Abstract
The prostaglandin endoperoxide synthase (PTGS) pathway is a potent driver of tumour development in humans by enhancing the biosynthesis and signalling of prostaglandin (PG) E2. PTGS2 expression and PGE2 biosynthesis is elevated in endometrial adenocarcinoma, however the mechanism whereby PTGS and PGE2 regulate endometrial tumour growth is unknown. Here we investigated (a) the expression profile of the PGE synthase enzymes (PTGES, PTGES-2, PTGES-3) and PGE receptors (PTGER1–4) in endometrial adenocarcinomas compared with normal endometrium and (b) the role of PTGER4 in endometrial tumorigenesis in vivo. We found elevated expression of PTGES2 and PTGER4 and suppression of PTGER1 and PTGER3 in endometrial adenocarcinomas compared with normal endometrium. Using WT Ishikawa endometrial adenocarcinoma cells and Ishikawa cells stably transfected with the full length PTGER4 cDNA (PTGER4 cells) xenografted in the dorsal flanks of nude mice, we show that PTGER4 rapidly and significantly enhances tumour growth rate. Coincident with enhanced PTGER4-mediated tumour growth we found elevated expression of PTGS2 in PTGER4 xenografts compared with WT xenografts. Furthermore we found that the augmented growth rate of the PTGER4 xenografts was not due to enhanced angiogenesis, but regulated by an increased proliferation index and hypoxia. In vitro, we found that PGE2 and hypoxia independently induce expression of PTGER4 indicating two independent pathways regulating prostanoid receptor expression. Finally we have shown that PGE2 and hypoxia synergise to promote cellular proliferation of endometrial adenocarcinoma cells.
Introduction
Endometrioid adenocarcinoma arising from the endometrial glandular epithelium is one of the leading causes of cancer-related morbidity in women world-wide [1], [2]. The onset of the disease occurs more frequently post menopause and is associated with a host of risk factors, including high levels of unopposed estrogen, endometrial hyperplasia and obesity [1].
Although the molecular mechanisms responsible for the initiation of the disease are multifactorial, there is now much evidence to substantiate genetic alterations and the inactivation of tumour suppressor genes in the neoplastic transformation of cells to facilitate uncontrolled proliferation and tumour growth [3]. Indeed one of the most common mutations in endometrial adenocarcinomas is located in the dual specificity phosphatase PTEN (phosphatase and tensin homologue deleted from chromosome ten) gene [2]. Animal models in which PTEN expression is inactivated in the endometrium have shown that loss of the PTEN function rapidly and unfailingly induces endometrial cancer [4]. Inactivation of PTEN function promotes protein kinase B (also called Akt) activation which in turn stimulates the activity of several target genes involved in cell proliferation [5]. One the major targets of Akt signalling in endometrial adenocarcinoma cells, is prostaglandin endoperoxide synthase (PTGS) 2 (also called cyclooxygenase 2) [4], [6].
PTGS2 converts arachidonic acid, the rate limiting substrate in the prostaglandin biosynthesis cascade to the unstable intermediate prostaglandin (PG)G2 which is subsequently converted to PGH2 [7]. In turn PGH2 is metabolised by terminal prostaglandin synthase enzymes, which are named according to the prostaglandin they biosynthesise. For example prostaglandin E synthase (PTGES) enzymes, of which there are three isoforms (PTGES, PTGES-2, PTGES-3) produce PGE2 [8]. PTGS2 expression is elevated in numerous neoplastic diseases including endometrial adenocarcinomas resulting in elevated biosynthesis of PGE2 [9], [10]. In vitro and in vivo model systems overexpressing PTGS2 have shown that PGE2 can promote tumorigenesis by altering cell cycle progression, inhibiting apoptosis and enhancing cellular proliferation [11], [12], [13]. Furthermore PGE2 can promote tumour progression by down-regulating tumour suppressor genes such as tuberous sclerosis-2 (TSC2) [14], P53 and retinoblastoma in epithelial cells [11].
Following biosynthesis, PGE2 is transported out of the cell where it binds to and activates PGE2 G protein-coupled receptors of which there are four isoforms PTGER 1–4 [15]. PTGER4 expression is elevated in numerous cancers where it can transduce pathways important for cancer cell survival and tumour progression, such as the Akt, extracellular signal regulated kinase (ERK1/2) and early growth response factor-1 [16], [17], [18]. The aim of this study was to identify the components of the PTGS-PGE2 pathway in endometrial adenocarcinomas which regulate tumour growth.
Here, we show suppression of PTGER1 and PTGER3 and elevated expression of PTGES2 and PTGER4 in endometrial adenocarcinomas compared with normal endometrium. We show that inoculation of nude mice with Ishikawa endometrial adenocarcinoma cells stably expressing PTGER4 promotes formation of tumour xenografts which grow at a significantly faster rate compared with tumours arising from WT control cells. Moreover these tumours displayed elevated expression of PTGS2 compared with tumours arising from WT Ishikawa cells. Morphometric and stereological analyses showed no difference in blood vessel density or VEGF expression in PTGER4 tumours compared with WT tumours indicating that PTGER4-mediated tumour growth was not a result of increased angiogenesis. The PTGER4 tumours displayed an increase in cellular proliferation and increased areas of hypoxia. Using in vitro models, we subsequently demonstrated that hypoxia and PGE2 synergise to induce expression of PTGER4 leading to increased cellular proliferation.
Materials and Methods
Ethics Statement
Ethical approval was obtained from Lothian Research Ethics Committee (LREC/07/S1103/32, LREC/05/S1103/29 and LREC/1999/6/4) and written informed consent was obtained from all subjects before tissue collection. All animal care and experimental protocols were approved by the animal ethics committee of the University of Edinburgh and the Home Office of the United Kingdom government under the guidelines of the Animals (Scientific Procedures) Act 1986.
Human tissue
Poorly (grade 3; n = 10), moderately (grade 2; n = 10) and well (grade 1; n = 9) differentiated endometrial adenocarcinoma tissues with clinical characteristics as described in Table 1 [19] were collected from women undergoing hysterectomy. All women had been pre-diagnosed on endometrial biopsy to have endometrial adenocarcinoma of the endometrioid type. The diagnosis of endometrial adenocarcinoma was confirmed histologically in all cases as defined in Table 1 and the percentage of tumour cells to stroma was estimated to be not less than 75%∶25%. Normal endometrium with clinical parameters as outlined in Table 2 from the proliferative (n = 10), early secretory (n = 10), mid secretory (n = 10) and late secretory (n = 10) phases of the menstrual cycle, was collected from women undergoing surgery for gynecological procedures in whom histological examination of endometrium was normal with no underlying endometrial pathology (Pipelle, Laboratoire CCD, France). All biopsies were dated according to stated last menstrual period (LMP) and confirmed by hormone analysis and histological assessment according to the criteria of Noyes et al. [20].
