Abstract
Purpose: To conduct and evaluate a two-phased community-based approach to recruit lower socioeconomic status, minority, or Spanish-speaking adults at risk of developing diabetes to a randomized trial of a lifestyle intervention program delivered by a public health department. Design: Within geographic areas comprising our target population, 4 community organizations provided local space for conducting the study and program. Phase I—outreach in venues surrounding these organizations—included diabetes education, a short diabetes risk appraisal (DRA), and diabetes risk screening based on a fasting fingerstick glucose test. Phase II—trial recruitment—began concurrently for those found to be at risk of developing diabetes in Phase I by explaining the study, lifestyle program, and research process. Those interested and eligible enrolled in the 1-year study. Results: Over 2 years, approximately 5,110 individuals received diabetes education, 1,917 completed a DRA, and 1,164 were screened of which 641 (55%) had an elevated fingerstick result of ≥106 mg/dl. Of the study sampling frame—persons over age 25 at risk of developing diabetes (N = 544)—238 (43%) enrolled in the trial; of those who were study eligible (n = 427), 56% enrolled. In the final sample, mean age was 56 years (SD = 17), 78% were ethnic minorities, 32% were Spanish-speaking, and 15% had a high school education or less. Implications: Providing diabetes health education and screening prior to study recruitment may help overcome barriers to research participation in underserved communities, thus helping address difficulties recruiting minority and older populations into research, particularly research pertaining to chronic disease risk factors.
Keywords: Translational research, Recruitment, Health education, Minority populations, Academic–Community partnership
Two large-scale clinical trials, the Diabetes Prevention Program and the Finnish Diabetes Prevention Study, have provided unequivocal evidence that type 2 diabetes mellitus in high-risk individuals can be prevented through lifestyle modifications, such as increased physical activity, weight loss, and dietary changes (Diabetes Prevention Program Research Group, 2002; Tuomilehto et al., 2001). Efforts to translate such lifestyle modification programs for individuals at risk of type 2 diabetes from health care settings into community settings are an important next step. A greater risk of diabetes is observed for ethnic minority (Centers for Disease Control and Prevention, 2008; Liao et al., 2004) and lower socioeconomic status (SES) groups (Robbins, Vaccarino, Zhang, & Kasl, 2005) compared to Whites of similar ages.
Two issues in translating such lifestyle programs from medical to community settings to reach these vulnerable population groups are to identify a community organization that can deliver a lifestyle program within existing infrastructure and community-based methods for identifying people at risk of diabetes. To evaluate such programs through research also requires addressing study recruitment issues because ethnic minorities and individuals of lower SES are less likely than their counterparts to participate in interventions and randomized trials (Glasgow, Toobert, & Hampson, 1991; Yancey, Ortega, & Kumanyika, 2006). Addressing these recruitment and translational issues requires using existing community resources, collaborating with community organizations and leaders, and understanding and working within existing networks and relationships between these organizations and community members (Israel, Schulz, Parker, & Becker, 1998).
This article describes a two-phased community-based approach to identify and recruit lower SES, ethnic minority, and Spanish-speaking adults at risk of developing diabetes to a randomized trial of a lifestyle program to reduce risk through diet and physical activity. Our approach was designed to work within the community infrastructure and incorporate local resources. We describe our collaboration with community organizations, methods used to identify our target groups and screen for diabetes risk, and report the number of people who completed screening and their levels of risk using these different methods. We then describe methods for recruiting a subset of those found to be at risk into the randomized trial, report response rates and sampling bias assessment, and describe our enrolled sample.
Methods
The project was a partnership between the City of Berkeley Division of Public Health (BDPH) and the University of California San Francisco (UCSF). BDPH staff delivered the lifestyle program through its chronic disease prevention infrastructure, and UCSF conducted the randomized trial. The research protocol was approved by the UCSF Institutional Review Board; written consent was obtained from all study participants. Our methods were designed to overcome barriers to recruitment of lower income, minority, and older adults including factors related to the study, environment, individuals, and the intervention (Nápoles-Springer, Santoyo, & Stewart, 2005; Warren-Findlow, Prohaska, & Freedman, 2003) based on recommendations for overcoming these barriers (Levkoff & Sanchez, 2003; Nápoles-Springer et al., 2000; UyBico, Pavel, & Gross, 2007; Warren-Findlow et al., 2003; Yancey et al., 2006).
Study Population
BDPH identified geographic areas with high poverty rates within its service area. Within these areas, recruitment focused on African Americans, Latinos, and lower SES adults of any race/ethnicity because these groups have higher rates of diabetes and its risk factors than their counterparts nationally (noted above) and locally (City of Berkeley Public Health Division Community Health Action and Assessment Section, 2007).
Identify Community Partners
To provide outreach, recruitment, study, and program components in convenient and familiar locations, we sought a few community organizations serving our target groups to partner with us to provide the needed space. Three senior centers and a Latino community center agreed to be key partners. In return, we offered free diabetes education and screening events at these centers and a physician-quality weight/height scale. We also generated a flow of new people to these centers based on our outreach to adults patronizing nearby venues, such as adult schools and places of worship.
