Abstract
Objectives. We examined relationships of spatial access to syringe exchange programs (SEPs) and pharmacies selling over-the-counter (OTC) syringes with New York City drug injectors’ harm reduction practices.
Methods. Each year from 1995 to 2006, we measured the percentage of 42 city health districts’ surface area that was within 1 mile of an SEP or OTC pharmacy. We applied hierarchical generalized linear models to investigate relationships between these exposures and the odds that injectors (n = 4003) used a sterile syringe for at least 75% of injections in the past 6 months.
Results. A 1-unit increase in the natural log of the percentage of a district's surface area within a mile of an SEP in 1995 was associated with a 26% increase in the odds of injecting with a sterile syringe; a 1-unit increase in this exposure over time increased these odds 23%. A 1-unit increase in the natural log of OTC pharmacy access improved these odds 15%.
Conclusions. Greater spatial access to SEPs and OTC pharmacies improved injectors’ capacity to engage in harm reduction practices that reduce HIV and HCV transmission.
Research indicates that individuals who live closer to mental health and primary care clinics are more likely to use these services.1–5 Accordingly, the US Department of Health and Human Services and other public health agencies promote easy spatial access to health care service sites in small geographic areas (e.g., clusters of census tracts).6,7 Syringe exchange programs (SEPs) and pharmacies that sell syringes without a prescription, or over the counter (OTC), are health care services that substantially increase the likelihood that drug injectors will use sterile syringes, thus reducing their probability of becoming infected with HIV, HCV, and possibly other injection-related bacterial infections.8–19 Multiple studies have concluded that the prevalence of injection-related HIV and related risk behaviors is higher in nations, states, and other large geographic areas with poor spatial access to SEPs or OTC pharmacies,9,20–25 but little research has focused on the impact of spatial access to SEPs and OTC pharmacies in small geographic areas on local injectors’ injection practices and rates of injection-related infection.
Spatial access to SEPs and OTC pharmacies often varies across small geographic areas within a city, metropolitan area, or state. Municipal ordinances may prohibit SEPs from operating within a specific distance of a school or park, and local opposition may prevent a new SEP from opening in a neighborhood or may force an existing SEP to close.26–28 Some states permit pharmacies to choose whether to sell OTC syringes, and the distribution of pharmacies themselves across neighborhoods is uneven.29–31 The few studies of local access to SEPs have found that, as with other health services,1–5 proximity increases utilization.32–35 For example, Rockwell et al. found that injectors living within a 10-minute travel distance of an SEP in New York City in 1993 were almost 3 times as likely as other injectors to attend an SEP and half as likely to report injecting with used syringes.33 A recent study, however, found no relationship between OTC pharmacy access and injection-related behaviors among injectors living within 1 kilometer of a pharmacy.34
Quantifying the effect of spatial access to SEPs on injection practices in local areas is particularly pressing now. After decades of withholding federal funds from SEPs, the US Congress in 2009 approved an appropriations bill permitting federal funding of SEPs. These funds could permit new SEPs to open and allow existing SEPs to add sites. As the appropriations bill underwent congressional review, the geographic location of federally funded SEPs became a source of debate. The House version of the bill restricted federal funding to SEPs located more than 1000 feet from an educational institution, public recreation area, “or an event sponsored by any such entity.”36(sec523) The Senate version contained no geographic restrictions. The final appropriations bill shifts decisions about SEP locations to local governments: the bill prohibits granting federal funds to SEPs located in sites “that local public health or law enforcement agencies determine to be inappropriate.”37(p8) Research on the effect of spatial access to SEPs on injection practices may inform local advocacy and decisions about which SEP sites may receive federal funding.
We conducted a longitudinal (1995–2006) multilevel analysis of whether variations in spatial access to SEPs and OTC pharmacies across New York City health districts affected the likelihood that local injectors used sterile syringes. Although state law required a prescription to purchase a syringe throughout the study period, syringe access has evolved over time. Starting in 1992, the New York State Department of Health permitted select SEPs to operate legally; as of January 1, 2001, pharmacists who voluntarily registered with the department were permitted to sell OTC syringes.38,39
METHODS
We applied multilevel analysis methods to quantify relationships between variations in health district access to SEPs and OTC pharmacies and the odds that injectors reported injecting with sterile syringes in the past 6 months. Individual-level data were drawn from the Risk Factors for AIDS Among Intravenous Drug Users study (principal investigator, D. C. D. J.), a series of cross-sectional surveys of people entering the Beth Israel Hospital detoxification program. Recruitment methods did not change between 1995–2006; details have been published elsewhere.40 To be included in our analyses, participants had to report injecting drugs in the past 6 months, take part in the study between 1995–2006, and have a valid New York City zip code (homeless people were assigned the zip code where they had slept most in the past 6 months). A total of 4178 Risk Factors participants met those criteria.
We combined cross-sectional Risk Factors data for 1995–2006, thereby creating a multilevel data set in which each of the 4178 Risk Factors participants was nested in the study year in which the respondent was surveyed (missing data reduced the final sample size to 4003). Study years in turn were nested in New York City's 42 populated health districts. Health districts are aggregations of 3 to 9 adjacent zip code areas that have similar sociodemographic characteristics.41 In 1995, the median district population size was 179 189 (range = 28 739–428 867).42
Variables
Spatial access to syringe exchange programs.
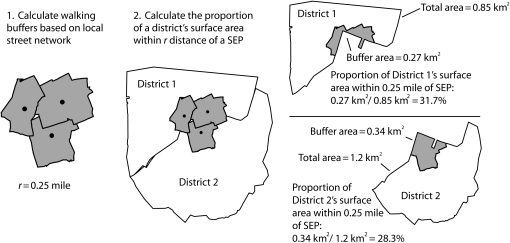
We used geospatial methods to develop measures of spatial access to SEPs in each New York City health district for each year of the 12-year study period. For each year, we applied a 3-stage process to create a continuous variable that captured the percentage of each district's surface area within a given radius (r) of an SEP site (Figure 1).
