Abstract
Objectives. We examined the link between incarceration and sexually transmitted infection (STI), including HIV, from a social network perspective.
Methods. We used data collected during a social network study conducted in Brooklyn, NY (n = 343), to measure associations between incarceration and infection with herpes simplex virus-2, chlamydia, gonorrhea, and syphilis or HIV and sex with an infected partner, adjusting for characteristics of respondents and their sex partners.
Results. Infection with an STI or HIV was associated with incarceration of less than 1 year (adjusted prevalence ratio [PR] = 1.33; 95% confidence interval [CI] = 1.01, 1.76) and 1 year or longer (adjusted PR = 1.37; 95% CI = 1.08, 1.74). Sex in the past 3 months with an infected partner was associated with sex in the past 3 months with 1 partner (adjusted PR = 1.42; 95% CI = 1.12, 1.79) and with 2 or more partners (adjusted PR = 1.85; 95% CI = 1.43, 2.38) who had ever been incarcerated.
Conclusions. The results highlight the need for STI and HIV treatment and prevention for current and former prisoners and provide preliminary evidence to suggest that incarceration may influence STI and HIV, possibly because incarceration increases the risk of sex with infected partners.
Jail and prison inmates face a high risk of infectious disease.1,2 Inmates experience a disproportionate burden of sexually transmitted infections (STIs),3–8 including 4 to 5 times the prevalence of HIV than that observed in the general population.9,10 HIV infection also is elevated among individuals whose recent sex partners have been incarcerated.11 Although numerous surveys among jail and prison inmates document high infection levels among incarcerated populations, few studies have assessed whether personal history of incarceration or incarceration of a sex partner is associated with STI or HIV infection independent of adverse background factors such as poverty and substance use.
The association between personal and partner incarceration and infection with an STI or HIV may exist in part because incarceration may contribute to the drug and sexual risk behaviors that drive transmission of STIs and HIV. Personal and sex partner incarceration are independent correlates of new, multiple, and concurrent sex partnerships and transactional sex and hence may contribute to these risk behaviors.12–20 Incarceration may contribute to high-risk sex partnerships because incarceration is a disruptive life event that destabilizes social and sexual networks.21–25 Extant literature suggests that 50% to 80% of inmates are in committed relationships at the time of their incarceration26–28 and that a substantial proportion of these relationships end during incarceration.27 Since being in a committed relationship protects against sexual risk-taking,29,30 dissolution of such relationships during incarceration may contribute to new and multiple partnerships among partners of inmates during the incarceration, among inmates during the incarceration, and among former inmates during the period of reentry. Furthermore, disruption of relationships during incarceration weakens social cohesion and support networks. Reduced social support inhibits the ability of inmates and their partners to cope during the stressful periods of incarceration and reentry, which may result in known determinants of STI risk, such as diminished mental health (i.e., depression, anxiety), increased self-medication with drugs, and elevated levels of sex partnerships.31
In addition to the growing body of evidence supporting the hypothesis that incarceration promotes sexual risk behaviors, researchers have also hypothesized that incarceration may influence transmission of STI and HIV by increasing involvement in high-risk social and sexual networks—both during and after periods of incarceration. Evidence shows that incarceration introduces inmates into high-risk networks characterized by high levels of drug trade and use (i.e., gangs),32,33 in which sexual risk-taking and infection levels may be elevated. Involvement in these networks may increase the risk of sex with an infected partner34–36 and STI or HIV transmission. To our knowledge, no prior study has examined the link between prior incarceration and sex with partners infected with an STI or HIV (hereafter “infected partners”), probably because of the limited availability of data sources that provide information on incarceration and biologically confirmed STI and HIV infection (i.e., confirmation of infection status by STI and HIV testing, as opposed to self-reported infection status) for respondents and their sex partners.
Sexual network studies in which incarceration experience is assessed and STI and HIV testing is conducted provide data that enable assessment of whether prior incarceration is an independent correlate of biologically confirmed STI or HIV among former prisoners and their partners. Such data also allow preliminary assessment of the hypothesis that incarceration may lead to infection not only via increased levels of sexual risk behavior but also via increased exposure to infected partners. Given the high and growing incarceration rate in the United States, such data should be used to assess relationships among incarceration, sex with infected partners, and STI or HIV infection. Another benefit of an investigation of incarceration and STI or HIV using social network data is the ability to visualize and describe the degree to which incarceration-related STI or HIV transmission may affect former inmates, their partners, and other members of their sexual networks.
We examined links between incarceration and infection with an STI or HIV using data collected during the Networks, Norms and HIV Risk Among Youth (NNAHRAY) Study,34,37 a social network study conducted in Bushwick, Brooklyn38–40 that collected data on incarceration and biologically confirmed STI and HIV infection. We measured the association between incarceration variables (respondent history of incarceration and sex partner incarceration) and infection with an STI or HIV. To examine whether incarceration may contribute to sex with infected partners, we also measured the association between incarceration variables and sex with an infected partner.
METHODS
Recruitment for the NNAHRAY study has been described previously.34,37 Between 2002 and 2004, a total of 465 adults aged 18 years or older were recruited, including 112 index cases and 353 identified risk contacts. Index cases were recruited from 3 sources of Bushwick residents, comprising 1 population-representative sample and 2 nonrepresentative samples. The population-representative sample of index cases were 66 individuals aged 18 to 30 years, recruited door-to-door within randomly selected blocks. Of these, 25 had been included in a population-representative sample of Bushwick youth during a previous study40 and 41 were members of households targeted during that study who were too young to participate at that time, but who were aged 18 years or older during the NNAHRAY study. In addition, a convenience sample of injection drug user (IDU) index cases was recruited (n = 38), including members of a population of IDUs specifically targeted during that earlier study, walk-ins who met study criteria, and those recruited by project staff in known drug-purchasing venues, at shooting galleries, or at needle exchanges in Bushwick. IDUs had to have injected drugs within the prior 3 months and have visible track marks or provide other evidence of current injection during detailed verbal questioning. Finally, a convenience sample of individuals involved in a group sex party culture were recruited as index cases (n = 8).
