Abstract
Background
The accuracy of ectopic pregnancy rates based on nationally representative data has been compromised for many years, impairing surveillance and evaluation of the continued public health importance of this condition.
Purpose
To estimate long-term population-based ectopic pregnancy rates and trends within a defined population over a largely unevaluated time period, including the evaluation of trends in outpatient versus inpatient management and medical versus surgical treatment modalities.
Methods
Using computerized Group Health Cooperative inpatient and outpatient data, age-adjusted and age-specific ectopic pregnancy rates were calculated from 1993 to 2007 among enrollees aged 15–44 years. Overall trends and trends for care setting (inpatient versus outpatient) and treatment modality (medical versus surgical) were also evaluated. Analyses were conducted in 2009.
Results
Between 1993 and 2007, 2114 ectopic pregnancy cases (726 inpatient; 1388 outpatient) were identified among 1 180 070 woman-years, an annual age-adjusted ectopic pregnancy rate of 17.9 per 10 000 woman-years. Rates were stable from 1993 to 2004 and increased in the most recent 3 years (2005–2007, rate = 21.1 per 10 000 woman-years). Rates per 1000 pregnancies increased over the 15-year period from 19.2 to 26.2 per 1000 pregnancies (p-value = 0.001). Inpatient-diagnosed cases decreased from 45.4% in 1993–1995 to 26.9% in 2005–2007 (p-value < 0.0001) and the percentage with surgical treatment decreased from 48.1% to 30.7% (p-value < 0.0001).
Conclusions
The results suggest a trend toward increasing ectopic pregnancy rates over a recent 15-year period. Rates are similar to the last available national estimate suggesting that the significance of ectopic pregnancy as a public health problem has not diminished in these intervening years.
Ectopic pregnancy, the implantation of a fertilized egg outside the uterine corpus, is a serious acute medical condition leading to substantial future reproductive morbidity, including subsequent ectopic pregnancy and infertility. According to national surveillance data from the National Hospital Discharge Survey (NHDS), ectopic pregnancy rates in the U.S. increased nearly fourfold between 1970 and 1989, from 4.2 to 15.5 per 10 000 women/girls aged 15–44 years.1 Although the trend may be partially explained by improved surveillance and sensitivity of diagnostic tests, it parallels increases in sexually transmitted infections such as Chlamydia trachomatis, and increases in other ectopic pregnancy risk factors such as mean maternal age, fertility treatment with ovulation-inducing drugs, and utilization of intrauterine devices.2–5 Reliance on national hospital discharge survey data for estimation of ectopic pregnancy rates was possible historically because virtually all known cases were surgically treated in inpatient settings. However, in the late 1980s medical treatment on an outpatient basis became more commonplace.2 An evaluation of available U.S. sources of incidence data in 1992 concluded that, in light of increasing outpatient treatment, no nationally representative data sources, either alone or in combination, could provide accurate surveillance of ectopic pregnancy occurrence in the U.S. since they capture only inpatient visits.2;6 Thus, the last national estimate of incidence was published over 15 years ago, and the question of whether rates in the U.S. have sustained the peak reached in 1989 remains largely unanswered. As reliance of national surveillance on hospitalization surveys is thought to underestimate true ectopic pregnancy rates, alternative surveillance methods are needed to evaluate recent trends and assess the continued public health importance of this condition. This report presents population-based data on long-term (1993–2007) trends in ectopic pregnancy within a large U.S. health maintenance organization through analyses of data from an extensive set of administrative and clinical data sources.
Methods
Study population
This study was conducted in Group Health Cooperative (GH), a nonprofit, mixed model healthcare system serving over 540 000 residents of Washington State and western Idaho. Utilization data for women/girls aged 15–44 years enrolled in the integrated group practice portion of GH who received their care solely through GH providers and facilities were summarized from January 1, 1993 and December 31, 2007. The study protocol was reviewed and approved by the GH IRB.
