Abstract
Objective
Transmission patterns of drug-resistant Mycobacterium tuberculosis (MTB) may be influenced by differences in socio-demographics, local tuberculosis (TB) endemicity and efficaciousness of TB control programs. This study aimed to investigate the impact of DOTS on the transmission of drug-resistant TB in eastern rural China.
Methods
We conducted a cross-sectional study of all patients diagnosed with drug-resistant TB over a one-year period in two rural Chinese counties with varying lengths of DOTS implementation. Counties included Deqing, with over 11 years' DOTS implementation and Guanyun, where DOTS was introduced 1 year prior to start of this study. We combined demographic, clinical and epidemiologic information with IS6110-based restricted fragment length polymorphism (RFLP) and Spoligotyping analysis of MTB isolates. In addition, we conducted DNA sequencing of resistance determining regions to first-line anti-tuberculosis agents.
Results
Of the 223 drug-resistant isolates, 73(32.7%) isolates were identified with clustered IS6110RFLP patterns. The clustering proportion among total drug-resistant TB was higher in Guanyun than Deqing (26/101.vs.47/122; p,0.04), but not significantly different among the 53 multidrug-resistant isolates (10/18.vs.24/35; p,0.35). Patients with cavitary had increased risk of clustering in both counties. In Guanyun, patients with positive smear test or previous treatment history had a higher clustering proportion. Beijing genotype and isolates resistant to isoniazid and/or rifampicin were more likely to be clustered. Of the 73 patients with clustered drug-resistant isolates, 71.2% lived in the same or neighboring villages. Epidemiological link (household and social contact) was confirmed in 12.3% of the clustered isolates.
Conclusion
Transmission of drug-resistant TB in eastern rural China is characterized by small clusters and limited geographic spread. Our observations highlight the need for supplementing DOTS with additional strategies, including active case finding at the village level, effective treatment for patients with cavities and drug susceptibility testing for patients at increased risk for drug-resistance.
Introduction
Drug-resistant Mycobacterium tuberculosis (MTB) once confined to hospitals and institutional settings,is now widespread in some communities and stands to undermine global tuberculosis control efforts. Of particular concern is the occurrence of multidrug-resistant tuberculosis (MDR-TB), defined as resistance to at least isoniazid and rifampicin. MDR-TB patients respond poorly to conventional first-line therapy, are costly to manage, and typically remain infectious for prolonged periods of time due to inefficient bacillary clearance [1], [2], [3]. Clearly, a better understanding of drug-resistant TB epidemiology is paramount to inform evidence-based control strategies for MDR-TB.
Drug-resistance is associated with a number of factors including poor adherence to anti-TB treatment[4]. MDR-TB comes about as a result of the stepwise accumulation mutations in drug-resistance conferring genes. Previously, drug-resistant MTB strains were thought to be less infectious and less likely to cause disease when compared to their drug-susceptible counterparts [5]. However, recent studies have shown that they are able to transmit and cause disease as often as drug-susceptible organisms [6], [7], [8]. In addition to de novo acquisition, primary transmission of already resistant organisms may be fueling the ongoing MDR-TB epidemic [9], [10].
Directly observed treatment, short course (DOTS) is a cost-effective strategy to control TB, where standardized chemotherapy observed by trained health providers is the key element for treatment compliance and in preventing drug-resistance. However, MDR-TB cases are increasingly reported in DOTS-covered areas [10], . In China, DOTS-based TB control programs have been implemented comprehensively since its introduction over 15 years ago and by 2007 DOTS coverage in China had reached almost 100% [13]. Despite DOTS penetration, there remains significant increase in prevalence of MDR-TB particularly in rural areas. China is considered one of the “hotspot” regions for drug-resistant TB by WHO [14] and accounts for a quarter of the global burden.
A recent study conducted in eastern rural China reported a significantly higher proportion of MDR-TB in regions with long-term DOTS coverage when compared to short-term DOTS covered areas [15]. In addition, drug-resistant MTB circulating in these communities in rural China was strongly associated with specific resistance conferring mutations [16]. Furthermore, a major subgroup within the Beijing family[17] and strains with katG315T [18] possess an increased predisposition to develop MDR and transmission in rural China. Based on these observations, we sought to systematically determine the extent of transmission of drug-resistant MTB in these two counties, with varied lengths of DOTS implementation. Furthermore, we examined transmission of drug-resistant TB at the phenotypic and genotypic level, explored risk factors for the recent transmission, as well as assessed relative geographic distances between patients infected with “clustered” MTB IS6110 RFLP genotypes in two counties, in an attempt to provide the knowledge base to understand the epidemic of drug-resistant TB as well as to inform TB control activities in rural China.
Materials and Methods
The study was approved by the Institutional Review Board of Fudan School of Public Health. Written informed consent was obtained from all the participants.
Study sites
Jiangsu Province and Zhejiang Province are located in eastern China and border each other. Two counties Deqing and Guanyun were selected separately from these two provinces as the study sites. The selection of study sites was based on the comparable socioeconomics, demographics, general health systems, capacity and willingness of local partners. While Deqing implemented the DOTS-based National TB Control Program guidelines 11 years ago, Guanyun adopted the DOTS strategy less than 1 year prior to start of this study. In both counties, the county TB dispensary is the only designated health facility for TB diagnosis, treatment and case management. Due to limited resources, bacterial culturing and drug susceptibility testing (DST) were not routinely performed. TB treatment was based on the standardized therapy using 1st-line anti-TB agents.
