuals face a greater probability of disability, associated healthcare costs and lost productivity.13 The negative consequences of obesity is said to potentially exceed those of smoking or problem drinking.14 Unfortunately, American Indians living on reservations are very difficult to capture in national health surveys due to remoteness and mistrust towards outside researchers; as such, estimates of the prevalence and temporal trends of morbid obesity among rural American Indians are not easily available. In this study we investigated the health status and sociodemographics of morbidly obese rural American Indians in California.
Methods
The study design was a cross-sectional randomized household study of American Indians residing on rural reservation sites in California. As a part of a needs assessment, American Indian residents in 13 rural California counties were surveyed to identify the health problems and wellness issues confronting rural American Indian populations. During 2002–2003, all American Indian clients who visited one of 13 rural American Indian clinics within the past five years were identified by family groups. Households were then randomized into groupings, contacted and a questionnaire was completed by all adult (aged ≥18 years) American Indian residents of those households. Five hundred individuals were contacted and 459 participated in the survey. Approvals for research were obtained from each site’s tribal council and/or health clinic. Institutional Review Board approvals were obtained from the University of California at Berkeley, University of California at San Francisco, University of Minnesota and the Indian Health Service. All participants received verbal and written study overviews and consented in accordance with Human Subjects Committee procedures. All participants were told that their participation was voluntary and that they did not have to answer any survey question that they did not want to. Also, we carefully explained that services at the tribal, clinic or community centers did not depend upon participation in the study.
The survey instrument was a 60 minute self-administered questionnaire and included the following health status and sociodemographic measures.
General Health Status
A single question, “How would you rate your health, nowadays? Would you say that it is excellent, very good, good, fair or poor?” was used to measure health status.
Major Health Problems
Information on major diagnosed health problems was requested, such as if the participant had high blood pressure, diabetes, cancer, lung disease, heart problems, stroke, psychological problems or arthritis.
Sociodemographics
Measures included sex, age, tribal affiliation, tribal enrollment, degree of Indian blood (reported as 25%, 50%, 75% or 100%), language (ability to speak the tribal language), employment (employed in some capacity), income (monthly and annual median and average household income), other financial resources (such as food stamps or other household support), marital status (married or living as married, divorced, separated, single or widowed), number of household members (children and adults), number of children (live births) and educational attainment (high school degree and above vs fewer years of education).
Morbid Obesity
The measure of obesity was based on BMI, (kg/m2). Morbid obesity was defined as a BMI >40, obesity defined as a BMI of 30 to 39.9, overweight as 25 to 29.9, healthy weight as18.5 to 24.9, and underweight was defined by a BMI <18.5.6,13
The survey results were entered in a computerized data analysis package.15 Participant identifiers were coded to ensure confidentiality. Frequencies on all variables were run for descriptive purposes. Chi-square tests were used to assess statistical differences among categorical data and ANOVA methods were used for normally distributed continuous variables.
Results
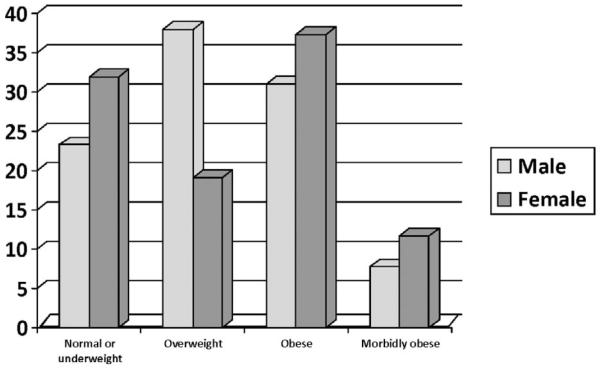
Study results indicated that a very high proportion of American Indian females were morbidly obese (11.6%) or obese (37.3%), while American Indian males were significantly represented in the overweight (38%) group (P=.0007) (See Figure 1). Our data show the combined rate for morbidly obese and obese rural Californian American Indian women (48.9%) is higher than that reported for Black women (36.6%), White women (20.3%), and American Indian and Alaska Native women nationwide (29.4%).16
Fig 1.