Table 1. Clinical parameters and tumour characteristics for well (n = 10), moderately (Mod, n = 10) and poorly differentiated (n = 10) endometrial adenocarcinomas.
| SAMPLE NO | GRADE | FIGO STAGE |
| 1 | Well | Ib |
| 2 | Well | Ib |
| 3 | Well | Ia |
| 4 | Well | Ic |
| 5 | Well | IIIa |
| 6 | Well | Ib |
| 7 | Well | Ib |
| 8 | Well | Ib |
| 9 | Well | Ia |
| 10 | Mod | Ic |
| 11 | Mod | Ic |
| 12 | Mod | Ia |
| 13 | Mod | Ib |
| 14 | Mod | IIb |
| 15 | Mod | Ib |
| 16 | Mod | Ic |
| 17 | Mod | IIb* |
| 18 | Mod | IIIa |
| 19 | Mod | Ib |
| 20 | Poor | Ia |
| 21 | Poor | IIIa |
| 22 | Poor | Ib |
| 23 | Poor | Ib |
| 24 | Poor | IIIa |
| 25 | Poor | Ib |
| 26 | Poor | Ib |
| 27 | Poor | IIIa |
| 28 | Poor | IIIa |
| 29 | Poor | IIb* |
All endometrial adenocarcinomas studied were of pure or predominantly of endometrioid type. There were no pure serous or clear cell subtypes in the series and none of the tumours showed carcinosarcoma.
*in these two samples myometrial invasion was <50%.
Table 2. Clinical parameters for normal endometrial samples from proliferative phase, early secretory, mid secretory and late secretory phase endometrium (n = 10).
| SAMPLE NO | HISTOLOGY | PROGESTERONE nmol/L | ESTRADIOL pmol/L |
| 1 | Proliferative | 4.26 | 339.38 |
| 2 | Proliferative | 2.22 | 641.37 |
| 3 | Proliferative | 4.62 | 525.00 |
| 4 | Proliferative | 4.57 | 495.00 |
| 5 | Proliferative | 2.82 | 214.00 |
| 6 | Proliferative | 1.78 | 400.00 |
| 7 | Proliferative | 4.80 | 204.00 |
| 8 | Proliferative | 3.12 | 731.00 |
| 9 | Proliferative | 2.32 | 1796.00 |
| 10 | Proliferative | 0.17 | 989.70 |
| 11 | Early Secretory | 63 | 353 |
| 12 | Early Secretory | 16.55 | 556 |
| 13 | Early Secretory | 63 | 458 |
| 14 | Early Secretory | 93.15 | 848 |
| 15 | Early Secretory | 9.03 | 90.43 |
| 16 | Early Secretory | 11.58 | 75.99 |
| 17 | Early Secretory | 10.371 | 876.16 |
| 18 | Early Secretory | 38.48 | 243.08 |
| 19 | Early Secretory | 26.74 | 768.92 |
| 20 | Early Secretory | 101.1 | 584 |
| 21 | Mid Secretory | 33.29 | 242.72 |
| 22 | Mid Secretory | 36.94 | 280.35 |
| 23 | Mid Secretory | 4.54 | 544.04 |
| 24 | Mid Secretory | 79.8 | 748 |
| 25 | Mid Secretory | 32.67 | 277 |
| 26 | Mid Secretory | 25.74 | 292 |
| 27 | Mid Secretory | 37.54 | 658 |
| 28 | Mid Secretory | 36.17 | 294.79 |
| 29 | Mid Secretory | 14.53 | 392 |
| 30 | Mid Secretory | 9.78 | 248.03 |
| 31 | Late Secretory | 0.47 | 0 |
| 32 | Late Secretory | 6.60 | 174.75 |
| 33 | Late Secretory | 8.36 | 326 |
| 34 | Late Secretory | 65.65 | 1075 |
| 35 | Late Secretory | 133.6 | 876 |
| 36 | Late Secretory | 3.85 | 55 |
| 37 | Late Secretory | 7.67 | 248.89 |
| 38 | Late Secretory | 20 | 410.91 |
| 39 | Late Secretory | 8.36 | 326 |
| 40 | Late Secretory | 65 | 1075 |
Cell culture
Wild-type (WT) Ishikawa cells (European Collection of Cell Culture, Wiltshire, UK) were maintained as described previously [14]. Stable PTGER4 transfectant cells (PTGER4 cells) were maintained under the same conditions with the addition of a maintenance dose of 200 µg/ml G418 (Calbiochem, UK).
PTGER4 amplification and Cell Transfections
The PTGER4 receptor cDNA clone and stable cell lines were constructed by Cytomix Ltd (Cambridge, UK). PTGER4 cDNA (GenBank Accession N0. D28472) was amplified by polymerase chain reaction (PCR) and the product was directionally cloned into the mammalian expression vector gWIZ3.0 (Gene Therapy Systems, Cambridge, UK) at the Hind III and Bam H1 restriction sites and the orientation of the construct confirmed by automated DNA sequencing. The PTGER4 cDNA was transfected into Ishikawa cells and individual cell populations were selected for with addition of 800 µg/ml G418. Full selection was confirmed by the 100% death of non-transfected control cells and five single PTGER4 sense clones were selected and expanded for Western blot analysis. The clones with the highest level of PTGER4 expression were expanded and stored in liquid nitrogen. Based on the relative quantification of PTGER4 expression, two sense clones (S20 and S22) exhibiting similar phenotypic and biochemical alterations were supplied. The results of our studies using the S22 clone are presented here.
cAMP Assay
PGE2 induced cAMP accumulation was determined by seeding 2×105 WT or PTGER4 cells/well in 6-well plates. The cells were serum-starved in the presence of 3 µg/ml of indomethacin. Thereafter, the cells were pre-treated with the phosphodiesterase inhibitor 3-isobutyl-1-methyl xanthine (IBMX; Sigma, Dorset, UK) to a final concentration of 0.2 mM in serum-free medium for 30 min. Cells were treated for 5 min with 100 nM PGE2, or left unstimulated (time 0). After incubation the cells were lysed in R&D Cell Lysis Buffer™ (R&D Systems, Oxford UK) and cAMP release was determined by ELISA using cAMP Kit (R&D Systems) according to manufacturer's protocol. Data are represented as mean ± SEM of three independent experiments.
Xenograft Experiments
WT or PTGER4 cells (2.5×106) were subcutaneously injected in a volume of 100 µl into the left and right flanks of ten CD1-Foxn1nu mice (Charles River, Tranent, UK). All animals were housed in individually ventilated cages.
The resulting tumours (n = 20 WT tumours and n = 20 PTGER4 tumours) were measured twice weekly by digital calipers. Tumour volume was calculated using the formula; Volume = 0.5×(vertical measurement/10)×(horizontal measurement/10)×(horizontal measurement/10). After a period of 35 days, the animals were sacrificed. Two hours prior to sacrifice, the animals received an intraperitoneal (i.p) injection of 50 mg/kg of 5-Bromo-deoxy Uridine (BrdU, Sigma, UK). One hour prior to sacrifice, the animals received an i.p injection of 60 mg/kg of Hypoxyprobe (pimonidazole hydrochloride; HPI, Inc, Burlington, MA, USA). The tumours were removed and half of each was placed in 4% neutral buffered formalin (NBF, Sigma, UK) and a quarter section was snap-frozen in QIAzol (Qiagen, Crawley, UK) for RNA extraction.
Quantitative RT-PCR
RNA from the tumours was extracted using the RNeasy Mini Kit (Qiagen). RNA samples were reverse-transcribed using VILO (Invitrogen, Paisley, UK) according to the manufacturer's guidelines. RT-PCR analysis of the genes of interest was carried out using an ABI Prism 7500 (Applied Biosystems, Warrington, UK). Primer and FAM (6-carboxyfluorescein)-labelled probe sequences are shown in Table 3. For PTGES3, primer only amplification products were detected using SYBR™ Green (Applied Biosystems) incorporation during the PCR reaction. Gene expression was normalised to 18S ribosomal RNA (Applied Biosystems) as an internal standard. Results are expressed relative to a standard (pooled normal human endometrial tissue cDNA) included in all reactions. Data are represented as mean ± SEM.
