Abstract
Background
Fractures of the distal radius are among the most common fractures in adults. Recently, there has been a trend towards open reduction and internal fixation of these fractures through a volar approach. The purpose of this study was to assess the early complications of volar locking plate fixation of distal radius fractures with an emphasis on defining the relationship between surgeon experience and incidence of complications.
Materials and Methods
Following IRB approval, we conducted a retrospective chart review of the initial 96 distal radius fractures (92 patients) treated by open reduction and internal fixation of distal radius fracture using a volar locked plate. Our outcome measurements were incidence of postoperative complications and radiographic loss of reduction.
Results
Twenty-two complications occurred in 21 patients. Of these, five complications (5%) required surgical treatment or hospitalization. Seventeen complications (18%) required no surgical intervention or hospitalization. Transient nerve dysfunction was the most common complication, accounting for 12 of 22 complications. The first 30 patients experienced significantly more complications than those treated later in the series (p = 0.03). There was a trend towards increased incidence of complications in cases where more than 10 days elapsed between injury and surgery or where supplementary Kirschner wire fixation was used. There was no correlation between patient age, sex, severity of fracture, or presence of ulnar styloid fracture and the development of complications or loss of reduction.
Discussion
The incidence of complications decreased significantly with increased surgeon experience, suggesting that many of these early complications are avoidable.
Keywords: Distal radius fracture, Learning curve, Surgery complications, Volar plating
Introduction
Fractures of the distal radius are among the most common fractures in adults, and their incidence continues to rise as the average age of the population increases [8, 13]. Distal radius fractures can be managed successfully with a variety of treatment methods, from closed reduction and splinting to surgical reduction and fixation. Reported complication rates of distal radius fracture treatment vary widely, from 9% to 60% [1, 8]. Although most complications are minor, such as skin irritation or scar problems, more serious complications such as infection, hardware failure, or tendon rupture do occur.
Recently, there has been a trend towards open reduction and internal fixation through a volar approach using a precontoured plate with fixed angle screws. These devices are designed to improve and maintain anatomic alignment even in patients with poor metaphyseal bone quality [9]. Initial reports of this technique by Orbay et al. reported very few complications (3–4%) [9, 10], but subsequent studies have indicated a higher complication rate. Rozental et al. reported a 22% incidence of complications following fixation using a 2.4-mm LCP volar distal radius plate (Synthes, Inc, West Chester, PA) or distal volar radius plate (DVR™; Hand Innovations LLC, Miami, FL) [12]. Arora et al. reported an overall complication rate of 27% after fixation with the LCP volar distal radius plate [13].
The risk of complications may increase whenever a surgeon uses a new technique or implant. For example, Wierks et al. reported a substantial intraoperative complication rate in their first ten patients treated by reverse total shoulder arthroplasty compared with the subsequent group of ten patients [14].Patients in their second cohort were only 10% as likely to experience an intraoperative complication than their first cohort [14]. Similarly, Laffosse et al. experienced 11 significant intraoperative complications in their first 42 minimally invasive total hip arthroplasties compared to two intraoperative complications in the following 58 cases [7]. This “learning curve” suggests that with increased experience, surgeons gain knowledge and skill that permit them to avoid pitfalls and possible complications in later cases.
The purpose of this study was to assess the early complications of volar locking plate fixation of distal radius fractures with an emphasis on defining the relationship between surgeon experience and incidence of complications.
Materials and Methods
IRB approval was obtained to perform this retrospective chart and radiographic review.
Patient Population
Medical records were searched to identify all patients treated by a single surgeon with open reduction and internal fixation of a distal radius fracture using the distal volar radius plate (DVR™; Hand Innovations LLC, Miami, FL) between 2003 and 2008. We included 96 consecutive distal radius fractures in 92 patients beginning with the surgeon’s first use of the volar plate device in 2003. Patients were excluded if they had prior treatment using another form of fixation or if the volar plate was used in conjunction with other hardware besides supplementary K-wires.
The series included 56 female and 36 male patients with a mean patient age of 48.4 years (range, 21–88 years). Thirty-one fractures involved the patients’ dominant extremity, 41 fractures were on the non-dominant side, and hand dominance was not reported in 24 patients. There were 94 closed fractures and two grade 1 open fractures. Mean time from injury to surgery was 6 days (range, 0–30 days). Mean follow-up was 12.01 weeks (range, 4–53 weeks).