Body mass index groups by sex for American Indian rural adults in California (%)
Table 1 shows the sociodemographic characteristics of the morbidly obese and compares it to participants in other BMI categories. The average age of the morbidly obese was 47 years (range of 27–79). With regard to ethnic identities, 35% of the target population spoke their tribal language, 87% were enrolled in a tribe and 46% reported that they had ≥50% Indian blood. Forty-two percent were married, 29% had less than 12th grade education, 54% reported being employed and the average monthly household income was $2,126 for the morbidly obese, with a median monthly/annual household income of $1,200 and $17,500, respectively. The average weight reported by the morbidly obese participants was 266 pounds (P<.0001) (Table 2), with a range of 196–450 pounds.
Table 1.
Sociodemographic Characteristics for California rural American Indian adults
| Characteristics | Overall (N=457) |
Underweight/ normal (n=139) |
Overweight (n=109) |
Obese (n=161) |
Morbidly obese (n=48) |
P |
|---|---|---|---|---|---|---|
| mean (SE) | ||||||
| Age | 44.8 (15.9) | 44.0 (17.8) | 46.4 (16.8) | 43.6 (14.2) | 47.0 (13.4) | .39 |
| Average monthly household income | 2170(3146) | 2541(3410) | 1892(1166) | 2134(3735) | 2126(2955) | .87 |
| % | ||||||
| Female | 74.3 | 79.9 | 59.3 | 77.6 | 81.3 | .0007* |
| Married | 52.4 | 50 | 60 | 52.5 | 41.7 | .18 |
| Employed | 62.6 | 61.7 | 60.4 | 67.3 | 54.2 | .36 |
| Education <12th grade | 24.5 | 25.9 | 20.2 | 24.8 | 29.2 | .61 |
| Enrolled in a tribe | 87.1 | 90.4 | 80.2 | 89.2 | 87.0 | .10 |
| ≥50% Indian blood | 42.9 | 45.3 | 46.8 | 37.3 | 45.8 | .35 |
| Able to speak tribal language | 25.7 | 26.5 | 29.7 | 20 | 35.1 | .17 |
P: based on a comparison of four BMI categories: normal or underweight/overweight/obese/morbidly obese
significant difference between different BMI Categories at alpha=.05
Table 2.
Health related variables by BMI categories for California rural American Indian adults
| Characteristics | Overall (N=457) |
Underweight/ normal (n=139) |
Overweight (n=109) |
Obese (n=161) |
Morbidly obese (n=48) |
P |
|---|---|---|---|---|---|---|
| mean (SE) | ||||||
| Weight, pounds | 187 (46) | 140 (23) | 169 (22) | 199 (26) | 266 (51) | <.0001* |
| % | ||||||
| Good general health status | 41.0 | 41.2 | 53.2 | 38.5 | 20.8 | .002* |
| Type 2 diabetes | 18.4 | 13.0 | 14.9 | 19.3 | 38.1 | .003* |
| Arthritis | 25.1 | 21.1 | 26.7 | 22.2 | 41.9 | .04* |
| Hypertension | 25.1 | 23.5 | 19.0 | 25.3 | 42.2 | .03* |
| Limitation in activities | 28.9 | 23.8 | 24.3 | 29.4 | 51.1 | .003* |
| Arthritis/rheumatism limits activities | 8.1 | 7.9 | 8.3 | 5.6 | 16.7 | .11 |
| Back/neck problem limits activities | 7.4 | 8.6 | 3.7 | 8.1 | 10.4 | .35 |
| Walking problem limits activities | 3.3 | 2.9 | 2.8 | 4.4 | 2.1 | .81 |
| Fractures/bone/joint injury limits activities | 2.6 | 2.2 | .9 | 1.2 | 12.5 | .0001* |
| Lung/breathing problem limits activities | 1.5 | 1.4 | 1.8 | 1.2 | 2.1 | .97 |
| Hearing problem limits activities | 1.5 | .7 | 2.8 | 1.9 | 0 | .47 |
| Eye/vision problem limits activities | 2.6 | 3.6 | 1.8 | 1.9 | 4.2 | .66 |
| Heart problem limits activities | 1.5 | .7 | .9 | .6 | 8.3 | .0009* |
| Stroke problem limits activities | .9 | 0 | 0 | 1.2 | 4.2 | .04* |
| Hypertension limits activities | 1.8 | .7 | 0 | 3.1 | 4.2 | .1 |
| Diabetes limits activities | 2.0 | 1.4 | 1.8 | 1.2 | 6.3 | .16 |
| Cancer limits activities | .2 | 0 | 0 | .6 | 0 | .61 |
| Depression/Anxiety/Emotional Problem limits activities |
.4 | .7 | 0 | 0 | 2.1 | .22 |
P: based on a comparison of four BMI categories: normal or underweight/overweight/obese/morbidly obese
significant difference between different BMI Categories at alpha =.05