Stage 1: geocoding SEP sites. We obtained lists of the street addresses of all legal SEP sites that operated during the study period from the New York State Department of Health and SEP directors. Sites that were located in New York City and within 1 mile of the city's boundaries were included. We geocoded each site's address to a latitude and longitude point; van stops and other sites with no street address were geocoded to the nearest intersection or block midpoint. Eighty sites operated during the study period; we geocoded 100% of the sites to their street address or nearest intersection. We created SEP site maps for each year.
Stage 2: creating buffers for each site. We overlaid a digital road network map on each annual SEP site map.43 We created a walking distance buffer for each site that extended r distance from the site along the local street network.
Stage 3: calculating the proportion of a district's surface area within r distance of an SEP. We overlaid a digital map of district boundaries and a grid of cells (cell size = 10 m2) on each annual map created in stage 2. For each year, we calculated the percentage of a district's surface area within r distance of an SEP site by dividing the number of cells falling within a buffer by the total number of cells in that district. Cells that were covered by the buffers of more than 1 SEP were counted once.
FIGURE 1.
Stages used to develop the spatial measure of district-level access to syringe exchange programs.
We created 3 measures of SEP access, with r equal to 1.00 mile, 0.50 mile, or 0.25 mile. We selected these distances for consistency with previous research, which measured spatial access to SEPs in 1-mile and 10-minute travel distances (people can usually walk 0.25–0.50 mile in 10 minutes).32–35
Spatial access to over-the-counter pharmacies.
We applied our 3-stage process to create a measure for 2001 to 2006. We obtained an inventory of the addresses of all pharmacies that registered to sell OTC syringes from the New York State Department of Health. We were able to geocode 97% of the 1316 pharmacies selling OTC syringes to their street address or nearest intersection. When we received these data, no information was available on withdrawal from this voluntary program.
Individual-level outcome.
We assessed sterile syringe use through injectors’ self-reports of the percentage of injection events in the past 6 months in which they had injected with a sterile syringe (i.e., a syringe that neither they nor anyone else had used previously). This ordinal variable had 3 values: use of a sterile syringe in 25% or fewer of injection events, in 26% to 74% of injection events, or in 75% or more of injection events.
Individual-level covariates.
Injection frequency (past 6 months), years since first injection, sexual orientation, self-reported HIV serostatus, and age might confound the relationships between sterile syringe use and spatial access to SEPs and to OTC pharmacies.44–46 We used self-reported race/ethnicity, gender, and homelessness as effect modifiers or possible confounders of our focal relationships.47–50 We treated all covariates as dichotomous variables except years since first injection (continuous) and injection frequency (an ordinal variable with 3 values: < 1, 1–3, or ≥ 4 times/day).
District-level covariates.
Local poverty rates and racial/ethnic composition were other potential confounders of the relationships of interest.30,51 We calculated time-varying measures of local poverty rates and racial/ethnic composition (percentage of residents who were non-Hispanic or Latino Whites) from 1990 and 2000 decennial US Census data and expressed them as continuous variables. We imputed intercencile data points with an assumption of linear change over time.
Time.
Study year was a continuous variable ranging from zero in 1995 to 12 in 2006. Years since pharmacies were allowed to sell OTC syringes (OTC time) was a continuous variable ranging from zero in 1995–2001 to 6 in 2006. We also classified time with a dichotomous variable denoting whether OTC sales were legal during that year.
Analyses
We investigated trends in each variable's distribution over time and across districts through exploratory data analysis.52 In inferential analyses, we applied 3-level hierarchical generalized linear models with an ordinal outcome to investigate the relationship between district-level access to SEPs and OTC pharmacies and the individual-level outcome.53 Model A was a growth curve model designed to describe temporal trends in the odds of injecting with a sterile syringe and to identify optimal variance–covariance structures.54 In all models, to minimize the likelihood that compositional changes in the Risk Factors study sample over time confounded our analyses, we controlled for compositional changes related to our outcome (i.e., age, gender, race/ethnicity, homeless status, sexual orientation, self-reported HIV status, injection frequency, and years since initiation of injecting). In models B through D, we added district-level SEP access and possible district-level confounders (model B, r = 1.00 mile; model C, r = 0.50 mile; model D, r = 0.25 mile). Subsequent models included OTC pharmacy–related variables. We ran separate models for each OTC pharmacy access radius; only 1 set of results is shown for model E, because results were similar across radii.
We investigated random effects, lagged and nonlinear relationships between exposures and outcomes, and intralevel and cross-level interactions. We selected optimal models with likelihood ratio tests when models were nested, with visual displays of data, and with relevant literature.53,54 We mean-centered level 1 continuous variables and centered level 2 continuous variables at their initial value.53,54 We probed interactions for regions of significance (i.e., values on each variable for which the interaction was statistically significant) with the Johnson–Neyman technique.55,56 Study year and district were entered as random variables, the optimal covariance structure for time-varying observations was autoregressive, and the optimal covariance structure was unstructured for district-level observations. District-level racial/ethnic composition and poverty rates were highly correlated (Pearson correlation coefficient = −0.75); we included only the former construct because past research suggests that local racial/ethnic composition predicts injection practices.51 We conducted all analyses in SAS version 9.257 and ArcInfo version 9.3.58
RESULTS
During the 12-year study period, almost half of the participants reported injecting with a sterile syringe in 25% or fewer of their injection events in the past 6 months, while a third reported using sterile syringes at least 75% of the time (Table 1). Approximately 80% of the participants were men, and half were Latino. One third of the participants were homeless.