Methods of Outreach and Recruitment: Two Phases
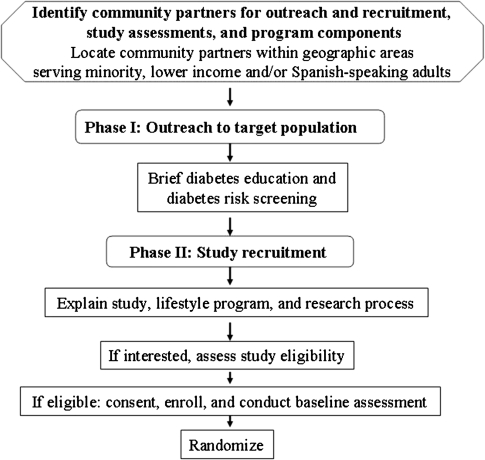
Outreach and recruitment were conducted in two phases (Figure 1). Phase I (outreach) included diabetes health education and screening which was offered by the public health department to people of all ages. Study recruitment (Phase II) began with those found to be at risk for developing diabetes in Phase I. This two-phased approach allowed us to first establish contact and provide a service (diabetes education and screening) to help establish trust and credibility before attempting to recruit people into the study. All of our outreach materials are available on the Live Well, Be Well Web site (http://iha.ucsf.edu/LiveWellBeWell/).
Figure 1.
Overview of outreach and recruitment process.
Phase I: Outreach to Target Population.—
We used four broad types of outreach: person-to-person involving project staff, referral by friend or family member, outreach by professionals and community partners/organizations, and traditional media. Person-to-person outreach involved trained project staff, which was ethnically and linguistically diverse and included community health workers and research staff. Formal presentations were hour-long diabetes education presentations. Informal, brief 5-min presentations were made at our key community sites, for example, to a class. Tabling—having a table at community events such as farmers markets—enabled staff to engage passersby to discuss diabetes and its preventability. Person-to-person outreach also was conducted in other settings such as small business districts. At screening events, passersby often inquired about what we were doing (“onlookers”), thus screenings also served as “tabling” events. All person-to-person methods included invitations to upcoming screenings for a fasting fingerstick test (described below).
Other types of outreach did not involve project staff. We encouraged people who had received a screening to tell family members and friends about upcoming formal presentations or screenings, offering $5 for referring someone. We encouraged community professionals such as nurses/physicians, senior housing coordinators, and senior-center van drivers to refer people to events. Our community partners conducted some outreach on their own, for example, advertised screenings in their newsletters. Also emails, including a motivating health message, were sent to health department employees advertising screenings. Traditional media-based outreach included local newspaper and community radio station ads inviting people to events. All media information (written, visual, or auditory) was delivered in English and Spanish and designed for lower-literacy individuals and to be culturally appropriate.
Brief diabetes education.
All staff-based outreach involved brief diabetes education, that is, that type 2 diabetes is preventable, that many individuals at risk do not know it, and describing diabetes risk factors. Individuals were invited to complete a “diabetes risk appraisal” (DRA), a 1-page tool we created based on published diabetes risk factors such as family history of diabetes. The DRA, adapted from existing American Diabetes Association (ADA) and Finnish Diabetes Prevention Study diabetes risk tools for community settings, used only self-reported variables and simplified scoring. Each item was weighted to determine level of risk. Weights were based on those used in the ADA and Finnish tools, and a ≥4 cut-point (range 0–16) was used to identify those “likely at risk for developing diabetes” akin to the ADA tool. With the DRA, we aimed to raise awareness of personal diabetes risk factors and motivate people to obtain a fasting fingerstick glucose test. Staff administered, scored, and explained the DRA score. Having staff administer the DRA helped those with low literacy/numeracy or trouble seeing and facilitated engaging individuals to discuss diabetes risk and prevention. Individuals received a card with their score and an interpretation, were encouraged to attend a screening, and given a flyer of upcoming screenings with fasting instructions.
Diabetes risk screening.
The screenings aimed to provide individuals with their fasting fingerstick glucose test result as an objective diabetes risk indicator (in addition to the DRA) and increase awareness of the meaning of fasting glucose (diabetes education). Because fasting venous blood tests are inconvenient, expensive, and not routine public health methods, we measured fasting capillary (fingerstick) blood glucose levels using the Accu-chek glucometer (hereafter referred to as the fingerstick test). The fingerstick test, used primarily by diabetes patients to self-monitor glucose levels, is a simple procedure that can be done by trained staff, thus providing a feasible community-based method to screen for risk. Fingerstick test results provided an estimate of diabetes risk; this test is not recommended for establishing a diagnosis of diabetes. We obtained verbal consent for the fingerstick test and to retain their results.
We used data from two large community-based studies to determine appropriate thresholds of fasting fingerstick (capillary) blood glucose levels that would correlate with elevated venous blood glucose results (≥95 mg/dl; Rolka et al., 2001; Zhang et al., 2003). All participants were given a results card with an interpretation, received appropriate diabetes education materials, and were offered light refreshments and a $5 gift card.
Participants were classified into three categories: (a) <106 mg/dl, (b) 106–160 mg/dl, or (c) >180 mg/dl. Those in Category 3 were told they should contact their physician within two weeks. Those with borderline values (161–180 mg/dl) were offered a venous blood test for confirmation; venous blood values ≥126 mg/dl were classified as Category 3 and values between 100 and 125 mg/dl were classified as Category 2. Those who declined were classified as Category 3.