Each index case was asked to identify and provide locator information for risk contacts, including: (1) sex partners in the past 3 months (≤ 10 partners); (2) partners with whom the respondent injected drugs in the past 3 months, even if syringes or equipment were not shared (≤ 5 IDU partners); or (3) a person with whom the respondent attended a group sex event in the past 3 months (≤ 8 contacts). A total of 3 waves of network tracing were performed to obtain the sample of risk contacts. Risk contacts were identified and recruited in 1 of 3 ways: participants brought in their contacts to be interviewed, participants gave their risk contact a coupon to be redeemed, or study staff located and directly recruited the risk contact. A total of 353 additional participants who were directly or indirectly linked to 1 or more of the 112 index cases were recruited.
Eligible participants who were successfully located by NNAHRAY staff and who provided written informed consent were enrolled. Staff administered a 1-hour structured face-to-face sexual behavior and drug use survey that assessed sociodemographic characteristics, drug use, sexual and drug risk behaviors, size and composition of sexual and drug networks, perceived levels of social support and burden, experiences with discrimination, peer norms, participants' own norms, measures of community activism, and measures of health activism. After the completion of the survey, staff collected 10 ml of blood and 10 ml of urine for STI and HIV testing and provided a cash incentive ($20 for the interview, $10 for blood sample, and $10 for urine sample). As described previously,37 a venous blood sample was tested for HIV with an enzyme-linked immunosorbent assay (ELISA; Abbott Laboratories, Abbott Park, IL) and a Western blot (BioRad Laboratories, Hercules, CA), for herpes simplex virus-2 (HSV-2) with a type-specific ELISA (HerpeSelect, Focus Technologies, Cypress, CA), and for syphilis with a rapid plasma reagin test (Wampole Laboratories, Princeton, NJ) confirmed by a Treponema pallidum particle agglutination antibody assay (Serodia, Fujirebio Diagnostics, Malvern, PA). Urine was tested for chlamydia and gonorrhea with a nucleic acid amplification test (BDProbeTec ET Chlamydia trachomatis/Neisseria gonorrhoeae Amplified DNA Assays, BD Diagnostic Systems, Sparks, MD).
Because we examined respondent incarceration history and sex partner incarceration as explanatory factors of respondent and sex partner infection with an STI or HIV, the analytic sample was restricted to respondents involved in at least 1 sex partnership in the past 3 months for which interview data for both members of the partnership were available (n = 343 participants).
Because each of these 343 individuals was a participant in the NNAHRAY study, each responded to the structured face-to-face sexual behavior and drug use survey and was offered STI and HIV testing. Responses to the survey were used to create indicators of sex partners' sociodemographic and behavioral characteristics, and biologically confirmed STI and HIV infection data were used to code indicators of sex partners' infection with an STI or HIV.
Measures
Respondent incarceration.
Respondents were asked if they had ever been sentenced to jail or prison, and if yes, the cumulative number of months they spent in jail or prison during their lifetime. On the basis of this measure, we coded a 3-level variable measuring the duration of time the respondent had ever been incarcerated (never in lifetime, less than 1 year, or 1 year or more).
Sex partner incarceration.
Respondents were linked to partners who they named or who had named them. Sex partners were interviewed and self-reported whether they had ever been sentenced to jail or prison. On the basis of this measure, we coded a 3-level variable measuring the number of sex partners with a history of incarceration that each respondent had had in the past 3 months (0, 1, or 2 or more recent partners with a history of incarceration).
Outcomes.
We examined 2 dichotomous indicators of STI or HIV risk. Current STI or HIV was defined as biologically confirmed infection with HSV-2, chlamydia, gonorrhea, syphilis, or HIV (yes vs no). Recent sex with an infected partner was defined as having had at least 1 sex partner in the past 3 months who tested positive for HSV-2, chlamydia, gonorrhea, syphilis, or HIV (yes vs no).
Covariates.
We evaluated gender as a potential effect measure moderator in models that included no additional covariates. We included the following covariates in adjusted models, identified as potential confounding variables on the basis of prior research and conceptual models: respondent's sociodemographic characteristics (age ≥ 25 years, Black race, less than high school education, current unemployment), respondent's drug use history (ever used crack, cocaine, or heroin; ever used injection drugs), respondent's same-sex partnership history, and characteristics of respondent's recent sex partners (had at least 1 sex partner in the past 3 months who was aged ≥ 25 years; was currently unemployed; had ever used crack, cocaine, or heroin; had ever used injection drugs; or had a history of same-sex partnerships).
Data Analysis
We performed analyses in Stata, version 10.0 (StataCorp LP, College Station, TX). We examined bivariable relationships between the sociodemographic and behavioral characteristics of respondents by status of infection with STI or HIV, calculating prevalence ratios and 95% confidence intervals for the associations between respondent characteristics and STI or HIV using a generalized linear model with probability weights, log link, Poisson distribution without an offset, and a robust variance estimator.41–43
Using the same regression methods, we estimated unadjusted and adjusted prevalence ratios and 95% confidence intervals for the associations between incarceration and STI or HIV infection and sex with infected partners.