Table 3. Sequences of Taqman primers and probe.
| Gene Symbol | Position | Nucleotide Sequence (5′-3′) |
| HIF-1α | Forward | CGC ATC TTG G ATA AGG CCT CTG T |
| Reverse | AAT CAC CAG G CAT CCA GAA GTT TC | |
| PTGER1 | Forward | AGA TGG TGG GCC AGC TTG T |
| Reverse | GCC ACC AAC ACC AGC ATT G | |
| PTGER2 | Forward | GAC CGC TTA CCT GCA GCT GTA C |
| Reverse | TGA AGT TGC AGG CGA GCA | |
| PTGER3 | Forward | GAC GGC CAT TCA GCT TAT GG |
| Reverse | TTG AAG ATC ATT TTC AAC ATC ATT ATC A | |
| PTGER4 | Forward | ACG CCG CCT T ACT CCT ACA TG |
| Reverse | AGA GGA CGGG TGG CGA GAA T | |
| PTGES | Forward | TCA ACT GTG G ATG GCA AGA GC |
| Reverse | CTA ACC TCC C TGA GCC CTC CT | |
| PTGES1 | Forward | CGG AGG CCC CCA GTA TTG |
| Reverse | GGG TAG ATG GTC TCC ATG TCG TT | |
| PTGES2 | Forward | CCT CAT CAG CAA GCG ACT |
| Reverse | CCA CTT GTC AGC AGC CTC A |
Confocal Immunofluorescent microscopy
Approximately 1.0×104 WT or PTGER4 cells were seeded in chamber slides and fixed in 100% ice-cold methanol. Following fixing, cells were washed in TBS (50 mM Tris-HCl, 150 mM NaCl pH 7.4) and blocked using 5% normal swine serum diluted in TBS. Subsequently, the cells were incubated with polyclonal rabbit anti-PTGER4 antibody at a dilution of 1∶50 at 4°C for 18 hours. Control cells were incubated with rabbit immunoglobulin (IgG). Thereafter, the cells were incubated with secondary swine anti-rabbit tetramethyl rhodamine isothyocyanate (TRITC; Dako Corp, High Wycombe, UK) at 25°C for 20 mins. Cells were then mounted in Permafluor (Immunotech-Coulter, Buckinghamshire, UK) and coverslipped prior to imaging.
Immunohistochemistry
Tumour tissue was embedded in paraffin wax and sections of 5 µm thickness of WT (n = 10) and PTGER4 (n = 10) tumours were cut and mounted on to coated slides. The sections were de-waxed and rehydrated through graded alcohols before antigen retrieval in 0.01 M citrate phosphate buffer. Immunostaining was performed using the Vision Biosystems Bond Immunostaining Robot (Leica Microsystems, Wezlar, Germany) under normal operating conditions as described in our previous study [21] using a sheep-anti-BrdU antibody (1∶6000; Fitzgerald, UK) or Hypoxyprobe mouse monoclonal antibody (Vision Biosystems mouse polymer protocol at 1∶50 dilution). For CD31, sections were blocked in normal porcine serum and incubated with rabbit-anti-CD31 (1∶250; Abcam, Cambridge, UK) overnight at 4°C. Sections were incubated with a 1∶250 dilution of swine-anti-rabbit biotinlyated secondary antibody (DAKO, Cambridge, UK). The sections were then incubated with streptavidin peroxidase (1∶1000) and detected using 3-3′ diaminobenzidine (DAB; DAKO) prior to imaging.
Stereological analysis
Images were captured using a ×40 plan apo objective from a BH2 microscope (Olympus, Tokyo, Japan) fitted with an automatic stage (Prior Scientific Instruments Ltd., Cambridge, UK) and video camera (HV-C20; Hitachi, Tokyo, Japan) and were analyzed with Image-Pro Plus 4.5.1 software with a Stereology 5.0 plug-in (Media Cybernetics, Wokingham, Berkshire, UK). 100 random fields of view were counted for each tumour section (n = 5 WT and PTGER4 tumour sections for Hypoxyprobe counts, n = 7 tumour sections each for BrdU counts and n = 11 tumour sections each for CD31 counts).
Hypoxia experiments
Ishikawa WT and PTGER4 cells were plated at a density of 2.5×105 cells per well in triplicate in 6 well plates. Cells were cultured under normoxic conditions (20% oxygen) in a standard incubator at 37°C, 95% air/5% CO2 or placed in hypoxia chamber (1% oxygen) at 37°C, 80% N2/10% H2/10% CO2 for 24 hours in the presence/absence of 8.4 µM indomethacin [22]. RNA was extracted, reverse transcribed and PTGER4 expression was determined by quantitative RT-PCR as described above. In the case of hypoxic cells, these manipulations were performed inside the hypoxia chamber to avoid reoxygenation. Data are represented as mean ± SEM of four independent experiments.
Proliferation assay
Ishikawa WT and PTGER4 cells were plated at a density of 5.0×103 cells per well in 96 well plates. The following day cells were incubated in serum free medium in the absence/presence of 8.4 µM indomethacin. Thereafter cells were treated with vehicle or 1 µM PGE2 in the presence/absence of indomethacin. Plates were incubated under normoxic or hypoxic conditions as described above for 24 hours. Cell proliferation was measured using the CellTitre96Aqueous One Solution Proliferation Reagent (Promega, Southampton, UK) as per the manufacturer's protocol. Data are represented as mean ± SEM of four independent experiments.
Statistics
Data were analysed using an unpaired t-test or a one-way ANOVA with Tukey's multiple comparison post test where applicable (GraphPad Prism, GraphPad Software Inc., USA). Box and whisker plots: Boxes represent the data lying within the 5th to the 95th percentile and the whiskers represent the minimum and maximum values.
Results
Expression profiling of the PGE2-PTGER signalling pathway in endometrial adenocarcinomas
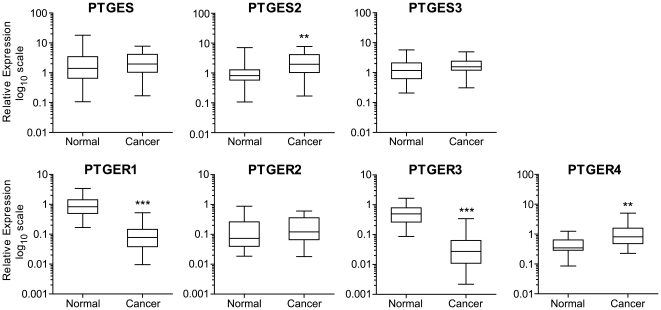
We recently undertook a comprehensive analysis of the expression profile of the prostaglandin enzymes and receptors in normal endometrium across the menstrual cycle [23]. Here, we undertook a comprehensive analysis of the expression profile of the PGE synthase enzymes (PTGES, -2, -3) and E-series prostanoid receptors (PTGER1–4) in endometrial adenocarcinoma by quantitative RT-PCR analysis (Figure 1 and Figure S1). We found no significant difference in expression patterns of the synthase enzymes or prostanoid receptors between the different grades of endometrial adenocarcinoma investigated and henceforth pooled the data for analysis. We found elevated expression of PTGES2 (P<0.01) and PTGER4 (P<0.01) in all grades of endometrial adenocarcinomas compared with pooled normal endometrium. Interestingly, within our sample set, the present study revealed a significant decrease in the expression of PTGER1 (P<0.001) and PTGER3 (P<0.001), which are reported to differentially couple to Gq/11 and Gi proteins and which mobilises intracellular calcium and suppresses cAMP respectively. These results indicate a bias towards the PGE2-PTGER4-cAMP pathway as a potential driver of endometrial cancer.
