Abstract
This report summarizes highlights of the ‘Philadelphia Chromosome Symposium: Past, Present and Future’, held September 28, 2010, to commemorate the 50th anniversary of the discovery of the Philadelphia chromosome. The symposium sessions included presentations by investigators who made seminal contributions concerning the discovery and molecular characterization of the Ph chromosome and others who developed a highly successful therapy based on the specific molecular alteration observed in chronic myelogenous leukemia. Additional presentations highlighted future opportunities for the design of molecularly targeted therapies for various types of cancer. Also included here are reminiscences connected with the discovery of the Ph chromosome by David Hungerford and Peter Nowell, the discovery that the abnormality arises from a chromosomal translocation, by Janet Rowley, and the cloning of the 9;22 translocation breakpoints by Nora Heisterkamp, John Groffen and colleagues.
Keywords: BCR, ABL, translocation, imatinib, targeted therapies
To celebrate the 50th anniversary of the discovery of the Ph chromosome, the city bearing its name hosted the ‘Philadelphia Chromosome Symposium: Past, Present and Future – the 50th Anniversary of the Discovery of the Philadelphia Chromosome’. The main activities were held on September 28, 2010, which was proclaimed ‘Philadelphia Chromosome Day’ by Philadelphia’s City Council and Mayor Michael Nutter. The symposium was held, appropriately, in the city’s historic area, near the Liberty Bell, Independence Hall, and the National Constitution Center. The symposium was sponsored by Fox Chase Cancer Center (FCCC), where David A. Hungerford spent his entire professional life, and the location of the event was not far from the University of Pennsylvania, School of Medicine, the institution with which Peter C. Nowell has been associated since 1956.
The symposium included sessions devoted to the discovery and molecular characterization of the Ph chromosome, the development of a successful treatment for chronic myelogenous leukemia (CML), and future opportunities for the design of molecularly targeted therapies for various types of cancer. The symposium was conceived and organized by Joseph R. Testa, and the invited speakers included Felix Mitelman, Peter Nowell, Janet D. Rowley, Nora C. Heisterkamp, Owen N. Witte, Nicholas B. Lydon, John M. Goldman, Charles L. Sawyers, and William R. Sellers. In addition, retrospective posters and memorabilia, including the original microscope used to first identify the Ph chromosome, were presented by Jennifer J.D. Morrissette and Peter Nowell and by two of us who worked closely with David Hungerford (H. Sharat Chandra and Alice Hungerford).
The atmosphere of the meeting was both electric and passionate, with many in attendance expressing gratitude for the opportunity to celebrate this special event. Despite being only a 1-day event, there were registrants from 18 States and 10 different countries. More than a few of the cytogeneticists mentioned to the organizers that the discovery of the Ph/9;22 translocation provided the spark that drew them into the field. In addition to the outstanding presentations and posters, Alice Hungerford read a poignant letter of gratitude to the scientific community from basketball legend Kareem Abdul-Jabbar, the NBA′s all-time leading scorer, who was diagnosed with CML two years ago; his letter credited imatinib for permitting him to be alive and well today. Another CML patient, Ryan Corbi, gave a heart-warming testimonial, telling the audience that he has been able to lead a healthy, full life the last five years thanks to imatinib. In addition to internationally prominent speakers, four of whom (Nowell, Rowley, Lydon and Sawyers) have received Lasker Awards for work on CML, others in attendance included Nobel Laureate Baruch S. Blumberg and Lasker awardee Alfred G. Knudson, Jr. Some of the speakers, organizers and other dignitaries in attendance are shown in Figure 1. Cytogeneticists who attended the symposium are shown in Figure 2.
Fig. 1.
Speakers, organizers and other invited guests who attended the “Philadelphia Chromosome Symposium”. Front, from left: Janet Rowley, Alice Hungerford (holding photo of David Hungerford), John Goldman, Nora Heisterkamp, Charles Sawyers, and Hope Punnett. Rear, from left: Felix Mitelman, Alfred Knudson, Joseph Testa, Peter Nowell, Nicholas Lydon, William Sellers, and Owen Witte.
Fig. 2.
Group photograph of cytogeneticists who attended the “Philadelphia Chromosome Symposium: Past, Present and Future,” to commemorate the 50th anniversary of the discovery of the Philadelphia chromosome. The Symposium attracted nearly 200 registrants from 18 States and 10 countries, including Mexico, Canada, India, Australia, and five European nations.
In this report, we summarize highlights of presentations by investigators who made seminal scientific contributions in the Philadelphia chromosome ‘saga’. One recurring theme of the symposium was that answers to exciting questions often languished because of the technical or methodological limitations of the day. Interestingly, most of the major breakthroughs took a decade or more, awaiting the technological tools needed to advance the field. For example, the discovery of the Ph by Nowell and Hungerford in 1960 (1-3) awaited the development of improved culture and chromosome preparation methods, the discovery that the Ph chromosome arises from a translocation by Rowley in 1973 (4) required the development of chromosomal banding techniques, and the cloning of the t(9;22) breakpoints by John Groffen, Heisterkamp and colleagues in 1983-1984 (5, 6) required important advances in recombinant DNA technology. These discoveries were conducted painstakingly in ways that we believe are historically important to document for future generations. Thus, we decided that this paper should also include reminiscences surrounding each of these major genetic discoveries.