Morbidly obese adults reported more health problems and physical limitations than other BMI categories. Table 2 shows that obesity status and major health conditions were significant for type 2 diabetes (38%, P=.003), arthritis (42%, P=.04) and hypertension (42%, P=.03). A significantly larger proportion of the morbidly obese (51% morbidity obese vs. 29% obese) felt that their health status limited their activities (P=.003). Fracture/bone/joint injury was reported to limit activities for 12.5% of the morbidly obese, which is a significantly higher percentage compared to that for all other BMI categories (P=.0001) in the sample. Similarly, 8.3% of morbidly obese participants reported that heart problems limited activities (P=.0009) and 4.2% reported stroke problems limited activities (P=.04). Twenty one percent of the morbidly obese adults said they had good general health, which was significantly lower than the percentages reported by all other BMI categories (P=.002).
Overall, study participants reported extremely high rates of morbid obesity, twice the US adult rate, 13% vs. 5.9% respectively.16 Indeed, a striking 82% of the study sample had a BMI that placed them within the broad category range of “overweight, obese, or morbidly obese,” significantly higher than the rate reported for the general population.16 Only 14% of the sample was of normal weight and 4% underweight.
Discussion
While obesity is known as a growing epidemic in the United States, it is highly disconcerting that obesity rates among American Indians exceed those of the general population and continue to rise. Our study documents that rural California American Indian adults are critically overweight, with levels of weight gain that cause them to be significantly over-represented in the obese and morbidly obese categories. Further, it appears that American Indian women are more likely to transition into the obese, and then into the higher-risk morbidly obese group, mirroring the trend documented for the US general population.3 American Indians have long faced disparities in health; unfortunately, the risks to this population’s quality of life, health status, and risk of mortality are further compounded by such high morbid obesity rates.
The profile of the morbidly obese rural American Indian who participated in our study was female, less likely to be married, reporting low monthly income and educational attainment, middle aged, weighing between 196 and 450 pounds and reporting comorbid health problems that limited physical activities. Further, our study found that this cohort of morbidly obese had a higher level degree of Indian blood (at least 50%), spoke their tribal language and enrolled as a member of an American Indian tribe. American Indian adults who are single, with low educational levels and low income appear to be susceptible to weight gain and severe obesity, much more so than the general population. The study’s morbidly obese adults (42%) were found to be less likely to be married as compared to American Indian or Alaska Native adults nationwide (49.7%), White adults (60.8%), or Asian adults (64.9%), but more likely to be married compared to Black adults (38.5%).17 Being single may reduce the support needed for those trying to keep their weight at a healthy level.
Two factors that place American Indian communities at significantly greater risk for obesity and morbid obesity are poor diet and sedentary lifestyles. The diet of American Indians is often poorer in quality than that of other ethnic groups as many American Indian communities eat high-fat and high-sugar foods and do not consume sufficient fruit and vegetables. A general lack of physical activity also contributes to buildup of fatty tissue, which can lead to type 2 diabetes and morbid obesity.