Bacterial isolates and clinical data
In this population-based epidemiological study, a total of 399 diagnosed pulmonary TB patients, 182 in Deqing and 217 in Guanyun, registered at local TB dispensaries during 12 months consecutive in 2004–2005 were enrolled. All patient specimens at TB dispensaries were submitted to the microbiology laboratory in School of Public Health, Fudan University for culturing and identification. After identification by implanting colonies separately in PNB and TCH containing culture media, 387 isolates was defined as MTB by presenting TCH positive and PNB negative. MTB isolates were further examined for their susceptibilities to isoniazid (INH), streptomycin (STR), ethambutol (EMB) and rifampicin (RIF) by proportion method [19]. Results from culturing and drug susceptibility testing as well as demographic and clinic information were available for 164 (90.1%) isolates in Deqing and 187 (86.2%) isolates in Guanyun, respectively. These MTB isolates were included in the present study.
Genotyping
Genotyping was performed on each isolate using both IS6110-based Restricted Fragment Length Polymorphism (RFLP) and Spoligotyping. IS6110 RFLP was performed according to methods described by van Embden and coworkers [20]. Briefly, chromosomal DNA was digested with restriction endonuclease PvuII and hybridized with a probe prepared from a 245-bp PCR product of IS6110. IS6110 Southern blot hybridization pattern was visualized using a commercial kit (Maarssen, The Netherlands). The DNA fingerprint patterns of the isolates were compared both by Gelcompar software (version 3.lb, Applied Maths, Kortrijk, Belgium) and by visual examination. A molecular “cluster” was defined as two or more persons whose organisms had identical IS6110 RFLP patterns, while the organisms with orphan IS6110 RFLP pattern was defined as “unique” strain. Typically, clustered strains indicate recent transmission while unique strains indicate reactive disease from a remote infection.
Spoligotyping was performed to differentiate the Beijing family from other genotypes. The spacer between the direct repeats in the target region was amplified using two 18 bp nucleotide primers as described elsewhere [21]. The PCR products were hybridized to commercial membrane (Isogen Bioscience BV, Maarssen, The Netherlands). Hybridized DNA was detected using an enhanced chemiluminescene kit from Isogen Bioscience BV (Maarssen, The Netherlands), which resulted in patterns for each strain reminiscent of a ‘barcode’. Strain family was determined by comparing Spoligotyping patterns with the SpoligDB4 database [21]. Beijing family MTB was defined as those hybridizing the last nine spacer oligonucleotides (spacers 35 to 43) of the Spoligotyping pattern.
DNA sequencing
We targeted the 5′ and 3′ flanking resistance determining regions of rpoB(Genebank assession No.L27989), katG(Genebank assession No.X68081), rpsL(Genebank assession No.L08011) and embB(Genebank assession No.U68480), using oligonucleotide primers previous described[16]. Targeted PCR products were sequenced using an Applied Biosystem 3730/3730×l DNA analyzer. DNA sequencing data was aligned manually using Sequencer 4.7 software (Gene Codes Corporation). All the nucleotide data has been submitted and deposited in GenBank.
Statistical analysis
Descriptive analyses were performed using SPSS 11.0 (SPSS, Chicago, IL, USA). ANOVA and  tests were used to examine difference in baseline information between the two rural counties. Univariate and multivariate analysis were conducted using binary logistic regression model. Odds ratio (OR) and 95% confidence interval (CI) were reported after adjusting for age, sex and counties. Statistical significance was defined as p value of 0.05 or less.
tests were used to examine difference in baseline information between the two rural counties. Univariate and multivariate analysis were conducted using binary logistic regression model. Odds ratio (OR) and 95% confidence interval (CI) were reported after adjusting for age, sex and counties. Statistical significance was defined as p value of 0.05 or less.
Results
Detailed characteristics of studied patients and the drug-resistant pattern and the genetic mutation of MTB isolates have been reported previously [15], [16]. Summary characteristics of subjects were shown in Table 1. No statistically significant differences were observed in the socio-demographic and clinical features of patients from the two counties.
Table 1. Demographic and clinic characteristics of patients and drug-resistant patterns at diagnosis in Deqing and Guanyun.
| Variables | Deqing (n = 164) | Guanyun (n = 187) | χ2 | p | ||
| No. | % | No. | % | |||
| Male (sex) | 109 | 66.5 | 128 | 68.4 | 0.157 | 0.69 |
| Age (mean±SD) | 48.44±18.96 | 48.20±19.76 | 0.045a | 0.83 | ||
| Cavity | 22 | 13.4 | 33 | 17.6 | 1.184 | 0.28 |
| Smear positive | 110 | 67.1 | 129 | 69.0 | 0.147 | 0.70 |
| BMI value (mean±SD) | 18.33±2.62 | 18.90±3.00 | 3.579a | 0.06 | ||
| Previously treated | 42 | 25.6 | 51 | 27.3 | 0.124 | 0.73 |
| Drug-resistant pattern at diagnosis | ||||||
| Pan-drug sensitive | 63 | 38.4 | 65 | 34.8 | 4.089 | 0.13 |
| MDR-TB | 18 | 11.0 | 35 | 18.7 | ||
| Other drug-resistance | 83 | 50.6 | 87 | 46.5 | ||
aF value for ANOVA test.