For each analysis, we tested a gender-by-incarceration product-interaction term in the crude model to evaluate whether associations differed significantly by gender (P < .15 level). Because no associations differed significantly by gender, we aggregated men and women in all analyses. All fully adjusted models included respondent and sex partner control variables.
We used UCINET (Version V for Windows, Analytic Technologies, Natick, MA) to construct a diagram of risk contacts among study respondents and describe the distribution of incarceration and infection with HSV-2 or HIV (the 2 most common STIs in the sample) within the network structure. To best illustrate the implications for incarceration-related STI or HIV transmission through the network, the diagram presents members of the network who are linked by recent sex or drug use, given that HIV is transmitted through sexual and drug-using routes.
RESULTS
Of the 465 individuals who participated in the NNAHRAY study, a total of 343 had at least 1 sex partner who was recruited and who also participated in the NNAHRAY study. Among the 343 individuals involved in at least 1 sex partnership, a total of 296 sex partnerships occurred for which we had interview data for both members. Most (68%) of the 343 respondents had had 1 partnership in the past 3 months, 22% had had 2 partnerships, 7% had had 3 partnerships, and small percentages reported 4 to 8 partnersips.
Of the 343 individuals included in the analytic sample, a little more than half (53%) were male, approximately 70% were Latino, and 21% were Black. The mean age was 31 years (33 years among men, 27 years among women), 44% had less than a high school education, and 80% reported being unemployed at the time of the interview (Table 1). Nearly three quarters (73%) had ever used noninjected crack, cocaine, or heroin; 38% had ever used injection drugs, all of whom had also used noninjected drugs. Nearly one third of men reported ever having had at least 1 male sex partner, and 43% of women reported ever having had at least 1 female sex partner.
TABLE 1.
Characteristics and Sexually Transmitted Infection (STI) or HIV Among Respondents Aged 18 to 60 Years Involved in at Least 1 Sex Partnership in the Past 3 Months: Networks, Norms and HIV Risk Among Youth Study, Brooklyn, NY, 2002–2004
| Participant Characteristics | No. of Participants (%)a | % With STI or HIV | Unadjusted PR (95% CI) |
| Gender | |||
| Men (Ref) | 182 (53.1) | 49.4 | 1.00 |
| Women | 161 (46.9) | 64.1 | 1.29 (1.06, 1.59) |
| Race | |||
| Latino (Ref) | 239 (69.7) | 51.9 | 1.00 |
| Black | 72 (21.0) | 70.2 | 1.35 (1.10, 1.66) |
| White | 22 (6.4) | 50.0 | 0.96 (0.61, 1.52) |
| Other | 10 (2.91) | 70.0 | 1.35 (0.88, 2.07) |
| Age, y | |||
| 18–24 (Ref) | 12 (35.0) | 37.2 | 1.00 |
| 25–29 | 61 (17.8) | 67.9 | 1.83 (1.35, 2.48) |
| 30–34 | 39 (11.4) | 58.8 | 1.58 (1.09, 2.29) |
| 35–39 | 48 (14.0) | 70.0 | 1.88 (1.38, 2.58) |
| ≥40 | 75 (21.9) | 71.4 | 1.92 (1.44, 2.56) |
| Less than high school education | |||
| No (Ref) | 151 (44.0) | 57.0 | 1.00 |
| Yes | 150 (43.7) | 60.3 | 1.06 (0.86, 1.29) |
| Currently unemployed | |||
| No (Ref) | 68 (19.8) | 47.5 | 1.00 |
| Yes | 275 (80.2) | 58.6 | 1.23 (0.93, 1.65) |
| Ever used noninjected crack, cocaine, or heroin | |||
| No (Ref) | 86 (25.1) | 32.1 | 1.00 |
| Yes | 249 (72.6) | 64.8 | 2.02 (1.44, 2.84) |
| Ever used injection drugs | |||
| No (Ref) | 214 (62.4) | 51.5 | 1.00 |
| Yes | 129 (37.6) | 65.4 | 1.27 (1.05, 1.54) |
| Men who ever had sex with a man | |||
| No (Ref) | 123 (67.6) | 38.1 | 1.00 |
| Yes | 59 (32.4) | 71.7 | 1.88 (1.40, 2.53) |
| Women who ever had sex with a woman | |||
| No (Ref) | 92 (57.1) | 58.0 | 1.00 |
| Yes | 69 (42.9) | 71.9 | 1.23 (0.97, 1.58) |
| ≥ 2 sex partnerships in past 3 mo | |||
| No (Ref) | 173 (50.4) | 49.7 | 1.00 |
| Yes | 170 (49.6) | 63.2 | 1.27 (1.04, 1.56) |
Note. CI = confidence interval; PR = prevalence ratio. Sample size was n = 343. A total of 56% of the analytic sample tested positive for an STI (herpes simplex virus-2, chlamydia, gonorrhea, syphilis) or HIV.
Percentages may not sum to 100% because of missing values or rounding.
Incarceration, Sex With Infected Partners, and Personal Infection
Among those included in the analytic sample, approximately 45% had ever been incarcerated (27% of women, 62% of men), including 13% who had been incarcerated for a cumulative total of less than 1 year and 33% who had been incarcerated for 1 year or more. Approximately 55% had had sex in the past 3 months with a partner who had ever been incarcerated (69% of women, 43% of men), including 43% who had had 1 partner with an incarceration history and 13% who had had 2 or more partners with an incarceration history.