The rural adults sampled in this study reporting low educational level and low income were found to be more susceptible to weight gain and morbid obesity as compared to the general population, similar to the findings of Kahn, Williamson and Stevens (1991).18 This cohort of morbidly obese American Indian (29%) was more likely than Black adults (25.2%) and twice as likely as White adults (15.8%) and Asian adults (13.9%) to have less than a high school diploma.17 Also, their average annual household income was reported to be the lowest of all weight categories; $17,500 (median annual income) is strikingly lower than the 2003 national median for Whites ($48,000), Blacks ($30,000), Hispanics ($33,000) and Asians ($55,500).19 This indicates the need for low literacy health education materials targeting low income and low educational level groups. Culturally-tailored cookbooks, or other materials describing techniques for purchasing low-cost nutritional foods and methods of cooking without frying foods in fat, lard or grease could be of great value for helping severely obese American Indian populations change poor cooking and eating habits. Similarly, basic, culturally-relevant and regionally-appropriate instructions for physical exercise, as well as how to accomplish increased movement as an obese or morbidly obese individual may serve as motivation to be more active, aiding weight loss efforts.
In a study of marital status and health in the general population, Schoenborn (2004) found that married adults are the healthiest and are less likely to have health problems than unmarried adults.20 Our study came to a similar conclusion, finding that a significant proportion of the morbidly obese were not married and reported poorer health status. Because of their severe weight status, the morbidly obese reported having more health problems and experienced physical limitations at a higher rate than those in lower level BMI categories. The consequences of carrying excessive weight, especially if it exceeds 100 pounds over normal weight, results in complications due to type 2 diabetes (including disabling loss of vision, loss of limbs, and neuropathy), arthritis resulting from increased weight bearing down on bones and cartilage, and high blood pressure leading to stroke and cardiovascular disease. Indeed, the study sample reported a statistically significant increase in physical limitations due to heart problems, strokes, bone fractures and joint injuries. Multiple health problems leading to severe physical limitations are major barriers to weight reduction and may contribute to increasing weight gain, which must be taken into consideration for any weight loss intervention.
The obesity epidemic in the American Indian population is a severe and multifactorial problem. Unfortunately, there is a shortage of data to inform healthcare providers, policy makers, and researchers regarding the profile of American Indians who exceed the obese category and are advancing into the morbidly obese category. This study identified American Indian females as significantly represented in the obese and the morbidly obese categories, thus we recommend prioritizing this subgroup as part of the call to action against obesity. Additionally, since those with low educational levels and low income appear to be most susceptible to weight gain and morbid obesity, it is of utmost importance to focus policy and programs efforts with careful consideration of this population’s needs and barriers. In addition, particular attention must be paid to ameliorating physical limitations in order to address the overwhelming poor health status currently experienced by morbidly obese American Indians.
Limitations of the study are that the data are self-reported and come from rural sites in California, thus results cannot be generalized to the larger population of American Indians or of those living in urban locales. Although research indicates that self-reported weight and height are accurate to a large extent, studies have shown that heavier people tend to underreport their weight more so than normal weight people.21 Nevertheless, this research provides much needed data on the obesity status of rural American Indian populations in California.
Acknowledgments
We are grateful for the editorial assistance from Briana Cardoza, MPH, Tracy Line, MPH and Fernando Martinez, MSc. This study was supported by a grant from the National Institute for Nursing Research, NIH, R01NR04528.
Contributor Information
Felicia S. Hodge, University of California, Los Angeles, School of Nursing, Berkeley, California.
Betty Geishirt Cantrell, Communities, Adolescents, Nutrition, Fitness – CANFIT, Berkeley, California.
Soeun Kim, University of California, Los Angeles, School of Nursing, Berkeley, California.