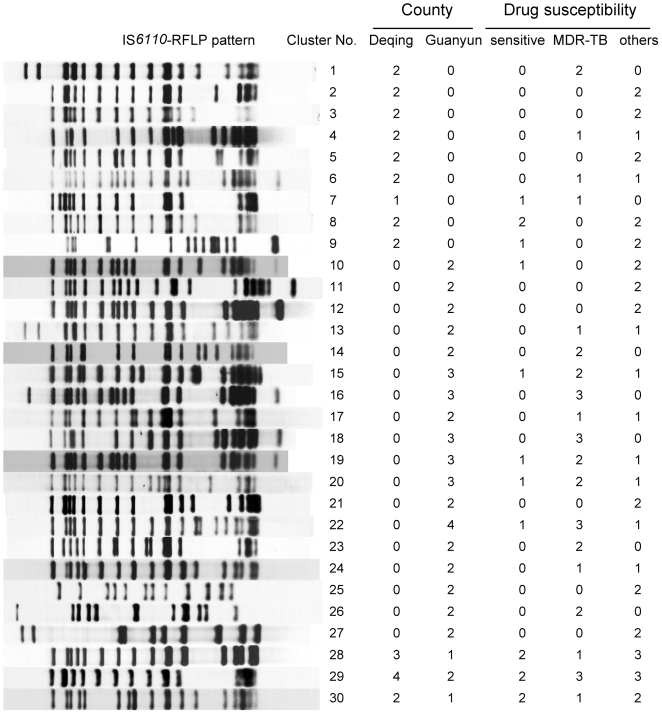
Of the 223 drug-resistant MTB isolates, a total of 180 IS6110 RFLP genotype patterns were observed, with 30 clusters composed of 73 drug-resistant isolates (32.7%). Of these clusters, 19 clusters were composed solely by 40 drug-resistant isolates, and the other 11 clusters were shared with 33 drug-resistant and 15 pan-drug sensitive isolates. The remaining 150 drug-resistant isolates (67.3%) gave the unique fingerprint patterns. A total of 12 and 21 clusters were observed in Deqing and Guanyun, with three IS6110 RFLP patterns shared between the two counties. The clustering proportion of drug-resistant TB was significantly higher in Guanyun than that in Deqing (26/101.vs.47/122; p, 0.04), but there was no significant difference for MDR-TB (10/18.vs.24/35; p, 0.35) (Figure 1). Results from Spoligotyping showed that 163 (73.1%) isolates belonged to Beijing family. Spoligotype-based lineages for 46 of the remaining 60 isolates were as follows: Family 33 (17/223 or 7.6%), T lineage (15/223 or 6.7%), Haarlem (5/223 or 2.2%), LAM (8/223 or 3.6%) and EAI (1/223 or 0.4%). Twelve isolates shared identical Spoligotyping patterns, of which 2 were in family 33 shared Spoligotyping International Type (SIT) 54 (Octal value 7777 7777 7763 771), 2 and 4 isolates in T1 shared SIT 52(Octal 7777 7777 7760 731) and SIT53 (Octal value 7777 7777 7760 771), 2 and 2 in LAM family shared SIT 1755 (Octal 6777 7760 7560 771) and new SIT(Octal value 7777 7760 3560 731) (Table S1).
Figure 1. The clustering patterns of IS6110 RFLP and their distribution in counties and 1st-line drug susceptibilities groups.
The isolates in the counties represented the clustered drug-resistant MTB with the identical IS6110 RFLP patterns.
Results from the multivariate analysis are shown in Table 2. Stratified by county, drug-resistant isolates within Beijing family had a significantly higher clustering proportion than those from the other strain families (Deqing: OR, 6.18; 95%CI, 1.332–28.64; Guanyun: OR, 3.75; 95%CI, 1.396–10.06). Drug-resistant isolates from the patients with cavitary disease were more likely to be clustered than those without cavitation (Deqing: OR, 4.50; 95%CI, 1.421–14.26; Guanyun: OR, 2.85; 95%CI:1.195 –6.782). In Guanyun, previous treatment history (OR, 5.66; 95%CI, 2.332–13.73) and positive sputum smear status (OR, 2.98; 95%CI, 1.191–7.441) were independently associated with clustering among drug-resistant MTB isolates (Table 2).