Phase II: Study Recruitment.—
Study recruitment was initiated only for those who had a fingerstick result of 106–160 mg/dl (Category 2 above), were at least 25 years of age, and had a DRA score ≥4. Individuals meeting these three criteria were classified as “likely at risk for developing diabetes.” Although initially we designed the study for middle-aged and older adults (40 years and older) who are most at risk of diabetes, we lowered the minimum to 25 years because our screening in the Latino community identified many adults at younger ages who were at risk of developing diabetes and could benefit from the program. The recruitment process included asking if they would be interested in hearing about the free lifestyle program and research study and then explaining the lifestyle program, study, and research process. Those still interested were screened for study eligibility, and those eligible were enrolled.
The lifestyle program promoted increased physical activity, improved diet, and weight loss through an introductory session, an individual planning session, a participant program binder, telephone calls, and group workshops (Delgadillo et al., 2010). A counselor provided education, skills, and support according to participants’ preferences and readiness for change. The study was a randomized controlled trial in which those randomly assigned to the intervention group received the one-year lifestyle intervention beginning immediately, and those assigned to the wait-list control group were offered the lifestyle program at the end of the year.
Special efforts were made to explain the research process to address lack of knowledge and distrust of research of lower SES, minority, Spanish-speaking, and older adults (Brown & Topcu, 2003; Levkoff & Sanchez, 2003; Nápoles-Springer et al., 2000; Yancey et al., 2006). To help individuals visualize the entire commitment, we created a research reference guide, a graphic of the twelve-month timeline for each randomized group. Using the guide, staff explained the lifestyle program and randomization, such as why we had two groups and how groups were selected randomly. We discussed what was expected (e.g., one-year commitment, three assessments including clinical measures, blood draws, and questionnaires). We emphasized that assessments were interviewer administered (to reassure those with low literacy). Staff answered questions and, to address potential transportation and time limitation barriers, explained that group-based program components and study assessments were held in the local community center from which they were screened and that taxi vouchers were available.
For those interested in participating, we determined study eligibility. Medical history exclusion criteria included: (a) told by a physician they have diabetes (other than gestational), (b) use of insulin or other diabetes medications, (c) heart attack, heart failure, stroke, or heart surgery (e.g., angioplasty) in past six months, (d) hip or knee replacement in past three months, (f) implanted defibrillator, and (g) insufficient cognitive functioning to complete program procedures. To include as many older adults as possible (who are more likely to have chronic conditions), other medical conditions were exclusionary only if physician consent was not obtained: pacemaker, heart disease, heart rhythm abnormalities or atrial fibrillation as well as chest pain, or faintness/dizziness in the past six months. Individuals needing physician consent were asked if they had a medical provider. We offered to help obtain physician consent (with their permission). Those without a medical provider were given a list of community health clinics. If physician consent was obtained, individuals continued enrollment procedures; if not, they were ineligible. Additional study exclusion criteria were (a) not conversant in English or Spanish, (b) plans to move out of the area within one year, (c) spouse/partner already enrolled, and (d) being pregnant.
Those eligible and still interested were scheduled for an enrollment appointment at which staff reviewed informed consent and answered questions. Individuals signed the consent, received a copy, and continued with blood draws, clinical measures, and questionnaires. On completion, they were given $25 cash and randomized.
Outreach and Recruitment Data Collected and Methods of Analysis
Two types of data were collected to track outreach and recruitment: event-level data describing each outreach and screening event and person-level data tracking each person throughout the entire process. Event data were collected for each outreach screening. Each event was assigned a unique identifier and documented on an event summary sheet. We recorded the type of event (e.g., presentation), date, location (e.g., adult school), staffing, duration, number of people reached, number of DRAs and fingerstick tests administered, and a narrative description. Event data were entered into an “event-level” Access database.
To track each person throughout outreach and recruitment, a person-level tracking form was begun when we first obtained a person's name. Each person was assigned a unique identifier. Along with basic information (contact information, age category, DRA score), we asked how they heard about the screening. Tracking form data were entered into a “person-level” Access database. As people attended subsequent events or were screened for eligibility, the form was updated (with verbal consent), including the date and outcome of each contact (e.g., phone call, screening event) and the final disposition code.
To summarize the amount of outreach required to identify the target population, we classified outreach venues into eight types based on event data forms: adult schools, K-12 schools and childcare centers, nonprofit sector, private sector, housing, places of worship, general community events, and public settings (e.g., contact without a specific locale). For each type, we calculated the number of events held, the number of people reached at those events, the average number reached per event, and the number of DRAs completed.
To report the yield of the various outreach methods, based on how people heard about the screenings or presentations, we calculated for each type of method the number of people who completed a fingerstick test, the number having an elevated fingerstick result of ≥106 mg/dl, and the number randomized. To indicate the extent to which we enrolled our target population, we present demographic data on our enrolled sample.