Overview
Felix Mitelman presented an elegant historical overview of cancer cytogenetics. One of the displays at the symposium juxtaposed Hungerford’s original microscope with a state-of-the-art cytogenetic workstation of today. Seeing the stark contrast between these microscopes, one was reminded of how far we have come technologically over the last 50 years; paralleling these technical advances, Mitelman traced the history of cancer cytogenetics from the time of the discovery of the Ph chromosome to our current understanding of the molecular implications of cancer-related recurrent chromosomal rearrangements. He noted that approximately 1000 recurrent balanced chromosomal rearrangements have now been reported to date, and 600 fusion genes have been identified. He also pointed out that interest in genetic aspects of cancer erupted after the discovery of the Ph translocation by Rowley and that the remarkable success of imatinib for the treatment of Ph-positive CML has led to the emergence of molecularly targeted therapies, a field now known as ‘personalized’ medicine.
Before embarking on this quintessential translational research journey, it would be necessary to improve the methods used to culture and prepare metaphase spreads from hematopoietic cells, and the distinct skill sets of Hungerford and Nowell were collectively primed to do so.
Discovery of the Ph chromosome
Peter Nowell gave an overview of the very early history of cytogenetics from the time of Wilhelm von Waldemeyer, who coined the term ‘chromosome’ (colored body) in the late 1880s, and David P. von Hansemann, who in 1890 described multipolar mitoses and other aberrant mitotic figures in carcinoma samples and suggested that these aberrant cell divisions were responsible for the abnormal chromatin content found in cancer cells. Nowell also discussed the work by Theodor Boveri, who proposed that cancer begins with a single cell in which the chromosomal makeup becomes scrambled, permitting cells to proliferate uncontrollably. Nowell characterized the 1920s to the 1950s as the ‘dark ages’ of cytogenetics due to technical limitations which are described in detail in the reminiscences portion of this paper. In his presentation, he referred to himself as the ‘Prince of Serendip’, after the fairy-tale ’The Three Princes of Serendip′, in which the heroes were ‘…. always making discoveries, by accidents and sagacity, of things they were not in quest of′. He explained that he began studying the proliferation and differentiation of human leukemic cells in short-term cultures. The cells were grown on slides and, in accordance with his training in pathology, he accidentally rinsed some slides under tap water and stained them with Giemsa prior to examining them under the microscope. Through this accident, he was able to clearly see metaphase spreads, which led him to seek the assistance of a young cytogeneticist, David Hungerford (see reminiscences).
By the end of the 1960s, it seemed as if the Ph chromosome was an exception and that such specific chromosomal changes would not be characteristic of other malignancies. Moreover, it was not clear at that time whether the Ph chromosome was a simple deletion or whether there was a translocation of chromosomal material. This was of course before Rowley’s discovery of the translocation underlying the Ph chromosome and all the other exciting developments since then, recounted at this commemorative meeting by some of the key scientists themselves. In 1960, who could have foreseen that the observation by Nowell and Hungerford would become, as Michael V. Seiden, President of FCCC, said at the symposium, “…. the first page of the first chapter of what is now called personalized medicine.”
Discovery of the 9;22 translocation
Janet Rowley summarized how she used a combination of solid Giemsa-staining and quinacrine (Q) banding to first demonstrate that the Ph was the result of a translocation, not a deletion, with exchange of material between chromosomes 9 and 22 (see reminiscences). She reminded the audience that the presence of the t(9;22) in all or nearly all bone marrow cells from CML patients implied that the abnormality was involved in the initiation, rather than as a consequence, of the malignancy. She and her colleagues at the University of Chicago went on to report a number of other recurrent translocations in various subtypes of acute leukemia, including the t(15;17) specifically associated with acute promyelocytic leukemia (APL). Her descriptions of these clinicopathologic-cytogenetic associations quelled any remaining skepticism about the relationship between clonal chromosome rearrangements and leukemogenesis. However, she noted that many questions remained, even today, such as why and how translocations occur and how secondary cytogenetic changes lead to the acute, blastic phase of the disease.
Molecular characterization of the t(9;22)
Nora Heisterkamp presented a history of the molecular characterization of the Ph chromosome and described the very laborious efforts required to determine the breakpoints on chromosomes 9 and 22 (see reminiscences). John Groffen, Heisterkamp and colleagues later cloned genomic DNA from CML patients and identified chromosomal breakpoints within a limited region on chromosome 22, which they dubbed the ‘breakpoint cluster region’ (BCR) (6). Two of 19 CML patients who did not have rearrangements within the BCR lacked the Ph chromosome. The highly specific presence of a chromosomal breakpoint within BCR in Ph-positive CML patients strongly suggested the involvement of the BCR gene, which encodes a phosphoprotein associated with serine/threonine kinase activity, in this type of leukemia. The ABL gene encodes a tyrosine kinase whose activity is tightly regulated, and both genes were found to be truncated as a result of the formation of the t(9;22). Two fusion genes were generated: BCR-ABL on the derivative 22q– chromosome and ABL-BCR on chromosome 9q+.