Table 2. Univariate and multivariate analysis on the factors influencing the clustering proportion of drug-resistant TB (n = 223).
| Variable | Deqing county | Guanyun county | ||||||||||
| Total | Clustered | cOR | aORa | p a | 95%CIa | Total | Clustered | cOR | aORa | p a | 95%CIa | |
| BMI | ||||||||||||
| >18.5 | 51 | 10 (19.6) | 1.00 | 1.00 | 58 | 19(32.8) | 1.00 | 1.00 | ||||
| ≤18.5 | 50 | 16 (32.0) | 1.93 | 1.92 | 0.17 | 0.760–4.820 | 64 | 28(43.8) | 1.60 | 1.77 | 0.15 | 0.818–3.840 |
| TB contact | ||||||||||||
| No | 88 | 22 (25.0) | 1.00 | 1.00 | 92 | 34(37.0) | 1.00 | 1.00 | ||||
| Yes | 13 | 4 (30.8) | 1.33 | 1.38 | 0.63 | 0.382–4.963 | 30 | 13(43.3) | 1.30 | 1.37 | 0.48 | 0.579–3.235 |
| Sputum smear test | ||||||||||||
| negative | 28 | 6 (21.4) | 1.00 | 1.00 | 38 | 8 (21.1) | 1.00 | 1.00 | 0.02 | |||
| positive | 73 | 20(27.4) | 1.38 | 1.38 | 0.54 | 0.488–3.910 | 84 | 39(46.4) | 3.25 | 2.98 | 0.01b | 1.191–7.441 |
| Cavity | ||||||||||||
| No | 86 | 18(20.9) | 1.00 | 1.00 | 92 | 30(32.6) | 1.00 | 1.00 | ||||
| Yes | 15 | 8 (53.3) | 4.32 | 4.50 | 0.01b | 1.421–14.26 | 30 | 17(56.7) | 2.70 | 2.85 | 0.02 b | 1.195–6.782 |
| Treatment history | ||||||||||||
| New | 68 | 17(25.0) | 1.00 | 1.00 | 79 | 21(26.6) | 1.00 | 1.00 | ||||
| Prior treated | 33 | 9 (27.3) | 1.13 | 1.14 | 0.78 | 0.443–2.945 | 43 | 26(60.5) | 4.22 | 5.66 | 0.01 b | 2.332–13.73 |
| Strain family | ||||||||||||
| Non-Beijing | 27 | 2 (7.4) | 1.00 | 1.00 | 33 | 6(18.2) | 1.00 | 1.00 | ||||
| Beijing genotype | 74 | 24(32.4) | 6.00 | 6.18 | 0.02b | 1.332–28.64 | 89 | 41(46.1) | 3.84 | 3.75 | 0.01b | 1.396–10.06 |
OR and 95% CI was adjusted for age and sex in the binary logistics regression model.
p<0.05.
Clustering proportion among drug-resistant MTB isolates was compared to the 128 drug-susceptible MTB isolates collected simultaneously. Isolates resistant to INH (48.1%.vs. 30.5%; p, 0.008; OR, 2.01; 95%CI, 1.204–3.369), RIF (53.8%.vs.30.5%; p, 0.003; 2.62; 95%CI, 1.382–4.980) and MDR-TB (64.2%.vs. 30.5%; p, 0.0001; OR, 3.87; 95%CI, 1.924–7.764) were more likely to be clustered compared to drug-susceptible isolates (Table 3). The association between drug-resistance conferring genotype and clustering was investigated by comparing the clustering proportion between drug-resistant genotype and wide type isolates. Among INH resistant isolates, katG 315Thr alleles (73.0%.vs18.0%; p, 0.0001; OR, 12.7; 95%CI: 6.357–14.80) were strongly associated with clustering. No other alleles conferring resistance to RIF, STR and EMB were associated with clustering.
Table 3. Clustering proportion between the MTB isolates with different drug-resistant pattern and genetic mutation (n = 223).
| No.of isolates | crude | Adjusted ORb | p b | 95%CIb | |||
| Total | Clustered(%) | ORa | |||||
| Isolates resistant to: | |||||||
| Sensitive | 128 | 39(30.5) | 1.00 | 1.00 | |||
| INH | 131 | 63(48.1) | 2.05 | 2.01 | 0.008c | 1.204–3.369 | |
| RIF | 65 | 35(53.8) | 2.66 | 2.62 | 0.003c | 1.382–4.980 | |
| STR | 115 | 26(22.6) | 0.67 | 0.68 | 0.19 | 0.376–1.215 | |
| EMB | 42 | 12(28.6) | 0.91 | 0.90 | 0.79 | 0.405–1.988 | |
| MDR-TB | 53 | 34(64.2) | 4.08 | 3.87 | 0.0001c | 1.924–7.764 | |
| Other combinations | 170 | 39(22.9) | 0.82 | 0.82 | 0.15 | 0.634–1.070 | |
| Drug-resistant isolates with mutation in: | |||||||
| katG | |||||||
| wt | 50 | 9 (18.0) | 1.00 | 1.00 | |||
| others | 7 | 0 (0) | - | - | - | - | |
| 315Thr | 74 | 54(73.0) | 12.3 | 12.7 | 0.0001c | 6.357–14.80 | |
| rpoB | |||||||
| wt | 5 | 1(20.0) | 1.00 | 1.00 | |||
| others | 23 | 10 (43.5) | 4.22 | 4.88 | 0.12 | 0.597–19.298 | |
| 531Leu | 37 | 24 (64.9) | 8.71 | 8.50 | 0.08 | 0.771–93.65 | |
| rpsL | |||||||
| wt | 37 | 9 (24.3) | 1.00 | 1.00 | |||
| others | 18 | 2 (11.1) | 0.33 | 0.55 | 0.49 | 0.099–3.035 | |
| 43Arg | 60 | 15(25.0) | 1.04 | 1.41 | 0.51 | 0.511–3.865 | |
| embB | |||||||
| wt | 21 | 5(23.8) | 1.00 | 1.00 | |||
| 306lle | 8 | 2(25.0) | 1.27 | 1.19 | 0.87 | 0.164–8.584 | |
| 306Val | 13 | 5(38.5) | 1.80 | 1.59 | 0.14 | 0.673–9.100 | |
Note: INH,isoniazid; RIF,rifampicin; STR, streptomycin; EMB, ethambutol.