Traditional response rates (i.e., the proportion of those eligible who enrolled) do not reflect precisely our recruitment process because of the iterative nature in which we learned about ineligibility. Because ineligibility was often learned by staff during conversations with potential participants (e.g., during a screening), those from the sampling frame we knew were ineligible were not queried about interest in hearing about the study. Thus, there is no clear denominator of potentially eligible participants by which to calculate meaningfully the percent of eligible who enrolled. Response rates were thus calculated using two denominators, that is, the number of people who enrolled out of the entire sampling frame and the number who enrolled from the portion of the sampling frame that was not ineligible (an imprecise estimate of those who were eligible).
Among those never determined to be ineligible, we assessed potential sampling bias by comparing those who enrolled and those who did not on three demographic variables obtained on the individual tracking forms for people who were ever contacted: age category, sex, and race/ethnicity using chi-square tests and simple logistic regression. All analyses were done using SAS 9.1.
Results
Table 1, organized by the type of community setting, summarizes the types and number of project-staffed outreach and screening events held, the number of people estimated to have been contacted with brief diabetes education, the average number of people reached per event, and the number who completed a DRA. Links to over 180 unique venues were established and 335 “project-staffed” outreach events were held. A total of 5,114 persons were reached of which about 1,917 completed a DRA. Because most screenings were held at our key community partner sites, the number of events in the non-profit sector venues was the highest. The average number of people reached per event varied from 7.5 (private sector settings) to 53.9 (general community events); the average overall was about 15.
Table 1.
Type and Number of Project-Staffed Outreach and Diabetes Risk Screening Events and Number of People Reached by Types of Community Settings (7/2006–7/2008)
| Type of community settinga | Description | Types of eventsb | Number of events | Number of people contacted | Average number of people per event | Number of DRAs |
| Adult schools (n = 2) | City sponsored schools offering low-cost/free classes including academic classes, courses in job training and English as a second language, community classes such as dance and art, and classes for adults aged 50 years and older. | FP, T, SE | 6 | 252 | 42 | 65 |
| K-12 schools or childcare centers (n = 15) | Schools (elementary, middle, or high school), childcare centers, and day camps (where parents pick up/drop off children). School health fairs or festivals. | FP, T, SE | 19 | 484 | 25.5 | 285 |
| Non-profit sector (n = 17 + 4 = 21) | Community centers or organizations, e.g., senior centers, recreation centers, public health department, libraries, health centers, and social services agencies. Social events and classes. | O, IP, FP, T, SE | 69 | 816 | 11.8 | 304 |
| 4 key partners comprising one community center serving Spanish speakers and three senior centers. Social events and classes. | O, IP, T, FP, SE | 153 | 1,170 | 7.6 | 469 | |
| Private sector (n = 88) | Commercial settings including stores, beauty salons, barber shop, auto shops, laundromats, restaurants, ethnic-specific shops. Allowed to speak to customers of small businesses. | O, T | 20 | 149 | 7.5 | 27 |
| Housing (n = 8) | Subsidized housing facilities for seniors, disabled residents, and low-income families (some Section 8 housing from HUD). | FP, SE | 13 | 132 | 10.2 | 76 |
| Places of worship (n = 13) | Churches and temples. Health fairs, before/after services, and meeting rooms. | O, IP, FP, T, SE | 22 | 637 | 29 | 220 |
| General community events (n = 24) | Health fairs and expos; farmers markets; bike rodeos; various public events held in parks, college campuses, or hospitals. | O, IP, T, SE | 26 | 1,402 | 53.9 | 463 |
| Public open areas (n = 12) | Direct contact with people in parks, at bus stops, street corners, in parking lots, or in small business districts. | O | 7 | 72 | 10.3 | 8 |
| Total | 335 | 5,114 | 15.3 | 1,917 |
Notes: DRA = diabetes risk appraisal.
aNumber in parentheses indicates number of unique settings for each category.
FP = formal presentation; IP = informal presentation; O = one-on-one; SE = screening event; T = tabling.
In Table 2, we present the number of people who completed a fasting fingerstick glucose test, the number having an elevated fingerstick result of ≥106 mg/dl, and the number randomized in the study. These numbers are shown according to the major types of outreach methods based on reports of how people heard about the screening. We present separately efforts by professionals in the Latino community because of differences in approach. Column one shows the number completing screening (n = 1,164) with subtotals for each type of outreach. Nearly 1/3 of those who completed screening (378/1,164) heard about it through person-to-person staff outreach. Nearly half heard about the event through professionals and community partners/organizations: about 25% through efforts by the Latino community and 24% through efforts by other professionals and community organizations. Also in Table 2, of 1,164 completing a fasting fingerstick glucose test, 641 (55%) had an elevated fingerstick result of ≥106 mg/dl, a proportion that was fairly consistent across the five types of outreach.
Table 2.