The identification of the genes involved in the t(9;22) led to considerable interest in the mechanism of action of the oncogenic fusion product. Owen Witte’s presentation summarized seminal work performed in his laboratory, which showed expression of a mutant form of ABL both in a leukemia cell line derived from a CML patient and in primary cells from CML patients (7, 8). Western blot analysis revealed that mutant ABL ran at a different molecular weight, 210 kD, than the normal ABL protein product, suggesting differences between the native protein and the fusion protein found in CML cells. Two groups showed that the mRNA product of the ABL gene seen in Ph-positive CML cells was actually a fusion transcript of the two genes, BCR and ABL, and they hypothesized that the expressed fusion protein was a necessary step in the evolution of CML (9, 10). Witte and his colleagues showed that the BCR-ABL fusion protein present in CML cells contained tyrosine kinase activity comparable to the activity seen in v-ablexpressing cells, due to the replacement of the first exon of ABL with sequences from the BCR gene, resulting in a BCR-ABL fusion gene whose protein product showed enhanced tyrosine kinase activity (11, 12). In vivo experiments demonstrated that introduction of the BCR-ABL fusion gene into irradiated mice led to the development of a CML-like disease (13, 14). Thus, the presence of the BCR-ABL fusion protein over-expressing an aberrant tyrosine kinase in the leukemia cells of virtually every patient with CML provided strong evidence of its pathogenetic role.
Imatinib – preclinical studies
The specificity of the BCR-ABL fusion and its presence in all cases of chronic phase CML led Brian Druker and Nicholas Lydon to consider this molecule as a target for small molecule therapy. Since the critical oncogenic event had been shown to be the creation of a constitutively active tyrosine kinase, the tyrosine pocket domain was an attractive target for small molecule regulation. In his presentation, Lydon noted that there were many individuals who did not share the same optimistic view. Some of the objections (as reviewed in (15)) were that molecules could not be developed with enough specificity for the BCR-ABL kinase that would not cross react with other critical tyrosine kinases necessary for normal cell functions. Another concern was that even if specific small molecule inhibitors could be developed, would they be sufficient to eradicate or control the disease? The first inhibitors were a class of compounds called 2-phenylaminopyrimidines, which were able to down-regulate activity from protein kinase C (PKC), ABL, and platelet derived growth factor receptor (PDGFR) (16). Modifications of the lead compound, particularly the substitution of a methyl group of the anilinophenyl ring, retained inhibition against ABL and PDGFR kinases, but had no activity against PKC (16). The efficacy of the small molecule tyrosine kinase inhibitors, determined by the ablation of phosphotyrosine, was determined by in vitro studies using the monoclonal antibody 4G10, developed by Brian Druker. These studies led to the identification of STI571, a specific inhibitor of the ABL1 and c-kit tyrosine kinases and without pleiotropic effects that would render the drug intolerable (17). The results provided strong evidence for an essential role of BCR-ABL kinase activity in CML and demonstrated the potential for the development of anticancer drugs based on the specific molecular alteration that drives a given human malignancy.
Clinical studies of imatinib and therapeutic horizons
One critical piece to develop a strategy for treatment of CML was to identify patients who would benefit from the treatment. One of the symposium speakers, John Goldman, has had a history of pioneering strategies for the treatment of patients with CML, showing efficacy with autografting of peripheral blood stem cells as well as allogeneic stem cell transplantation for CML (reviewed in (18)). His development of sensitive PCR protocols to detect BCR-ABL transcripts for studies of minimal residual disease (19) allowed treatment efficacy to be monitored, and remains a gold-standard in determining molecular remission of CML patients. Using these methods and others, Goldman and his colleagues confirmed the loss of BCR-ABL transcripts in preclinical trials and were the first to treat CML patients in the clinical trials of STI571 (imatinib; brand name: Gleevec).
The response to imatinib was initially overwhelmingly positive. However, over time a subset of patients was found to lose their cytogenetic response to Gleevec due to mutations in the BCR-ABL kinase domain. Another symposium speaker, Charles Sawyers, became interested in BCR-ABL during a postdoctoral fellowship in Witte’s laboratory. Sawyers became involved in the early clinical trials that evaluated Gleevec and collaborated with other translational researchers. Building on the development of Gleevec as a model, Sawyers began working with scientists at Bristol-Myers Squibb on a new drug called Sprycel (dasatinib), designed as a second-line therapy for patients who no longer responded to Gleevec. His approach combined DNA studies of patients’ CML cells with structural biology data. In clinical trials led by Sawyers and collaborators at M.D. Anderson Cancer Center, Sprycel was shown to be effective against all but one of the commonly occurring BCR-ABL mutations (20). “That′s now the last nut to crack with CML,” said Sawyers. A potential treatment for patients with that stubborn mutation, T315I, is now in phase I clinical trials. Sawyers indicated that physicians will ultimately be able to offer patients a pill containing a cocktail of BCR-ABL inhibitors that work against all common mutations of the enzyme, dramatically reducing the likelihood of drug resistance.
Ph-positive CML is a crucial example of the genetic-therapeutic paradigm. Targeted therapies such as imatinib for patients with CML have provided dramatic benefit in this disease; however, the extent to which this experience may apply to the majority of human cancers is uncertain. In most cancers, monotherapies are unlikely to lead to such dramatic results as have been seen in CML. Recent studies have shown that many cancer genome aberrations converge to activate a limited set of downstream oncogenic signaling pathways. Among the most heavily affected oncogenic pathways are the PI3K and the MAPK signaling pathways, which are central regulators of oncogenic transformation and tumor maintenance (21). The symposium’s final speaker, William Sellers, provided a comprehensive overview of the future of targeted therapies. Sellers’ work has unraveled the role of genetic alterations in prostate cancer, including the role of PTEN mutations in deregulating the PI3K pathway (22). Rather than providing therapeutic strategies for each individual mutation in different cancer types, Sellers proposed that targeting modulators of critical downstream pathways is an increasingly attractive option (21). Small synthetic molecules targeting these pathways have been developed and are currently undergoing clinical testing. Increasingly, pharmaceutical companies are using new approaches for drug development that are hypothesis driven and employ large-scale combination screens of hundreds of tumor cell lines and compounds. These exciting future opportunities continue the legacy of the discovery of the Ph chromosome.