TABLE 1.
Sociodemographic Characteristics and Injection Practices of Injection Drug Users: New York City, 1995–2006
| Characteristics of Individual Injectors (Self-Reported) | No. (%) or Median (Range) |
| Gender | |
| Women | 825 (20.61) |
| Men | 3178 (79.39) |
| Race/ethnicity | |
| Hispanic/Latino (regardless of race) | 2022 (50.51) |
| Non-Hispanic Black/African American | 848 (21.18) |
| Non-Hispanic White and Othera | 1133 (28.30) |
| Age, y | 38 (18–75) |
| Sexual orientation | |
| Women who have sex with women | 254 (6.35) |
| Men who have sex with men | 170 (4.25) |
| Heterosexual | 3579 (89.41) |
| Homeless | 1344 (33.57) |
| HIV-positive | 456 (11.39) |
| Years since started injecting | 14 (0–52) |
| Injection frequency in past 6 mo, times/d | |
| < 1 | 820 (20.48) |
| 1–3 | 1479 (36.95) |
| ≥ 4 | 1704 (42.57) |
| Used sterile syringe in past 6 mo, % of injection events | |
| ≤ 25 | 1914 (47.81) |
| 26–74 | 757 (18.91) |
| ≥ 75 | 1332 (33.28) |
Note. The sample size was n = 4003.
Only 87 participants reported that they were not Latino/Hispanic, White, or Black/African American. These 87 individuals were grouped in analyses with non-Hispanic Whites, the racial/ethnic group to which their risk profile was most similar.
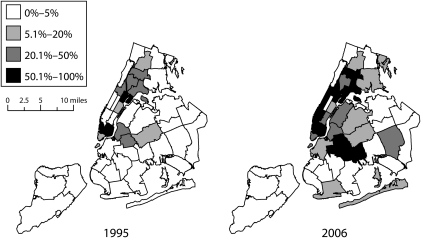
Regardless of the buffer, at least half of the health districts had no SEP access in 1995, and at least half of the districts experienced minimal or no increase in spatial access to SEPs between 1995–2006 (Table 2; Figure 2). Between 7.60% and 91.11% of the surface area of one quarter of the districts lay within 1 mile of an SEP in 1995; by 2006, one quarter of the districts experienced absolute increases of 19.94% or more in the percentage of their surface area located within 1 mile of an SEP. SEP access values in 1995, and increases in these values over time, were lower when we measured access with 0.50-mile and 0.25-mile buffers than when we used a 1.00-mile buffer.
TABLE 2.
Sociodemographics and Spatial Access to Syringe Exchange Programs and to Pharmacies Selling Syringes Over the Counter in New York City Health Districts: 1995–2006
| Characteristics of Health Districts | Mean (SD) | Median | Interquartile Range | Range |
| % surface area within 1.00 mile of an SEP | ||||
| Baseline | 11.75 (22.26) | 0.00 | 0.00–7.60 | 0.00–91.10 |
| Difference in spatial coverage between baseline and end of study | 13.13 (19.30) | 2.18 | 0.00–19.94 | −6.58–76.86 |
| % surface area within 0.50 mile of an SEP | ||||
| Baseline | 4.18 (9.70) | 0.00 | 0.00–0.87 | 0.00–37.96 |
| Difference in spatial coverage between baseline and end of study | 5.15 (8.63) | 0.02 | 0.00–7.77 | −7.47–33.83 |
| % surface area within 0.25 mile of an SEP | ||||
| Baseline | 1.29 (3.21) | 0.00 | 0.00–0.01 | 0.00–13.12 |
| Difference in spatial coverage between baseline and end of study | 1.56 (3.08) | 0.00 | 0.00–2.72 | −3.43–15.44 |
| % surface area within 1.00 mile of an OTC pharmacy | ||||
| Year when OTC sales legalized | 77.51 (19.20) | 83.27 | 63.26–95.15 | 34.42–99.81 |
| Difference in spatial coverage between 2001 and 2006 | 5.41 (7.00) | 2.70 | 0.14–8.90 | −0.60–27.69 |
| % surface area within 0.50 mile of an OTC pharmacy | ||||
| Year when OTC sales legalized | 47.77 (24.56) | 49.06 | 24.62–65.44 | 11.55–95.86 |
| Difference in spatial coverage between 2001 and 2006 | 12.30 (9.39) | 10.55 | 6.71–14.41 | 0.80–40.17 |
| % surface area within 0.25 mile of an OTC pharmacy | ||||
| Year when OTC sales legalized | 21.68 (19.11) | 17.49 | 7.27–26.03 | 2.52–79.23 |
| Difference in spatial coverage between 2001 and 2006 | 11. 04 (7.91) | 9.55 | 6.23–14.24 | 1.72–43.66 |
| % population living in povertya | ||||
| Baseline | 20.27 (11.51) | 17.07 | 11.79–30.68 | 4.95–47.30 |
| Difference between baseline and end of study | 1.54 (2.90) | 2.05 | −0.94–3.62 | −6.42–7.26 |
| % residents who were non-Hispanic White | ||||
| Baseline | 42.43 (27.27) | 47.28 | 13.26–66.94 | 1.75–89.89 |
| Difference between baseline and end of study | −7.33 (7.60) | −5.53 | −11.98–−1.03 | −30.75–2.85 |
Note. OTC = over the counter; SEP = syringe exchange program. Health districts, n = 42. Baseline was 1995, OTC sales were legalized in 2001, and the study ended in 2006.
Defined as living below federal poverty level determined by US Census Bureau.
FIGURE 2.
Percentage of New York City health districts’ surface areas within 1 mile of a syringe exchange program in 1995 and 2006.