Data sources
GH maintains comprehensive computerized clinical and administrative databases. The databases contain health plan enrollment information, inpatient and outpatient clinical visits, external claims and pharmacy records. The inpatient database captures all inpatient hospitalization visits, recording admission and discharge dates as well as up to ten ICD-9 discharge diagnoses and up to ten Current Procedural Terminology (CPT-4) codes. The outpatient database captures all primary care outpatient clinic visits, urgent care visits, and ER visits recording ICD-9 diagnoses and CPT-4 codes. The external claims database captures all outpatient (clinic, urgent care, and ER) and inpatient visits by GH enrollees to non-GH facilities where GH is financially responsible for the care. The pharmacy database captures all medications dispensed to GH enrollees at GH-owned pharmacies. All databases are linked through a unique medical record number assigned to each enrollee, precluding multiple counting of the same health event for individuals across sources.
Ectopic pregnancy case identification
All ectopic pregnancy cases among women aged 15–44 years between January 1, 1993 and December 31, 2007 were identified. An ectopic pregnancy visit was defined as having an ICD-9 code (633, 633.0x–633.9x) assigned to an outpatient visit or a hospitalization, or a procedure code for removal of ectopic fetus in an outpatient setting (CPT-4 code of 59120, 59121, 59130, 59135, 59136, 59140, 59150 or 59151) or inpatient setting (ICD-9 code of 66.0, 66.01, 66.02, 66.62 or 74.3). Multiple ectopic pregnancy visits occurring within a 180-day period were considered to be part of the same episode, with the diagnosis date defined as the date of the first ectopic pregnancy visit in an episode. An episode was classified as inpatient if any visit in the episode occurred in an inpatient setting. To obtain information on medical treatment of ectopic pregnancy, the pharmacy database was used to identify methotrexate dispensed to cases between 7 days before and 180 days after the diagnosis date. An ectopic pregnancy episode was classified as involving a surgical treatment if any procedure code for the removal of an ectopic fetus was found during an episode, regardless of the presence of medical treatment.
Statistical Analysis
Ectopic pregnancy rates were calculated based on two denominators: (1) woman-years or the length of enrollment among women/girls aged 15–44 years during the study period, and (2) number of pregnancies in this group of women during the same time period. Both denominators were stratified by 3–calendar year group and 5-year age group. Pregnancies included all live births, ectopic pregnancies and induced abortions. All databases described for the identification of ectopic pregnancy (inpatient, outpatient, and claims databases) were also used to search for evidence of live births (ICD-9 code of 640.x through 677.x, V22, V23, V27 or V28) and induced abortions (CPT-4 code of 59840, 59841, 59850, 59851, 59852, 59855, 59856 or 59857). Rates per 10 000 woman-years and per 1000 pregnancies were calculated as the number of ectopic pregnancy cases divided by the total woman-years and the total number of pregnancies, respectively.
Poisson regression models adjusting for overdispersion, with calendar-year group (1993–1995, 1996–1998, 1999–2001, 2002–2004, 2005–2007) fitted as a continuous variable, were used to evaluate any linear trends in rates over the study period between 1993 and 2007. Ectopic pregnancy rates and trend tests were calculated for all age groups combined as well as stratified by 5-year age group. In addition, cases with an inpatient diagnosis and surgical treatment over the same time period were evaluated using percentages and time trends.
The age distribution of GH enrollees changed over the 15-year study period. Thus, in addition to the crude ectopic pregnancy rates, age-adjusted rates per 10 000 woman-years and per 1000 pregnancies, standardized to the GH population distribution in year 2000 were calculated.
Results
The number of cases, total woman-years, number of pregnancies, and crude and adjusted ectopic pregnancy rates by 3-year intervals for 1993–2007 are reported in Table 1. Between 1993 and 2007, there were 2114 ectopic pregnancy cases (726 inpatient and 1,388 outpatient) identified among 1 180 070 woman-years, for an annual age-adjusted rate of 17.9 per 10 000 woman-years among women aged 15–44 years. Rates were stable, between 16.6 and 17.8 per 10 000 woman-years, from 1993 to 2004 and then increased in the most recent 3 years to an annual age-adjusted ectopic pregnancy rate of 21.1 per 10 000 woman-years between 2005 and 2007. However, there was not a significant increase in ectopic pregnancy rates over time based on the woman-years denominator (p-value for trend = 0.23). Using the number of pregnancies as the denominator, the age-adjusted rates ranged from 19.2 to 26.2 per 1000 pregnancies and did show a significant increase over time (p-value for trend = 0.001). The percentage of inpatient-diagnosed cases decreased from 45.4% in 1993–1995 to 26.9% in 2005–2007 (p-value for trend < 0.0001). From 1993 to 2007, there was a decrease in surgical treatment from 48.1% in 1993–1995 to 30.7% in the most recent 3 years (p-value for trend < 0.0001).