REMINISCENCES
Nowell and Hungerford
The collaboration between Nowell and Hungerford, a clinical scientist and a geneticist trained in the basic sciences, respectively, was rare in those days. The two investigators had complementary skills and abilities that enabled a discovery that neither might have been able to make alone. In a personal account of their work, Nowell has described this discovery as being the outcome of a ‘happy collaboration’ (23). He has more recently provided a personal perspective covering over four decades of research on CML (24). Sometime around 1973 Hungerford was diagnosed with multiple sclerosis, which cut short his career and ultimately led to his death in 1993.
In a poster presented at the symposium, Sharat Chandra followed Hungerford’s career beginning at The Institute for Cancer Research, as FCCC was then known. From 1951-1955, Hungerford had trained in chromosome cytology first with Jack Schultz and George Rudkin and later with T. S. Hauschka. Hungerford had experimented with various combinations of prefixation treatment with salt solutions (25, 26) and exposure to colchicine (27) reported by others and made chromosome preparations by the squash technique (28). With Marie DiBerardino, he made a detailed investigation of the effects of various pre-treatment protocols on cells of mouse and frog embryos (29). The experience gained from these time-consuming investigations would prove useful in his subsequent work with Nowell on chromosomes of leukemic cells. In addition, Hungerford continued to experiment with various hypotonic solutions for prefixation treatment of cells, the most successful of which was 0.075 M KCl (30), now in widespread use. In 1955, Stanley Reimann, the Institute’s first director, urged Hungerford to work on human chromosomes, an area in which Schultz and Patricia St. Lawrence had earlier been active (31) and begin graduate work at the University of Pennsylvania. He would not come to know Nowell until 1957, when Hungerford received a phone call from him offering to initiate a collaboration (see below).
As noted earlier, Nowell was a new faculty member at the University of Pennsylvania School of Medicine when he first started culturing human leukemic cells and accidentally rinsed some slides under tap water before staining them. As he noted in a review paper after receiving the Lasker Award, “Unaware that this procedure was an accidental rediscovery of the technique of hypotonic cytogenetic preparation, I simply noted that my slides contained metaphase stage chromosomes. I knew nothing of cytogenetics, but this seemed worth pursuing and I was soon directed to a graduate student, David Hungerford, who was attempting to find material for his thesis project. We promptly began a collaboration: I obtained the cells and cultured them, and Dave (using the ′squash′ technique of the time) examined both acute and chronic leukemic cells from a number of patients. The first positive finding was his identification of a characteristic small chromosome in the neoplastic cells of two male patients with CML. Subsequently, using an improved air-drying technique of slide preparation (32), we identified the same tiny chromosome in other patients” (33). At the symposium, Nowell chuckled about the fact that their Science paper was only a paragraph long. In fact, although that is the paper most of us cite, it was actually a meeting abstract, and publication of a peer-reviewed short letter and a full report appeared elsewhere (2, 3).
In accordance with the nomenclature of the First International Conference on Cytogenetics, held in Denver in 1960, the minute chromosome was referred to as the Philadelphia chromosome, Ph1 for short, in honor of the co-discoverers (34). At the symposium, Mitelman quipped that the superscript ‘1’ in the abbreviation is no longer used, much to the delight of secretaries and publishers around the world. A photo of Nowell and Hungerford shortly after publication of the report of the Ph chromosome is shown in Fig. 3.
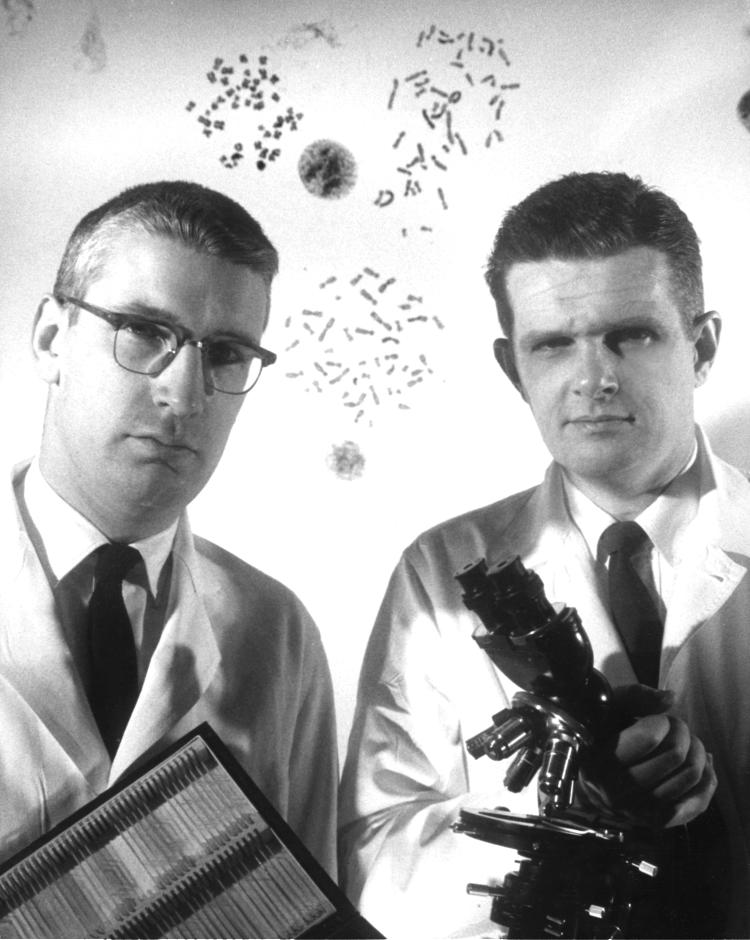
Fig. 3.