Figure 1. Expression profile of the PTGES-PTGER system in endometrial adenocarcinoma and normal endometrium.
mRNA expression of PGE2 synthase isoforms (PTGES, -2, -3) and E-series prostaglandin receptors (PTGER1–4) in normal endometrium (n = 40; comprising a pool of proliferative n = 10; early secretory n = 10; mid-secretory n = 10 and late secretory n = 10 phase endometrium) and endometrial cancer (n = 29; comprising a pool of poorly differentiated n = 10, moderately differentiated n = 10 and well differentiated endometrial adenocarcinoma n = 9). **, *** represent significance at P<0.01 and P<0.001 for cancer vs normal.
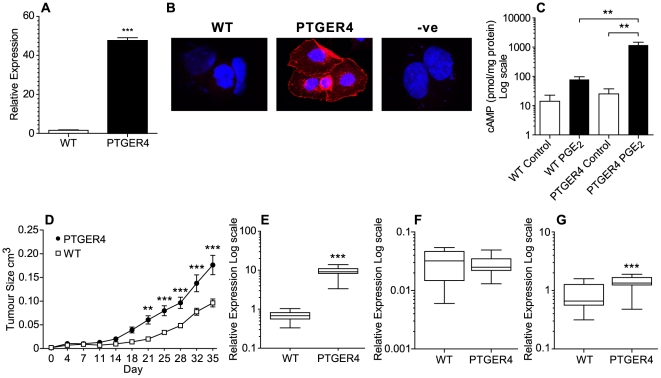
PTGER4 enhances growth of tumour xenografts in vivo
In endometrial adenocarcinomas, PTGER4 is localised to the neoplastic epithelial compartment [9]. To elucidate a role for the PGE2-PTGER4-cAMP pathway in endometrial tumour growth, we stably transfected Ishikawa endometrial epithelial cells with the full length PTGER4 cDNA transcript. Quantitative RT-PCR analysis showed elevated PTGER4 expression in PTGER4 cells compared with WT cells (Figure 2A, P<0.001). Using immunohistochemistry and confocal laser microscopy, we localised the site of expression of the translated PTGER4 transgene to the plasma membrane compartment (Figure 2B).
Figure 2. PTGER4 enhances tumour growth in a nude mouse xenograft model.
(A) PTGER4 mRNA expression in WT Ishikawa cells compared with Ishikawa cells stably transfected with the full length PTGER4 cDNA transcript (n = 3). (B) Immunolocalisation of PTGER4 expression in WT and PTGER4 stable cell lines. (C) cAMP accummulation in WT and PTGER4 stable cell lines in response to treatment with 100 nM PGE2 for 0 or 5 minutes (n = 3). (D) Tumour growth in CD1-Foxn1nu mice following dorsal flank injection with either Ishikawa WT or PTGER4 stable cells. Tumour growth in WT (n = 20) and PTGER4 (n = 20) xenografts was monitored over a 35 day period as described in the methods. (E) PTGER4 (F) PTGS1 and (G) PTGS2 mRNA expression in either Ishikawa WT (n = 10) or PTGER4 (n = 10) xenograft tumours. **, *** represent significance at P<0.01 and P<0.001.
PTGER4 couples to Gs resulting in increased cAMP accumulation. We assessed functionality of the transfected PTGER4 cDNA transcript by cAMP ELISA in response to treatment with 100 nM PGE2 for 5 minutes. A significant increase in cAMP accumulation was observed in PTGER4 cells compared with WT cells following treatment with PGE2 (Figure 2C, P<0.05).
To assess the role of PTGER4 in endometrial cell tumorigenesis in vivo, we xenografted either WT cells or PTGER4 cells into the dorsal flanks of CD1-Foxn1nu mice and measured the resulting tumour growth over a 35 day period. We found a significant divergence in the growth rate of the tumours arising from the respective cell types, with PTGER4 xenograft tumours growing at a significantly higher rate after day 21 compared with WT xenograft tumours (Figure 2D; ** p<0.01 to *** p<0.001 comparing the volume of PTGER4 xenograft tumours versus WT xenograft tumours). We confirmed elevated PTGER4 expression levels in PTGER4 xenograft tumours compared with WT xenograft tumours by quantitative RT-PCR analysis (Figure 2E, P<0.001) indicating that expression of the transgene was maintained in vivo.
Since tumour growth in vivo has been shown to be regulated by the PTGS-PGE2 pathway [24], we next assessed the expression of the prostaglandin endoperoxide synthase enzymes responsible for producing PGE2. We found elevated expression of PTGS2 (Figure 2G, P<0.001) but not PTGS1 (Figure 2F) in PTGER4 xenograft tumours compared with WT tumours.
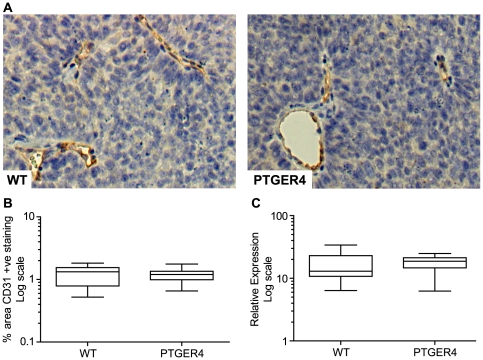
Xenograft tumour growth in PTGER4 tumours is not due to enhanced angiogenesis
The PTGS-PG pathway has been shown to promote tumorigenesis by enhancing angiogenesis [25], [26], [27]. We investigated whether the enhanced growth observed in PTGER4 tumours compared with WT tumours was a result of increased angiogenesis. We investigated blood vessel density by immunohistochemistry (Figure 3A) and quantitative stereology (Figure 3B) using the endothelial cell marker CD31. We found no difference in immunoreactive staining for CD31 as a percentage area of the tumour in PTGER4 tumours compared with WT tumours (Figure 3B). Since VEGF is the progenitor factor responsible for angiogenesis [28], we investigated whether VEGF levels were altered between the WT and PTGER4 tumours. Similarly, we found no significant difference in VEGF mRNA levels between the two groups, confirming that the enhanced tumour growth in PTGER4 tumours was not a result of increased angiogenesis (Figure 3C).
Figure 3. Differential tumour growth between WT and PTGER4 xenograft tumours is not due to enhanced angiogenesis.
(A) Detection of blood vessels in WT (n = 11 sections) and PTGER4 (n = 11 sections) xenograft tumours as determined by immuno-staining with the endothelial cell marker CD31. (B) Quantitative stereology of blood vessel density in WT and PTGER4 xenograft tumours as determined by percentage area positively stained for CD31. (C) mRNA expression of the angiogenic factor VEGF in WT (n = 10) and PTGER4 (n = 10) xenograft tumours.