Fifty-six percent of respondents were STI or HIV infected. The most common infection was HSV-2 (50%), followed by HIV (11%), chlamydia (6%), syphilis (3%), and gonorrhea (1%). Fifty-seven percent of respondents had had sex in the past 3 months with an infected partner.
Infection by Respondent Characteristics
Infection with an STI or HIV was more common among women than among men (prevalence ratio [PR] = 1.29; 95% confidence interval [CI] = 1.06, 1.59) and among Blacks than among Latinos (PR = 1.35; 95% CI = 1.10, 1.66; Table 1). Those aged 25 years or older were 1.5 to 2 times more likely to be infected than those aged 18 to 24 years. Infection with an STI or HIV was strongly associated with noninjection drug use (PR = 2.02; 95% CI = 1.44, 2.84) and was weakly associated with injection drug use (PR = 1.27; 95% CI = 1.05, 1.54). History of same-sex partnerships was strongly associated with infection among men (PR = 1.88; 95% CI = 1.40, 2.53) and was weakly associated with infection among women (PR = 1.23; 95% CI = 0.97, 1.58).
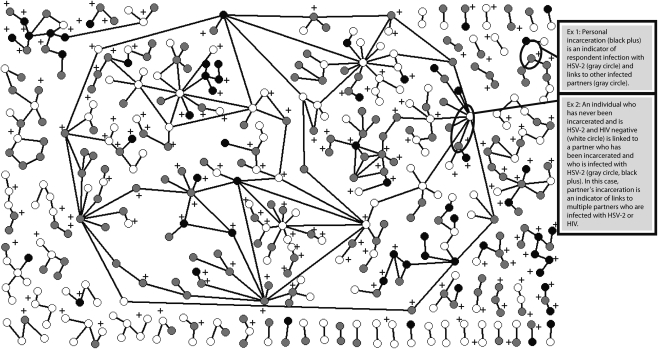
Distribution of Incarceration and Sexually Transmitted Infection
Figure 1 displays the locations of participants in the social network. The diagram illustrates that incarceration history (plus signs) and infection with either HSV-2 or HIV (gray circles) or with both HSV-2 and HIV (black circles) were common, and that respondent and partner incarceration were correlated with HSV-2 or HIV infection. Many NNAHRAY participants with an incarceration history were HSV-2 or HIV infected or were connected to sexual or drug-using contacts who were HSV-2 or HIV infected.
FIGURE 1.
Distribution of incarceration and herpes simplex virus-2 (HSV-2) and HIV infection among sexual or drug-using partners: Networks, Norms and HIV Risk Among Youth Study, Brooklyn, NY, 2002–2004.
Note. Incarceration is indicated by a black plus sign. A white circle indicates no infection with HSV-2 or HIV, a gray circle indicates HSV-2 or HIV infection, and a black circle indicates HSV-2–HIV coinfection.
Example 1 illustrates a case in which respondent incarceration (black plus) is an indicator of respondent infection with HSV-2 (gray circle) as well as an indicator of being linked to 2 infected partners. The diagram also indicates that respondents who had recent sexual or drug-using contacts with an incarceration history were likely to be HSV-2 or HIV infected or were connected to a contact who was HSV-2 or HIV infected.
Example 2 highlights the link between partner incarceration and infection. In this case, an individual who had never been incarcerated and who was HSV-2 and HIV negative (white circle) was linked to a partner who had been incarcerated and who was infected with HSV-2 (gray circle, black plus). This individual also was linked to multiple other partners, many of whom were HSV-2 or HIV infected.
The diagram indicates a high level of connectivity among network members. There is a very large connected component comprising 206 participants and smaller components of 22, 15, 13, and 8 members; in addition, there are 2 components of 7 members each, 1 of 6 members, 6 of 5 members, 3 of 4 members, 10 of 3 members, and 28 of 2 members. The diagram suggests that if incarceration contributes to STI or HIV transmission, effects of incarceration on infection risk have the potential to be rapidly and widely disseminated through the network.
Associations Between Incarceration and Infection
Respondent incarceration.
Participants who had a history of incarceration and who had spent less than 1 year in jail or prison were more likely to be infected with an STI or HIV than those with no history of incarceration (PR = 1.52; 95% CI = 1.18, 1.97; Table 2). In analyses adjusting for respondent and sex partner sociodemographic characteristics, substance use history, and history of same-sex partnership, the association between incarceration of less than 1 year and STI or HIV infection weakened but remained (adjusted PR = 1.33; 95% CI = 1.01, 1.76).
TABLE 2.
Associations Between Respondent and Sex Partner Incarceration and Sexually Transmitted Infection (STI) or HIV: Networks, Norms and HIV Risk Among Youth Study, Brooklyn, NY, 2002–2004
| Respondent Currently Infected With STI or HIV | |||
| Incarceration | No. (%) | Unadjusted PR (95% CI) | Adjusteda PR (95% CI) |
| Cumulative duration of respondent's incarceration in lifetime | |||
| Never (Ref; n = 168) | 78 (46.4) | 1.00 | 1.00 |
| < 1 y (n = 41) | 29 (70.7) | 1.52 (1.18, 1.97) | 1.33 (1.01, 1.76) |
| ≥ 1 y (n = 94) | 64 (68.1) | 1.47 (1.18, 1.82) | 1.37 (1.08, 1.74) |
| No. of respondent's sex partners in past 3 mo who had a history of incarceration | |||
| 0 (Ref; n = 131) | 57 (43.5) | 1.00 | 1.00 |
| 1 (n = 130) | 77 (59.2) | 1.36 (1.07, 1.73) | 1.09 (0.84, 1.41) |
| ≥ 2 (n = 42) | 37 (88.1) | 2.02 (1.62, 2.54) | 1.23 (0.92, 1.64) |
Note. CI = confidence interval; PR = prevalence ratio. A total of 303 participants had nonmissing values for all STI and HIV outcomes (herpes simplex virus-2, chlamydia, gonorrhea, syphilis, HIV) and were included in the analysis.