Peter Nowell (left) and David Hungerford (right) in 1960, soon after reporting their discovery of the Ph chromosome.
Rowley
In 1961-62, Janet Rowley and her family accompanied husband Donald Rowley, an immunologist, when he took a sabbatical leave in Oxford, England. Rowley obtained a position as a trainee in the Radiology Laboratory at Churchill Hospital in Oxford, where she learned human cytogenetics. During another of her husband′s sabbaticals, from 1970 to 1971, she also took a leave of absence and again worked at the laboratory in Oxford, this time learning chromosomal banding analysis. She had found a number of clonal chromosomal abnormalities in leukemias and pre-leukemias (now MDS) in the 1960s, but there was no way to tell whether or not the abnormalities were the same in different patients. The consequences of the answers would be profound. She had found that the most common changes were gains or losses of the C group chromosomes (6-12 plus the X), which was the largest group. Whether the changes were random or specific was impossible to answer before 1970. Banding analysis could answer this question. Joseph Testa, then a postdoctoral trainee in Rowley’s laboratory, recalls with fondness hearing Rowley explain that she was in an English pub when first excitedly discussing the potential application of these new banding methods for more precise analysis of bone marrow chromosomes from leukemias and other hematopoietic disorders.
In 1972, Rowley had collected bone marrow samples from several CML patients with extra C group chromosomes that she had studied in the acute blast phase. She recalled that, “At the time, I used quinacrine fluorescence, which faded quickly under ultraviolet illumination, so I rephotographed the metaphase spreads I had previously photographed with standard Giemsa-stain (unbanded), which provided clear images of the size and shape of each chromosome.” She cut out the corresponding unbanded and banded chromosomes from each pair of spreads, which permitted her to determine the identity of each individual chromosome. “I did this at home on my dining room table, because I worked only three days a week. With my sons at school, I had the quiet I needed to concentrate on the chromosomes. Initially I studied two patients, both with extra C-group chromosomes. It was immediately clear that they both had one or two extra chromosomes 8. Analysis of spreads from other patients with an extra C-group chromosome showed that they, too, most often had an extra chromosome 8, so that lent credence to the idea that chromosome changes were not just helter-skelter!” Because metaphases from these blast phase cells had a number of abnormalities, she looked carefully at all of the chromosomes. “The cells had the Ph chromosome, but they all had extra pale material at the end of the long arm of a chromosome 9. It could be a translocation!”, she thought excitedly. Rowley had already discovered one translocation in AML involving chromosomes 8 and 21 (35), so she wondered whether this was another. She also had metaphase spreads from the chronic phase of the disease, which she stained, photographed and analyzed. She found that the chronic phase cells had only one alteration, the possible translocation. “I studied four patients, wrote a letter and sent it to Nature, only to have it rejected relatively promptly. By that time, I now had studied seven patents, and I had obtained peripheral blood from several chronic phase patients and could show that the PHA-stimulated T cells were normal. So I updated and revised the letter; this time it was accepted, but it took about five months before it was published (4). The observation was so easy to make that I was extremely fearful that I would be scooped, because I had talked about this finding at meetings of cytogeneticists and, later, physicians.” As it turned out, she was not scooped, and the paper was published in June of 1973. A photograph of Rowley from about the time of her discovery is shown in Fig. 4.
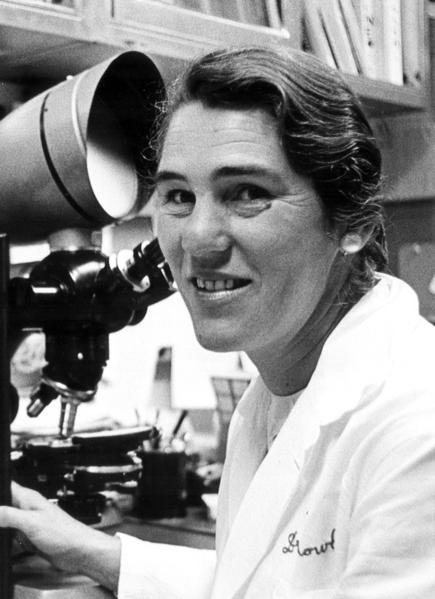
Fig. 4.
Photograph of Janet Rowley from the early 1970s, at about the time of her discovery that the Ph chromosome arises from a 9;22 translocation.
Rowley recalled that many questions remained at the time; most importantly, what was going on? Was the translocation the same in different patients? She noted that, “In a few years, I could state that the answer appeared to be yes. But until John Groffen and Nora Heisterkamp cloned the breakpoint and identified the genes, we really did not know ‘what was going on’!”