Number of People Completing Diabetes Risk Screening, Number With Elevated Fingerstick Result, and Number Randomized by How They Heard About Event
| How people heard about a screening event or presentation | Number completing fingerstick glucose test | Number with fingerstick result of ≥106 mg/dl | Number randomized |
| Person-to-person involving project staff person | |||
| Formal presentation (places of worship and housing centers) | 16 | 13 | 6 |
| Informal presentation | 70 | 27 | 7 |
| Tabling | 148 | 99 | 39 |
| One-on-one outreach | 13 | 5 | 2 |
| Onlookers at fingerstick screening events (“tabling” at these events) | 131 | 77 | 22 |
| Subtotal | 378 | 221 | 76 |
| Referral by friend or family member of those already screened | |||
| Word of mouth—friend or family | 135 | 80 | 21 |
| Word of mouth—“bring a friend” campaign | 34 | 19 | 8 |
| Subtotal | 169 | 99 | 29 |
| Outreach by professionals and community partners/organizations: the Latino community | |||
| ESL teacher (to ESL students) | 106 | 27 | 3 |
| School teacher/administrator (to parents) | 112 | 60 | 22 |
| Other professional (phone or in person) | 29 | 17 | 8 |
| Flyer from school (to parents) | 33 | 13 | 9 |
| School telephone “tree” (automated calls to parents) | 14 | 7 | 6 |
| Subtotal | 294 | 124 | 48 |
| Outreach by other professionals and community partners/organizations | |||
| Word of mouth—other professional | 59 | 42 | 10 |
| Mass email to employees about on-site screening | 71 | 35 | 16 |
| Senior center or church newsletter about on-site screening | 39 | 23 | 11 |
| Flyers about on-site screening | 108 | 61 | 29 |
| Subtotal | 277 | 161 | 66 |
| Media | |||
| Community newspaper ad | 42 | 32 | 16 |
| Community radio ad | 4 | 4 | 3 |
| Subtotal | 46 | 36 | 19 |
| Grand total | 1,164 | 641 | 238 |
Note: ESL = English as Second Language.
Figure 2 presents the flowchart of recruitment. The sampling frame comprised 544 individuals who were “likely at risk of developing diabetes” according to the fingerstick test, had a DRA score ≥4, and were at least 25 years of age. Of the 544, 68 were known to be ineligible based on staff knowledge or judgment, thus 476 were invited to hear about the program and study.
Figure 2.
Flowchart of recruitment of sampling frame of persons age ≥25 years and likely at risk of developing diabetes.
Recruitment and Sampling Outcomes
Throughout the entire process, from the initial sampling frame of 544 persons, a total of 117 (22%) were ineligible and 189 (35%) were not interested or lost to follow-up (Figure 2). The most common reasons for ineligibility were planning to move (n = 33), language barriers (n = 32), and having diabetes (n = 30). Common anecdotal reasons for not participating were having no time, wanting to work with their physician or join a lifestyle program offered through their medical group, or felt they were already living a healthy lifestyle.
To understand the extent to which the two-phased approach resulted in people who might be interested, of those invited to learn about the lifestyle program and study (476), 429 (90%) were interested in hearing an explanation, suggesting some readiness to consider such a step after learning their risk. After hearing about the study and program, 93 individuals were not interested in enrolling. Thus, of those persons invited to hear about the study and program, a total of 140 (29%) were not interested.
Of the sampling frame of 544, the response rate was 44% (238/544); the rate was higher for Spanish-speaking individuals (47%) than English speakers (43%). Of 427 eligible persons (544 − 117 = 427), 238 (56%) were randomized; this rate also was slightly higher for Spanish-speaking persons (57%) than for English speakers (55%).
Regarding sample bias, among those never identified as ineligible (N = 427), there were no age group or sex differences between those who enrolled and those who did not.
Sample characteristics of those enrolled are shown in Table 3 for the total sample (N = 238) and separately for Spanish-speaking Latinos (N = 77) and English-speaking individuals (N = 161). Of the total sample, 39% were Latino, 22% African American, and 22% Caucasian. About 40% had a high school diploma or less; 23% had no health insurance, and 32% had experienced financial hardship in the past year. Approximately 78% were aged 40 years and older (32% were 65 years and older). Thus, we were successful in enrolling an ethnically and socioeconomically diverse sample. Group differences between English and Spanish speakers reflect differences in the demographics of the communities targeted.
Table 3.
Sample Characteristics of Individuals Randomized in the Study by Language
| English speaking (n = 161), n (%) | Spanish speaking (n = 77), n (%) | Total (n = 238), n (%) | |
| Age, years | |||
| M (SD) | 64.1 (13.3) | 38.8 (8.9) | 55.9 (16.9) |
| Range | 28–91 | 25–66 | 25–91 |
| Age category in years | |||
| 25–39 | 6 (3.7) | 46 (59.7) | 52 (21.9) |
| 40–64 | 80 (49.7) | 30 (39.0) | 110 (46.2) |
| 65+ | 75 (46.6) | 1 (1.3) | 76 (31.9) |
| Gender | |||
| Female | 105 (65.2) | 71 (92.2) | 176 (74.0) |
| Male | 56 (34.8) | 6 (7.8) | 62 (26.1) |
| Race/ethnicity | |||
| Caucasian | 52 (32.3) | 0 | 52 (21.9) |
| Black/African American | 53 (32.9) | 0 | 53 (22.3) |
| Latino or Hispanic | 14 (8.7) | 77 (100) | 91 (38.2) |
| South Asian | 5 (3.1) | 0 | 5 (2.1) |
| Other Asian | 32 (19.9) | 0 | 32 (13.5) |
| Native American, Pacific Islander | 2 (1.2) | 0 | 2 (0.8) |
| Multiethnic | 3 (1.9) | 0 | 3 (1.3) |
| Education | |||
| <8 years | 2 (1.2) | 30 (39.0) | 32 (13.5) |
| 9–11 years | 6 (3.7) | 21 (27.3) | 27 (11.3) |
| High school diploma | 21 (13.0) | 15 (19.5) | 36 (15.1) |
| Some college | 52 (32.3) | 5 (6.5) | 57 (24.0) |
| Bachelor's degree | 51 (31.7) | 6 (7.8) | 57 (24.0) |
| Professional degree | 29 (18.0 | 0 | 29 (12.2) |
| Married/living with a partner | 61 (38.1) | 64 (83.1) | 125 (52.5) |
| Health insurance | |||
| Any private | 117 (73.1) | 24 (33.3) | 141 (60.8) |
| Public | 23 (14.4) | 14 (19.4) | 37 (16.0) |
| None | 20 (12.5) | 34 (47.2) | 54 (23.3) |
| Financial hardship in past yeara | 30 (18.6) | 45 (58.4) | 75 (31.5) |
| Arthritisb | 69 (43) | 12 (16) | 81 (34) |
| Hypertensionc | 100 (62) | 11 (14) | 111 (47) |
Notes: aIn the past twelve months, was there ever a time when you did not have enough money to meet your daily needs?