Surgical Technique
We approached the volar distal radius through the flexor carpi radialis (FCR) sheath. The distal and radial insertions of the pronator quadratus were released and the muscle elevated subperiosteally to expose the fracture. After the fracture was reduced, one or two 0.062 K-wires were inserted retrograde from the radial styloid into the shaft under fluoroscopic guidance. Early in our experience in using volar plate fixation, the K-wire(s) were left in place postoperatively for 3–4 weeks in some patients with comminuted fractures. This practice was abandoned after several patients who were treated in this manner developed pin tract infections, and no K-wires were left postoperatively in the last 25 cases. Furthermore, we became more confident that the plate provided sufficient fixation that additional K-wire fixation was unnecessary. We continued to use a K-wire for provisional fixation during surgery in some cases, but removed the K-wire prior to wound closure. The remainder of the procedure followed standard technique.
Chart Review
After identifying eligible patients, a retrospective chart review was conducted. Demographic data including age, sex, hand dominance, side of injury, and tobacco use were recorded for each patient. The medical record of each return evaluation was reviewed for complications, either reported by the patient or the physician.
Radiographic Review
Fractures were classified based on preoperative radiographs using the AO classification system [6]. Initial postoperative radiographs and final postoperative radiographs were assessed for quality and maintenance of reduction. Volar tilt and ulnar variance were measured on digital lateral and posteroanterior radiographs, respectively. Loss of reduction was defined as dorsal radial tilt greater than 10°, or volar tilt greater than 20°, and ulnar variance greater than or equal to 3 mm that was not present on initial postoperative radiographs.
Statistical Analysis
Patients were grouped based on demographic factors (age and gender), treatment factors (time from injury to surgery, number in case series, presence of supplementary K-wires), and fracture characteristics (AO classification and presence of ulnar styloid fracture). The number of patients developing complications or loss of reduction was tabulated for each group. Chi-square tests were used to assess correlations between groups and development of complications. Due to the small sample size of patients experiencing loss of reduction, Fisher’s exact tests were used to assess correlations between patient variables and loss of reduction.
Results
Complications
A total of 22 complications (23%) in 21 patients were identified in the chart review. Three patients (3%) developed carpal tunnel syndrome (CTS) requiring surgical release. However, two of the three patients who underwent carpal tunnel release had nerve conduction studies consistent with bilateral carpal tunnel syndrome, and both elected to have carpal tunnel release performed on both their injured and uninjured extremities on different dates. One patient (1%) who underwent carpal tunnel release had simultaneous hardware removal.
Paresthesias or numbness occurred in nine patients (9%). Of those, four patients had symptoms of carpal tunnel syndrome, but symptoms were either transient (two patients) or mild enough to be controlled with nighttime splinting (two patients). One of the two patients treated with splinting had documented CTS prior to her injury, and she felt that her symptoms were unchanged postoperatively. Two patients (2%) had persistent thenar eminence numbness in the palmar cutaneous branch distribution. Three patients had transient superficial radial nerve dysesthesias emanating from the area of the temporary styloid K-wire.
Two patients experienced transient flexor pollicis longus (FPL) dysfunction, identified by decreased thumb interphalangeal joint flexion strength. Of the 11 patients who had supplementary K-wires left in place postoperatively, three patients developed superficial pin tract infections which were treated successfully with oral antibiotics and pin removal. One patient each had an asymptomatic but radiographically prominent screw in the radial styloid, severe finger stiffness, and a cast sore. One patient (1%) was admitted to the hospital for postoperative EKG changes. No patient experienced tendon rupture.
Patients were grouped by different demographic characteristics in an attempt to identify fracture or patient characteristics associated with complications. There was no significant difference in complication rates between males and females (p value = 0.88) or patients under age 50 and over age 50 (p value = 1.00). There was a trend towards more frequent complications in patients who underwent surgery more than 10 days after injury, but this did not reach statistical significance (p value = 0.07).