cOR: crude odds ratio were calculated by comparing the clustering proportion between drug- resistant MTB isolate and drug-susceptible isolate in binary logistic regression model.
aOR: adjusted odds ratio and 95%CI were calculated by comparing the clustering proportion between drug-resistant TB isolate and drug-susceptible isolate, adjusted by age, sex, and counties of the subjects in a binary logistic regression model.
p<0.05.
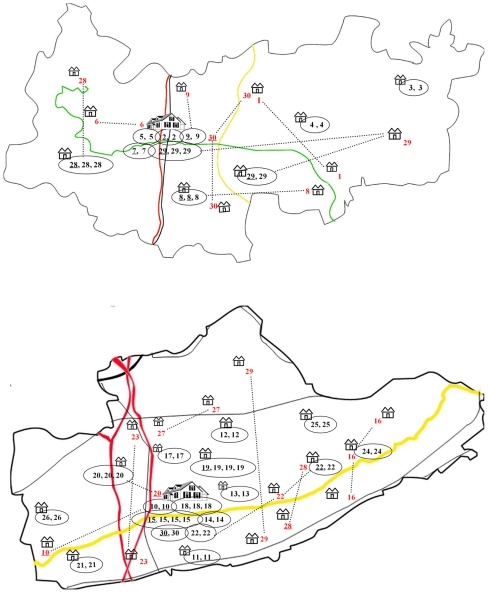
Epidemiological links within drug-resistant clusters and geographic distribution based on patients' residence are depicted in Figure 2. Of the 30 clusters (i.e. identical IS6110 RFLP patterns), 9 in Deqing and 16 in Guanyun were geographically restricted, originating from the same or neighboring village in the same town. The town central of Deqing and Guanyun contained 5 and 6 clusters respectively, involving 8 and 13 drug-resistant patient isolates. The isolates from the 3 clusters in Deqing and 5 clusters in Guanyun were obtained from different localities. From potential contact perspective, 4 of 26 (15.4%) clustered isolates from Deqing and 5 of 47 (10.6%) clustered isolates from Guanyun were obtained from family members (household contact), friends or working colleagues (social contact). No epidemiological links or geographic correlation was established for 9 clustered drug-resistant isolates (34.6%) in Deqing and 11 clustered drug-resistant isolates (23.4%) in Guanyun.
Figure 2. The geographic distribution of the patients with the clustered MTB isolates in Deqing(upper) and Guanyun(lower).
Note: cottage represented the township; vile represented the central area of the counties; No. marked the IS6110 RFLP clusters; the underlined No. represented the drug-susceptible MTB isolates; Eclipse marked the clustered isolates distributed in the same township; the dotted line connected the clustered isolate without geographic correlation.
Discussion
Transmission patterns of drug-resistant MTB has been well documented in low TB incidence countries, however there is paucity of reports from high TB burden countries like China; this information could be very important in decision-making for TB control. To that end, the present study aimed to describe the transmission of drug-resistant TB in two comparable rural Chinese communities with different duration of DOTS implementation, and to identify risk factors for developing appropriate strategies for prevention and control of drug-resistant TB in eastern rural China.
IS6110 DNA fingerprinting indicated that the degree of MTB genotypic heterogeneity did not vary significantly between Deqing and Guanyun, with 87 and 86 IS6110 RFLP patterns respectively. This may be expected given the overwhelming dominance of the Beijing family strain in most regions in China [17], [22]. In addition to its overall prevalence, Beijing family members are increasingly found associated with MDR-TB [23], [24] and enhanced transmissibility in some areas [25], [26]. Similarly in the present study, the majority (73.1%) of drug-resistant TB were from members of the Beijing family. Drug-resistant TB isolates within Beijing family showed a relatively high level of clustering (40.0%), suggesting active transmission. Furthermore, three Beijing IS6110 RFLP clusters were simultaneously observed in Deqing from Zhejiang Province and Guanyun from Jiangsu Province, possibly due to its inter-provincial transmission. This tendency may suggest high transmissibility potential for some specific members of Beijing family [17]. The active transmission of such subgroups may contribute to the ongoing epidemic of drug-resistant TB in rural China and highlights the need for better control measures to prevent the primary transmission.