Heisterkamp and Groffen
John Groffen and Nora Heisterkamp were graduate students in Groningen, the Netherlands in the period from 1970-1980 when the techniques that made it possible to molecularly clone DNA, such as the isolation of restriction enzymes and DNA ligases, were being developed. Groffen decided he wanted to learn molecular cloning. Groffen and Heisterkamp recalled that at the time, the world-wide scientific community had concerns about potential biohazards of this new technology, and in 1974 a moratorium had been put in place on certain recombinant DNA experiments in the USA. In 1976, the first NIH research guidelines for recombinant DNA were developed. Groffen contacted Richard Flavell, who was at the Dutch Cancer Institute (NKI) in Amsterdam at the time, but he was in the process of moving his laboratory to the ICRF in London, UK because in 1978 recombinant DNA work was not permitted in the Netherlands. Groffen joined the Flavell lab in the UK just after their move and was able to spend a year working there with Frank Grosveld and others to learn these techniques, including how to make DNA libraries with substantially larger inserts, using cosmid vectors.
After completing their doctoral studies, Groffen and Heisterkamp became Fogarty Fellows in the laboratory of John Stephenson, a virologist, at the NCI – Frederick Cancer Research Facility (FCRF) in Maryland, USA. Stephenson was interested in transforming type C RNA viruses, which had transduced a segment of the feline (v-fes, v-fms) or mouse (v-abl, v-raf) genomes. To be able to examine the human DNA sequences homologous to these virally transduced sequences, Groffen started with the first steps of constructing a cosmid library in 1981, before returning to Flavell’s lab in the UK to finish it. At that time, Gerard Grosveld was doing work related to his doctoral studies in the same lab.
Groffen flew to Philadelphia with a box full of bacterial plates containing the cosmid library as hand luggage, and, after some anxious moments with the customs agents, was allowed to carry on. By October 1981, they had cloned parts of the human ABL locus from this cosmid library and mapped and characterized the location of the Abl-homologous regions. A month later, they obtained DNAs of somatic cell hybrids from Nigel Spurr in Walter Bodmer’s lab in the UK, to try to localize the ABL gene on a particular human chromosome, an effort that stretched out over a few months, as some hybrids were either not informative or the DNAs were undigestable. After repeated experiments, they obtained sufficient evidence to state in June 1982 that the human ABL gene was located on chromosome 9, possibly in the region involved in the t(9;22) (36).
In the summer of 1982, Frank Grosveld paid a visit to the USA and gave a seminar at the FCRF. In the evening, while enjoying a glass of wine, Groffen, Heisterkamp and Grosveld talked about ABL and the idea that there might be a connection with CML, because ABL was located on chromosome 9 and in the Ph translocation there usually was a clearly visible 9q+ derivative chromosome that had acquired DNA from chromosome 22. According to Groffen and Heisterkamp, “As fate would have it, Frank said that his brother Gerard had moved back to Holland and was now working at the Erasmus University, in the lab of Dirk Bootsma. Gerard had obtained his Ph.D. and had been recruited to clone the Ph chromosome breakpoint. At the time Anne Hagemeijer led a group in the same department which was making somatic cell hybrids that contained the 22q− or the 9q+ chromosome. Frank Grosveld suggested that Groffen call his brother. This happened, and Groffen and Heisterkamp sent ABL probes to Rotterdam.” Using these somatic cell hybrids to separate the derivative chromosome 9 from the Ph (derivative chromosome 22), de Klein et al. then showed that the ABL proto-oncogene was present on the Ph chromosome and not on the derivative chromosome 9, indicative of a reciprocal exchange between chromosomes 9 and 22 (37).
In August 1982, Groffen and Heisterkamp isolated DNA from 3 CML patients, but they found no evidence of any rearrangements of ABL. They decided to ‘walk’ more upstream, to the 5’ of the piece of DNA they had cloned, with the idea that perhaps there could be a breakpoint there. However, the cosmid library Groffen had made did not contain clones that extended to the 5’ end, and so they made a phage library of human DNA and screened that with a probe from the 5’ end of ABL. Progress was very slow, but bit by bit they extended the stretch of known DNA by cloning and mapping it. Mapping meant determining the location of sites that were cut by different restriction enzymes and their initial low-tech approach to this was to cut out strips of paper to represent a length of DNA and to try to fit them together on a large glass plate! When they had made a map of the new piece of DNA, they made probes from it and hybridized it to Southern blots of the 3 CML DNAs.
In February 1983, they saw something extremely exciting on a Southern blot that had been hybridized to a new probe they had just isolated. Heisterkamp and Groffen described it as follows: “The floor on which we worked had a huge darkroom and tanks for the manual developing of X-ray films. You would stand there with the red light on and wait until your eyes adjusted to the gloom. Then you would take the exposed film out of the cassette, attach it to a metal bracket and immerse it in developer. You could monitor a bit what was happening by dipping it out of the tank and seeing black areas emerge. It was always the best part of a day and we usually did this together – you sometimes literally would not know what could develop. The day that we developed Southern blot #57 was a day we will never forget. Seeing an extra band in the lane that contained BamHI-digested DNA of one CML patient was the most exciting moment in our career.”
