Abstract
Purpose of the study: To assess the recruitment, adherence, and retention of urban elderly, predominantly African Americans to a falls reduction exercise program. Design and methods: The randomized controlled trial was designed as an intervention development pilot study. The goal was to develop a culturally sensitive intervention for elderly persons who suffered a fall and visited an emergency department (ED). Participants were taught exercises during 4 on-site group classes and encouraged to continue exercising at home for 12 weeks and attend additional on-site monthly classes. The protocol included a specifically designed intervention for increasing retention through trained community interventionists drawn from the participants’ neighborhoods. Results: The screening of 1,521 ED records after falling yielded the recruitment of 204 patients aged 65 years and older. Half were randomized into the falls prevention program. Of the 102 people in the intervention group, 92 completed the final 6-month assessment, 68 attended all on-site sessions, but only 1 reported exercising at home all 12 weeks. Those who lived alone were more likely (p = .03) and those with symptoms of depression were less likely (p = .05) to attend all on-site exercise classes. The final recruitment rate was estimated as 31.8%. The final retention rates were 90.2% and 87.3% for the intervention and control groups, respectively. Implications: Recruitment of frail elderly African American patients is resource intensive. Adherence to the on-site exercise classes was better than to the home-based component of the program. These findings have implications for the design of future community-based exercise programs and trials.
Keywords: African American, Aged, Clinical protocols, Accidental falls, Depression, Social supports, Compliance
Historically, minority populations in the United States have been underrepresented among participants in clinical research (Lai et al., 2006; Pinsky et al., 2008). Factors such as lack of information, education, lifestyle, and mistrust of clinical trials have been identified as some of the barriers in achieving proportional levels of minority enrollment, especially among African Americans (BeLue, Taylor-Richardson, Lin, Rivera, & Grandison, 2006; Phipps et al., 2004; Wilbur et al., 2006; Yancey et al., 2001). Underrepresentation of minorities needs to be addressed as successful recruitment, and retention of members of different cultures is necessary to enhance generalizability of findings (Robinson & Trochim, 2007) One conceptual model recognizes awareness and opportunities to participate and to accept or refuse to participate in clinical trials as important factors that influence recruitment of underrepresented minorities (Ford et al., 2008). Although underrepresented minorities are often interested in participating in research, culturally appropriate contact methods and educational materials need to be developed to reach this population. Finally, there is need to improve quality and quantity of studies on the recruitment and retention of underrepresented populations.
Falls are a major risk factor for hip fracture and subsequent nursing home placement among persons aged 65 years and older (Grisso et al., 1991; Nevitt, Cummings, Kidd, & Black, 1989; Sattin et al., 1990; Tinetti, Speechley, & Ginter, 1988; Tinetti & Williams, 1997). Here, we report recruitment, adherence, and retention data from the Exercise and Training in Aging (EXTRA) protocol development study that applied mixed methods (National Institutes of Health Office of Behavioral and Social Science Research, 1997) to design a culturally appropriate intervention for elderly, largely African American urban residents who suffered a fall of sufficient severity to incur an emergency department (ED) visit. The EXTRA protocol design targeted two elements. The first element was an intervention to reduce the risk of falls. The second element was an intervention to increase adherence and retention that was tailored to the socioeconomic, cultural, and ethnic characteristics of the target community. The EXTRA falls risk reduction intervention was based, in part, on the successful exercise programs applied by Tinetti and colleagues (1994) in the FICSIT studies. The exercise program included on-site group exercise classes and an at-home component.
There is growing movement toward recognizing the importance of applying techniques such as Community-Based Participatory Research (CBPR) that by partnering with local communities can enhance the ecological validity and effectiveness of behavioral-based trials aimed at reducing health disparities (Bogart & Uyeda, 2009; Viswanathan et al., 2004). The adherence intervention for EXTRA applied CBPR principles to gain a more accurate understanding of community circumstances, increase mutual trust, and enhance knowledge from local community through focus groups (described later; Viswanathan et al., 2004). Although the exercise component was modeled after the Fraility and Injuries: Cooperative Studies of Intervention Techniques (FICIT) trials, it was adapted in accordance with information obtained from the local African American community (Lavizzo-Mourey et al., 2001). Also, the program was carried out in partnership with community interventionists drawn from the communities in which the participants lived who provided peer support to the participants and were involved in carrying out all aspects of the protocol.
The objectives of this article are to describe the recruitment and retention of elderly people with sufficiently severe falls to have visited inner-city EDs, contrast adherence to the on-site and at-home components of the exercise program, and identify factors that appear to affect adherence to that program. Because we expected that elements from the physical as well as social environments could be either barriers or facilitators to exercise, we selected a biopsycho-ecological framework to conceptualize variable domains for explaining adherence (Stineman, 2001). The biopsycho-ecological framework expands on the biopsychosocial model to include the natural and man-made environments along with sociocultural variables, physical health, and mental well-being as motivating health-related behaviors (Stineman & Streim, 2010), There is growing recognition of the importance of ecological factors along with individual level characteristics when developing and studying participants’ responses to multilevel interventions (Bogart & Uyeda, 2009). Ecological factors are expected to drive overall retention and adherence particularly to programs that depend on voluntary participation among populations likely to experience disparities. Ease of access as determined by the person's functional or health status along with the physical and cultural environments presumably shapes internal motivations influencing adherence to interventions.
We hypothesized that it would be feasible to recruit and retain the population through the development of a culturally appropriate protocol with the continued involvement of community interventionists. Based on early information from focus groups drawn from the local community about exercise preferences, we expected that adherence would be lower for the at-home than for the on-site component of the program (Lavizzo-Mourey et al., 2001). We also hypothesized that determinants of adherence would be multifactorial. We anticipated that older persons with less education, reduced physical and mental well-being, and lower general health status would be less likely to adhere, and those living alone would be more likely to put forth effort to attend the on-site exercise classes based on desire and need for socialization.
Design and Methods
This study was approved by the Institutional Review Board at the University of Pennsylvania in Philadelphia, Pennsylvania.
Local Community Involvement
Five focus groups were convened from the local urban African American community prior to completing the development of the EXTRA protocol design. This grass roots effort included 38 elderly people recruited from an urban senior center, social group, day program, and a church. Their contributions were valuable, providing insights about local contexts, effective recruitment and retention strategies, and optimal approaches to the development of the exercise component of the EXTRA protocol. Details regarding the focus group methods are described in detail elsewhere (Lavizzo-Mourey et al., 2001). Themes from the discussions were identified to uncover attitudes and beliefs about barriers and facilitators of exercise that could inform protocol development (Freedman, 1998; Harris, 1992; Lavizzo-Mourey et al., 2001).