In Guanyun, a county with recent DOTS implementation, most clusters were among cases with previous treatment history. In addition, cavitary lesions and sputum smear positivity (indicating infectiousness) were significantly more common among the drug-resistant cases with clustered genotypes than those infected with unique genotypes. Our findings are consistent with those reported by others [27], [28]. Typically, patients with cavitary disease harbor higher bacillary burdens, thereby increasing the likelihood of selecting mutants during therapy [29], [30]. Smear positivity would similarly indicate higher bacillary burden and increased infectiousness. The high proportion of clustering pattern in previously treated cases is also troubling as it indicates that inadequate previous treatment increasing the risk of drug-resistance and primary transmission. While in Deqing where DOTS had been implemented for over 15 years, only patients with cavities had increased risk for clustering. Previous treatment history wasn't found a risk factor for clustering as it was in Guanyun County. The differences between the counties might indicate population-level effects of long-term regulated and standardized TB treatment (i.e. DOTS). However, we did not observe the significant difference in the clustering proportion among MDR-TB isolates between two counties, suggesting that without routine bacteriologic-based diagnosis and drug susceptibility testing and without regulated treatment for drug-resistant TB, DOTS itself might not be able to prevent the risk of community-level MDR-TB transmission. Therefore, MDR-TB control programs in China may be modified according to local settings and needs additional strategies such as establishing referral system for patients at high risk of drug-resistant TB, improving ability of diagnosis for drug-resistance in TB clinics and hospitals, and providing individualized treatment for drug-resistant TB patients.
Resistance to anti-TB drugs can develop as a result of treatment failure (acquired resistance), but it can also occur as a result of infection with drug-resistant strains (primary resistance). Among drug-resistant TB patients in our study, INH resistant, RIF resistant and MDR-TB had a significantly higher clustering proportion compared to the drug-susceptible MTB isolates, highlighting the significance of the primary resistance. Comparably, the reactivation from the remote infection might be the main reason for the STR and EMB resistance. A high clustering proportion of katG315Thr allele was observed in this study. This allele was associated with MDR-TB as reported elsewhere [18], [31], [32]. Therefore, this allele may be the major genotype responsible for the recent transmission of MDR-TB and INH resistant strain in the studied areas. The different epidemic mechanism for drug-resistant TB implies that tailored strategies are needed for in control of drug-resistant TB. Considering the transmissibility of INH and RIF resistant TB, susceptibility testing of INH and RIF should be provided, and fast diagnosis of drug-resistance is paramount.
The geographic distribution of isolates from clusters containing drug-resistant TB is consistent with the distribution of rural population. Most clones of drug-resistant strains were found to infect small groups of patients. This suggests that active transmission of drug-resistant MTB strain may be limited in Chinese rural communities. Furthermore, a relative high proportion of patients in the clusters lived in the same or neighboring villages. TB patients are usually weak and unable to work, and they have to take treatment for 6–8 months at home. Thus, the scope of their activity is limited, especially in rural China, which might limit the contacts within the same village and makes transmission circle restricted at the village and neighborhood level.
Although clusters came from a wide geographic area, a high level of clustered MTB isolate was observed in the central districts. The central district in rural China commonly has the highest population density and also serves as centers for cultural and social activities. Furthermore, the central districts contain county-level hospitals and TB dispensaries for the diagnosis and treatment of TB. These conditions in central areas may facilitate transmission of MTB. In addition, the present study also noted clustered isolates scattered from different localities, where no clear epidemiological link was identified. Lack of epidemiological links, in the context of clustering, may indicate the existence of wide spread endemic MTB strains. Of note, our one-year study period as well as the passive case detection strategies may have missed intermediate cases in the transmission chain. Our primary genotyping method, IS6110 RFLP has long served as a gold standard technique with highest discriminatory power for high-copy number isolates including Beijing genotype isolates. However, some recent studies have pointed to clustering misclassification using IS6110 RFLP alone [33], [34], [35]. Therefore to better define the genotypes of MTB in certain settings, the future studies may benefit from combining IS6110 RFLP with alternative genotyping methods such as 24-loci variable number tandem repeat analysis.
Adoption of DOTS to prevent the generation of drug-resistant strains and careful introduction of second-line drugs to treat patients with MDR-TB are the top priorities for proper containment of MDR-TB. As reported above in rural China, the transmission pattern of drug-resistant TB was sporadic distribution and in small groups. The spread of drug-resistance may be restricted due to limited social activity of rural populations. Based on our data, anti-TB intervention should focus mainly on individuals proximal to the infectious TB case, rapid identification of drug-resistance, and include active case finding strategies.
Supporting Information
Spoligotyping pattern and drug-resistant pattern and genetic mutation of drug-resistant MTB isolates with non-Beijing family. Note: SIT, Spoligotyping International Type; wt, wide type. aSpotclust program-assigned clade. bProbaiblity that the Spoligotyping pattern belongs to the clades. cSequence of drugs was Isoniazid, Rifampin, Streptomycin, Ethambutol; R, resistant; S, susceptible.