Has a health professional ever told you that you had arthritis or other joint problems?
By clinical assessment, systolic >140 mmHg or diastolic >90 mmHg, or self-report of using any blood pressure medication.
Discussion
Our success recruiting our target population (lower SES, minority, or Spanish-speaking adults at risk of developing diabetes) suggests that our overall strategy may be a model for other studies trying to reach vulnerable and underserved groups. Indeed, about 80% of our final sample is either ethnic minority or had less than or equal to a high school education. Based on Census 2000 and American Community Survey 2006–2008 data for the City of Berkeley (U.S. Census Bureau, 2000, 2008), we overrepresented Latinos and African Americans as well as individuals with a high school or less education. Given difficulties recruiting minority and underserved populations, our approach may offer new ideas for recruiting these population groups into research pertaining to chronic diseases or randomized trials.
We designed outreach and recruitment to utilize existing community resources, to address as many known barriers to recruitment as possible for our targeted groups, and to take advantage of cultural factors supporting participation in research. Most of our methods, delivered in a variety of community settings, are commonly used to recruit vulnerable populations. The uniqueness is that we used these approaches to recruit people to a screening event to assess diabetes risk, not to recruit people directly into the study.
Because outreach and screening were conducted “in-person” by our diverse staff and held at familiar community venues, once a person was deemed “likely at risk of developing diabetes” and recruitment efforts initiated, familiarity with the staff and the setting may have overcome lack of trust, a common barrier (Escobar-Chaves, Tortolero, Masse, Watson, & Fulton, 2002; Stewart et al., 2006; Warren-Findlow et al., 2003). Holding study and program components in local venues and offering to help with transportation and childcare made it more convenient to participate (Escobar-Chaves et al., 2002; UyBico et al., 2007; Warren-Findlow et al., 2003; Yancey et al., 2006). Explaining the research process using a simple systematic approach may have helped overcome lack of familiarity with research, aversion to randomization, and concern about low literacy (Escobar-Chaves et al., 2002; Fisher et al., 2002; Warren-Findlow et al., 2003; Yancey et al., 2006). Although others have suggested doing this (Dennis & Neese, 2000), few studies have done so systematically.
We considered possible reasons why people decided to enroll. First, in Phase II, we were working within a “window of opportunity” in which people had just learned they were “at risk,” thus the study and program were offered as a potential action that could be taken. Consistent with the Health Belief Model (Janz, Champion, & Strecher, 2002), this “perception of risk” may have helped people decide to do something. Second, once people invest time in something, they are more likely to continue (Rubin et al., 2002); the fact that individuals had received diabetes education, completed a DRA, and attended a screening event may have influenced their decision to enroll. This is supported by our finding that 90% of those invited to hear more about the study were interested in having the study explained. Last, many people in our targeted neighborhoods had limited access to health care, precluding opportunities for education and lifestyle programs. The “opportunity” of this lifestyle program may have helped people decide to enroll. Despite our successes, we are concerned that almost 30% of those “at risk” and potentially eligible were not interested at the outset.
This project adhered to several principles of Community-Based Participatory Research (Israel et al., 1998) including building on community strengths and resources, facilitating collaborative partnerships, and integrating knowledge and action for the mutual benefit of all partners. By joining with a health department that already served our target population, we built on community resources, enabling us to conduct a large health education and screening effort modeled after the health department's usual programs. We had two types of collaborative partnership—with the health department to conduct outreach, recruitment, and deliver the lifestyle program and with the four community centers that provided space throughout the entire project. Finally, this project was mutually beneficial: to the university to complete the randomized trial, to the health department because the program was designed to be theirs and remained so at the end of the study, and to the community centers that received several benefits described in our methods. In addition, all outreach and screening took place in the communities in which our target population lived, thus people never had to travel outside of their neighborhood.
Although we could not assess the relative efficiency of the different methods of outreach, our results have implications for future recruitment efforts. To get people to attend a screening event, we invested the most time and staffing in outreach events involving project staff, for example, presentations and tabling. However, results showed that nearly half of those attending a screening event had heard about the screenings through professionals and community partners, which was clearly less expensive. It must be kept in mind, however, that these professionals were inviting people to a diabetes screening, not to a research study. Thus, effort by these community professionals may have been because the diabetes education and screenings provided a unique resource to otherwise underserved communities. Referral by friends or family members also had minimal associated study costs but yielded about 15% of those screened.