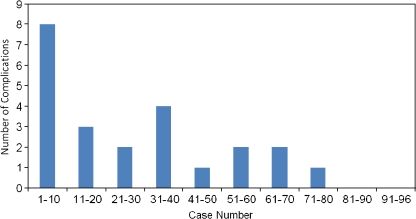
The incidence of complications decreased with increasing surgeon experience. Eight of the 22 complications occurred in the first ten cases, and 11 complications occurred in the first 30 cases (Fig. 1). The first 30 patients treated had significantly more complications (37% complication rate) than those treated later in the series (17% complication rate; p value = 0.03).
Fig. 1.
Number of complications by case number
Radiographic Outcome
Using the AO classification system [6], there were 29 type A fractures (22 A2 and seven A3), one type B fracture (B3), and 66 type C fractures (23 C1, 23 C2, and 20 C3). For statistical purposes, A and B fractures were grouped (‘less severe’) and compared with type C fractures (‘more severe’). Thirty-one patients had an ulnar styloid fracture.
On initial postoperative films, mean volar tilt was 10°, mean ulnar variance was 0.3 mm, and initial radial inclination was 20°. Final postoperative films showed minimal changes, with mean volar tilt of 9°, mean ulnar variance of 0.7 mm, and mean radial inclination of 20°. Loss of reduction was identified in six patients (6%); two wrists in the first 30 cases, two wrists in cases 31–60, and two wrists in cases 61–96. There was no significant correlation between patient age at surgery, sex, severity of fracture, or presence of ulnar styloid fracture and development of either complications or loss of reduction.
Discussion
Although initial reports by Orbay documented few complications with volar locking plate fixation of distal radius fractures [9, 10], as new surgical techniques are adopted by other surgeons and indications for surgery are expanded, more complications may be encountered. In this series of patients, our overall complication rate of 23% is comparable with some previous reports. Rozental et al. reported a 22% incidence of complications, with soft tissue irritation by hardware accounting for one-third of the said complication rate [12]. Arora et al. reported an overall complication rate of 27%, including tendon irritation or rupture in 17 patients (out of 114) [2]. Drobetz et al. described a complication rate of 17%, with FPL rupture occurring in six of the 41 patients [5].
Unlike these series, we had few patients with tendon complications; only two patients experienced transient FPL dysfunction, and no patient suffered tendon rupture. This lower incidence of tendon complications could be due to our careful avoidance of dorsal cortex screw penetration, use of the low profile Hand Innovations plate, and careful placement of the plate proximal to the watershed line. Rampoldi et al. found that all of their patients with extensor tendon ruptures had screws that penetrated the dorsal cortex [11]. Drobetz et al. believed that the multiple FPL ruptures in their series could be attributed to the sharp edges of the screws and volar plate [5]. Casaletto et al. noted that FPL ruptures were often associated with distal placement of the volar plate [4]. The absence of tendon rupture in our series could also be due to the short follow-up (mean, 12 weeks), as Drobetz et al. reported a mean time to tendon rupture of 10 months [5]. However, reports of tendon irritation have occurred as early as 1 month postoperatively [11].
We had a higher than previously reported incidence of postoperative nerve dysfunction. Median nerve dysfunction was the most common complication in our series, occurring in nine patients (9%). Median nerve symptoms can be caused by the original trauma and not related to any specific surgical technique. In their series of 236 fractures treated with a variety of methods, McKay et al. found a 22% incidence of median nerve symptoms [8]. Bienek et al. reported a 20% incidence of carpal tunnel syndrome in 60 patients with distal radius fractures treated conservatively, with a mean onset of symptoms 10 months after the injury [3].
Alternatively, median nerve-related symptoms could be attributed to traction on the nerve during the volar approach to the radius. The decreasing incidence of median nerve complaints with increased surgeon experience supports this assertion. In our series, four of the first ten cases (and six of the first 30 cases) reported some sort of median nerve dysfunction. As the surgeon becomes more comfortable with the volar plate technique, he or she likely requires less aggressive and less prolonged retraction on the FCR and adjacent median nerve, resulting in fewer median nerve complaints.
K-wires used for provisional and supplementary fixation can be a source of complications. In some patients, the radial styloid K-wire was retained postoperatively for supplementary fixation. Three of these 11 patients developed pin tract infections. We have since abandoned this practice. In addition, three patients, in whom K-wires were used only intraoperatively, reported superficial radial nerve irritation. In these patients, multiple attempts at K-wire placement during fracture reduction were likely responsible for the superficial radial nerve irritation.