Table 1.
Ectopic pregnancy rate and treatment setting among women aged 15–44 years, Group Health Cooperative, 1993–2007
| Years | |||||
|---|---|---|---|---|---|
| 1993–1995 | 1996–1998 | 1999–2001 | 2002–2004 | 2005–2007 | |
| Number of ectopic pregnancies (EP) | 476 | 478 | 382 | 354 | 424 |
| Age at EP [M (SD)] | 30.0 (6.5) | 29.3 (6.6) | 29.6 (6.6) | 29.8 (6.7) | 29.4 (6.5) |
| Total woman-years | 273,800 | 266,959 | 230,889 | 211,488 | 196,934 |
| Total number of pregnancies | 26,725 | 24,724 | 19,662 | 17,680 | 17,326 |
| Age at pregnancy [M (SD)] | 28.8 (6.4) | 28.4 (6.4) | 28.7 (6.5) | 29.5 (6.2) | 29.7 (6.1) |
| EP rate (per 10 000 woman-years) | |||||
| Crude rate | 17.4 | 17.9 | 16.6 | 16.8 | 21.5 |
| Age-adjusted rate | 17.1 | 17.8 | 16.6 | 16.7 | 21.1 |
| EP rate (per 1000 pregnancies) | |||||
| EP rate (per 1000 pregnancies) Crude rate* |
17.8 | 19.3 | 19.4 | 20.0 | 24.5 |
| Age-adjusted rate | 19.2 | 20.3 | 19.9 | 22.4 | 26.2 |
| Percentage EP diagnosed in an inpatient setting* | 45.4 | 33.9 | 33.8 | 29.7 | 26.9 |
| Percentage EP with surgical treatment* | 48.1 | 40.2 | 39.5 | 36.2 | 30.7 |
p-value for trend test < 0.05
EP = ectopic pregnancy
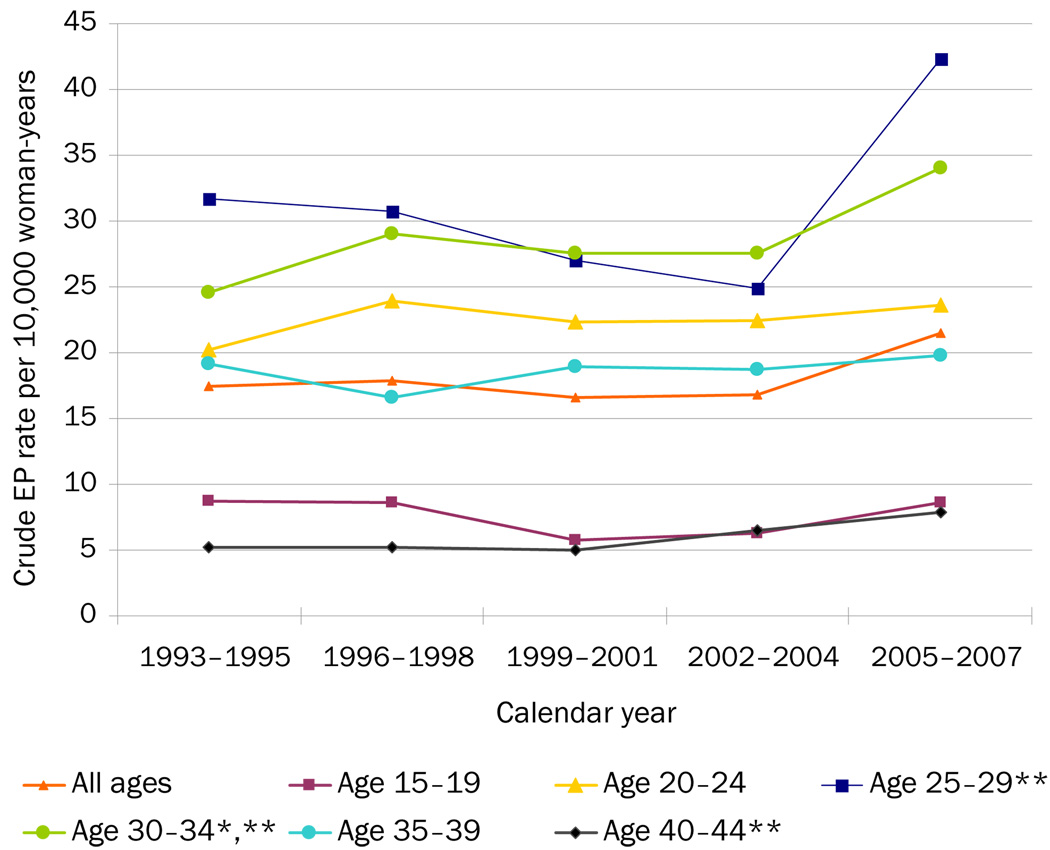
Figure 1 shows the ectopic pregnancy rates per 10 000 woman-years stratified by 5-year age categories. The lowest rates were seen in the youngest (aged 15–19 years) and the oldest (aged 40–44 years) age groups. The rates for those aged 25–29 years and 40–44 years remained relatively constant between 1993 and 2004. In 2005–2007 there was a considerable increase in ectopic pregnancy in these two age groups (p-values comparing 2002–2004 rates with 2005–2007 for those aged 25–29 years and 40–44 years were 0.0018 and < 0.0001, respectively). Over the 15-year time period there was a significant increase in the rate of ectopic pregnancy for those aged 30–34 years (p-value for trend = 0.023), as well as a borderline significant increase in the rate comparing the most recent 3–year calendar time intervals for this age group (p-value = 0.048 for 2002–2004 vs 2005–2007).