Coverage of OTC pharmacies was high beginning in the first year these sales were permitted. In 2001, half of all districts had 83% or more of their surface area within 1 mile of an OTC pharmacy, while half of all districts had 49% or more of their area within one half mile, and half of all districts had 17.50% or more within one quarter mile. Increases in spatial access to OTC pharmacies between 2001 and 2006 were smaller for the 1-mile buffer measure than for the other measures, perhaps because of a ceiling effect.
The intercepts in model A, the growth curve model, indicated that on average across districts, in 1995 16% of respondents reported injecting with a sterile syringe during 75% or more of injection events (95% confidence interval [CI] = 0.09, 0.28), and 38% reported using a sterile syringe 26% or more of the time in the past 6 months (95% CI = 0.23, 0.65), when other covariates were controlled (Table 3). Coefficients describing relationships between predictors and the outcome were identical regardless of which cutpoint we used; therefore, we report results with the 75% cutpoint.
TABLE 3.
Multilevel Ordinal Regression of the Likelihood of Injecting With a Sterile Syringe on Spatial Access to SEPs and to Pharmacies Selling Syringes OTC in New York City Health Districts: 1995–2006
| Predictor Variable | Model A: Growth Curve, OR (95% CI) | Model B: SEP Access Within 1.00 Mile, OR (95% CI) | Model C: SEP Access Within 0.50 Mile, OR (95% CI) | Model D: SEP Access Within 0.25 Mile, OR (95% CI) | Model E: OTC Pharmacy and SEP Access Within 0.50 Mile,a OR (95% CI) |
| Individual-level covariates | |||||
| Intercept 1b | 0.16 (0.09, 0.28) | 0.11 (0.05, 0.26) | 0.11 (0.05, 0.24) | 0.12 (0.06, 0.27) | 0.10 (0.05, 0.21) |
| Intercept 2c | 0.38 (0.23, 0.65) | 0.27 (0.13, 0.59) | 0.25 (0.11, 0.55) | 0.29 (0.13, 0.63) | 0.23 (0.22, 0.50) |
| Age, y | |||||
| 18–30 | 0.89 (0.74, 1.07) | 0.89 (0.73, 1.06) | 0.88 (0.74, 1.06) | 0.88 (0.74, 1.06) | 0.88 (0.73, 1.05) |
| > 30 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Gender | |||||
| Men (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Women | 1.26 (1.07, 1.49) | 1.26 (1.07, 1.48) | 1.26 (1.07, 1.49) | 1.26 (1.07, 1.49) | 1.26 (1.07, 1.48) |
| Race/ethnicity | |||||
| Hispanic/Latino (any race; Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-Hispanic Black | 1.05 (0.88, 1.25) | 1.06 (0.89, 1.25) | 1.06 (0.90, 1.26) | 1.06 (0.90, 1.26) | 1.05 (0.88, 1.24) |
| Non-Hispanic White/Other | 0.80 (0.68, 0.94) | 0.83 (0.71, 0.98) | 0.83 (0.70, 0.97) | 0.82 (0.67, 0.96) | 0.82 (0.70, 0.96) |
| Homeless | 0.77 (0.67, 0.88) | 0.76 (0.66, 0.87) | 0.76 (0.66, 0.87) | 0.76 (0.66, 0.87) | 0.76 (0.66, 0.87) |
| Lesbian/gay/bisexual | 0.89 (0.72, 1.11) | 0.88 (0.71, 1.10) | 0.88 (0.71, 1.09) | 0.87 (0.70, 1.09) | 0.87 (0.70, 1.08) |
| HIV-positive (self-report) | 1.00 (0.81, 1.22) | 1.00 (0.81, 1.21) | 0.99 (0.81, 1.21) | 0.98 (0.80, 1.20) | 0.98 (0.80, 1.20) |
| Injection frequency in past 6 mo, times/d | |||||
| < 1 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–3 | 0.53 (0.45, 0.63) | 0.53 (0.45, 0.63) | 0.53 (0.45, 0.63) | 0.53 (0.44, 0.63) | 0.53 (0.44, 0.63) |
| ≥ 4 | 0.38 (0.32, 0.45) | 0.38 (0.32, 0.45) | 0.38 (0.32, 0.45) | 0.37 (0.31, 0.44) | 0.37 (0.32, 0.45) |
| Deviation from mean years of injecting for district and year | 1.00 (0.99, 1.01) | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) |
| District-level predictors | |||||
| Time-varying predictors | |||||
| Years since study began | 0.80 (0.74, 0.86) | 0.76 (0.70, 0.83) | 0.77 (0.71, 0.84) | 0.78 (0.72, 0.85) | 0.87 (0.83, 0.92) |
| Years since study began, squared | 1.02 (1.01, 1.03) | 1.03 (1.02, 1.03) | 1.02 (1.02, 1.03) | 1.02 (1.02, 1.03) | … |
| Years since OTC pharmacy sales permitted | … | … | … | … | 0.20 (0.11, 0.38) |
| Years since OTC pharmacy sales permitted × years since study began | … | … | … | … | 1.16 (1.10, 1.21) |
| OTC pharmacy sales permitted | … | … | … | … | 3.61 (2.17, 6.02) |
| Mean years since first injection for that district and year | 1.01 (0.99, 1.03) | 1.01 (0.99, 1.03) | 1.02 (1.00, 1.03) | 1.02 (1.00, 1.03) | 1.02 (1.00, 1.03) |
| Decline in % of residents who were non-Hispanic White in that year and districtd | … | 1.25 (0.99, 1.60) | 1.27 (1.00, 1.61) | 1.22 (0.96, 1.55) | 1.22 (0.97, 1.54) |
| Natural log of annual change in spatial access to an SEP since 1995 | … | 1.23 (1.01, 1.52) | 1.30 (1.03, 1.64) | 1.34 (1.01, 1.84) | 1.25 (1.00, 1.55) |
| Natural log of spatial access to OTC pharmacy | … | … | … | … | 1.15 (1.03, 1.27) |
| Time-invariant predictors | |||||
| Natural log of spatial access to SEPs in 1995 | … | 1.26 (1.03, 1.54) | 1.46 (1.14, 1.86) | 1.69 (1.18, 2.41) | 1.43 (1.13, 1.80) |
| Natural log of % of residents who were non-Hispanic White in 1995 | … | 0.95 (0.87, 1.04) | 0.95 (0.87, 1.03) | 0.93 (0.85, 1.01) | 0.95 (0.87, 1.03) |
| Cross-level interaction | |||||
| Natural log of spatial access to SEPs in 1995 × natural log of annual change in spatial access to SEPs since 1995 | … | 0.95 (0.88, 1.02) | 0.89 (0.81, 0.98) | 0.79 (0.65, 0.96) | 0.90 (0.82, 0.98) |
Note. CI = confidence interval; OR = odds ratio; OTC = over the counter; SEP = syringe exchange program. Ellipses indicate the predictor was not applicable. Injectors, n = 4003; health districts, n = 42.