Results from the focus groups indicated that older persons exercised infrequently and often believed that carrying out routine activities of daily living constituted adequate exercise. Although interest in greater levels of activity was widespread, opportunities for planned exercise were rarely available. Participants stated that they would prefer group program exercise classes or dancing to exercising privately at home. They noted opportunities for mutual stimulation, inspiration, and improved personal motivation. They believed that frequently recommended options such as walking outdoors were not feasible because of concerns about safety when walking in the environments of their low-income urban neighborhoods.
Themes that emerged about the importance of social and community supports to continued involvement in exercise were applied in both the adherence intervention design and the exercise component of the EXTRA protocol (detailed later). Specifically, we (a) developed on-site exercise classes intended to encourage and complement the at-home exercise program, (b) developed endurance and balance exercises that could be done indoors and abandoned the outdoor walking program originally planned, (c) established telephone support and hired community interventionists drawn from the same community as the participants to offer personal support and encouragement and facilitate all aspects of the program, and (d) optimized opportunities for socialization among participants through on-site group exercise and personalized ongoing involvement with the community interventionists.
Recruitment and Enrollment Procedures for the EXTRA Program
People aged 65 years and older who did not reside in a nursing home and visited one of three urban EDs (Hospital of the University of Pennsylvania, Presbyterian Medical Center of Philadelphia, and Misericordia Hospital Division of Mercy Catholic Medical Center) because of a fall were eligible for inclusion. Exclusion criteria were severe neurologic, rheumatologic, or orthopedic disorders, inability to walk across a room (even with an assistive device), severe cardiopulmonary disease, need for hemodialysis, inability to travel by taxi to the clinical testing site, or cognitive impairment as defined by a Folstein Mini-Mental State Examination (MMSE) score of less than 17 (Folstein, Folstein, & McHugh, 1975).
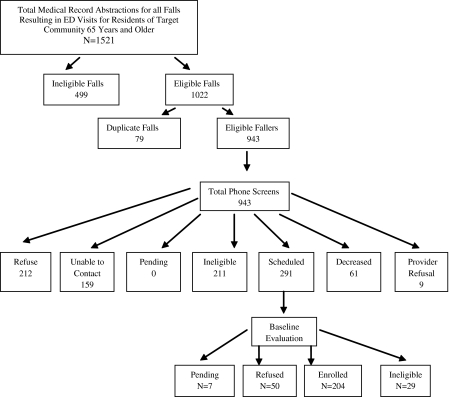
Recruitment procedures began with the initial screening and abstraction of all ED medical records for people aged 65 years and older who sought care for a fall (Figure 1). Next, letters were sent, and phone calls were made to all eligible patients. If a person was hesitant or wanted to postpone participation, a different staff member followed up later. Also, several different staff members left messages on patients’ answering machines in case certain patients responded better to different voices. The patient was not categorized as “unable to contact” until the following criteria were met: (a) Participants had been called at least six times with attempts being made at different days and times during the week, (b) medical record abstraction contained no phone number or emergency contact number, or (c) participant's phone was disconnected for at least three months. Home visits were attempted for those who could not be reached by phone, but this strategy was abandoned as it was not effective. Follow-up letters were sent on attractive stationary to increase the chance of their being read.
Figure 1.
Participant recruitment and enrollment.
For persons who were eligible after the phone screen and willing to participate, the primary care providers were contacted to ask if their patient was medically able to participate. Those cleared by their providers were invited for an on-site evaluation. Registered nurses, a physical therapist, and a physician who were not involved in administering the protocol performed the on-site baseline history, physical examination, and testing and made final eligibility determinations. Patients still eligible after the evaluation provided voluntary informed consent and were randomized into a control and experimental group. The control group underwent the same evaluations as the group receiving the exercise program. They were only provided a generic pamphlet that discussed the benefits of walking three times a week for 30 min a day.
Intervention
The exercise program focused on endurance, resistance, and balance training over a four-month period, with a final evaluation at six months. The intervention included frequent personalized feedback and counseling to increase knowledge about exercise and risk of falling, setting of realistic exercise goals, group support, providing exercise equipment for use in the home, distribution of written and audio-taped instructional materials, an exercise log, and regularly supervised exercise sessions. Each exercise was graded so that the strenuousness of the participant's efforts could be increased or decreased in intensity over time depending on his or her tolerance.
The completed protocol included intertwined on-site group exercise training classes (Tinetti et al., 1993) and at-home exercise components. In addition, a registered nurse used a list generated by the study physicians to determine if the participant was taking any medications that could increase risk of falls. A letter was sent to the participants’ primary care provider with recommendations for any pharmacological adjustments. Also, a home assessment was carried out by an occupational therapist and the community interventionist. The purpose of the home visit was to perform a safety check and advise the participant on ways to reduce home environmental hazards and other factors known to contribute to risk of falls. Participant characteristics were determined at baseline prior to beginning the protocol, at three months, and at six months after randomization. A description of the exercise program follows.
Month 1: On-Site Exercise Classes.—
During the first month, participants attended four weekly on-site classes. Participants were taught how to do the 19 exercises focused on fitness, balance, strength, and flexibility. Each class consisted of six to eight persons. Classes and testing were held in a large room within a geriatric wellness program with an exercise leader, a registered nurse, an occupational therapist, and two or three community interventionists. As the exercises were taught to the participants, clinicians monitored them for tolerance and safety in order to determine the right grade of exercise difficulty on an individual basis. At the end of the first month, participants were provided with written instructions and a walkman with recorded instructions for each exercise to be continued at home. Initially, participants were taught the least intensive version of each exercise.
Months 2, 3, and 4: On-Site and At-Home Exercises.—
Participants visited the on-site location one time each month so that their tolerance and progress could be monitored and to assess whether or not they were ready for more strenuous grades of exercise. Participants were asked to exercise three times a week at home, and a community interventionist visited or called once a week to offer encouragement and determine if the home exercise was occurring. Goals for exercise were modified by the community interventionist in collaboration with the occupational therapist and other clinicians involved in the study in order to challenge the participants to perform at optimal levels without the program being so difficult as to discourage adherence at home or cause possible danger.
The Adherence and Retention Intervention
Ongoing community involvement was sought through nonprofessional but trained community interventionists recruited from the participants’ neighborhoods in efforts to tailor the intervention to the participants. The community interventionists served as the participants’ primary contact and were involved in carrying out the study. They attended all on-site classes, learned the exercises, served as coaches for the participants through both components of the exercise program, and helped in setting individual exercise goals. The community interventionists attended a home safety visit with an occupational therapist to identify barriers in the home that could enhance risk of falling, determine need for assistive technology, etc. They scheduled all on-site exercise classes, reminded participants to attend, and facilitated transportation to the center through taxi vouchers. To enhance adherence to the home program, the community interventionists made weekly phone calls to encourage the participants and remind them to complete their exercise calendars.