Figure 1.
Age-specific EP rates, Group Health Cooperative, 1993–2007
Ages given in years
* p-trend <0.05, p-value to evaluate linear trend of ectopic pregnancy rates from 1993 to 2007 in 3-year intervals
** p-value <0.05 comparing ectopic pregnancy rates in 2002–2004 with rates in 2005–2007 EP, ectopic pregnancy
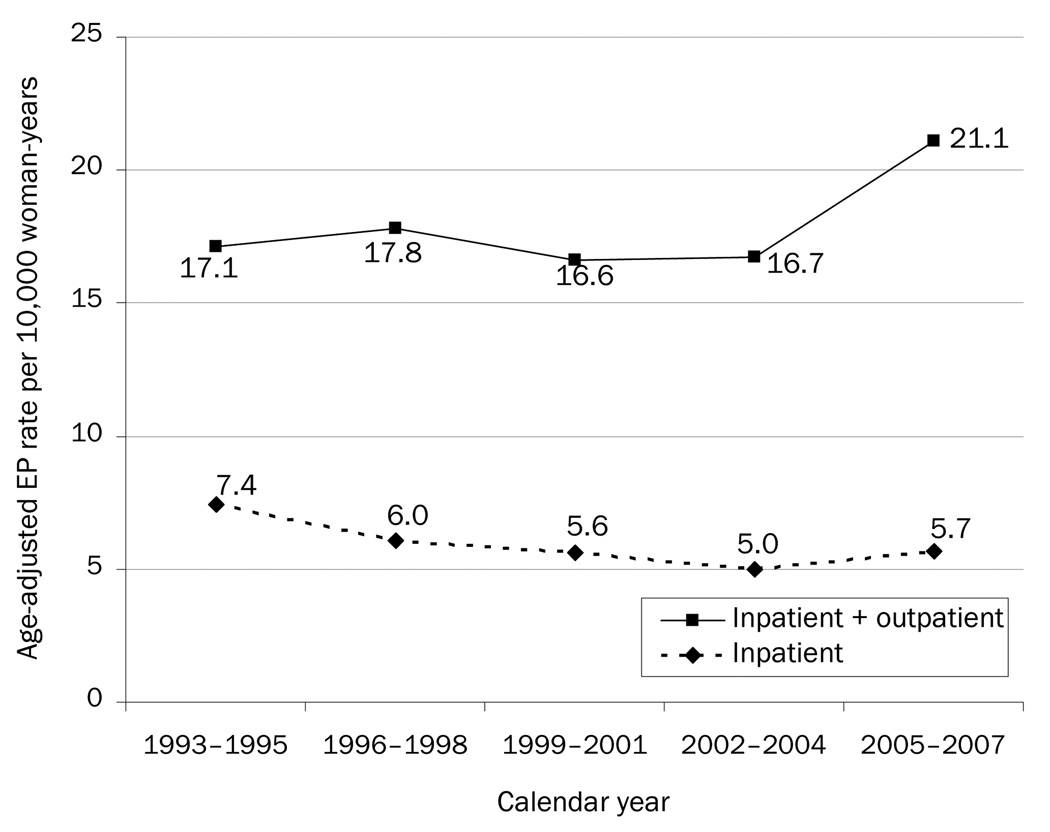
Figure 2 shows the age-adjusted ectopic pregnancy rates per 10 000 woman-years for inpatient setting only and for the combined inpatient and outpatient settings. Although not significant, the rate for cases diagnosed in an inpatient setting decreased over the entire study interval, while the rate for cases diagnosed in both inpatient and outpatient settings remained steady then increased in the most recent 3-year interval.
Figure 2.
Age-adjusted EP rates from inpatient sources and combined inpatient and outpatient sources, Group Health Cooperative, 1993–2007 EP, ectopic pregnancy
Discussion
This study demonstrates a trend of increasing ectopic pregnancy rates over a recent 15-year time period and reports trends toward decreasing inpatient diagnosis as well as surgical treatment. A few recent studies of ectopic pregnancy relying on inpatient data have reported low rates and/or declining secular trends in ectopic pregnancy.7–12 For example, Calderon et al reported an ectopic pregnancy rate in California of 11.2 per 1000 pregnancies during 1991–20007, Sewell et al noted a rate in Maryland of 5.2 per 10 000 women aged 15–44 years between 1994 and 199910, and Stulberg et al. reported a rate of 5.4 per 10 000 women aged 13–50 years utilizing Illinois Hospital Association discharge data from 2000–2006.11
However, by relying on inpatient data sources, these studies may have missed a proportion of cases. Using both inpatient and outpatient ectopic pregnancy occurrences Hoover et al reported a somewhat higher and relatively constant ectopic pregnancy rate of 6.7 per 10 000 women aged 15–44 years between 2002 and 2007 from a large