Efforts by professionals and community organizations to invite people to a screening had almost no associated cost. Thus, engaging professionals in getting the word out about a study (or screening) clearly is a benefit. Indirectly, organizations that allowed us to conduct outreach and screening at their sites served as “gatekeepers” known to be influential in recruitment (Sinclair et al., 2000). Several Latino community organizations made considerable effort to recruit people to the screenings, which was important in recruiting Spanish-speaking Latinos. Although we informed professionals in all communities about the screenings and study, professionals in the Latino community made primarily “person-to-person” contacts. For example, an adult school director invited us to discuss diabetes and the screening events to English as Second Language teachers, many of whom invited us to speak to their students. One school implemented an automated “phone tree” informing parents about the screenings, and several principals sent flyers home to parents. These extra efforts by professionals in the Latino community suggest that we filled a need for bilingual health education and screening.
Although our use of community-based diabetes education and screening as a first step was unique at the time we designed the study, several recent lifestyle intervention studies have used community-based approaches. One focusing on young African American women offered community-based blood pressure screening and recruited those at risk (Staffileno & Coke, 2006). Ackermann, Finch, Brizendine, Zhou, and Marrero (2008) used a self-report screening tool and non-fasting capillary glucose testing in community settings to identify people at risk of developing diabetes for their YMCA-based lifestyle program. However, only people with one of several listed diabetes risk factors were eligible to attend the screenings. Others have used community-based screening; however, it was to determine study eligibility rather than to screen for risk as a community service (Seidel, Powell, Zgibor, Siminerio, & Piatt, 2008). Given the substantial differences in the target population and the sequence of offering screening as a first step, it is not useful to compare our response rate to these studies.
Implications
Our approach may offer some innovative solutions to investigators struggling with known difficulties recruiting minority, lower SES, and older populations into research pertaining to chronic disease risk factors. Our university–public health department partnership and involvement of key community organizations provide a model of “mutually beneficial” outreach and screening. For academic researchers, recruitment typically involves identifying potential participants, explaining the research study, and motivating people to join, clearly a labor-intensive task, particularly when done one person at a time. By joining with a health department that conducts health education and screening routinely, in addition to adding credibility to academic researchers in the community, much “preparation” and awareness of the relevance of an issue can be done prior to recruitment. Indicators of the usefulness of our approach are that our final sample reflects our targeted population groups known to be underrepresented in research and our response rate considering we asked for a commitment to a one-year randomized trial.
Funding
This work was supported by a translational research grant (R18 DK067896-01A2) from the National Institute of Diabetes and Digestive and Kidney Diseases and by a grant (P30-AG15272) under the Resource Centers for Minority Aging Research program of the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases, National Institute on Aging, or the National Institutes of Health.
Acknowledgments
Several City of Berkeley Division of Public Health staff members were critical to the success of the outreach, screening, and recruitment, including Kristen Tehrani, Tanya Moore, LeConté Dill, Michelle Irving, Elisa Gallegos, Lawrence Williams Jr., and Jerry Gooden. Kate Clayton, MPH, Health Promotion Chief, provided ongoing oversight to the outreach and recruitment. Sunoz “Sunny” Soroosh contributed enormously to this effort through an NIH/NIDDK STEP-UP summer internship. Priya Asthana and Julie Thai dedicated valued efforts as volunteers during the outreach and recruitment process. We are grateful to administrators and staff of our four community partners who generously provided space and support during this entire process: North Berkeley Senior Center, South Berkeley Senior Center, Downtown Oakland Senior Center, and the Latina Community Center. Steve Gregorich, PhD, provided statistical guidance.