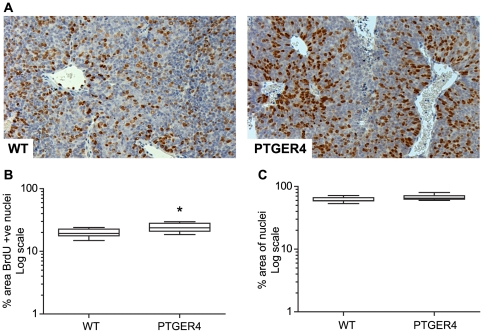
Cellular proliferation is enhanced in PTGER4 xenograft tumours
We assessed whether the rapid increase in growth and volume of the PTGER4 tumours compared to WT tumours was due to an enhanced rate of cellular proliferation of PTGER4 cells in vivo. Immunohistochemistry (Figure 4A) and quantitative stereology (Figure 4B) revealed a significant increase in proliferation index in epithelial cells as observed by incorporation of BrdU in PTGER4 tumours compared with WT tumours (Figure 4B, P<0.05). Furthermore we found no alteration in tumour cell density per unit area between PTGER4 tumours and WT tumours (Figure 4C). This suggests that the larger PTGER4 tumours were a result of hyperplasia rather than hypertrophy or non-proliferative tumour expansion.
Figure 4. Cellular proliferation is enhanced in PTGER4 xenograft tumours.
(A) Immunohistochemistry for detection of cellular proliferation in WT (n = 7 sections) and PTGER4 (n = 7 sections) xenograft tumours as determined by staining for BrdU incorporation in the nuclei. (B) Quantitative stereology of cellular proliferation in WT and PTGER4 xenograft tumours as determined by percentage area positively stained for BrdU incorporation in the cell nuclei. (C) Quantitative stereology of cell density in WT and PTGER4 xenograft tumours as determined by percentage area stained positive for nuclear counterstain. * represents significance at P<0.05.
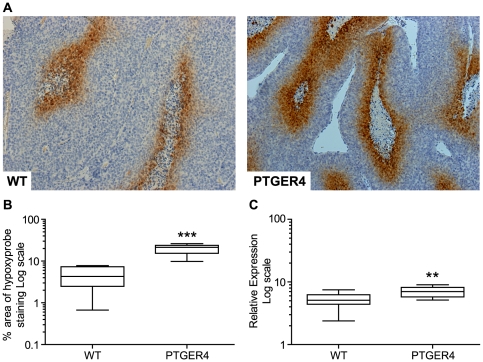
PTGER4 xenograft tumours display an increased area of hypoxia
Hypoxia is a common recognised driver in many solid tumours and is thought to contribute to development of endometrial adenocarcinoma [29]. We assessed whether the level of hypoxia was altered in the tumours. We found PTGER4 tumours to have increased areas of hypoxia in comparison to WT tumours as indicated by the immunoreactivity for the Hypoxyprobe, pimonidazole, per area of tumour investigated (Figure 5A and 5B, P<0.001). Increased tissue hypoxia in the PTGER4 tumours compared with WT tumours is also supported by quantitative RT-PCR analysis demonstrating higher expression of the hypoxia inducible factor HIF1α (Figure 5C, P<0.01).
Figure 5. PTGER4 xenograft tumours display increased areas of hypoxia compared with WT control.
Immunohistochemistry for detection of hypoxia in WT (n = 5 sections) and PTGER4 (n = 5 sections) xenograft tumours as determined by staining for the Hypoxyprobe pimonidazole. (B) Quantitative stereology of hypoxia in WT and PTGER4 xenograft tumours as determined by percentage area stained positive for Hypoxyprobe. (C) mRNA expression of the hypoxia inducible factor HIF1α in WT (n = 10) and PTGER4 (n = 10) xenograft tumours. **, *** represents significance at P<0.01 and P<0.001 for PTGER4 versus WT respectively.
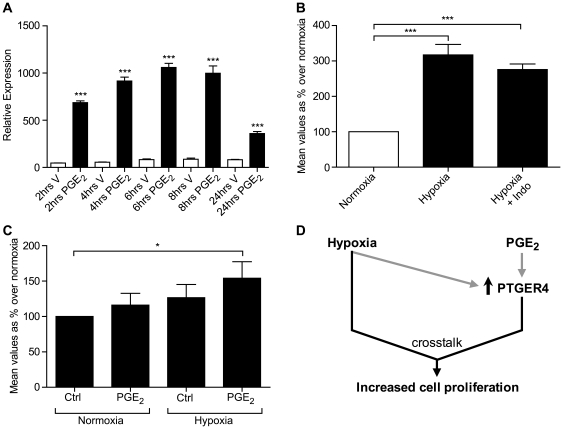
Hypoxia and PGE2 via PTGER4 crosstalk to promote cellular proliferation
Since we found PTGER4 tumours to have an increased proliferation index and hypoxia, we investigated the molecular mechanism regulating PTGER4 expression and proliferation of PTGER4 cells in vitro and the contribution of hypoxia to this. We found that treatment of PTGER4 cells with 100 nM PGE2 rapidly induced expression of PTGER4 at all time points investigated (Figure 6A, P<0.001). Furthermore, we found that incubation of PTGER4 cells, under hypoxic conditions also induced PTGER4 mRNA expression (Figure 6B, P<0.001). This hypoxia-induced expression of PTGER4 was independent of the PTGS-PG system, as co-incubation of cells with the dual PTGS enzyme inhibitor indomethacin had no effect on PTGER4 expression induced by hypoxia (Figure 6B, P<0.001). These data indicate two independent regulators of PTGER4 expression, the PTGS-PG system and hypoxia induced pathways. Finally we investigated the impact of PGE2 signaling and hypoxia on proliferation of PTGER4 cells in vitro. We have shown that neither PGE2 nor hypoxia alone can promote proliferation of PTGER4 cells. However, proliferation was significantly elevated following culture of cells with PGE2 and hypoxia in combination (Figure 6C, P<0.05).
Figure 6. Mechanism of regulation of cellular proliferation in PTGER4 cells in vitro.
(A) PTGER4 mRNA expression in PTGER4 cells treated with vehicle or 100 nM PGE2 for 2, 4, 6, 8 and 24 hours (n = 3). (B) PTGER4 expression in PTGER4 cells grown for 24 hours under normoxic and hypoxic conditions, in the absence or presence of the PTGS enzyme inhibitor indomethacin (n = 4). (C) Cellular proliferation in PTGER4 cells grown for 24 hours under normoxic (N) or hypoxic (H) conditions in the absence or presence of 1 µM PGE2 (n = 4). (D) Schematic diagram of findings demonstrating that hypoxia and PGE2 both independently elevate PTGER4 expression and synergise to enhance proliferation of PTGER4 cells. *, *** represent significance at P<0.05 and P<0.001 respectively.
Discussion
The PTGS-PG pathway is a potent driver of tumorigenesis in several cancers, including colon, prostate and breast [30], [31], [32], [33]. Expression of PTGS enzymes and biosynthesis of PGE2 is elevated in cancers of the female reproductive tract, including endometrial and cervical carcinomas [9], [10], [34]. These findings indicate that PGE2, via specific E-series prostanoid receptors may drive the development and progression of reproductive tract cancer in a similar manner to other solid tumours.
We undertook a comprehensive analysis of the expression profile of the PTGES-PGE2-PTGER system in normal endometrium across the menstrual cycle and endometrial adenocarcinoma of all grades. As the endometrium of post-menopausal women is no longer under normal hormonal control, the tissue is atrophic and rarely attainable for analysis, we chose normal endometrium as our comparator. We found a variation in the expression of the PTGES-PTGER system across the menstrual cycle, as shown in Figure S1 and is discussed in our recent study [23]. However, of particular significance to this study was the observation of a significant increase in expression of PTGER4 in endometrial cancer compared with normal endometrium across the menstrual cycle. These findings using a substantially larger sample size are consistent with our original observations for expression of these proteins in neoplastic epithelial cells in endometrial cancer [9]. However, more interestingly, within this sample set we found a significant reduction in the expression patterns of PTGER1 and PTGER3 in endometrial adenocarcinomas compared with normal endometrium. These two G protein-coupled receptors differentially couple with Gq and Gi respectively resulting in activation of inositol 1,4,5 trisphosphate and suppression of cAMP [35]. The suppression of these receptors and augmentation of PTGER4, strongly suggest that PGE2, produced via PTGS and PTGES2, is a driver of endometrial tumour development via the activation of PTGER4 and initiation of cAMP signalling. Indeed, PTGER4 has been demonstrated to promote human lung and colorectal cancer cell growth [30], [31]. Moreover antagonism of PTGER4 signalling with small molecule receptor antagonists or RNA interference has been shown to inhibit cell growth, proliferation, invasion [33] and metastasis of breast cancer cells [32].