The only way to find out what that extra band meant was to molecularly clone this abnormal DNA fragment so it could be examined in more detail. By late May of 1983, they had a recombinant DNA clone that contained this piece of DNA, and they then used a 1.2 kb-probe from the part of this fragment that did not line up with the ABL map to show that it originated from chromosome 22, using somatic cell hybrid DNAs that had been sent to them from Rotterdam. The groups from the USA and the Netherlands submitted a jointly co-authored manuscript to Nature reporting these findings, which were published in November 1983 (5). Groffen and Heisterkamp next cloned a chimeric breakpoint fragment from one of the CML patients, which contained a piece of chromosome 22 joined to a segment upstream of the ABL gene. Using the same cosmid library and a molecular probe from that piece of chromosome 22 DNA, they were able to clone and map the region on chromosome 22 which contained that one breakpoint. To their surprise, they found it contained breakpoints of all the CML DNAs they had available. Because of this, they dubbed this region the “breakpoint cluster region” (BCR), which they later showed contained a gene (6, 38). BCR/ABL would become the first of now hundreds of fusion genes that have been identified in human malignancy.
Acknowledgments
The authors thank all of the speakers for contributing to the success of the Philadelphia Chromosome Symposium. Joseph Testa, being at Fox Chase Cancer Center for two decades, conceived of the idea of the symposium a number of years earlier, but the program might not have come about without the encouragement of Janet Rowley and Felix Mitelman. Rowley, Alice Hungerford and Suresh C. Jhanwar provided much appreciated input and calming perspective as representatives of the scientific organizing committee. We thank Michael V. Seiden, J. Robert Beck, and Jeff Boyd for embracing this special event and providing institutional support. We also express our gratitude to the following for assistance in organizing the symposium: Lisa Bailey, Louise Blasick, Norma Gentner, Frank Hoke, Jessica Hui, Joe Hurley, Kathy Ireton, Turid Knutsen, Diana Quattrone, Chris McKinney, Kathy Smith, Tom Stephano, Kathy Truesdale, Karen Trush, and Bob Wilkens. We also thank John Groffen for contributions to the reminiscences regarding the cloning of the 9;22 translocation breakpoints and Vania N. Aikawa for assistance with the preparation of portions of the meeting summaries. Preparation of this article was aided in part by NCI grant P30 CA006927 (to Fox Chase) and by a grant to H. Sharat Chandra from the Indian National Science Academy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nowell PC, Hungerford DA. A minute chromosome in human chronic granulocytic leukemia. Science. 1960;132:1497. doi: 10.1126/science.144.3623.1229. (abstract) [DOI] [PubMed] [Google Scholar]
- 2.Nowell PC, Hungerford DA. Aetiology of leukæmia. Lancet. 1960;275:113–4. [Google Scholar]
- 3.Nowell PC, Hungerford DA. Chromosome studies on normal and leukemia human leukocytes. J Natl Cancer Inst. 1960;25:85–109. [PubMed] [Google Scholar]
- 4.Rowley JD. A new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature. 1973;243:290–3. doi: 10.1038/243290a0. [DOI] [PubMed] [Google Scholar]
- 5.Heisterkamp N, Stephenson JR, Groffen J, et al. Localization of the c-abl oncogene adjacent to a translocation breakpoint in chronic myelocytic leukemia. Nature. 1983;306:239–42. doi: 10.1038/306239a0. [DOI] [PubMed] [Google Scholar]
- 6.Groffen J, Stephenson JR, Heisterkamp N, et al. Philadelphia chromosomal breakpoints are clustered within a limited region, bcr, on chromosome 22. Cell. 1984;36:93–9. doi: 10.1016/0092-8674(84)90077-1. [DOI] [PubMed] [Google Scholar]
- 7.Witte ON, Rosenberg NE, Baltimore D. Identification of a normal cellular protein cross-reactive to the major Abelson murine leukaemia virus gene product. Nature. 1979;281:396–8. doi: 10.1038/281396a0. [DOI] [PubMed] [Google Scholar]
- 8.Konopka JB, Watanabe SM, Witte ON. An alteration of the human c-abl protein in K562 leukemia cells unmasked associate tyrosine kinase activity. Cell. 1984;37:1035–42. doi: 10.1016/0092-8674(84)90438-0. [DOI] [PubMed] [Google Scholar]
- 9.Shtivelman E, Lifshitz B, Gale RP, et al. Fused transcript of abl and bcr genes in chronic myelogenous leukemia. Nature. 1985;315:550–4. doi: 10.1038/315550a0. [DOI] [PubMed] [Google Scholar]
- 10.Stam K, Heisterkamp N, Grosveld G, et al. Evidence of a new chimeric bcr/c-abl mRNA in patients with chronic myelocytic leukemia and the Philadelphia chromosome. N Engl J Med. 1985;313:1429–33. doi: 10.1056/NEJM198512053132301. [DOI] [PubMed] [Google Scholar]