Spatial access to OTC pharmacies was assessed for 2003 onward; previous values were set to zero.
Intercept when the outcome was injecting with a sterile syringe during at least 75% of injection events in the past 6 months.
Intercept when the outcome was injecting with a sterile syringe during at least 26% of injection events in the past 6 months.
Reference was stasis or no decline.
In the optimal growth curve model, time was expressed through 2 variables: number of years since 1995 and the square of this variable. Together, these variables indicated that the odds of injecting with a sterile syringe during at least 75% of injection events (also referred to here as always or almost always injecting with a sterile syringe) declined during the study period (adjusted odds ratio [AOR] = 0.80; 95% CI = 0.74, 0.86) and that this decline decelerated over time (AOR = 1.02; 95% CI = 1.01, 1.03). By applying Singer and Willett's inflection formula (which identifies the point where a curve shifts from being concave to convex or vice versa),54 we determined that this declining trajectory reversed direction in 2001.
Model B quantified the relationship of variations in the percentage of district surface area within 1 mile of an SEP with the odds of always or almost always injecting with a sterile syringe. We took the natural log of this SEP variable to linearize its relationship to the outcome (we applied this transformation to all SEP and OTC access variables for the same reason). The resulting model indicated that, on average across districts, residents of districts that were 1 unit higher on this logged exposure at baseline had higher odds of reporting always or almost always injecting with a sterile syringe in the past 6 months (AOR = 1.26; 95% CI = 1.03, 1.54). A 1-unit increase in this exposure over time had a similar effect (AOR = 1.23; 95% CI = 1.01, 1.52).
In model C, the relationship between SEP access (r = 0.50 mile) and the outcome was best described by an interaction between 1995 access and changes in that access. At baseline, on average across districts, residents of districts that were 1 unit higher on this logged exposure had higher odds of reporting always or almost always injecting with a sterile syringe (AOR = 1.46; 95% CI = 1.14, 1.86). In districts with no surface area within one half mile of an SEP in 1995, a 1-unit increase in the natural log of SEP access over time was associated with a 30% increase in the odds of injecting with a sterile syringe at least 75% of the time (AOR = 1.30; 95% CI = 1.03, 1.64). This effect was attenuated in districts with spatial access to an SEP at baseline (AOR = 0.89; 95% CI = 0.81, 0.98). This interaction was statistically significant across all values of the one half mile SEP access variable in our data set.
Results of model D (r = 0.25 mile) indicated that, on average, residents of districts that were 1 unit higher in the natural log of this access measure in 1995 had higher odds of reporting always or almost always injecting with a sterile syringe (AOR = 1.69; 95% CI = 1.18, 2.41). Although the coefficient for the interaction of baseline SEP access and changes in access was statistically significant in the full model (AOR = 0.79; 95% CI = 0.65, 0.96), probing indicated that it was significant for only 1 district. Thus, for most districts, the impact of subsequent increases in SEP access was associated with a 34% increase in the outcome, regardless of baseline access (95% CI = 1.01, 184).
In model E, we added OTC pharmacy variables. We reexpressed time as (1) a dichotomous variable denoting whether such sales were legal that year, (2) the number of years since the sales became legal, (3) the number of years since the study began, and (4) an interaction of the latter 2 variables. The odds of injecting with a sterile syringe at least 75% of the time were 3.61 times as high after the legalization of OTC pharmacy sales as before legalization (95% CI = 2.17, 6.02). We interpreted the remaining expressions of time to show that the likelihood of this outcome increased after 2001 and that this increase accelerated over time. From 2003 on, a 1-unit increase in the natural log of spatial access to an OTC pharmacy was associated with a 15% increase in the odds of always or almost always injecting with a sterile syringe (95% CI = 1.03, 1.27). This variable attained statistical significance only after 2002, and its effect did not vary according to radius. The magnitude of the SEP access coefficients remained unchanged when we added OTC pharmacy variables to the model. We found no effect modification by individual race/ethnicity, homeless status, or gender.
DISCUSSION
Regardless of the size of the buffer selected, injection drug users residing in New York City health districts with more surface area within an SEP buffer zone in 1995 had higher odds of reporting always or almost always injecting with a sterile syringe; subsequent rises in spatial coverage over the study period increased these odds. Results from models B to D further suggest the importance of spatial access: AORs for the relationships between SEP access and the outcome were greater when the radius was smaller, although AOR confidence intervals overlapped.