(DOC)
Acknowledgments
We wish to thank health authorities and investigators in Deqing county and Guanyun county for their cooperation.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by two grants (PI, Biao Xu, No. 30771843; PI, Yi Hu, No. 30901223) from National Natural Science Foundation of China, Shanghai Leading Academic Discipline Project (No. B118) and National Key Project for Infectious Disease (No.2008ZX10003-010). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Cohn DL, Bustreo F, Raviglione MC. Drug-resistant tuberculosis: review of the worldwide situation and the WHO/IUATLD Global Surveillance Project. International Union Against Tuberculosis and Lung Disease. Clin Infect Dis. 1997;24(Suppl 1):S121–130. doi: 10.1093/clinids/24.supplement_1.s121. [DOI] [PubMed] [Google Scholar]
- 2.Resch SC, Salomon JA, Murray M, Weinstein MC. Cost-effectiveness of treating multidrug-resistant tuberculosis. PLoS Med. 2006;3:e241. doi: 10.1371/journal.pmed.0030241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohammadi A, Nassor ZS, Behlim T, Mohammadi E, Govindarajan R, et al. Epidemiological and cost analysis of multidrug-resistant tuberculosis in Oman. East Mediterr Health J. 2008;14:1240–1245. [PubMed] [Google Scholar]
- 4.Pritchard AJ, Hayward AC, Monk PN, Neal KR. Risk factors for drug resistant tuberculosis in Leicestershire—poor adherence to treatment remains an important cause of resistance. Epidemiol Infect. 2003;130:481–483. doi: 10.1017/s0950268803008367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohn ML, Davis CL. Infectivity and pathogenicity of drug-resistant strains of tubercle bacilli studied by aerogenic infection of guinea pigs. Am Rev Respir Dis. 1970;102:97–100. doi: 10.1164/arrd.1970.102.1.97. [DOI] [PubMed] [Google Scholar]
- 6.Agerton T, Valway S, Gore B, Pozsik C, Plikaytis B, et al. Transmission of a highly drug-resistant strain (strain W1) of Mycobacterium tuberculosis. Community outbreak and nosocomial transmission via a contaminated bronchoscope. JAMA. 1997;278:1073–1077. [PubMed] [Google Scholar]
- 7.Gandhi NR, Moll A, Sturm AW, Pawinski R, Govender T, et al. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006;368:1575–1580. doi: 10.1016/S0140-6736(06)69573-1. [DOI] [PubMed] [Google Scholar]
- 8.Shenoi SV, Escombe AR, Friedland G. Transmission of drug-susceptible and drug-resistant tuberculosis and the critical importance of airborne infection control in the era of HIV infection and highly active antiretroviral therapy rollouts. Clin Infect Dis. 2010;50(Suppl 3):S231–237. doi: 10.1086/651496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basu S, Andrews JR, Poolman EM, Gandhi NR, Shah NS, et al. Prevention of nosocomial transmission of extensively drug-resistant tuberculosis in rural South African district hospitals: an epidemiological modelling study. Lancet. 2007;370:1500–1507. doi: 10.1016/S0140-6736(07)61636-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun YJ, Lee AS, Wong SY, Heersma H, Kremer K, et al. Genotype and phenotype relationships and transmission analysis of drug-resistant tuberculosis in Singapore. Int J Tuberc Lung Dis. 2007;11:436–442. [PubMed] [Google Scholar]
- 11.Quitugua TN, Seaworth BJ, Weis SE, Taylor JP, Gillette JS, et al. Transmission of drug-resistant tuberculosis in Texas and Mexico. J Clin Microbiol. 2002;40:2716–2724. doi: 10.1128/JCM.40.8.2716-2724.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X, Zhang Y, Shen X, Shen G, Gui X, et al. Transmission of drug-resistant tuberculosis among treated patients in Shanghai, China. J Infect Dis. 2007;195:864–869. doi: 10.1086/511985. [DOI] [PubMed] [Google Scholar]
- 13.Wang L, Liu J, Chin DP. Progress in tuberculosis control and the evolving public-health system in China. Lancet. 2007;369:691–696. doi: 10.1016/S0140-6736(07)60316-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright A, Zignol M, Van Deun A, Falzon D, Gerdes SR, et al. Epidemiology of antituberculosis drug resistance 2002-07: an updated analysis of the Global Project on Anti-Tuberculosis Drug Resistance Surveillance. Lancet. 2009;373:1861–1873. doi: 10.1016/S0140-6736(09)60331-7. [DOI] [PubMed] [Google Scholar]
- 15.Hu Y, Mathema B, Wang W, Hoffner S, Kreiswirth B, et al. Prevalence of multidrug-resistant pulmonary tuberculosis in counties with different duration of DOTS implementation in rural China. Microb Drug Resist. 2008;14:227–232. doi: 10.1089/mdr.2008.0823. [DOI] [PubMed] [Google Scholar]
- 16.Hu Y, Hoffner S, Jiang W, Wang W, Xu B. Genetic characterisation of drug-resistant Mycobacterium tuberculosis in rural China: a population-based study. Int J Tuberc Lung Dis. 2010;14:210–216. [PubMed] [Google Scholar]
- 17.Hu Y, Ma X, Graviss EA, Wang W, Jiang W, et al. A major subgroup of Beijing family Mycobacterium tuberculosis is associated with multidrug resistance and increased transmissibility. Epidemiol Infect. 2011;139:130–138. doi: 10.1017/S0950268810000890. [DOI] [PubMed] [Google Scholar]
- 18.Hu Y, Hoffner S, Jiang W, Wang W, Xu B. Extensive transmission of isoniazid resistant M. tuberculosis and its association with increased multidrug-resistant TB in two rural counties of eastern China: a molecular epidemiological study. BMC Infect Dis. 2010;10:43. doi: 10.1186/1471-2334-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The WHO. The WHO/IUATLD Global Project on Anti-tuberculosis drug resistance surveillance. Anti-tuberculosis Drug Resistance in the World, 4th Global Report. 2008. Available: http://www.who.int/tb/publications/2008/drs_report4_26feb08.pdf. Accessed 2010 Jun 1.