- 11.Konopka JB, Watanabe SM, Singer JW, et al. Cell lines and clinical isolates derived from Ph1-positive chronic myelogenous leukemia patients express c-abl proteins with a common structural alteration. Proc Natl Acad Sci USA. 1985;82:1810–4. doi: 10.1073/pnas.82.6.1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis RL, Konopka JB, Witte ON. Activation of the c-abl oncogene by viral transduction or chromosomal translocation generates altered c-abl proteins with similar in vitro kinase properties. Mol Cell Biol. 1985;5:204–13. doi: 10.1128/mcb.5.1.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daley GQ, Van Etten RA, Baltimore D. Induction of chronic myelogenous leukemia in mice by the P210bcr/abl gene of the Philadelphia chromosome. Science. 1990;247:824–30. doi: 10.1126/science.2406902. [DOI] [PubMed] [Google Scholar]
- 14.Kelliher MA, McLaughlin J, Witte ON, et al. Induction of a chronic myelogenous leukemia-like syndrome in mice with v-abl and BCR/ABL. Proc Natl Acad Sci USA. 1990;87:6649–53. doi: 10.1073/pnas.87.17.6649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lydon NB, Druker BJ. Lessons learned from the development of imatinib. Leuk Res. 2004;28(Suppl 1):S29–38. doi: 10.1016/j.leukres.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Buchdunger E, Zimmermann J, Mett H, et al. Inhibition of the Abl protein-tyrosine kinase in vitro and in vivo by a 2-phenylaminopyrimidine derivative. Cancer Res. 1996;56:100–4. [PubMed] [Google Scholar]
- 17.Druker BJ, Talpaz M, Resta DJ, et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med. 2001;344:1031–7. doi: 10.1056/NEJM200104053441401. [DOI] [PubMed] [Google Scholar]
- 18.Goldman JM. Allogeneic bone marrow transplantation: state of the art and future directions. Bone Marrow Transplant. 1989;4(Suppl. 1):133–4. [PubMed] [Google Scholar]
- 19.Cross NC, Melo JV, Feng L, et al. An optimized multiplex polymerase chain reaction (PCR) for detection of BCR-ABL fusion mRNAs in haematological disorders. Leukemia. 1994;8:186–9. [PubMed] [Google Scholar]
- 20.Shah NP, Nicoll JM, Nagar B, et al. Multiple BCR-ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia. Cancer Cell. 2002;2:117–25. doi: 10.1016/s1535-6108(02)00096-x. [DOI] [PubMed] [Google Scholar]
- 21.Paez J, Sellers WR. PI3K/PTEN/AKT pathway. A critical mediator of oncogenic signaling. Cancer Treat Res. 2003;115:145–67. [PubMed] [Google Scholar]
- 22.Stuart D, Sellers WR. Linking somatic genetic alterations in cancer to therapeutics. Curr Opin Cell Biol. 2009;21:304–10. doi: 10.1016/j.ceb.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Nowell PC. A happy collaboration. Fox Chase. 1986;7:3–4. [Google Scholar]
- 24.Nowell PC. Progress with chronic myelogenous leukemia: a personal perspective over four decades. Annu Rev Med. 2002;53:1–13. doi: 10.1146/annurev.med.53.082901.103519. [DOI] [PubMed] [Google Scholar]
- 25.Hsu TC, Pomerat CM. Mammalian chromosomes in vitro. II. A method for spreading the chromosomes of cells in tissue culture. J Hered. 1953;44:23–9. [Google Scholar]
- 26.Hughes A. Some effects of abnormal tonicity on dividing cells in chick tissue cultures. Q J Microsc Sci. 1952;93:207–19. [Google Scholar]
- 27.Levan A. Colchicine-induced c-mitosis in two mouse ascites tumors. Hereditas. 1954;40:1–64. [Google Scholar]
- 28.Hungerford DA. Chromosome numbers of ten-day fetal mouse cells. J Morph. 1955;97:497–509. [Google Scholar]
- 29.Hungerford DA, DiBerardino M. Cytological effects of prefixation treatment. J BiophysBiochem Cytol. 1958;4:391–400. doi: 10.1083/jcb.4.4.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hungerford DA. Leukocytes cultured from small inocula of whole blood and the preparation of metaphase chromosomes by treatment with hypotonic KCl. Stain Technol. 1965;40:333–8. doi: 10.3109/10520296509116440. [DOI] [PubMed] [Google Scholar]
- 31.Schultz J, St. Lawrence P. A cytological basis for a map of the nucleolar chromosome in man. J Hered. 1949;40:31–8. doi: 10.1093/oxfordjournals.jhered.a105979. [DOI] [PubMed] [Google Scholar]
- 32.Moorhead PS, Nowell PC, Mellman WJ, et al. Chromosome preparations of leukocytes cultured from human peripheral blood. Exp Cell Res. 1960;20:613–6. doi: 10.1016/0014-4827(60)90138-5. [DOI] [PubMed] [Google Scholar]
- 33.Nowell P, Rowley J, Knudson AJ. Cancer genetics, cytogenetics—defining the enemy within. Nature Med. 1998;4:1107–11. doi: 10.1038/2598. [DOI] [PubMed] [Google Scholar]
- 34.Tough IM, Brown WM Court, Baikie AG, et al. Cytogenetic studies in chronic myeloid leukaemia and acute leukaemia associated with mongolism. Lancet. 1961;1:411–7. doi: 10.1016/s0140-6736(61)90001-0. [DOI] [PubMed] [Google Scholar]
- 35.Rowley JD. Identificaton of a translocation with quinacrine fluorescence in a patient with acute leukemia. Ann Genet. 1973;16:109–12. [PubMed] [Google Scholar]
- 36.Heisterkamp N, Groffen J, Stephenson JR, et al. Chromosomal localization of human cellular homologues of two viral oncogenes. Nature. 1982;299:747–9. doi: 10.1038/299747a0. [DOI] [PubMed] [Google Scholar]
- 37.de Klein A, van Kessel AG, Grosveld G, et al. A cellular oncogene is translocated to the Philadelphia chromosome in chronic myelocytic leukaemia. Nature. 1982;300:765–7. doi: 10.1038/300765a0. [DOI] [PubMed] [Google Scholar]
- 38.Heisterkamp N, Stam K, Groffen J, et al. Structural organization of the bcr gene and its role in the Ph′ translocation. Nature. 1985;315:758–61. doi: 10.1038/315758a0. [DOI] [PubMed] [Google Scholar]