administrative claims database of U.S. commercial health plans.13 In that study a restrictive case definition was used, requiring the presence of both an ectopic pregnancy ICD-9 diagnosis code and a CPT procedure code.13 Because some women diagnosed with ectopic pregnancy receive medical treatment only or are monitored closely without medical or surgical treatment, requiring the presence of a surgical procedure may have resulted in an underestimate of ectopic pregnancy occurrence. Additionally, the population studied—women with commercial insurance—may represent a segment of the reproductive-age population at lower ectopic pregnancy risk.
In another recent population-based study including both inpatient and outpatient cases within a California HMO, Van Den Eeden et al reported ectopic pregnancy rates that were nearly double the estimates from those of Hoover et al (20.7 per 1000 pregnancies and 10.3 per 10 000 women, aged 15–44 years, during 1997–2000).14 The current results from Washington State, similarly using combined inpatient and outpatient sources from a health plan that includes women with Medicaid coverage and a case definition comparable to the surveillance-based CDC case definition, arrived at estimates similar to the Van Den Eeden study for the years these reports overlap.
The importance of including outpatient-diagnosed cases is illustrated in the current study: in Figure 2, analysis of ectopic pregnancy trends based solely on inpatient sources would suggest declining trends over time. However, this reflects a decrease in surgical treatment and not an actual decline in ectopic pregnancy occurrence, as evidenced by the data in the same figure based on combined inpatient and outpatient sources and the data in Table 1 showing the significant decline in the proportion of inpatient-diagnosed cases over the 15-year study period. Rather, the current data suggest a significant increase in ectopic pregnancy for the most recent 3-year interval, based on combined inpatient and outpatient sources (Table 1, Fig. 2).