Collectively, our results suggest that better spatial access to SEPs increases local injectors’ capacity to use sterile syringes. This conclusion is consistent with a large body of health services research on the importance of spatial access to services1–5; the conclusion also echoes, on a smaller geographic scale, past research on the health-promoting effects of spatial access to SEPs in nations, metropolitan areas, and cities.9,20–25
Previous analyses of Risk Factors study data have found that HIV prevalence among participants declined from 54% in 1990 to 13% in 2001.16 Our analyses support the attribution of some of this decline to improving SEP access.
The legalization of OTC sales for registered pharmacies was associated with a substantial increase in the odds of always or almost always injecting with a sterile syringe. The effects of this legal shift strengthened between 2001 and 2006, and spatial access to pharmacies only attained statistical significance in 2003. Past research suggests an explanation for this amplifying effect: injectors’ awareness of the legal change, and their willingness to purchase OTC syringes, grew over time.8,59,60
Relationships between spatial access to OTC pharmacies and the outcome were similar across radii (AOR = ∼1.15). Unpublished focus group data from the early years of these sales suggest that some injectors avoided purchasing OTC syringes from pharmacies located near their home to reduce the likelihood that neighbors might discover that they injected (Crystal Fuller, PhD, personal communication, October 1, 2009). Possibly, some injecting residents developed more comfort purchasing syringes from local pharmacies over time, although some may have continued to travel farther afield.
Limitations
Several limitations might have biased our results toward the null. Our measures of SEP access failed to account for public transportation to SEPs and excluded satellite SEPs and illegal SEPs. We therefore likely systematically underestimated SEP access in districts connected to SEPs via buses or subways or with satellite or illegal SEPs operating within or near their boundaries. Likewise, we do not know which pharmacies stopped selling OTC syringes or whether injectors encountered barriers to purchasing syringes at enrolled pharmacies. Thus, we may have overestimated OTC pharmacy access in some districts.
The effects of 3 additional limitations are unknown. We did not measure the number of syringes that SEPs distributed, and yet this volume varies considerably across programs and over time. In addition, our adjustment for compositional changes in the Risk Factors study sample may have been incomplete. Future analyses will explore the role of public transportation in shaping SEP access and will assess the effect of variations in syringe distribution across SEPs and over time on local injection practices. Future analyses will also explore the utility of creating spatial access measures based on local road networks rather than district surface area.
High local drug-related arrest rates impede SEP functioning and injectors’ capacity to use SEP services and to inject safely.61–66 Possibly, the relationship between SEP access and injection practices varies by local arrest rates. We could not test this hypothesis because of the high correlation between arrest rates and SEP access in New York City health districts.
Conclusions
Our findings suggest that greater spatial access to SEPs and OTC pharmacies increases the odds that local injectors will consistently use sterile syringes. When SEP sites operate in or near a district and when pharmacies sell OTC syringes, local injectors use these health services and engage in practices that reduce the incidence of HIV and HCV. Laws, policies, and community mobilizations designed to restrict the locations where SEPs operate may hinder injectors’ ability to behave in ways that promote the public's health.
Acknowledgments
This research was supported by the National Institute on Drug Abuse (grants 5R21DA023391, 5R01DA013336, and 5R01DA003574).
We thank our wonderful project officer, Elizabeth Lambert.
Human Participant Protection
The institutional review boards at Emory University and Beth Israel Medical Center approved this study.
References
- 1.Beardsley K, Wish ED, Fitzelle DB, O'Grady K, Arria AM. Distance traveled to outpatient drug treatment and client retention. J Subst Abuse Treat. 2003;25(4):279–285 [DOI] [PubMed] [Google Scholar]
- 2.Fortney JC, Booth BM, Blow FC, Bunn JY. The effects of travel barriers and age on the utilization of alcoholism treatment aftercare. Am J Drug Alcohol Abuse. 1995;21(3):391–406 [DOI] [PubMed] [Google Scholar]
- 3.Fortney J, Rost K, Zhang M, Warren J. The impact of geographic accessibility on the intensity and quality of depression treatment. Med Care. 1999;37(9):884–893 [DOI] [PubMed] [Google Scholar]
- 4.Haynes R, Bentham G, Lovett A, Gale S. Effects of distances to hospital and GP surgery on hospital inpatient episodes, controlling for needs and provision. Soc Sci Med. 1999;49(3):425–443 [DOI] [PubMed] [Google Scholar]
- 5.Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005;40(1):135–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health Resources and Service Administration Shortage designation: medically underserved areas & populations. Available at: http://bhpr.hrsa.gov/shortage/muaguide.htm. Accessed September 27, 2009
- 7.Community Mental Health Services Block Grant Application Federal Fiscal Year 2008–2010. Harrisburg: Pennsylvania Department of Public Welfare; 2007 [Google Scholar]
- 8.Pouget ER, Deren S, Fuller CM, et al. Receptive syringe sharing among injection drug users in Harlem and the Bronx during the New York State Expanded Syringe Access Demonstration Program. J Acquir Immune Defic Syndr. 2005;39(4):471–477 [DOI] [PubMed] [Google Scholar]