At least one home visit by the community interventionist took place each month. During these monthly home visits, the community interventionists followed through on suggestions made about safety during the home visits, helped participants remove hazards, and identified and called their clinician providers to obtain needed safety equipment or devices, such as hearing aids. The community interventionists helped identify a safe place at home to exercise and discussed any problems affecting the participant's ability to exercise. They performed the exercises with the participants in their homes and notified the project manager (a registered nurse) if the participant had problems doing the exercises.
Based on concerns expressed in the focus groups by elderly African Americans, the research team anticipated challenges associated with adherence and retention, particularly to the at-home component of the exercise program. The duration of on-site exercise classes was extended in an effort to reinforce the participants’ motivation for home exercise and encourage adherence and retention. Opportunities for socialization were built into the seven on-site group exercise classes, which included meals and individual counseling about exercise. Phone support and ongoing interactions with the community interventionists were built into the protocol to enhance socialization and adherence to the home-based program.
The community interventionists kept records of all home visits and phone calls and provided information to and sought guidance as needed from clinician members of the research team. Written and taped instructions, home exercise equipment, and t-shirts were provided to the participants to increase morale. The original protocol design called for a 6-month exercise program. Because of recruitment difficulties, high costs of the retention intervention, and the challenge of securing safe transportation for these frail participants from their homes to the exercise classes, it was financially necessary to reduce the length of the exercise program to four months from six.
Baseline Measures
The baseline measures were organized by the biopsycho-ecological framework into domains approximating sociocultural or environmental life contexts and those expressing health and well-being. Sociocultural or environmental variables included age, gender, education, marital status, race, living arrangement (home, apartment/town house/condo, and other), and lives alone versus lives with others.
Health and well-being was further divided into physical and mental health status. Physical health status was evaluated by the body mass index (BMI), blood pressure, the number of comorbidities, and the completion of the Medical Outcomes Study Short Form Health Survey (MOS SF-36). The 6-min walk test (Harada, Chiu, & Stewart, 1999) was conducted in the geriatric wellness center hallway covered with industrial carpeting. The hallway provided a straight path of 100 feet and was marked at every 10 feet. Higher scores indicate a greater distance (converted to meters) walked in 6 min. As reference, the mean for healthy adult men and women who were on average 60 and 62 years of age was 576 and 494 m, respectively (Enright & Sherrill, 1998). The MOS-SF-36 was selected as one of the most widely used measures of the impact of health on functioning. Four of the eight available subscales of the MOS-SF-36 item short form health survey were selected as most relevant to physical function, balance, and walking. These included the physical function scale, which contains 10 items and 21 levels; the role limitation due to physical problems scale with 4 items and 5 levels; the body pain scale, which contains 3 items and 11 levels; and the general health perceptions scale, which has 5 items and 21 levels. Higher scores indicated greater function (Brazier et al., 1992; McHorney, Ware, Rogers, Raczek, & Lu, 1992; Ware, 1993). Mental status was addressed through the 15-item Geriatric Depression Scale (GDS), where a higher value indicates greater depressive symptoms (Friedman, Heisel, & Delavan, 2005) and by the Folstein MMSE score, where a lower value indicates poorer cognitive functioning (Folstein et al., 1975). Finally, we included the number of psychotropic medications and the number of medications overall.
Recruitment and Enrollment
Recruitment and enrollment was addressed descriptively according to three phases. These phases included the total number of ED records screened, the yield from phone screens, and the final recruitment through in-person baseline evaluations. Refusals relative to total numbers of eligible participants were determined at the second and third phases, that is, the point of phone screening for eligibility and the point of enrollment and randomization following baseline evaluation. Enrollment was calculated as the proportion of eligible participants who could be recruited at each of these phases. Overall, final recruitment was calculated as the number of people agreeing to be randomized (numerator) divided by the number of all eligible fallers minus those who were ineligible or deceased (denominator).
Definition of Adherence for the On-Site Exercise Class Component
Adherence represents a subcomponent of retention intended to address the degree to which the participants actively took part in each detailed component of the exercise program. A variable was created that counted the number and determined the proportion of on-site exercise sessions that the participant attended out of a potential of seven sessions in total. This was also reported as the distribution according to the percentage of total sessions available. High adherence to the on-site exercise component was defined as attendance at all 7 on-site exercise programs.
Definition of Adherence for the At-Home Exercise Component
We determined adherence to the at-home portion of the intervention separately from the on-site portion. A variable was created that counted the number of weeks that the participant reported exercising three or more days that week (from diaries) and reports to the community interventionists. This was also reported as the distribution according to the percentage of weeks with reported exercise of the twelve possible weeks. High adherence to the at-home exercise component was defined as exercising at least three days every week for the 12 weeks.
Overall Retention
Overall retention refers to the ability of the team to retain participants in the trial for six months, comparing the intervention and control populations. Completion of the six-month final evaluation was considered the trial end. A variable was created that counted the number and determined the proportion of persons recruited who remained in the intervention and control groups.
Analysis
The intervention and control groups were described and contrasted. Variables believed to potentially influence adherence were divided into those influencing intrinsic mental and physical health status and those relating to the physical or sociocultural environments. We used t test and chi-square tests to compare sociodemographic and clinical variables between the intervention and control groups. A multivariable model was estimated to identify factors that independently predicted high adherence to the on-site program. To identify the baseline factors independently associated with adherence, we estimated logistic regression models to study the effects of candidate covariates listed in Tables 1 and 2. Using a block set approach, we estimated our model by adding sets of variables organized according to the biopsycho-ecological model. After the addition of each block, we only kept those variables that were statistically significant from the previous block. We used p < .10 as significant because the study was a pilot program, and with the small sample sizes, we were concerned about minimizing Type 2 errors to avoid being too conservative and hence missing important exploratory findings (Michels & Rosner, 1996). The first block set included age, gender, race, and education. The second added other social variables, including marital status, living arrangement, and live alone. The third added the physical functions and general health beginning with the SF-36 dimensions, followed by BMI, blood pressure, number of comorbidities, the 6-min walk test, and number of medications. The fourth block set added mental characteristics, including the GDS, the MMSE, and the number of psychotropic medications. The final model included only variables with p values lower than .10.
Table 1.