To determine a role for PTGER4 in endometrial tumour development, we stably transfected the full length PTGER4 cDNA transcript into Ishikawa endometrial epithelial cells. We demonstrated translation and functionality of the PTGER4 transgene in Ishikawa cells by immunohistochmistry and cAMP assay and showed that the protein was trafficked to the expected plasma membrane compartment. We investigated the impact of PTGER4 on endometrial tumour development in vivo using a nude mouse model. CD1-Foxn1nu mice were xenografted with WT or PTGER4 cells and xenograft tumour growth was measured over a 35 day period. We found that PTGER4 cells grew at a faster rate resulting in tumours of approximately twice the size compared to WT tumours. Furthermore, higher PTGER4 expression was maintained in PTGER4 tumour xenografts compared with xenografts from WT cells indicating that stability of the transgene was maintained throughout the duration of the experiment. Interestingly, we found that expression of PTGS2 but not PTGS1 was elevated in PTGER4 tumour xenografts compared with WT xenografts. These observations, together with our previous findings showing elevated expression of PTGS2, PGES2 and PGE2 in endometrial cancer [9] strongly support a role for PG in driving endometrial tumorigenesis via the PTGER4-cAMP pathway similar to observations in colon cancer cells [30], [36]. Furthermore, other signalling pathways may synergise with or augment PTGER4 signalling in vivo to promote the major increase in proliferation we observed in mice xenografts. For example, we have recently shown that multiple PG ligands can converge on the same prostanoid receptor to regulate gene transcription in vitro [37]. In addition we have shown that the PTGER2 and PTGFR receptors can crosstalk via the Gs and Gq pathways to enhance cAMP signalling and target gene transcription in endometrial adenocarcinoma cells in vitro [38]. It is plausible that similar mechanisms may regulate PTGER4 signalling in vivo to promote endometrial tumour cell growth.
Elevated PTGS2 expression and PGE2 biosynthesis and signalling has been shown to promote tumorigenesis by enhancing expression of angiogenic factors such as VEGF and increasing angiogenesis [27], [39]. We investigated whether the enhanced growth rate and tumour size in the PTGER4 xenografts compared with WT was due to an enhancement in the elaboration of vascular network to support tumour growth by enhancing nutrient supply and oxygen. However, surprisingly we found no difference in the blood vessel density between the PTGER4 compared with WT tumours as indicated by staining for the endothelial cell marker CD31 or expression of vascular endothelial growth factor. These findings indicate that the observed increase in tumour growth between WT and PTGER4 xenografts was not a consequence of enhanced angiogenesis.
Endometrial cancer growth at the invasive front is regulated by a higher rate of cellular proliferation, driven by the alteration in cell cycle regulation [40], [41]. Although PGE2 has been shown to inhibit cellular proliferation in certain cell types [42], blockade of PTGER4 expression inhibits both proliferation and invasion of human inflammatory breast cancer cells [33]. Moreover, alteration in cell cycle regulation and cellular proliferation is known to be regulated in colon cancer cells by the PTGS-PG-PTGER4 pathway [11], [36]. In accordance with these observations, we have found that the elevated growth rate of PTGER4 xenograft tumours in our study is mediated by an increase in the rate of cellular proliferation as indicated by an increase in the incorporation of BrdU in the nuclei of PTGER4 tumour xenografts compared with WT xenografts. Furthermore, we confirmed that the tumour growth was mediated by hyperplasia, rather than hypertrophy or non-proliferative tumour expansion such as enhanced cell migration, since we found no difference in the density of cells in PTGER4 xenograft tumours compared with WT tumours.
Since we found no alteration in angiogenesis, but rather an increase in cellular proliferation, we hypothesised that the PTGER4 xenograft tumours had a higher metabolic demand compared with WT tumours. This would impose higher oxygen and nutrient requirement, which coupled with absence of an increase in angiogenesis, would result in increased hypoxia. Since energy metabolism in cancer cells is regulated in part by hypoxia [43], and hypoxia is a well known driver of tumorigenesis, we investigated levels of hypoxia between the two groups. We found that the PTGER4 xenograft tumours had increased areas of hypoxia as determined by the immunoreactivity for the hypoxyprobe pimonidazole per area of tumour investigated. Moreover we found elevated expression of the hypoxia inducible factor HIF1α in PTGER4 xenografts. Hypoxia inducible factors are well recognised drivers in the tumour microenvironment. They have been shown to induce VEGF expression to promote angiogenesis and tumorigenesis [44]. Furthermore, HIF1α is induced by low oxygen levels and is elevated in fast growing tumours and can activate the inflammatory PTGS-PG system and enhance cellular proliferation [43], [45]. Although we didn't find a correlation with hypoxia and VEGF between the WT and PTGER4 xenografts in our study, it is plausible that hypoxia can induce VEGF equally in both groups early on during tumour growth independent of PTGER4 when vascular networks are forming. Since we didn't find any difference in VEGF expression between WT and PTGER4 xenografts at the time of analysis, it is possible that VEGF regulation by hypoxia in WT and PTGER4 xenografts was already at maximal at the time of analysis in our study.
Our in vivo data suggest that endometrial adenocarcinoma growth is regulated by the PTGER4 pathway and hypoxia. To investigate the mechanism and crosstalk whereby PTGER4 and hypoxia could regulate cellular proliferation in endometrial adenocarcinoma cells, we used our PTGER4 stable cell line in vitro. We found that PGE2 could induce expression of PTGER4, indicating a positive feedback system induced by the PTGS-PGE2 synthase-PGE2 pathway to maintain PTGER4 expression. Furthermore we found that under conditions of low oxygen tension, PTGER4 expression could similarly be induced independently of the PTGS-PG system. These findings indicate two independent pathways which could drive elevated expression of PTGER4. Perhaps most strikingly, we found that neither pathway alone could significantly induce cellular proliferation, but were required to synergise to promote cellular proliferation as outlined schematically in Figure 6D.
Taken together, our data for the first time highlight a role for PTGER4 in endometrial tumour development. Furthermore our data propose a novel molecular mechanism whereby PGE2 biosynthesis, driven by elevated expression of PTGS2 in endometrial adenocarcinoma cells, and hypoxia synergise to increase PTGER4 expression and subsequently enhance cell proliferation and tumour growth.
Supporting Information
Expression profile of the PTGES-PTGER system in endometrial adenocarcinoma and normal endometrium. mRNA expression of PGE2 synthase isoforms (PTGES, -2, -3) and E-series prostaglandin receptors (PTGER1–4) in normal endometrium (n = 40; comprising of proliferative n = 10; early secretory n = 10; mid-secretory n = 10 and late secretory n = 10 phase endometrium) and endometrial cancer (n = 29; comprising poorly differentiated n = 10, moderately differentiated n = 10 and well differentiated endometrial adenocarcinoma n = 9). *, **, *** represent significance at P<0.05, P<0.01 and P<0.001.