- 9.Friedman SR, Perlis T, Des Jarlais DC. Laws prohibiting over-the-counter syringe sales to injection drug users: relations to population density, HIV prevalence, and HIV incidence. Am J Public Health. 2001;91(5):791–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Needle Exchange Programs: Research Suggests Promise as an AIDS Prevention Strategy. Washington, DC: General Accounting Office; 1993 [Google Scholar]
- 11.Gibson DR, Brand R, Anderson K, Kahn JG, Perales D, Guydish J. Two- to sixfold decreased odds of HIV risk behavior associated with use of syringe exchange. J Acquir Immune Defic Syndr. 2002;31(2):237–242 [DOI] [PubMed] [Google Scholar]
- 12.Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15(11):1329–1341 [DOI] [PubMed] [Google Scholar]
- 13.Ksobiech KA. meta-analysis of needle sharing, lending, and borrowing behaviors of needle exchange program attenders. AIDS Educ Prev. 2003;15(3):257–268 [DOI] [PubMed] [Google Scholar]
- 14.Panel on Needle Exchange and Bleach Distribution Programs, National Research Council and Institute of Medicine. Normand J, Vlahov D, Moses LE, Preventing HIV Transmission: The Role of Sterile Needles and Bleach. Washington, DC: National Academies Press; 1995 [PubMed] [Google Scholar]
- 15.Wodak A, Cooney A. Effectiveness of sterile needle and syringe programmes. Int J Drug Policy. 2005;16(Suppl 1):S31–S44 [Google Scholar]
- 16.Des Jarlais DC, Perlis T, Arasteh K, et al. Reductions in hepatitis C virus and HIV infections among injecting drug users in New York City, 1990–2001. AIDS. 2005;19(Suppl 3):S20–S25 [DOI] [PubMed] [Google Scholar]
- 17.Van Den Berg C, Smit C, Van Brussel G, Coutinho R, Prins M, Amsterdam Cohort. Full participation in harm reduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus: evidence from the Amsterdam Cohort Studies among drug users. Addiction. 2007;102(9):1454–1462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomolillo CM, Crothers LJ, Aberson CL. The damage done: a study of injection drug use, injection related abscesses and needle exchange regulation. Subst Use Misuse. 2007;42(10):1603–1611 [DOI] [PubMed] [Google Scholar]
- 19.Hart GJ, Carvell AL, Woodward N, Johnson AM, Williams P, Parry JV. Evaluation of needle exchange in central London: behaviour change and anti-HIV status over one year. AIDS. 1989;3(5):261–265 [PubMed] [Google Scholar]
- 20.Ingold FR, Ingold S. The effects of the liberalization of syringe sales on the behavior of intravenous drug users in France. Bull Narc. 1989;41(1–2):67–81 [PubMed] [Google Scholar]
- 21.Wright-De Agüero L, Weinstein B, Jones TS, Miles J. Impact of the change in Connecticut syringe prescription laws on pharmacy sales and pharmacy managers’ practices. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(Suppl 1):S102–S110 [DOI] [PubMed] [Google Scholar]
- 22.Groseclose SL, Weinstein B, Jones TS, Valleroy LA, Fehrs LJ, Kassler WJ. Impact of increased legal access to needles and syringes on practices of injecting-drug users and police officers—Connecticut, 1992–1993. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;10(1):82–89 [PubMed] [Google Scholar]
- 23.Romeis JC, Gilchrist B, Northup T, Hager-Mace L, Friedman C, Des Jarlais DC. The Relationship Between State Statutory Restrictions on Access to Syringes and AIDS Rates Among Injecting Drug Users: Final Report. Jefferson City: Missouri Dept of Health: Bureau of AIDS Prevention; 1994 [Google Scholar]
- 24.Des Jarlais DC, Hagan H, Friedman SR, et al. Maintaining low HIV seroprevalence in populations of injecting drug users. JAMA. 1995;274(15):1226–1231 [DOI] [PubMed] [Google Scholar]
- 25.MacDonald M, Law M, Kaldor J, Hales J, Dore GJ. Effectiveness of needle and syringe programmes for preventing HIV transmission. Int J Drug Policy. 2003;14(5–6):353–357 [Google Scholar]
- 26.Tempalski B. Placing the dynamics of syringe exchange programs in the United States. Health Place. 2007;13(2):417–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tempalski B, Friedman R, Keem M, Cooper H, Friedman SR. NIMBY localism and national inequitable exclusion alliances: the case of syringe exchange programs in the United States. Geoforum. 2007;38(6):1250–1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson W. The New York Needle Trial: the politics of public health in the age of AIDS. Am J Public Health. 1991;81(11):1506–1517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spernak SM, Mintz M, Paulson J, et al. Neighborhood racial composition and availability of asthma drugs in retail pharmacies. J Asthma. 2005;42(9):731–735 [DOI] [PubMed] [Google Scholar]
- 30.Cooper HL, Bossak BH, Tempalski B, Friedman SR, Des Jarlais DC. Temporal trends in spatial access to pharmacies that sell over-the-counter syringes in New York City health districts: relationship to local racial/ethnic composition and need. J Urban Health. 2009;86(6):929–945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.New York State Department of Health Expanded syringe access program (ESAP): overview of the law and regulations. 2008. Available at: http://www.nyhealth.gov/diseases/aids/harm_reduction/needles_syringes/esap/overview.htm. Accessed January 7, 2009
- 32.Hutchinson SJ, Taylor A, Goldberg DJ, Gruer L. Factors associated with injecting risk behaviour among serial community-wide samples of injecting drug users in Glasgow 1990–94: implications for control and prevention of blood-borne viruses. Addiction. 2000;95(6):931–940 [DOI] [PubMed] [Google Scholar]
- 33.Rockwell R, Des Jarlais DC, Friedman SR, Perlis TE, Paone D. Geographic proximity, policy and utilization of syringe exchange programmes. AIDS Care. 1999;11(4):437–442 [DOI] [PubMed] [Google Scholar]
- 34.Bruneau J, Daniel M, Kestens Y, Zang G, Généreux M. Associations between HIV-related injection behaviour and distance to and patterns of utilisation of syringe-supply programmes. J Epidemiol Community Health. 2008;62(9):804–810 [DOI] [PubMed] [Google Scholar]