Adjusted for respondent's sociodemographic characteristics (age ≥ 25 years, Black, less than high school education, currently unemployed), respondent's drug use history (ever used crack, cocaine, or heroin; ever used injection drugs), respondent's same-sex partnership history, and characteristics of respondent's recent sex partners (had at least 1 sex partner in the past 3 months who was aged ≥ 25 years; was currently unemployed; had ever used crack, cocaine, or heroin; had ever used injection drugs; or had a history of same-sex partnerships).
Incarceration of 1 year or more was associated with STI or HIV infection in both unadjusted analyses (PR = 1.47; 95% CI = 1.18, 1.82) and analyses adjusting for respondent and partner characteristics (PR = 1.37; 95% CI = 1.08, 1.74).
Sex partner incarceration.
Those who had 1 sex partner in the past 3 months who had ever been incarcerated were more likely to be STI or HIV infected than those whose recent partners had not been incarcerated (PR = 1.36; 95% CI = 1.07, 1.73; Table 2). In analyses adjusting for sociodemographic and behavioral variables, the prevalence ratio was attenuated to 1.09 (95% CI = 0.84, 1.41). The change in estimate primarily was caused by adjustment for respondent gender, race, and noninjection drug use.
Having 2 or more sex partners in the past 3 months with a history of incarceration was strongly associated with STI or HIV infection (PR = 2.02; 95% CI = 1.62, 2.54). When we adjusted for respondent and partner variables, the association weakened considerably and was no longer statistically significant (adjusted PR = 1.23; 95% CI = 0.92, 1.64). The estimate was largely confounded by gender, age, race, noninjection drug use, and same-sex partnership history.
Associations Between Incarceration and Sex With an Infected Partner
Respondent incarceration.
Those who had been incarcerated for less than 1 year were more likely to have had sex in the past 3 months with an infected partner than those with no prior history of incarceration (adjusted PR = 1.36; 95% CI = 1.10, 1.70; Table 3). In analyses adjusting for respondent and sex partner characteristics, incarceration of less than 1 year remained associated with having an infected sex partner (adjusted PR = 1.25; 95% CI = 1.01, 1.54).
TABLE 3.
Associations Between Respondent and Sex Partner Incarceration and Sex With a Partner Infected With a Sexually Transmitted Infection (STI) or HIV: Networks, Norms and HIV Risk Among Youth Study, Brooklyn, NY, 2002–2004
| Respondent Had ≥ 1 Sex Partner in Past 3 Months Who Was Infected With STI or HIV | |||
| Incarceration | No. (%) | Unadjusted PR (95% CI) | Adjusteda PR (95% CI) |
| Cumulative duration of respondent's incarceration in lifetime | |||
| Never (Ref; n = 187) | 102 (54.6) | 1.00 | 1.00 |
| < 1 y (n = 43) | 32 (74.4) | 1.36 (1.10, 1.70) | 1.25 (1.01, 1.54) |
| ≥ 1 y (n = 113) | 78 (69.0) | 1.27 (1.06, 1.52) | 0.97 (0.79, 1.18) |
| No. of respondent's sex partners in past 3 mo who had a history of incarceration | |||
| 0 (Ref; n = 153) | 70 (45.8) | 1.00 | 1.00 |
| 1 (n = 146) | 100 (68.5) | 1.50 (1.22, 1.84) | 1.42 (1.12, 1.79) |
| ≥ 2 (n = 44) | 42 (95.5) | 2.09 (1.73, 2.51) | 1.85 (1.43, 2.38) |
Note. CI = confidence interval; PR = prevalence ratio. Sample size was n = 343.
Adjusted for respondent's sociodemographic characteristics (age ≥ 25 years, Black race, less than high school education, current unemployment), respondent's drug use history (ever used crack, cocaine, or heroin; ever used injection drugs), respondent's same-sex partnership history, and characteristics of respondent's recent sex partners (had at least 1 sex partner in the past 3 months who was aged ≥ 25 years; was currently unemployed; had ever used crack, cocaine, or heroin; had ever used injection drugs; or had a history of same-sex partnerships).
Those who had been incarcerated for 1 year or longer were more likely than those with no incarceration history to have had sex in the past 3 months with an infected partner (PR = 1.27; 95% CI = 1.06, 1.52). In adjusted analyses, the prevalence ratio was attenuated to 0.97 (95% CI = 0.79, 1.18). The estimate primarily was confounded by respondent age, race, and noninjection drug use.
Sex partner incarceration.
Those who had 1 sex partner in the past 3 months with an incarceration history were more likely than those whose recent partners had not been incarcerated to have had sex in the past 3 months with an infected partner (PR = 1.50; 95% CI = 1.22, 1.84; Table 3). In adjusted analyses, partner incarceration history remained an independent correlate of recent sex with an infected partner (adjusted PR = 1.42; 95% CI = 1.12, 1.79).
Having 2 or more recent partners who had ever been incarcerated was strongly associated with sex in the past 3 months with an infected partner in both unadjusted analyses (PR = 2.09; 95% CI = 1.73, 2.51) and adjusted analyses (adjusted PR = 1.85; 95% CI = 1.43, 2.38).