(TIF)
Acknowledgments
We would like to thank Mike Millar, Shelia MacPherson, Arantza Esnal and Nancy Evans (Histology Department, MRC HRSU) for their expert assistance and Ted Pinner (CRB Visual Aids, MRC HRSU) for graphic design. We thank Professor Richard Anderson and Anne Saunderson for patient recruitment and tissue collection.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by Medical Research Council core funding (U.1276.00.004.00002.01) awarded to H.N.J. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Doll A, Abal M, Rigau M, Monge M, Gonzalez M, et al. Novel molecular profiles of endometrial cancer-new light through old windows. J Steroid Biochem Mol Biol. 2008;108:221–229. doi: 10.1016/j.jsbmb.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 2.Di Cristofano A, Ellenson LH. Endometrial carcinoma. Annu Rev Pathol. 2007;2:57–85. doi: 10.1146/annurev.pathol.2.010506.091905. [DOI] [PubMed] [Google Scholar]
- 3.Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/s0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 4.Daikoku T, Hirota Y, Tranguch S, Joshi AR, DeMayo FJ, et al. Conditional loss of uterine Pten unfailingly and rapidly induces endometrial cancer in mice. Cancer Res. 2008;68:5619–5627. doi: 10.1158/0008-5472.CAN-08-1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luo J, Manning BD, Cantley LC. Targeting the PI3K-Akt pathway in human cancer: rationale and promise. Cancer Cell. 2003;4:257–262. doi: 10.1016/s1535-6108(03)00248-4. [DOI] [PubMed] [Google Scholar]
- 6.St-Germain ME, Gagnon V, Mathieu I, Parent S, Asselin E. Akt regulates COX-2 mRNA and protein expression in mutated-PTEN human endometrial cancer cells. Int J Oncol. 2004;24:1311–1324. [PubMed] [Google Scholar]
- 7.Marnett LJ, Rowlinson SW, Goodwin DC, Kalgutkar AS, Lanzo CA. Arachidonic acid oxygenation by COX-1 and COX-2. Mechanisms of catalysis and inhibition. J Biol Chem. 1999;274:22903–22906. doi: 10.1074/jbc.274.33.22903. [DOI] [PubMed] [Google Scholar]
- 8.Murakami M, Nakashima K, Kamei D, Masuda S, Ishikawa Y, et al. Cellular prostaglandin E2 production by membrane-bound prostaglandin E synthase-2 via both cyclooxygenases-1 and -2. J Biol Chem. 2003;278:37937–37947. doi: 10.1074/jbc.M305108200. [DOI] [PubMed] [Google Scholar]
- 9.Jabbour HN, Milne SA, Williams ARW, Anderson RA, Boddy SC. Expression of COX-2 and PGE synthase and synthesis of PGE2 in endometrial adenocarcinoma: a possible autocrine/paracrine regulation of neoplastic cell function via EP2/EP4 receptors. Br J Cancer. 2001;85:1023–1031. doi: 10.1054/bjoc.2001.2033. [DOI] [PubMed] [Google Scholar]
- 10.Tong BJ, Tan J, Tajeda L, Das SK, Chapman JA, et al. Heightened expression of cyclooxygenase-2 and peroxisome proliferator-activated receptor-delta in human endometrial adenocarcinoma. Neoplasia. 2000;2:483–490. doi: 10.1038/sj.neo.7900119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DuBois RN, Shao J, Tsujii M, Sheng H, Beauchamp RD. G1 delay in cells overexpressing prostaglandin endoperoxide synthase-2. Cancer Res. 1996;56:733–737. [PubMed] [Google Scholar]
- 12.Tsuji S, Kawano S, Sawaoka H, Takei Y, Kobayashi I, et al. Evidences for involvement of cyclooxygenase-2 in proliferation of two gastrointestinal cancer cell lines. Prostaglandins Leukot Essent Fatty Acids. 1996;55:179–183. doi: 10.1016/s0952-3278(96)90095-2. [DOI] [PubMed] [Google Scholar]
- 13.Tsujii M, DuBois RN. Alterations in cellular adhesion and apoptosis in epithelial cells overexpressing prostaglandin endoperoxide synthase 2. Cell. 1995;83:493–501. doi: 10.1016/0092-8674(95)90127-2. [DOI] [PubMed] [Google Scholar]
- 14.Sales KJ, Battersby S, Williams AR, Anderson RA, Jabbour HN. Prostaglandin E2 mediates phosphorylation and down-regulation of the tuberous sclerosis-2 tumor suppressor (tuberin) in human endometrial adenocarcinoma cells via the Akt signaling pathway. J Clin Endocrinol Metab. 2004;89:6112–6118. doi: 10.1210/jc.2004-0892. [DOI] [PubMed] [Google Scholar]
- 15.Jabbour HN, Sales KJ. Prostaglandin receptor signalling and function in human endometrial pathology. Trends Endocrinol Metab. 2004;15:398–404. doi: 10.1016/j.tem.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Regan JW. EP(2) and EP(4) prostanoid receptor signaling. Life Sci. 2003;74:143–153. doi: 10.1016/j.lfs.2003.09.031. [DOI] [PubMed] [Google Scholar]
- 17.Fujino H, Regan JW. Prostanoid receptors and phosphatidylinositol 3-kinase: a pathway to cancer? Trends Pharmacol Sci. 2003;24:335–340. doi: 10.1016/S0165-6147(03)00162-7. [DOI] [PubMed] [Google Scholar]
- 18.George RJ, Sturmoski MA, Anant S, Houchen CW. EP4 mediates PGE2 dependent cell survival through the PI3 kinase/AKT pathway. Prostaglandins Other Lipid Mediat. 2007;83:112–120. doi: 10.1016/j.prostaglandins.2006.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sales KJ, Grant V, Cook IH, Maldonado-Perez D, Anderson RA, et al. Interleukin-11 in endometrial adenocarcinoma is regulated by prostaglandin F2alpha-F-prostanoid receptor interaction via the calcium-calcineurin-nuclear factor of activated T cells pathway and negatively regulated by the regulator of calcineurin-1. Am J Pathol. 2010;176:435–445. doi: 10.2353/ajpath.2010.090403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noyes RW, Hertig AT, Rock J. Dating the endometrial biopsy. Fertil Steril. 1950;1:3–25. doi: 10.1016/j.fertnstert.2019.08.079. [DOI] [PubMed] [Google Scholar]
- 21.Sales KJ, Maldonado-Perez D, Grant V, Catalano RD, Wilson MR, et al. Prostaglandin F(2alpha)-F-prostanoid receptor regulates CXCL8 expression in endometrial adenocarcinoma cells via the calcium-calcineurin-NFAT pathway. Biochim Biophys Acta. 2009;1793:1917–1928. doi: 10.1016/j.bbamcr.2009.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hirani N, Antonicelli F, Strieter RM, Wiesener MS, Ratcliffe PJ, et al. The regulation of interleukin-8 by hypoxia in human macrophages–a potential role in the pathogenesis of the acute respiratory distress syndrome (ARDS). Mol Med. 2001;7:685–697. [PMC free article] [PubMed] [Google Scholar]