- 35.Schilling RF, Fontdevila J, Fernando D, El-Bassel N, Monterroso E. Proximity to needle exchange programs and HIV-related risk behavior among injection drug users in Harlem. Eval Program Plann. 2004;27(1):25–33 [Google Scholar]
- 36. Departments of Labor, Health and Human Services, and Education, and Related Agencies Appropriations Act, 2010 (Referred to Senate Committee After Being Received From House), HR 3293, 111th Cong, 1st Sess (2009)
- 37. Consolidated Appropriations Act of 2010, PL111–117 (2009)
- 38.New York State Expanded Syringe Access Demonstration Program Evaluation. New York, NY: New York Academy of Medicine; 2003 [Google Scholar]
- 39.Report on Syringe Access in New York State. New York, NY: New York State AIDS Advisory Council; 2005 [Google Scholar]
- 40.Des Jarlais DC, Perlis T, Arasteh K, et al. “Informed altruism” and “partner restriction” in the reduction of HIV infection in injecting drug users entering detoxification treatment in New York City, 1990–2001. J Acquir Immune Defic Syndr. 2004;35(2):158–166 [DOI] [PubMed] [Google Scholar]
- 41.United Hospital Fund Health Atlas. New York, NY: United Hospital Fund; 2005 [Google Scholar]
- 42.New York City Department of Health and Mental Hygiene New York City Health Department population estimates, 2000–2008. Available at: https://a816-healthpsi.nyc.gov/epiquery/EpiQuery/index.html. Accessed September 17, 2009
- 43.New York City Department of City Planning DCPLION. Available at: http://www.nyc.gov/html/dcp/html/bytes/applbyte.shtml. Accessed September 17, 2009
- 44.Des Jarlais DC, Perlis T, Friedman SR, et al. Behavioral risk reduction in a declining HIV epidemic: injection drug users in New York City, 1990–1997. Am J Public Health. 2000;90(7):1112–1116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Friedman SR, Ompad DC, Maslow C, et al. HIV prevalence, risk behaviors, and high-risk sexual and injection networks among young women injectors who have sex with women. Am J Public Health. 2003;93(6):902–906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marshall BD, Wood E, Li K, Kerr T. Elevated syringe borrowing among men who have sex with men: a prospective study. J Acquir Immune Defic Syndr. 2007;46(2):248–252 [DOI] [PubMed] [Google Scholar]
- 47.Des Jarlais DC, Braine N, Friedmann P. Unstable housing as a factor for increased injection risk behavior at US syringe exchange programs. AIDS Behav. 2007;11(6 Suppl):78–84 [DOI] [PubMed] [Google Scholar]
- 48.Montgomery SB, Hyde J, De Rosa CJ, et al. Gender differences in HIV risk behaviors among young injectors and their social network members. Am J Drug Alcohol Abuse. 2002;28(3):453–475 [DOI] [PubMed] [Google Scholar]
- 49.Salazar LF, Crosby RA, Holtgrave DR, et al. Homelessness and HIV-associated risk behavior among African American men who inject drugs and reside in the urban south of the United States. AIDS Behav. 2007;11(6 Suppl):70–77 [DOI] [PubMed] [Google Scholar]
- 50.Kottiri BJ, Friedman SR, Neaigus A, Curtis R, Des Jarlais DC. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. J Acquir Immune Defic Syndr. 2002;30(1):95–104 [DOI] [PubMed] [Google Scholar]
- 51.Bluthenthal RN, Do DP, Finch B, Martinez A, Edlin BR, Kral AH. Community characteristics associated with HIV risk among injection drug users in the San Francisco Bay Area: a multilevel analysis. J Urban Health. 2007;84(5):653–666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hartwig F, Dearing B. Exploratory Data Analysis. Newbury Park, CA: Sage; 1979 [Google Scholar]
- 53.Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. London, UK: Sage; 2002 [Google Scholar]
- 54.Singer J, Willett J. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003 [Google Scholar]
- 55.Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: inferential and graphical techniques. Multivariate Behav Res. 2005;40(3):373–400 [DOI] [PubMed] [Google Scholar]
- 56.Preacher K, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31(4): 437–448 [Google Scholar]
- 57.SAS/STAT, Version 9.2. [computer program] Cary, NC: SAS Institute; 2008 [Google Scholar]
- 58.ArcInfo, Version 9.3. [computer program] Redlands, CA: ESRI; 2006 [Google Scholar]
- 59.Fuller CM, Galea S, Caceres W, Blaney S, Sisco S, Vlahov D. Multilevel community-based intervention to increase access to sterile syringes among injection drug users through pharmacy sales in New York City. Am J Public Health. 2007;97(1):117–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Des Jarlais DC, McKnight C, Friedmann P. Legal syringe purchases by injection drug users, Brooklyn and Queens, New York City, 2000–2001. J Am Pharm Assoc (Wash). 2002;42(6 Suppl 2):S73–S76 [DOI] [PubMed] [Google Scholar]
- 61.Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Med Anthropol. 1997;18(1):61–83 [DOI] [PubMed] [Google Scholar]
- 62.Bluthenthal RN, Lorvick J, Kral AH, Erringer EA, Kahn JG. Collateral damage in the war on drugs: injection drug use. Int J Drug Policy. 1999;10(1):25–38 [Google Scholar]
- 63.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Soc Sci Med. 2005;61(3):673–684 [DOI] [PubMed] [Google Scholar]
- 64.Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Effects of an intensive street-level police intervention on syringe exchange program use in Philadelphia, PA. Am J Public Health. 2005;95(2):233–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Friedman SR, Cooper HL, Tempalski B, et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS. 2006;20(1):93–99 [DOI] [PubMed] [Google Scholar]
- 66.Wood E, Kerr T, Small W, Jones J, Schechter M, Tyndall MW. The impact of a police presence on access to needle exchange programs. J Acquir Immune Defic Syndr. 2003;34(1):116–118 [DOI] [PubMed] [Google Scholar]