Baseline Sociocultural Circumstances and Physical Living Environment (n = 204)
| Intervention group (n = 102) | Control group (n = 102) | p value | |
| Age in years, mean (SD) | 76.52 (8.0) | 75.59 (6.7) | .37 |
| Gender (%) | |||
| Male | 19 (18.6) | 33 (32.4) | .02 |
| Female | 83 (81.4) | 69 (67.7) | |
| Race (%) | |||
| African American | 90 (88.2) | 91 (89.2) | .82 |
| White or other | 12 (11.8) | 11 (10.8) | |
| Education (%) | |||
| ≤Grade 9 | 29 (28.4) | 20 (19.6) | .43 |
| Some high school | 23 (22.6) | 30 (29.4) | |
| High school graduate | 26 (25.5) | 25 (24.5) | |
| Post high school | 24 (23.5) | 27 (26.5) | |
| Marital status (married %) | |||
| No | 71 (69.6) | 70 (69.3) | .96 |
| Yes | 31 (30.4) | 31 (30.7) | |
| Living arrangement (%) | |||
| House | 79 (77.5) | 79 (78.2) | .77 |
| Apartment/townhouse/condo/other | 18 (17.7) | 19 (18.8) | |
| Other | 5 (4.9) | 3 (3.0) | |
| Do you live alone? (%) | |||
| No | 52 (51.0) | 51 (50.0) | .89 |
| Yes | 50 (49.0) | 51 (50.0) | |
Table 2.
Baseline Comparisons General Physical and Mental Health (n = 204)
| Intervention group (n = 102) | Control group (n = 102) | p value | |
| Mean (SD) | Mean (SD) | ||
| Body mass index | 26.85 (5.0) | 27.86 (6.5) | .21 |
| Blood pressure | |||
| Systolic | 135.03 (22.7) | 132.99 (19.9) | .50 |
| Diastolic | 74.43 (12.0) | 74.67 (12.1) | .89 |
| Number of comorbidities | 1.27 (0.9) | 1.31 (0.8) | .74 |
| 6-min walk test | 251.09 (109.2) | 236.00 (113.1) | .33 |
| General Health Status-Short Form-36 | |||
| Physical function | 54.22 (24.1) | 50.15 (28.1) | .27 |
| Role physical | 47.06 (39.1) | 40.44 (41.8) | .24 |
| Bodily pain | 58.81 (29.6) | 57.32 (27.3) | .71 |
| General health | 59.87 (21.3) | 58.05 (20.3) | .53 |
| Depression (Geriatric Depression Scale) mood | 2.66 (2.7) | 3.11 (2.9) | .26 |
| Mini-Mental State Examination score | 26.86 (2.8) | 26.97 (2.4) | .77 |
| Number of psychotropic medications | 0.22 (0.4) | 0.24 (0.5) | .77 |
| Number of medications | 4.98 (2.8) | 5.47 (3.1) | .25 |
Results
Participant Recruitment
There were 1,521 persons aged 65 years and older residing in the target community whose records were screened at local urban EDs. Of these, 943 had eligible falls and an attempt was made to reach them for phone screening (Figure 1). Of the 943 persons telephoned, 159 could not be contacted, 61 had died, and 211 were ineligible. Of the remaining 512 eligible persons, 291 were scheduled for an on-site baseline assessment, 212 refused, and 9 had primary care providers who refused patient access. Excluding those whose doctors refused access, 57.9% of the eligible persons who could be reached agreed to participate (291 of 503).
Of the 291 persons scheduled for the baseline assessment, 204 persons were enrolled. An additional 50 participants who had originally consented refused baseline evaluation, 7 failed to keep their appointments (pending at the time that recruitment ended), and 29 were found medically ineligible during baseline evaluation. Excluding those who were found ineligible, 77.9% of persons who agreed to the baseline evaluation were willing to be randomized (204 of 262). The final recruitment rate was estimated as 31.8% (204 of 662).
Tables 1 and 2 characterize the control and intervention groups. The average age of the entire sample was more than 75 years. Most participants (88.7%) were African American, female (74.5%), and not married (69.1%). Approximately half lived alone. The only statistically significant difference between the control and intervention groups was gender. The intervention group included a higher proportion of women compared with the control group.
Adherence to the On-Site and At-Home Components
There were 92 individuals who completed the four-month exercise program and were evaluated at the six-month protocol end point. Of the 10 individuals who dropped out of the program, 9 dropped out before attending any on-site exercise programs and a single individual dropped out before beginning the at-home exercise program component.
There were seven opportunities for participation in the on-site group programs. There were 81 of 93 participants (87.1%) who attended at least four or just over half of all available classes and 74 participants (79.6%) who attended at least 6 of the 7 available classes. There were 68 of 93 participants (73.1%) with complete adherence data who attended all 7 on-site exercise classes. These 68 persons formed the high and the remaining 25 constituted the low adherent group. That single person was included as among the other 92 participants in the on-site portion of the program.
Adherence to the At-Home Component
The goal of the at-home program was for the participant to perform the exercises at the same number of repetitions and grade as established through monitoring during the on-site group program. There were 12 opportunities for participants to participate in the at-home program. There were 68 (78.2%) persons who reported exercising just over half (7) of the twelve weeks. Only a single person (1 of 87 with complete data or 1.2%) reported exercising at home all twelve weeks at least three days a week and thus was classified as high adherent.
Factors Associated With Adherence to the On-Site Exercise Classes
Table 3 displays comparisons between those who were adherent versus not adherent. When looking at the unadjusted comparisons, advanced age, non-African American status, male gender, graduating from high school or higher education, living alone, and better health (across the domains of the SF-36) were associated with higher adherence to the on-site exercise program. Greater adherence to the on-site exercise program was also associated with a lower BMI (less obesity), fewer comorbid medical conditions, fewer medications overall, greater physical function, higher physical role function, better perceived general health, and further distance walked on the initial 6-min walk test. Moreover, those who adhered were, on average, less depressed, took fewer psychometric medications, and had higher MMSE scores.
Table 3.