The diagnosis of ectopic pregnancy has evolved considerably over the past 2 decades. Diagnosis has moved from laparoscopic surgery toward transvaginal ultrasound and serial β-hCG, allowing for medical treatment or, in some circumstances, observation for spontaneous resolution.15–17 This shift from an inpatient to outpatient event has made national surveillance data sources increasingly unreliable. Until 1989, the CDC reported ectopic pregnancy rates based on the NHDS, a sample of inpatient discharges from nonfederal, short-stay hospitals in the U.S.1 In 1992, the CDC reported rates based on the NHDS combined with data from the National Hospital Ambulatory Medical Care Survey (NHAMCS), a national probability sample of visits to the emergency and outpatient departments of hospitals with the same characteristics as those sampled in the NHDS.2 The calculated rate was still higher than in 1989 (19.7 per 1000 pregnancies), but surveillance combining both of these data sources could also introduce inaccuracies in two ways that cannot be corrected. First, the same ectopic pregnancy occurrence may be captured by both surveys, which could result in an overestimate of the true incidence of ectopic pregnancy. Second, neither survey includes patients examined and treated exclusively in physicians’ offices, which could result in an underestimate of the true incidence.
The ectopic pregnancy trends for a recent 15-year interval reported in the current study utilized multiple administrative databases from a managed care system with a defined population that includes enrolled women with Medicaid coverage. The use of the unique enrollee medical record number for linked data sources and a defined ectopic pregnancy episode captured diagnoses and treatment in all medical settings, and greatly reduced any chance of double counting of cases. Moreover, the trends were tracked in the same enrollee population (GH enrollees) using a consistent case definition over all years. The results are based on regional data and may not be directly representative of a national population sample. With the exception of age, the demographic composition of the GH population has remained stable over the time frame of interest and is generally representative of the surrounding community. The racial distribution in the age range of interest (aged 15–44 years) is 78%–82% white, generally similar to the community served by GH (76% white)18, and not dissimilar from women aged 15–44 years in the U.S. (72% white).19 Further, the GH rate estimates are similar to another population-based sample14, providing additional reassurance that the results are likely to generalize more broadly.
Results of this study provide evidence that ectopic pregnancy rates have not declined in the ensuing 15 years since the last U.S. national report and that its significance as a public health problem has not diminished. The decreases in inpatient and surgical treatment of ectopic pregnancy suggest the possible limitations of relying solely on those sources for rate and trend data. These results also suggest a potential role for large U.S. healthcare systems with well-defined populations and comprehensive databases in ongoing surveillance.
Acknowledgements
This work was supported by grants numbered R03 HD052687 (PI: Scholes, D.) and T32 HD052462 (PI: Williams, M.) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), NIH.
The authors gratefully acknowledge the contributions to the project by Jane Grafton, Patricia Yarbro, Linda Wehnes and Mary Sunderland.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Trends in ectopic pregnancies: U.S. 1970 to 1985. Stat Bull Metrop Insur Co. 1987;68(3):24–30. [PubMed] [Google Scholar]
- 2.Ectopic pregnancy—U.S., 1990–1992. MMWR Morb Mortal Wkly Rep. 1995;44(3):46–48. [PubMed] [Google Scholar]