References
- Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community: The DEPLOY pilot study. American Journal of Preventive Medicine. 2008;35:357–363. doi: 10.1016/j.amepre.2008.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DR, Topcu M. Willingness to participate in clinical treatment research among older African Americans and Whites. The Gerontologist. 2003;43:62–72. doi: 10.1093/geront/43.1.62. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National diabetes fact sheet: General information and national estimates on diabetes in the United States, 2007. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- City of Berkeley Public Health Division Community Health Action and Assessment Section. City of Berkeley health status report, 2007. Berkeley, CA: Department of Health and Human Services, Public Health Division; 2007. [Google Scholar]
- Delgadillo AT, Grossman M, Santoyo-Olsson J, Gallegos-Jackson E, Kanaya AM, Stewart AL. Description of an academic community partnership lifestyle program for lower income minority adults at risk for diabetes. Diabetes Educator. 2010;36:640–650. doi: 10.1177/0145721710374368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis BP, Neese JB. Recruitment and retention of African American elders into community-based research: Lessons learned. Archives of Psychiatric Nursing. 2000;14:3–11. doi: 10.1016/s0883-9417(00)80003-5. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar-Chaves SL, Tortolero SR, Masse LC, Watson KB, Fulton JE. Recruiting and retaining minority women: Findings from the Women on the Move study. Ethnicity and Disease. 2002;12:242–251. [PubMed] [Google Scholar]
- Fisher EB, Walker EA, Bostrom A, Fischhoff B, Haire-Joshu D, Johnson SB. Behavioral science research in the prevention of diabetes: Status and opportunities. Diabetes Care. 2002;25:599–606. doi: 10.2337/diacare.25.3.599. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Toobert DJ, Hampson SE. Participation in outpatient diabetes education programs: How many patients take part and how representative are they? Diabetes Educator. 1991;17:376–380. doi: 10.1177/014572179101700509. [DOI] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Janz NK, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research, and practice. 3rd ed. San Francisco, CA: Jossey-Bass; 2002. pp. 45–66. [Google Scholar]
- Levkoff S, Sanchez H. Lessons learned about minority recruitment and retention from the centers on minority aging and health promotion. In: Curry L, Jackson J, editors. The science of inclusion: Recruiting and retaining racial and ethnic elders in health research. Vol. 43. Washington, DC: Gerontological Society of America; 2003. pp. 8–16. [Google Scholar]
- Liao Y, Tucker P, Okoro CA, Giles WH, Mokdad AH, Harris VB. REACH 2010 surveillance for health status in minority communities—United States, 2001–2002. Morbidity and Mortality Weekly Report. Surveillance Summaries. 2004;53:1–36. [PubMed] [Google Scholar]
- Nápoles-Springer AM, Grumbach K, Alexander M, Moreno-John G, Forte D, Rangel-Lugo M, et al. Clinical research with older African Americans and Latinos: Perspectives from the community. Research on Aging. 2000;22:668–691. [Google Scholar]
- Nápoles-Springer AM, Santoyo J, Stewart AL. Recruiting ethnically diverse general internal medicine patients for a telephone survey on physician-patient communication. Journal of General Internal Medicine. 2005;20:438–443. doi: 10.1111/j.1525-1497.2005.0078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and diagnosed diabetes incidence. Diabetes Research and Clinical Practice. 2005;68:230–236. doi: 10.1016/j.diabres.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Rolka DB, Narayan KM, Thompson TJ, Goldman D, Lindenmayer J, Alich K, et al. Performance of recommended screening tests for undiagnosed diabetes and dysglycemia. Diabetes Care. 2001;24:1899–1903. doi: 10.2337/diacare.24.11.1899. [DOI] [PubMed] [Google Scholar]
- Rubin RR, Fujimoto WY, Marrero DG, Brenneman T, Charleston JB, Edelstein SL, et al. The Diabetes Prevention Program: Recruitment methods and results. Controlled Clinical Trials. 2002;23:157–171. doi: 10.1016/s0197-2456(01)00184-2. [DOI] [PubMed] [Google Scholar]
- Seidel MC, Powell RO, Zgibor JC, Siminerio LM, Piatt GA. Translating the Diabetes Prevention Program into an urban medically underserved community: A nonrandomized prospective intervention study. Diabetes Care. 2008;31:684–689. doi: 10.2337/dc07-1869. [DOI] [PubMed] [Google Scholar]
- Sinclair S, Hayes-Reams P, Myers HF, Allen W, Hawes-Dawson J, Kington R. Recruiting African Americans for health studies: Lessons from the Drew-RAND Center on Health and Aging. Journal of Mental Health and Aging. 2000;6:39–51. [Google Scholar]
- Staffileno BA, Coke LA. Recruiting and retaining young, sedentary, hypertension-prone African American women in a physical activity intervention study. Journal of Cardiovascular Nursing. 2006;21:208–216. doi: 10.1097/00005082-200605000-00009. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Grossman M, Bera N, Gillis DE, Sperber N, Castrillo M, et al. Multilevel perspectives on diffusing a physical activity promotion program to reach diverse older adults. Journal of Aging and Physical Activity. 2006;14:270–287. doi: 10.1123/japa.14.3.270. [DOI] [PubMed] [Google Scholar]
- Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. New England Journal of Medicine. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. U.S. Census 2000, summary files 1 and 3, demographic profile 1, 2, 3, and 4, census transportation planning package. 2000. Retrieved September 25, 2010, from http://www.bayareacensus.ca.gov/cities/Berkeley.htm. [Google Scholar]
- U.S. Census Bureau. 2006–2008 American Community Survey 3-year estimates. 2008. Retrieved September 25, 2010, from http://www.bayareacensus.ca.gov/cities/Berkeley.htm. [Google Scholar]
- UyBico SJ, Pavel S, Gross CP. Recruiting vulnerable populations into research: A systematic review of recruitment interventions. Journal of General Internal Medicine. 2007;22:852–863. doi: 10.1007/s11606-007-0126-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren-Findlow J, Prohaska TR, Freedman D. Challenges and opportunities in recruiting and retaining underrepresented populations into health promotion research. The Gerontologist. 2003;43:37–46. doi: 10.1093/geront/43.suppl_1.37. (Special Issue) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annual Review of Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- Zhang P, Engelgau MM, Valdez R, Benjamin SM, Cadwell B, Narayan KM. Costs of screening for pre-diabetes among US adults: A comparison of different screening strategies. Diabetes Care. 2003;26:2536–2542. doi: 10.2337/diacare.26.9.2536. [DOI] [PubMed] [Google Scholar]