Factors Associated With Adherence to the On-Site Component of the Exercise Program
| Variable | Univariate comparison of high vs. low adherence, Means/proportions |
Adjusted associations OR (95% CI) | |
| Adherent | Nonadherent | ||
| Age (mean ± SD) | 76.8 ± 7.9 | 74.2 ± 7.4 | |
| Gender | |||
| Male | 13 (19.1) | 4 (16.0) | |
| Female | 55 (80.9) | 21 (84.0) | |
| Race | |||
| African American | 59 (86.8) | 24 (96.0) | |
| White and other | 9 (13.2) | 1 (4.0) | |
| Education, n (%) | |||
| ≤ Grade 9 | 17 (25.0) | 8 (32.0) | |
| Some high school | 15 (22.1) | 7 (28.0) | |
| High school graduate | 18 (26.5) | 5 (20.0) | |
| Post high school | 18 (26.5) | 5 (20.0) | |
| Marital status (married) | 20 (29.4) | 7 (28.0) | |
| Married | 20 (29.4) | 7 (28.0) | |
| Not married | 48 (70.6) | 18(72.0) | |
| Living arrangement, n (%) | |||
| House | 49 (72.1) | 22 (88.0) | |
| Apartment/townhouse/condo or other | 19 (27.9) | 3 (12.0) | |
| Do you live alonea | |||
| Yes | 39 (57.4) | 8 (32.0) | 3.0 (1.1–8.1), p = .03 |
| No | 29 (42.6) | 17 (68.0) | |
| Body mass index (mean ± SD) | 26.5 ± 4.8 | 28.6 ± 5.5 | |
| Blood pressure at baseline (mean ± SD) | |||
| Systolic | 133.7 (25.1) | 141.6 (39.4) | |
| Diastolic | 74.8 (14.6) | 75.9 (14.7) | |
| Number of comorbidities (mean ± SD) | 1.2 ± 1.1 | 1.6 ± 1.2 | |
| Six-min walk test (mean ± SD) | 258.6 ± 129.4 | 240.0 ± 156.1 | |
| General Health Status-Short Form-36 (mean ± SD) | |||
| Physical function | 56.8 ± 28.2 | 48.2 ± 34.8 | |
| Role physical | 52.6 ± 47.1 | 38.0 ± 49.3 | |
| Bodily pain | 62.6 ± 35.3 | 51.6 ± 39.5 | |
| General health | 61.9 ± 25.0 | 56.3 ± 28.8 | |
| Depressed mood (mean ± SD)a | 2.3 ± 2.4 | 3.6 ± 3.6 | 0.85 (0.72–1.0) p = .05 |
| Mini-Mental State Examination score (mean ± SD) | 27.1 ± 3.2 | 26.4 ± 3.9 | |
| Psychotropic medication (mean ± SD) | 0.2 ± 0.5 | 0.2 ± 0.6 | |
| Number of medications (mean ± SD) | 4.8 ± 3.5 | 5.52 ± 3.2 | |
Note: aDepressed mood and living alone (no = referent) remained statistically significant at p ≤ .05 in the final block set approach logistic regression model. OR = odds ratio; CI = confidence interval.
The final adjusted model included only two statistically significant variables. Living alone status (odds ratio [OR] = 3.0, 95% confidence interval [CI] = 1.1, 8.1; p = .03) was associated with increased adherence, and the presence of depressed mood was associated with decreased adherence rates (OR = 0.85, 95% CI = 0.72, 1.0; p = .05) The number of variables included in the final model met the standard for logistic regression where approximately 10 observations are necessary in the smaller group (in this case, the lower adherents N = 25) per independent variable (Concato, Feinstein, & Holford, 1993). Factors associated with adherence for the at-home component of the exercise program were not studied because adherence was so low.
Retention
Enrolled participants were randomized to intervention (N = 102) and control (N = 102) groups. Seven participants dropped out because of illness, four died, one moved, and one refused the final evaluation. Of the 102 participants randomized to the intervention group, 92 completed the six-month evaluation, 3 dropped out due to illness, 4 died, and 3 refused the final evaluation. Of the 102 participants randomized to the control group, 89 completed the final six-month evaluation for the study. Thus, overall participant retention for the intervention group was 90.2% and 87.3% for the control group.
Discussion
It was possible to recruit and retain this largely African American urban population through the development of a culturally appropriate protocol, but the process was challenging and resource intensive. As hypothesized, adherence was far better for the on-site than for the home-based exercise component. Indeed, the recruitment, adherence, and retention of elderly African American persons seen in EDs in an urban setting following a fall proved difficult and incurred considerable economic and manpower costs.
Studies have documented that targeting individuals at greatest risk of falling and suggesting the use of falls prevention clinics would be clinically important, even if there was a small reduction in fall rates (Moore et al., 2010). Individuals with frequent history of falls who have not suffered major trauma may have a particularly good potential for injury prevention and improved functional status. Yet, our findings highlight the challenges of recruiting such individuals. Overall, recruitment was estimated at only 31.8%. Although differences in selection criteria and study design make direct comparisons of EXTRA recruitment with other studies difficult, 31.8% is below the published range of 38%–96% for recruitment in falls prevention trials targeted to the general elderly population (Bean et al., 2004; Li et al., 2005; Mahoney et al., 2007; Means, Rodell, & O’Sullivan, 2005; Nowalk, Prendergast, Bayles, D’Amico, & Colvin, 2001; Shumway-Cook et al., 2007). Even this modest recruitment required tremendous effort at great expense. It was hampered by difficulties contacting potential participants, obtaining physician clearance, and the various logistic challenges, such as difficulties in transportation inherent in working with this frail population. Consistent with strategies applied in our study, the provision of transportation, engineering of community partnerships, and applications of CBPR approaches have shown to lead to dramatic increases in the numbers of ethnic minorities enrolled and retained in a variety of protocols (Horowitz, Brenner, Lachapelle, Amara, & Arniella, 2009; Paskett et al., 2008; Rugkasa & Canvin, 2010). The greater resources required to successfully target and retain this urban population could have implications to the financial support and design of future studies addressing minority recruitment. In one trial of a physical activity intervention, the cost of recruitment was estimated at $449 per randomized participant (Katula et al., 2007). Once recruited, most participants were retained until the final six-month evaluation, with only three from the intervention group and one from the control group refusing the final evaluation.
Consistent with the biopsycho-ecological framework, the determinants of adherence appeared multifactorial and dependent on the environment. Adherence to the three days a week exercise regimen as specified by the home-based component was so limited that we did not study factors that appeared to explain it beyond describing it. As adherence to on-site group exercise classes was much higher, we were able to evaluate factors associated with adherence to this component of the program. Living alone appeared to strongly motivate attendance. People who lived alone had a threefold increased likelihood of fully adhering to the on-site exercise classes compared with those who lived with others. Conversely, reduced mental well-being (as measured by the GDS) was statistically significantly associated with reduced adherence. Interestingly, reduced mental well-being appeared to present a greater barrier to involvement than reduced physical well-being as captured across numerous objective and subjective variables. The strong tendency of those who lived alone to participate reinforces the importance of socialization within this community. The statistically significant association after adjustment between depressed mood as well as unadjusted trends supporting associations of lower education, greater physical illness, and lower mental and cognitive functioning with reduced adherence suggest that people most in need of structured exercise opportunities are least able to attend them. In contrast to our hypothesis, advanced age was not associated with lower adherence with the on-site program. This indicates that advanced age alone is not a barrier to participation. Similarly, although people who were African American appeared less likely to adhere before statistical adjustment, there were no statistically significant differences after adjustment. This suggests that apparent differences in adherence associated with African American status may relate to differences in the population other than race.