The association between partner incarceration and sex with an infected partner was largely a result of the correlation between incarceration history and infection with an STI or HIV among partners; the majority of respondents' partners who had been incarcerated also were infected with at least 1 STI or HIV. However, many of those who had at least 1 recent partner who was a former inmate also were likely to have had additional partners who had not been incarcerated but who were infected.
DISCUSSION
Incarceration was widespread in the NNAHRAY network. Forty percent of respondents had a history of incarceration, and more than half had a recent sex partner who had been incarcerated. Infection with an STI or HIV also was highly prevalent and disproportionately affected former inmates and their sex partners, highlighting the need for improved testing, treatment, and prevention education among current and former prisoners and members of their sexual networks. These results underscore the importance of correctional facility settings as priority venues for STI prevention interventions and highlight the urgent need for the development of community-based interventions for those affected by incarceration.2,44
In analyses adjusting for an extensive list of covariables, personal incarceration for a cumulative duration of less than 1 year and of 1 year or longer were each associated with infection with an STI or HIV. These results suggest that incarceration may be an independent correlate of infection with an STI or HIV. Prior studies have documented the association between incarceration and high-risk partnerships and have suggested that incarceration may be a factor contributing to these risk behaviors.12–19 Although the cross-sectional data structure of the NNAHRAY study limits the interpretability of the findings, these results provide preliminary evidence to suggest that incarceration may be a risk factor not only of sexual risk behaviors but also of biologically confirmed infection with an STI or HIV.
Increasing duration of prior incarceration was not associated with increasing elevations of infection with an STI or HIV. Any incarceration, whether for a short or long duration, is a disruptive life event and may translate to comparable elevations in infection risk. Prior studies conducted by members of this team have highlighted the potential importance of short-term incarcerations in infection risk.19,45 One of these studies indicated that short-term incarcerations were more strongly associated with HIV risk behaviors than long-term incarcerations; increased rates of migration through the criminal justice system may lead to increased disruptions of social networks and rates of sex partnership exchange.19 Further research is needed to explore how different durations of incarceration may differentially influence risk behavior and infection.
Whereas prior findings suggested that incarceration of a partner is associated with elevated levels of sexual risk behaviors independent of other risk factors,17,19 incarceration of a partner was not an independent correlate of infection among NNAHRAY participants; the association between partner incarceration and STI or HIV was attenuated in the multivariable models. Again, the results should be interpreted cautiously because of data limitations. The indicator of partner incarceration that was available for this analysis—sex in the past 3 months with a partner who had ever been incarcerated—may have occurred after acquisition of STI or HIV. Further research is needed to examine the prospective relationship between incarceration of a partner and STI or HIV risk.
Analysis of NNAHRAY data enabled investigation of the potential influences of incarceration on risk of involvement in networks with high levels of STI and HIV infection. In adjusted analyses, sex with infected partners was disproportionately high among those who had experienced short-term incarceration and among those who had 1 or more recent partners who had been incarcerated. The study provides preliminary evidence to suggest that if incarceration contributes to STI or HIV infection, it does so not only by increasing sexual risk-taking, as has been suggested in prior studies,12–19 but also by increasing the likelihood of sex partnerships with infected partners. To best evaluate the degree to which incarceration influences infection risk by increasing multiple partnerships and unprotected sex versus increasing risk of sex with an infected partner, a longitudinal study is needed that prospectively assesses personal history of incarceration and partner incarceration, potential mediating factors including sexual risk behaviors and changes in risk networks, and incident STI.
These network data enable visualization of the distribution of incarceration and infection with HSV-2 or HIV through a sexual and drug risk network (Figure 1). The results graphically represent what is known on the basis of tabulations of the data: incarceration and infection with HSV-2 or HIV affect substantial proportions of the network, and even if someone has not been incarcerated or is not HSV-2 infected, most likely he or she has a contact who has been incarcerated or is HSV-2 infected. The network diagram depicts the high level of interconnection among individuals in the network and suggests that if incarceration influences STI or HIV transmission, any deleterious effects of incarceration on health are likely to be disseminated through the network.
In addition to the limitations of the cross-sectional data structure, this study is limited because the results cannot be generalized to populations outside of the NNAHRAY network. Nonetheless, the results provide preliminary evidence to suggest that personal incarceration may be an independent risk factor of infection, and that one route by which incarceration may influence sexually transmitted infection, including HIV, is by increasing the risk of sex with infected individuals. The results highlight a need for additional studies on incarceration, STI and HIV infection, and links to high-risk partners in different populations, as well as the need for development of longitudinal network studies conducted to elucidate the prospective relationship between incarceration and infection and to better identify the pathways through which incarceration works to influence STI and HIV.
Even if incarceration only serves as a marker of infection, this study, with others, highlights the need for intensified STI and HIV treatment and prevention efforts among current and former inmates, their sex partners, and other members of their sexual networks. First, such programs should be strengthened in criminal justice settings. Prison settings, where inmates are held for an average of 2 or 3 years, provide an important opportunity to reach a highly vulnerable population with intensive STI and HIV testing, treatment, and prevention interventions while also addressing social, economic, mental health, substance use, and behavioral factors that drive risk of infection in the community.46 In addition, prison-based programs that aim to reduce network disruptions during the criminal justice process (e.g., by reducing barriers to calling or visitation) should be developed and evaluated as a means of reducing STI and HIV transmission risk. Given that there are more than 7 million releasees from local jails annually, failure to systematically offer jail-based rapid STI and HIV testing and treatment constitutes a continued missed opportunity to reach a vulnerable population with limited access to health care.47,48
Second, community-based interventions should be designed for partners of the incarcerated and newly released inmates. Drug treatment centers and harm reduction programs, which serve populations with high levels of involvement in the criminal justice system, serve as preexisting infrastructures from which STI and HIV treatment and prevention interventions can be administered. In addition, our prior research has indicated that social venues where those with a history of incarceration are likely to socialize and meet new sex partners may serve as sites for community-based interventions, including STI and HIV testing, treatment, education, and condom promotion.17 Although additional studies should continue to explore relationships among incarceration, sexual and drug risk behaviors, high-risk networks, and infection in diverse subpopulations, a clear need now exists for intervention studies to evaluate the effectiveness of STI and HIV treatment and prevention programs developed for a range of criminal justice system settings.