No significant correlation was found between the incidence of complications and gender, presence of ulnar styloid fracture, or fracture type. However, there was a correlation between surgeon experience and complication rate. The last 66 patients treated had significantly fewer complications than the first 30 patients, which likely represents the surgeon’s learning curve in applying this new technology. Specifically, excessive traction on the median nerve and multiple attempts at K-wire placement contributed to clinical complications. The decreasing incidence of these early postoperative complaints supports the assertion that they can be avoided with careful attention to surgical technique.
One limitation of this study is the short follow-up, with a mean time of 12 weeks. Some complications, such as tendon rupture, may occur later. The retrospective nature of this study and the lack of patient reported outcomes also influence the complications identified. Previous work by McKay et al. has illustrated that patients may report different complications than those reported by their surgeons [14]. Thus, relying on the medical record for complication information may exclude some complications experienced by the patient, but not recognized or reported by the clinician.
As with the adoption of any new technology, the surgeon must be aware of the complications that may occur with volar plate fixation of distal radius fractures. Reported complications include tendonitis, tendon rupture, and nerve dysfunction. In our study, the complication rate decreased with increasing surgeon experience, suggesting that many of these complications can be averted. Specifically, avoiding prolonged or aggressive traction on the median nerve may decrease postoperative neuropraxias. Supplemental K-wires should be avoided if possible. Attention to these early complications allowed us to adjust our practice to avoid similar problems in later cases.
Disclosure
No industry or governmental agencies provided funding support for this study.
Footnotes
The device used in this study (Hand Innovations DVR volar distal radius plate, Depuy Orthopaedics, Warsaw, IN) is FDA-approved for use as described in this study.
References
- 1.Al-Rashid M, Theivendran K, Craigen MAC. Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radial fractures. J Bone Joint Surg. 2006;88B:1610–1612. doi: 10.1302/0301-620X.88B12.17696. [DOI] [PubMed] [Google Scholar]
- 2.Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316–322. doi: 10.1097/BOT.0b013e318059b993. [DOI] [PubMed] [Google Scholar]
- 3.Bienek T, Kusz D, Cielinski L. Peripheral nerve compression neuropathy after fractures of the distal radius. J Hand Surg Br. 2006;31:256–260. doi: 10.1016/j.jhsb.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 4.Casaletto JA, Machin D, Leung R, Brown DJ. Flexor pollicis longus tendon ruptures after palmar plate fixation of fractures of the distal radius. J Hand Surg Eur. 2009;34:471–474. doi: 10.1177/1753193408100964. [DOI] [PubMed] [Google Scholar]
- 5.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27:1–6. doi: 10.1007/s00264-002-0393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma. 2006; 10 (Suppl 1:v–ix): 1–154. [PubMed]
- 7.Laffosse JM, Chiron P, Accadbled F, Molinier F, Tricoire JL, Puget J. Learning curve for a modified Watson-Jones minimally invasive approach in primary total hip replacement: analysis of complications and early results versus the standard-incision posterior approach. Acta Orthop Belg. 2006;72:693–701. [PubMed] [Google Scholar]
- 8.McKay SD, MacDermid JC, Roth JH, Richards RS. Assessment of complications of distal radius fractures and development of a complication checklist. J Hand Surg. 2001;26A:916–922. doi: 10.1053/jhsu.2001.26662. [DOI] [PubMed] [Google Scholar]
- 9.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg. 2002;27A:205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 10.Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg. 2004;29A:96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 11.Rampoldi M, Marsico S. Complications of volar plating of distal radius fractures. Acta Orthop Belg. 2007;73:714–719. [PubMed] [Google Scholar]
- 12.Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced unstable fractures of the distal radius. J Hand Surg. 2006;31A:359–365. doi: 10.1016/j.jhsa.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 13.Vasenius J. Operative treatment of distal radius fractures. Scand J Surg. 2008;97:290–296. doi: 10.1177/145749690809700403. [DOI] [PubMed] [Google Scholar]
- 14.Wierks C, Skolasky RL, Ji JH, McFarland EG. Reverse total shoulder replacement: intraoperative and early postoperative complications. Clin Orthop Relat Res. 2009;467:225–234. doi: 10.1007/s11999-008-0406-1. [DOI] [PMC free article] [PubMed] [Google Scholar]