- 23.Catalano RD, Wilson MR, Boddy SC, Jabbour HN. Comprehensive expression analysis of prostanoid enzymes and receptors in the human endometrium across the menstrual cycle. Mol Hum Reprod. 17:182–192. doi: 10.1093/molehr/gaq094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang D, Wang H, Brown J, Daikoku T, Ning W, et al. CXCL1 induced by prostaglandin E2 promotes angiogenesis in colorectal cancer. J Exp Med. 2006;203:941–951. doi: 10.1084/jem.20052124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chiarugi V, Magnelli L, Gallo O. Cox-2, iNOS and p53 as play-makers of tumor angiogenesis (review). Int J Mol Med. 1998;2:715–719. doi: 10.3892/ijmm.2.6.715. [DOI] [PubMed] [Google Scholar]
- 26.Gately S, Li WW. Multiple roles of COX-2 in tumor angiogenesis: a target for antiangiogenic therapy. Semin Oncol. 2004;31:2–11. doi: 10.1053/j.seminoncol.2004.03.040. [DOI] [PubMed] [Google Scholar]
- 27.Iniguez MA, Rodriguez A, Volpert OV, Fresno M, Redondo JM. Cyclooxygenase-2: a therapeutic target in angiogenesis. Trends Mol Med. 2003;9:73–78. doi: 10.1016/s1471-4914(02)00011-4. [DOI] [PubMed] [Google Scholar]
- 28.Jain RK, Booth MF. What brings pericytes to tumor vessels? J Clin Invest. 2003;112:1134–1136. doi: 10.1172/JCI20087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pijnenborg JM, Wijnakker M, Hagelstein J, Delvoux B, Groothuis PG. Hypoxia contributes to development of recurrent endometrial carcinoma. Int J Gynecol Cancer. 2007;17:897–904. doi: 10.1111/j.1525-1438.2007.00893.x. [DOI] [PubMed] [Google Scholar]
- 30.Chell SD, Witherden IR, Dobson RR, Moorghen M, Herman AA, et al. Increased EP4 receptor expression in colorectal cancer progression promotes cell growth and anchorage independence. Cancer Res. 2006;66:3106–3113. doi: 10.1158/0008-5472.CAN-05-3702. [DOI] [PubMed] [Google Scholar]
- 31.Zheng Y, Ritzenthaler JD, Sun X, Roman J, Han S. Prostaglandin E2 stimulates human lung carcinoma cell growth through induction of integrin-linked kinase: the involvement of EP4 and Sp1. Cancer Res. 2009;69:896–904. doi: 10.1158/0008-5472.CAN-08-2677. [DOI] [PubMed] [Google Scholar]
- 32.Ma X, Kundu N, Rifat S, Walser T, Fulton AM. Prostaglandin E receptor EP4 antagonism inhibits breast cancer metastasis. Cancer Res. 2006;66:2923–2927. doi: 10.1158/0008-5472.CAN-05-4348. [DOI] [PubMed] [Google Scholar]
- 33.Robertson FM, Simeone AM, Mazumdar A, Shah AH, McMurray JS, et al. Molecular and pharmacological blockade of the EP4 receptor selectively inhibits both proliferation and invasion of human inflammatory breast cancer cells. J Exp Ther Oncol. 2008;7:299–312. [PubMed] [Google Scholar]
- 34.Sales KJ, Katz AA, Howard B, Soeters RP, Millar RP, et al. Cyclooxygenase-1 is up-regulated in cervical carcinomas: autocrine/paracrine regulation of cyclooxygenase-2, prostaglandin e receptors, and angiogenic factors by cyclooxygenase-1. Cancer Res. 2002;62:424–432. [PMC free article] [PubMed] [Google Scholar]
- 35.Narumiya S, Sugimoto Y, Ushikubi F. Prostanoid receptors: structures, properties, and functions. Physiol Rev. 1999;79:1193–1226. doi: 10.1152/physrev.1999.79.4.1193. [DOI] [PubMed] [Google Scholar]
- 36.Cherukuri DP, Chen XB, Goulet AC, Young RN, Han Y, et al. The EP4 receptor antagonist, L-161,982, blocks prostaglandin E2-induced signal transduction and cell proliferation in HCA-7 colon cancer cells. Exp Cell Res. 2007;313:2969–2979. doi: 10.1016/j.yexcr.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sales KJ, Grant V, Jabbour HN. Prostaglandin E2 and F2alpha activate the FP receptor and up-regulate cyclooxygenase-2 expression via the cyclic AMP response element. Mol Cell Endocrinol. 2008;285:51–61. doi: 10.1016/j.mce.2008.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abera AB, Sales KJ, Catalano RD, Katz AA, Jabbour HN. EP2 receptor mediated cAMP release is augmented by PGF 2 alpha activation of the FP receptor via the calcium-calmodulin pathway. Cell Signal. 2010;22:71–79. doi: 10.1016/j.cellsig.2009.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsujii M, Kawano S, Tsuji S, Sawaoka H, Hori M, et al. Cyclooxygenase regulates angiogenesis induced by colon cancer cells. Cell. 1998;93:705–716. doi: 10.1016/s0092-8674(00)81433-6. [DOI] [PubMed] [Google Scholar]
- 40.Horree N, van Diest PJ, Sie-Go DM, Heintz AP. The invasive front in endometrial carcinoma: higher proliferation and associated derailment of cell cycle regulators. Hum Pathol. 2007;38:1232–1238. doi: 10.1016/j.humpath.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 41.Horree N, van Diest PJ, van der Groep P, Sie-Go DM, Heintz AP. Progressive derailment of cell cycle regulators in endometrial carcinogenesis. J Clin Pathol. 2008;61:36–42. doi: 10.1136/jcp.2006.043794. [DOI] [PubMed] [Google Scholar]
- 42.Weinberg E, Zeldich E, Weinreb MM, Moses O, Nemcovsky C, et al. Prostaglandin E2 inhibits the proliferation of human gingival fibroblasts via the EP2 receptor and Epac. J Cell Biochem. 2009;108:207–215. doi: 10.1002/jcb.22242. [DOI] [PubMed] [Google Scholar]
- 43.Marin-Hernandez A, Gallardo-Perez JC, Ralph SJ, Rodriguez-Enriquez S, Moreno-Sanchez R. HIF-1alpha modulates energy metabolism in cancer cells by inducing over-expression of specific glycolytic isoforms. Mini Rev Med Chem. 2009;9:1084–1101. doi: 10.2174/138955709788922610. [DOI] [PubMed] [Google Scholar]
- 44.Fukuda R, Kelly B, Semenza GL. Vascular Endothelial Growth Factor Gene Expression in Colon Cancer Cells Exposed to Prostaglandin E2 Is Mediated by Hypoxia-inducible Factor 1. Cancer Res. 2003;63:2330–2334. [PubMed] [Google Scholar]
- 45.Imtiyaz HZ, Simon MC. Hypoxia-inducible factors as essential regulators of inflammation. Curr Top Microbiol Immunol. 2010;810:105–120. doi: 10.1007/82_2010_74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Expression profile of the PTGES-PTGER system in endometrial adenocarcinoma and normal endometrium. mRNA expression of PGE2 synthase isoforms (PTGES, -2, -3) and E-series prostaglandin receptors (PTGER1–4) in normal endometrium (n = 40; comprising of proliferative n = 10; early secretory n = 10; mid-secretory n = 10 and late secretory n = 10 phase endometrium) and endometrial cancer (n = 29; comprising poorly differentiated n = 10, moderately differentiated n = 10 and well differentiated endometrial adenocarcinoma n = 9). *, **, *** represent significance at P<0.05, P<0.01 and P<0.001.
(TIF)