Acknowledgments
This research was supported by National Institute on Drug Abuse grant R01DA013128: Networks, Norms and HIV/STI Risk Among Youth (S. R. Friedman, principal investigator).
Human Participant Protection
Ethical approval for all procedures was granted by the institutional review board of the National Development and Research Institutes.
References
- 1.Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92(11):1789–1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braithwaite RL, Arriola KR. Male prisoners and HIV prevention: a call for action ignored. Am J Public Health. 2003;93(5):759–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chapter 3: prevalence of communicable disease, chronic disease, and mental illness among the inmate population. : The Health Status of Soon-to-Be-Released Inmates: A Report to Congress. Vol. 1 Chicago, IL: National Commission on Correctional Health Care; 2002:15–28 [Google Scholar]
- 4.Arriola KR, Braithwaite RL, Kennedy S, et al. A collaborative effort to enhance HIV/STI screening in five county jails. Public Health Rep. 2001;116(6):520–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mertz KJ, Schwebke JR, Gaydos CA, Beidinger HA, Tulloch SD, Levine WC. Screening women in jails for chlamydial and gonococcal infection using urine tests: feasibility, acceptability, prevalence, and treatment rates. Sex Transm Dis. 2002;29(5):271–276 [DOI] [PubMed] [Google Scholar]
- 6.Hardick J, Hsieh YH, Tulloch S, Kus J, Tawes J, Gaydos CA. Surveillance of Chlamydia trachomatis and Neisseria gonorrhoeae infections in women in detention in Baltimore, Maryland. Sex Transm Dis. 2003;30(1):64–70 [DOI] [PubMed] [Google Scholar]
- 7.Chen JL, Bovee MC, Kerndt PR. Sexually transmitted diseases surveillance among incarcerated men who have sex with men—an opportunity for HIV prevention. AIDS Educ Prev. 2003;15(1 suppl A):117–126 [DOI] [PubMed] [Google Scholar]
- 8.Hammett TM, Drachman-Jones A. HIV/AIDS, sexually transmitted diseases, and incarceration among women: national and southern perspectives. Sex Transm Dis. 2006;33(7 suppl):S17–S22 [DOI] [PubMed] [Google Scholar]
- 9.Maruschak LM. HIV in Prisons, 2007–08. Washington, DC: Dept of Justice, Bureau of Justice Statistics; 2009:1–8 [Google Scholar]
- 10.McQuillan GM, Kruszon-Moran D, Kottiri BJ, et al. Prevalence of HIV in the US household population: the National Health and Nutrition Examination Surveys, 1988 to 2002. J Acquir Immune Defic Syndr. 2006;41(5):651–656 [DOI] [PubMed] [Google Scholar]
- 11.Adimora AA, Schoenbach VJ, Martinson FE, et al. Heterosexually transmitted HIV infection among African Americans in North Carolina. J Acquir Immune Defic Syndr. 2006;41(5):616–623 [DOI] [PubMed] [Google Scholar]
- 12.Manhart LE, Aral SO, Holmes KK, Foxman B. Sex partner concurrency: measurement, prevalence, and correlates among urban 18-39-year-olds. Sex Transm Dis. 2002;29(3):133–143 [DOI] [PubMed] [Google Scholar]
- 13.Tyndall MW, Patrick D, Spittal P, Li K, O'Shaughnessy MV, Schechter MT. Risky sexual behaviours among injection drugs users with high HIV prevalence: implications for STD control. Sex Transm Infect. 2002;78(suppl 1):i170–i175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adimora AA, Schoenbach VJ, Martinson FE, Donaldson KH, Stancil TR, Fullilove RE. Concurrent partnerships among rural African Americans with recently reported heterosexually transmitted HIV infection. J Acquir Immune Defic Syndr. 2003;34(4):423–429 [DOI] [PubMed] [Google Scholar]
- 15.Adimora AA, Schoenbach VJ, Martinson F, Donaldson KH, Stancil TR, Fullilove RE. Concurrent sexual partnerships among African Americans in the rural South. Ann Epidemiol. 2004;14(3):155–160 [DOI] [PubMed] [Google Scholar]
- 16.Epperson M, El-Bassel N, Gilbert L, Orellana ER, Chang M. Increased HIV risk associated with criminal justice involvement among men on methadone. AIDS Behav. 2008;12(1):51–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan MR, Wohl DA, Weir SS, et al. Incarceration and risky sexual partnerships in a southern US city. J Urban Health. 2008;85(1):100–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan MR, Doherty IA, Schoenbach VJ, Taylor EM, Epperson MW, Adimora AA. Incarceration and high-risk sex partnerships among men in the United States. J Urban Health. 2009;86(4):584–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan MR, Miller WC, Schoenbach VJ, et al. Timing and duration of incarceration and high-risk sexual partnerships among African Americans in North Carolina. Ann Epidemiol. 2008;18(5):403–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epperson MW, Khan MR, El-Bassel N, Wu E, Gilbert L. A longitudinal study of incarceration and HIV risk among methadone maintained men and their primary female partners. AIDS Behav. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Comfort M, Grinstead O, McCartney K, Bourgois P, Knight K. “You can't do nothing in this damn place”: sex and intimacy among couples with an incarcerated male partner. J Sex Res. 2005;42(1):3–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lowenstein A. Coping with stress: the case of prisoner's wives. J Marriage Fam. 1984;46(3):699–708 [Google Scholar]