- 3.Egger M, Low N, Smith GD, Lindblom B, Herrmann B. Screening for chlamydial infections and the risk of ectopic pregnancy in a county in Sweden: ecological analysis. BMJ. 1998;316(7147):1776–1780. doi: 10.1136/bmj.316.7147.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farquhar CM. Ectopic pregnancy. Lancet. 2005;366(9485):583–591. doi: 10.1016/S0140-6736(05)67103-6. [DOI] [PubMed] [Google Scholar]
- 5.Kamwendo F, Forslin L, Bodin L, Danielsson D. Epidemiology of ectopic pregnancy during a 28 year period and the role of pelvic inflammatory disease. Sex Transm Infect. 2000;76(1):28–32. doi: 10.1136/sti.76.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zane SB, Kieke BA, Jr, Kendrick JS, Bruce C. Surveillance in a time of changing health care practices: estimating ectopic pregnancy incidence in the U.S. Matern Child Health J. 2002;6(4):227–236. doi: 10.1023/a:1021106032198. [DOI] [PubMed] [Google Scholar]
- 7.Calderon JL, Shaheen M, Pan D, Teklehaimenot S, Robinson PL, Baker RS. Multi-cultural surveillance for ectopic pregnancy: California 1991–2000. Ethn Dis. 2005;15(4 Suppl 5):S5–S4. [PubMed] [Google Scholar]
- 8.Coste J, Bouyer J, Germain E, Ughetto S, Pouly JL, Job-Spira N. Recent declining trend in ectopic pregnancy in France: evidence of two clinicoepidemiologic entities. Fertil Steril. 2000;74(5):881–886. doi: 10.1016/s0015-0282(00)01535-1. [DOI] [PubMed] [Google Scholar]
- 9.Irvine LM, Setchell ME. Declining incidence of ectopic pregnancy in a UK city health district between 1990 and 1999. Hum Reprod. 2001;16(10):2230–2234. doi: 10.1093/humrep/16.10.2230. [DOI] [PubMed] [Google Scholar]
- 10.Sewell CA, Cundiff GW. Trends for inpatient treatment of tubal pregnancy in Maryland. Am J Obstet Gynecol. 2002;186(3):404–408. doi: 10.1067/mob.2002.121623. [DOI] [PubMed] [Google Scholar]
- 11.Stulberg DB, Zhang JX, Lindau ST. Socioeconomic Disparities in Ectopic Pregnancy: Predictors of Adverse Outcomes from Illinois Hospital-Based Care, 2000–2006. Matern Child Health J. 2010 doi: 10.1007/s10995-010-0579-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mol F, van Mello NM, Mol BW, van der Veen F, Ankum WM, Hajenius PJ. Ectopic pregnancy and pelvic inflammatory disease: A renewed epidemic? Eur J Obstet Gynecol Reprod Biol. 2010 doi: 10.1016/j.ejogrb.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Hoover KW, Tao G, Kent CK. Trends in the diagnosis and treatment of ectopic pregnancy in the U.S. Obstet Gynecol. 2010;115(3):495–502. doi: 10.1097/AOG.0b013e3181d0c328. [DOI] [PubMed] [Google Scholar]
- 14.Van Den Eeden SK, Shan J, Bruce C, Glasser M. Ectopic pregnancy rate and treatment utilization in a large managed care organization. Obstet Gynecol. 2005;105(5 Pt 1):1052–1057. doi: 10.1097/01.AOG.0000158860.26939.2d. [DOI] [PubMed] [Google Scholar]
- 15.Bouyer J, Job-Spira N, Pouly JL, Coste J, Germain E, Fernandez H. Fertility following radical, conservative-surgical or medical treatment for tubal pregnancy: a population-based study. BJOG. 2000;107(6):714–721. doi: 10.1111/j.1471-0528.2000.tb13330.x. [DOI] [PubMed] [Google Scholar]
- 16.Hidlebaugh D, O'Mara P. Clinical and financial analyses of ectopic pregnancy management at a large health plan. J Am Assoc Gynecol Laparosc. 1997;4(2):207–213. doi: 10.1016/s1074-3804(97)80011-4. [DOI] [PubMed] [Google Scholar]
- 17.Luciano AA, Roy G, Solima E. Ectopic pregnancy from surgical emergency to medical management. Ann N Y Acad Sci. 2001;943:235–254. doi: 10.1111/j.1749-6632.2001.tb03805.x. [DOI] [PubMed] [Google Scholar]
- 18.Saunders KW, Davis RL, Stergachis A. Group Health Cooperative. In: Strom BL, Pepper GS, editors. Pharmacoepidemiology. England: John Wiley & Sons, Ltd.; 2005. pp. 223–239. [Google Scholar]
- 19. [accessed July 2010];U.S. Department of Commerce, U.S. Census Bureau Population Division. Census Population 1970–2000 for Public Health Research, CDC WONDER On-line Database. 2005 June; wonder.cdc.gov/.