Adherence to various types of exercise programs among persons drawn from the general elderly population has been shown to range from 36% to 100% for class-based and from 36% to 93% for home-based programs (Flegal, Kishiyama, Zajdel, Haas, & Oken, 2007; Hauer et al., 2001; van der Bij, Laurant, & Wensing, 2002). Thus, in EXTRA, although adherence to the group on-site exercise classes was well within the expected range (73.1%), adherence was far below expectation for the at-home component (1.2%). Although lower adherence to the at-home component was anticipated, the magnitude of difference in this study was greater than we expected (Lavizzo-Mourey et al., 2001).
In concordance with findings from our preliminary focus groups, a study of African Americans of all ages noted need for a buddy or partner to motivate physical exercise. Similarly, health problems and fatigue as well as dogs, neighborhood crime, lack of light, and cars driving too close to the curb were all cited as personal and physical environmental barriers to exercise (Bopp et al., 2007). Qualitative evidence from focus groups from both this and our studies about the perceived importance of neighborhood safety highlights the link between environmental issues and adherence to physical exercise. Providing a safe communal environment appears essential for the promotion of exercise and the healing of injuries experienced by elderly African Americans after a fall of sufficient severity to stimulate an ED visit. Clearly, there is need for recognizing both similarities and differences among persons of diverse ethnic background in the cultural tailoring of trials that require active participation and involvement in exercise (Alexander, Uz, Hinton, Williams, & Jones, 2008). The relative preference for community-based group programs may be greater among African Americans than in the general population. The importance of socialization is reflected in many cultural activities ranging from family reunions to religious worship and may explain why adherence to the on-site exercise class was so much higher.
The overwhelming preference for group over solitary exercise has implications with regard to the Health Insurance Portability and Accountability Act on services, such as rehabilitation, which increasingly encourages therapy in isolation from others to ensure privacy of health information (U.S. Department of Health and Human Services, 1996). Our inability to achieve adherence to the at-home component of the exercise program, even in light of an elaborate attempt to facilitate involvement, has major implications for the future design of protocols for elderly participants at risk of falls.
Although the weight of systematic evidence from over 55,000 participants involved in a variety of clinical trials is that exercise interventions reduce the risk of falls (Gillespie et al., 2009), some recent trials have been negative. These programs attempt to study the effectiveness of programs in usual care. Although these typically include a comprehensive multifaceted risk factor assessment, they rely on participants’ motivations to follow-up with referrals to primary care providers or existing community programs (Elley et al., 2008; Hendriks et al., 2008; Salminen, Vahlberg, Salonoja, Aarnio, & Kivelä, 2009). The translation of multidimensional falls prevention strategies into programs that are practical in usual care appears challenging.
These more recent studies, like the at-home component of our exercise program, depend on participant motivation for adherence. Our documented poor adherence of participants to the at-home component of the exercise program in spite of overall retention has implications both to future protocol development and to clinical practice. Because of cost containment, therapeutic exercise prescription, for example, relies increasingly on a very short period of physical therapy to teach patients exercises. There is increasing reliance on patients’ motivations for ongoing at-home exercise for the effects of treatment. Our findings suggest that patients may have difficulty adhering to such home-focused programs. Future studies documenting benefits or lack of benefits of such home-based programs will be essential.
We were able to recruit and successfully retain this predominantly African American population. Even though we had community interventionists and telephone support, follow through with exercise at home was poor. Nevertheless, participants enthusiastically attended and participated in the on-site group exercise classes. There was no evidence of disparity in adherence between the African Americans and the few individuals of other races in the program.
To our knowledge, few cohorts of people with falls sufficiently severe to require ED care have involved such a high proportion of African American participants. Indeed, the typical racial/ethnic proportions in published studies usually include 10% or fewer African Americans, whereas in our cohort, African Americans made up almost 90% of the participants. The high proportion of African Americans might be one explanation for the relatively high adherence to the on-site exercise classes, which may have stimulated feelings of community and connection.
This study was limited in a number of ways. One of the challenges to protocol designs of this nature is that, unlike many pharmacologic interventions that can be standardized, programs for frail clinically heterogeneous populations must be stepped or otherwise personalized to ensure safety and effectiveness. The challenges of recruitment and adherence were such that major reductions in the length of the exercise program from six months to four months became necessary in order to assure adequate resources and efforts (than originally budgeted). Thus, the intervention might not have been long enough to expect even functional change.
These findings are of considerable importance because of our focus on urban elderly African Americans, a population about whom little is known. It demonstrates the need for linkage between EDs, a major place of care for poor, elderly persons, and community outreach following treatment for a fall. Many urban African Americans are traditionally underserved, with excess vulnerability following one or more falls. Typically, less likely to enroll in trials, African American elderly participants in our study demonstrated interest, willingness, and enthusiasm for the on-site components of the falls prevention program but participated far less regularly in the at-home–based component of the program.
Conclusions
There is no doubt that people who are African Americans have been underrepresented in falls risk prevention studies. Published trials do not always characterize the samples according to race. Nevertheless, we believe that our study represents the largest recruitment of frail African Americans to such a program. This study suggests that it is feasible to successfully recruit large numbers of African Americans. In order to successfully retain and recruit this population, a plan for community support must be built into the protocol. Our program used information from focus groups drawn from the target population to discover ways to welcome the community we hoped to reach. The resulting adherence and retention intervention included telephone reminders and vouchers for taxi service because transportation was understood as a clear barrier to participation. Attempts were made to create an empowering environment by providing opportunities for socialization, such as the provision of a meal. There were opportunities for individual counseling about exercise, exercise supplies for the home, taped and written instructions, and community interventionists from the neighborhoods who provided additional support to study participants. Findings from both the focus group and the trial converge and suggest that frail elderly people need socialization and external supports in venues other than their homes if they are going to exercise. Such supports need to be considered when designing and budgeting trials. Senior centers and churches are a natural place where people congregate. Programs of this nature might be built into these centers and incorporated into church programs. Of particular note, religion plays a prominent place in the African American culture. Church is seen as promoting spiritual, mental, and physical well-being, and spirituality is seen as participation in healthy behaviors, particularly among women (Bopp et al., 2007). Future research targeted to older persons should be designed to incorporate specific strategies that will welcome and enhance the recruitment, adherence, and retention of people from diverse cultures and ethnic backgrounds. Information from focus groups of people drawn from the targeted population can be invaluable in trials that require participant motivation. Finally, we note the importance of living alone as a strong positive motivating factor to participation and depressed mood as a negative factor. These findings highlight the need to enhance opportunities for community involvement for elderly frail people who live alone and further to develop strategies for reaching those who isolate themselves because of depressive symptoms.
Funding
National Institute on Aging (1R01 AG16333), “Preventing Falls and Disability in Inner-City Elderly”; the John A. Hartford Foundation, Hartford Center of Geriatric Nursing Excellence, School of Nursing, University of Pennsylvania; the Resource Center for Minority Aging Research, “Reducing Health Disparities Across the Stages of Illness in Older Minority Populations with Chronic Disease,” (1P30AG031043-01) through the National Institutes of Health/National Institute on Aging, National Institute of Nursing Research, and the National Center on Minority Health and Health Disparities.