- 23.Browning S, Miller S, Lisa M. Criminal incarceration dividing the ties that bind: black men and their families. J Afr Am Men. 2001;6(1):87–102 [Google Scholar]
- 24.Rindfuss R, Stephen EH. Marital noncohabitation: separation does not make the heart grow fonder. J Marriage Fam. 1990;52:259–270 [Google Scholar]
- 25.Schneller D. Prisoner's families: a study of some social and psychological effects of incarceration on the families of negro prisoners. Criminology. 1975;12(4):402–412 [Google Scholar]
- 26.Morrow KM. HIV, STD, and hepatitis risk behaviors of young men before and after incarceration. AIDS Care. 2009;21(2):235–243 [DOI] [PubMed] [Google Scholar]
- 27.Behrend L, Khan M, White BL, Wohl DA. Dissolution of Stable Intimate Partnerships During Incarceration: Implications for HIV Transmission. Washington, DC: Society for Prevention Research; 2009 [Google Scholar]
- 28.Grinstead OA, Faigeles B, Comfort M, et al. HIV, STD, and hepatitis risk to primary female partners of men being released from prison. Women Health. 2005;41(2):63–80 [DOI] [PubMed] [Google Scholar]
- 29.Adimora AA, Schoenbach VJ, Bonas DM, Martinson FE, Donaldson KH, Stancil TR. Concurrent sexual partnerships among women in the United States. Epidemiology. 2002;13(3):320–327 [DOI] [PubMed] [Google Scholar]
- 30.Adimora AA, Schoenbach VJ, Doherty I. Concurrent sexual partnership among men in the US. Am J Public Health. 2007;97(12):2230–2237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78:458–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78(3):214–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore J. Bearing the burden: how incarceration weakens inner-city communities. : Vera Institute of Justice, The Unintended Consequences of Incarceration. New York, NY: Vera Institute of Justice; 1996:67–90 [Google Scholar]
- 34.Friedman SR, Bolyard M, Mateu-Gelabert P, et al. Some data-driven reflections on priorities in AIDS network research. AIDS Behav. 2007;11(5):641–651 [DOI] [PubMed] [Google Scholar]
- 35.Klovdahl AS, Potterat JJ, Woodhouse DE, Muth JB, Muth SQ, Darrow WW. Social networks and infectious disease: the Colorado Springs Study. Soc Sci Med. 1994;38(1):79–88 [DOI] [PubMed] [Google Scholar]
- 36.Rothenberg RB, Woodhouse DE, Potterat JJ, Muth SQ, Darrow WW, Klovdahl AS. Social networks in disease transmission: the Colorado Springs Study. NIDA Res Monogr. 1995;151:3–19 [PubMed] [Google Scholar]
- 37.Friedman SR, Bolyard M, Sandoval M, Mateu-Gelabert P, Maslow C, Zenilman J. Relative prevalence of different sexually transmitted infections in HIV-discordant sexual partnerships: data from a risk network study in a high-risk New York neighbourhood. Sex Transm Infect. 2008;84(1):17–18 [DOI] [PubMed] [Google Scholar]
- 38.Mahler L. Sexed Work: Gender, Race and Resistance in a Brooklyn Drug Market. Oxford, England: Oxford University Press; 1997 [Google Scholar]
- 39.Friedman SR, Curtis R, Neaigus A, Jose B, Des Jarlais DC. Social Networks, Drug Injectors' Lives, and HIV/AIDS. New York, NY: Kluwer/Plenum; 1999 [Google Scholar]
- 40.Friedman SR, Flom PL, Kottiri BJ, et al. Drug use patterns and infection with sexually transmissible agents among young adults in a high-risk neighbourhood in New York City. Addiction. 2003;98(2):159–169 [DOI] [PubMed] [Google Scholar]
- 41.Zocchetti C, Consonni D, Bertazzi PA. Estimation of prevalence rate ratios from cross-sectional data. Int J Epidemiol. 1995;24(5):1064–1065 [DOI] [PubMed] [Google Scholar]
- 42.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157(10):940–943 [DOI] [PubMed] [Google Scholar]
- 43.Zou GA. modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706 [DOI] [PubMed] [Google Scholar]
- 44.Vlahov D, Putnam S. From corrections to communities as an HIV priority. J Urban Health. 2006;83(3):339–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Epperson MW, El-Bassel N, Gilbert L, Chang M. Examining the temporal relationship between criminal justice involvement and sexual risk behaviors among drug-involved men. J Urban Health. 2010;87(2):324–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wolitski RJ. Relative efficacy of a multisession sexual risk-reduction intervention for young men released from prisons in 4 states. Am J Public Health. 2006;96(10):1854–1861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mertz KJ, Voigt RA, Hutchins K, Levine WC. Findings from STD screening of adolescents and adults entering corrections facilities: implications for STD control strategies. Sex Transm Dis. 2002;29(12):834–839 [DOI] [PubMed] [Google Scholar]
- 48.Freudenberg N. Coming Home From Jail: A Review of Health and Social Problems Facing US Jail Populations and of Opportunities for Reentry Interventions. Washington, DC: Urban Institute; 2006 [Google Scholar]