References
- 1.Sturm R. Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121(7):492–496. doi: 10.1016/j.puhe.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruhm CJ. Current and future prevalence of obesity and severe obesity in the United States. Forum for Health Economics and Policy. 2007;10(2):1–26. [Google Scholar]
- 3.U.S. Department of Health and Human Services [Last accessed on June 28, 2010];Obesity and American Indians/Alaska Natives. 2007 April; Available at: http://aspe.hhs.gov/hsp/07/AI-AN-obesity.
- 4.U.S. Department of Health and Human Services, Office of Minority Health [Last accessed on June 28, 2010];Obesity and American Indians/Alaska Natives. 2009 Available at: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=52.
- 5.Story M, Evans M, Fabsitz RR, Clay TE, Rock BH, Broussard B. The epidemic of obesity in American Indian communities and the need for childhood obesity–prevention programs. Am J Clin Nutr. 1999;69(4):747S–754S. doi: 10.1093/ajcn/69.4.747S. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention [Last accessed on December 9, 2009];Body mass index. 2009 Available at: http://www.cdc.gov/healthyweight/assessing/bmi.
- 7.U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General [Last accessed on September 6, 2009];The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity. 2001 Available at: http://www.surgeongeneral.gov/topics/obesity. [PubMed]
- 8.Gearhart RF, Gruber DM, Vanata DF. [Last accessed July 15, 2010];Obesity in the lower socio-economic status segments of American society, forum on public policy, Obesity Action Coalition. 2008 Available at: http://www.forumonpublicpolicy.com/archivespring08/gearhart.pdf.
- 9.Johnson CA, Xie B, Liu C, et al. Sociodemographic and cultural comparison of overweight and obesity risk and prevalence in adolescents in Southern California and Wuhan, China. J Adolesc Health. 2006;39:925.3l–925.e8. doi: 10.1016/j.jadohealth.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 10.Ewing R, Brownson RC, Berrigan D. Relationship between urban sprawl and weight of United States youth. Am J Prev Med. 2006;31(6):464–474. doi: 10.1016/j.amepre.2006.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 12.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 13.Obesity Action Coalition [Last accessed on July 15, 2010];All About Obesity. 2010 Available at: http://www.obesityaction.org/aboutobesity/morbidobesity/mo.php.
- 14.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Affairs (Millwood) 2002;21(2):245–254. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 15.Statistical Package for the Social Sciences, SPSS (Version 11.0) (Computer Software) Chicago, IL: [Google Scholar]
- 16.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) [Last accessed on December 11, 2009];Prevalence of overweight, obesity and extreme obesity among adults: United States, trends 1960–1962 through 2005–2006. Available at: http://www.cdc.gov/nchs/data/hestat/overweight/overweight_adult.htm.
- 17.Barnes PM, Adams PF, Powell-Griner E. Health Characteristics of the American Indian and Alaska Native Adult Population: United States, 1999–2003. Advance Data from vital and Health Statistics: no 356. National Center for Health Statistics; Hyattsville, MD: 2005. [PubMed] [Google Scholar]
- 18.Kahn H, Williamson D, Stevens J. Race and weight change in US women: the roles of socioeconomic and marital status. Am J Pub Health. 1991;81(3):319–323. doi: 10.2105/ajph.81.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeNavas W, Bernadette C, Proctor D, Mills RJ. U.S. Census Bureau, Current Population Reports, Income, Poverty, and Health Insurance Coverage in the United States: 2003. U.S. Government Printing Office; Washington, D.C: 2004. pp. 60–226. [Google Scholar]
- 20.Schoenborn C. Marital Status and Health: United States, 1999–2002, Advance Data from Vital and Health Statistics; no 351. National Center for Health Statistics; Hyattsville, MD: 2004. [PubMed] [Google Scholar]
- 21.Perry GS, Byers TE, Mokdad AH, Serdula MK, Williamson DF. The validity of self-reports of past body weights by U.S. adults. Epidemiol. 1995;6:1. doi: 10.1097/00001648-199501000-00012. [DOI] [PubMed] [Google Scholar]