Acknowledgments
The authors wish to acknowledge Bill Edwards for his remarkable energy, enthusiasm, and efforts in managing participant recruitment, adherence, and retention.
References
- Alexander GK, Uz SW, Hinton I, Williams I, Jones R. Culture brokerage strategies in diabetes education. Public Health Nursing. 2008;25(5):461–470. doi: 10.1111/j.1525-1446.2008.00730.x. [DOI] [PubMed] [Google Scholar]
- Bean JF, Herman S, Kiely DK, Frey IC, Leveille SG, Fielding RA, et al. Increased velocity exercise specific to task (InVEST) training: A pilot study exploring effects on leg power, balance, and mobility in community-dwelling older women. Journal of the American Geriatrics Society. 2004;52:799–804. doi: 10.1111/j.1532-5415.2004.52222.x. [DOI] [PubMed] [Google Scholar]
- BeLue R, Taylor-Richardson KD, Lin J, Rivera AT, Grandison D. African Americans and participation in clinical trials: Differences in beliefs and attitudes by gender. Contemporary Clinical Trials. 2006;27:498–505. doi: 10.1016/j.cct.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Bogart L, Uyeda K. Community-based participatory research: Partnering with communities for effective and sustainable behavioral health interventions. Health Psychology. 2009;28:391–393. doi: 10.1037/a0016387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bopp M, Lattimore D, Wilcox S, Laken M, McClorin L, Swinton R, et al. Understanding physical activity participation in members of an African American church: A qualitative study. Health Education Research. 2007;22:815–826. doi: 10.1093/her/cyl149. [DOI] [PubMed] [Google Scholar]
- Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: New outcome measure for primary care. British Medical Journal. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Annals of Internals Medicine. 1993;118:201–210. doi: 10.7326/0003-4819-118-3-199302010-00009. [DOI] [PubMed] [Google Scholar]
- Elley CR, Robertson MC, Garrett S, Kerse NM, McKinlay E, Lawton B, et al. Effectiveness of a falls-and-fracture nurse coordinator to reduce falls: A randomized, controlled trial of at-risk older adults. Journal of the American Geriatrics Society. 2008;56:1383–1389. doi: 10.1111/j.1532-5415.2008.01802.x. [DOI] [PubMed] [Google Scholar]
- Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. American Journal of Respiratory and Critical Care Medicine. 1998;158(5 Pt 1):1384–1387. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [PubMed] [Google Scholar]
- Flegal KE, Kishiyama S, Zajdel D, Haas M, Oken BS. Adherence to yoga and exercise interventions in a 6-month clinical trial. BMC Complementary and Alternative Medicine. 2007;7:37. doi: 10.1186/1472-6882-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer. 2008;112:228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- Freedman TG. Why don’t they come to Pike Street and ask us”?: Black American women's health concerns. Social Science and Medicine. 1998;47:941–947. doi: 10.1016/s0277-9536(98)00167-1. [DOI] [PubMed] [Google Scholar]
- Friedman B, Heisel MJ, Delavan RL. Psychometric properties of the 15-item geriatric depression scale in functionally impaired, cognitively intact, community-dwelling elderly primary care patients. Journal of the American Geriatrics Society. 2005;53:1570–1576. doi: 10.1111/j.1532-5415.2005.53461.x. [DOI] [PubMed] [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD007146.pub2. CD007146. [DOI] [PubMed] [Google Scholar]
- Grisso JA, Kelsey JL, Strom BL, Chiu GY, Maislin G, O’Brien LA, et al. Risk factors for falls as a cause of hip fracture in women. The Northeast Hip Fracture Study Group. New England Journal of Medicine. 1991;324:1326–1331. doi: 10.1056/NEJM199105093241905. [DOI] [PubMed] [Google Scholar]
- Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: Assessment with a 6-minute walk test. Archives of Physical Medicine and Rehabilitation. 1999;80:837–841. doi: 10.1016/s0003-9993(99)90236-8. [DOI] [PubMed] [Google Scholar]
- Harris EM. Accessing community development research methodologies. Canadian Journal of Public Health. 1992;83(Suppl. 1):S62–S66. [PubMed] [Google Scholar]
- Hauer K, Rost B, Rutschle K, Opitz H, Specht N, Bartsch P, et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. Journal of the American Geriatrics Society. 2001;49:10–20. doi: 10.1046/j.1532-5415.2001.49004.x. [DOI] [PubMed] [Google Scholar]
- Hendriks MRC, Bleijlevens MHC, van Haastregt JCM, Crebolder HFJM, Diederiks JPM, Evers SMAA, et al. Lack of effectiveness of a multidisciplinary fall-prevention program in elderly people at risk: A randomized, controlled trial. Journal of the American Geriatrics Society. 2008;56:1390–1397. doi: 10.1111/j.1532-5415.2008.01803.x. [DOI] [PubMed] [Google Scholar]
- Horowitz CR, Brenner BL, Lachapelle S, Amara DA, Arniella G. Effective recruitment of minority populations through community-led strategies. American Journal of Preventive Medicine. 2009;37(6 Suppl. 1):S195–S200. doi: 10.1016/j.amepre.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katula JA, Kritchevsky SB, Guralnik JM, Glynn NW, Pruitt L, Wallace K, et al. Lifestyle interventions and independence for elders pilot study: Recruitment and baseline characteristics. Journal of the American Geriatrics Society. 2007;55:674–683. doi: 10.1111/j.1532-5415.2007.01136.x. [DOI] [PubMed] [Google Scholar]
- Lai GY, Gary TL, Tilburt J, Bolen S, Baffi C, Wilson RF, et al. Effectiveness of strategies to recruit underrepresented populations into cancer clinical trials. Clinical Trials. 2006;3:133–141. doi: 10.1191/1740774506cn143oa. [DOI] [PubMed] [Google Scholar]
- Lavizzo-Mourey R, Cox C, Strumpf N, Edwards WF, Lavizzo-Mourey R, Stineman M, et al. Attitudes and beliefs about exercise among elderly African Americans in an urban community. Journal of the National Medical Association. 2001;93:475–480. [PMC free article] [PubMed] [Google Scholar]
- Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: A randomized controlled trial. Journal of Gerontology A Biological Sciences and Medical Sciences. 2005;60:187–194. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, Cech S, et al. Kenosha County falls prevention study: A randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. Journal of the American Geriatrics Society. 2007;55:489–498. doi: 10.1111/j.1532-5415.2007.01144.x. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Jr., Rogers W, Raczek AE, Lu JF. The validity and relative precision of MOS short- and long-form health status scales and Dartmouth COOP charts. Results from the Medical Outcomes Study. Medical Care. 1992;30(5 Suppl.):MS253–MS265. doi: 10.1097/00005650-199205001-00025. [DOI] [PubMed] [Google Scholar]
- Means KM, Rodell DE, O’Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: Effects of a rehabilitation exercise program. American Journal of Physical Medicine and Rehabilitation. 2005;84:238–250. doi: 10.1097/01.phm.0000151944.22116.5a. [DOI] [PubMed] [Google Scholar]
- Michels KB, Rosner BA. Data trawling: To fish or not to fish. Lancet. 1996;348:1152–1153. doi: 10.1016/S0140-6736(96)05418-9. [DOI] [PubMed] [Google Scholar]
- Moore M, Williams B, Ragsdale S, Logerfo JP, Goss JR, Schreuder AB, et al. Translating a multifactorial fall prevention intervention into practice: A controlled evaluation of a fall prevention clinic. Journal of the American Geriatrics Society. 2010;58:357–363. doi: 10.1111/j.1532-5415.2009.02683.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health Office of Behavioral and Social Science Research. Qualitative methods in health research: Opportunities and considerations in application and review, organized by the NIH culture and qualitative research interest group. 1997. Retrieved October 18, 2004, from http://www.csr.nih.gov/archives/reviewcriteria.htm. [Google Scholar]
- Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. Journal of the American Medical Association. 1989;261:2663–2668. [PubMed] [Google Scholar]
- Nowalk MP, Prendergast JM, Bayles CM, D’Amico FJ, Colvin GC. A randomized trial of exercise programs among older individuals living in two long-term care facilities: The FallsFREE program. Journal of the American Geriatrics Society. 2001;49:859–865. doi: 10.1046/j.1532-5415.2001.49174.x. [DOI] [PubMed] [Google Scholar]
- Paskett ED, Reeves KW, McLaughlin JM, Katz ML, McAlearney AS, Ruffin MT, et al. Recruitment of minority and underserved populations in the United States: The Centers for Population Health and Health Disparities experience. Contemporary Clinical Trials. 2008;29:847–861. doi: 10.1016/j.cct.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps E, Harris D, Brown N, Harralson T, Brecher A, Polansky M, et al. Investigation of ethnic differences in willingness to enroll in a rehabilitation research registry: A study of the Northeast Cognitive Rehabilitation Research Network. American Journal of Physical Medicine and Rehabilitation. 2004;83:875–883. doi: 10.1097/01.phm.0000143436.57173.e1. [DOI] [PubMed] [Google Scholar]
- Pinsky PF, Ford M, Gamito E, Higgins D, Jenkins V, Lamerato L, et al. Enrollment of racial and ethnic minorities in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. Journal of the National Medical Association. 2008;100:291–298. doi: 10.1016/s0027-9684(15)31241-4. [DOI] [PubMed] [Google Scholar]
- Robinson JM, Trochim WM. An examination of community members’, researchers’ and health professionals’ perceptions of barriers to minority participation in medical research: An application of concept mapping. Ethnic Health. 2007;12:521–539. doi: 10.1080/13557850701616987. [DOI] [PubMed] [Google Scholar]
- Rugkasa J, Canvin K. Researching mental health in minority ethnic communities: Reflections on recruitment. Qualitative Health Research. 2010 doi: 10.1177/1049732310379115. Retrieved from Qual Health Res OnlineFirst, doi:10.1177/1049732310379115. [DOI] [PubMed] [Google Scholar]
- Salminen MJ, Vahlberg TJ, Salonoja MT, Aarnio PT, Kivelä SL. Effect of a risk-based multifactorial fall prevention program on the incidence of falls. Journal of the American Geriatrics Society. 2009;57:612–619. doi: 10.1111/j.1532-5415.2009.02176.x. [DOI] [PubMed] [Google Scholar]
- Sattin RW, Lambert Huber DA, DeVito CA, Rodriguez JG, Ros A, Bacchelli S, et al. The incidence of fall injury events among the elderly in a defined population. American Journal of Epidemiology. 1990;131:1028–1037. doi: 10.1093/oxfordjournals.aje.a115594. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Silver IF, LeMier M, York S, Cummings P, Koepsell TD. Effectiveness of a community-based multifactorial intervention on falls and fall risk factors in community-living older adults: A randomized, controlled trial. Journal of Gerontology A Biological Sciences and Medical Sciences. 2007;62:1420–1427. doi: 10.1093/gerona/62.12.1420. [DOI] [PubMed] [Google Scholar]
- Stineman MG. A model of health environmental integration. Topics in Stroke Rehabilitation. 2001;8:34–45. doi: 10.1310/0L5G-NQHY-GH4K-HV58. [DOI] [PubMed] [Google Scholar]
- Stineman MG, Streim JE. The biopsycho-ecological paradigm: A foundational theory for medicine. PM & R. 2010;2(11):1035–1045. doi: 10.1016/j.pmrj.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, Baker DI, Garrett PA, Gottschalk M, Koch ML, Horwitz RI. Yale FICSIT: Risk factor abatement strategy for fall prevention. Journal of the American Geriatrics Society. 1993;41:315–320. doi: 10.1111/j.1532-5415.1993.tb06710.x. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. New England Journal of Medicine. 1994;331:821–827. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. New England Journal of Medicine. 1997;337:1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. The health insurance portability and accountability privacy rule. 1996. Retrieved July 9, 2009, from http://www.hhs.gov/ocr/privacy/index.html. [Google Scholar]
- van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: A review. American Journal of Preventive Medicine. 2002;22:120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr K, Griffith D, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2004. Community-based participatory research: Assessing the evidence. Evidence Report/Technology Assessment No. 99 (Prepared by RTI–University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016). AHRQ Publication 04-E022-2. Retrieved from http://www.ahrq.gov/downloads/pub/evidence/pdf/cbpr/cbpr.pdf. [PMC free article] [PubMed] [Google Scholar]
- Ware JE. SF-36 Health Survey: Manual and interpretation guide. Boston, MA: New England Medical Center; 1993. [Google Scholar]
- Wilbur J, McDevitt J, Wang E, Dancy B, Briller J, Ingram D, et al. Recruitment of African American women to a walking program: Eligibility, ineligibility, and attrition during screening. Research in Nursing and Health. 2006;29:176–189. doi: 10.1002/nur.20136. [DOI] [PubMed] [Google Scholar]
- Yancey AK, Miles OL, McCarthy WJ, Sandoval G, Hill J, Leslie JJ, et al. Differential response to targeted recruitment strategies to fitness promotion research by African-American women of varying body mass index. Ethnic Disease. 2001;11:115–123. [PubMed] [Google Scholar]