- 20.van Embden JD, Cave MD, Crawford JT, Dale JW, Eisenach KD, et al. Strain identification of Mycobacterium tuberculosis by DNA fingerprinting: recommendations for a standardized methodology. J Clin Microbiol. 1993;31:406–409. doi: 10.1128/jcm.31.2.406-409.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vitol I, Driscoll J, Kreiswirth B, Kurepina N, Bennett KP. Identifying Mycobacterium tuberculosis complex strain families using spoligotypes. Infect Genet Evol. 2006;6:491–504. doi: 10.1016/j.meegid.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Li GL, Zhao DF, Xie T, Ju HF, Mu C, et al. Molecular characterization of drug-resistant Beijing family isolates of Mycobacterium tuberculosis from Tianjin, China. Biomed Environ Sci. 2010;23:188–193. doi: 10.1016/S0895-3988(10)60051-7. [DOI] [PubMed] [Google Scholar]
- 23.Drobniewski F, Balabanova Y, Ruddy M, Weldon L, Jeltkova K, et al. Rifampin- and multidrug-resistant tuberculosis in Russian civilians and prison inmates: dominance of the beijing strain family. Emerg Infect Dis. 2002;8:1320–1326. doi: 10.3201/eid0811.020507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park YK, Shin S, Ryu S, Cho SN, Koh WJ, et al. Comparison of drug resistance genotypes between Beijing and non-Beijing family strains of Mycobacterium tuberculosis in Korea. J Microbiol Methods. 2005;63:165–172. doi: 10.1016/j.mimet.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Phyu S, Stavrum R, Lwin T, Svendsen OS, Ti T, et al. Predominance of Mycobacterium tuberculosis EAI and Beijing lineages in Yangon, Myanmar. J Clin Microbiol. 2009;47:335–344. doi: 10.1128/JCM.01812-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ohata R, Tada A. [Beijing family and other genotypes of Mycobacterium tuberculosis isolates in Okayama district]. Kekkaku. 2004;79:47–53. [PubMed] [Google Scholar]
- 27.Aristimuno L, Armengol R, Cebollada A, Espana M, Guilarte A, et al. Molecular characterisation of Mycobacterium tuberculosis isolates in the First National Survey of Anti-tuberculosis Drug Resistance from Venezuela. BMC Microbiol. 2006;6:90. doi: 10.1186/1471-2180-6-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Telles MA, Ferrazoli L, Waldman EA, Giampaglia CM, Martins MC, et al. A population-based study of drug resistance and transmission of tuberculosis in an urban community. Int J Tuberc Lung Dis. 2005;9:970–976. [PubMed] [Google Scholar]
- 29.D'Souza D T, Mistry NF, Vira TS, Dholakia Y, Hoffner S, et al. High levels of multidrug resistant tuberculosis in new and treatment-failure patients from the Revised National Tuberculosis Control Programme in an urban metropolis (Mumbai) in Western India. BMC Public Health. 2009;9:211. doi: 10.1186/1471-2458-9-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelly PM, Lumb R, Pinto A, da Costa G, Sarmento J, et al. Analysis of Mycobacterium tuberculosis isolates from treatment failure patients living in East Timor. Int J Tuberc Lung Dis. 2005;9:81–86. [PubMed] [Google Scholar]
- 31.Varela G, Gonzalez S, Gadea P, Coitinho C, Mota I, et al. Prevalence and dissemination of the Ser315Thr substitution within the KatG enzyme in isoniazid-resistant strains of Mycobacterium tuberculosis isolated in Uruguay. J Med Microbiol. 2008;57:1518–1522. doi: 10.1099/jmm.0.2008/001917-0. [DOI] [PubMed] [Google Scholar]
- 32.Ano H, Matsumoto T, Suetake T, Nagai T, Tamura Y, et al. Relationship between the isoniazid-resistant mutation katGS315T and the prevalence of MDR-/XDR-TB in Osaka, Japan. Int J Tuberc Lung Dis. 2008;12:1300–1305. [PubMed] [Google Scholar]
- 33.Mokrousov I, Narvskaya O, Vyazovaya A, Millet J, Otten T, et al. Mycobacterium tuberculosis Beijing genotype in Russia: in search of informative variable-number tandem-repeat loci. J Clin Microbiol. 2008;46:3576–3584. doi: 10.1128/JCM.00414-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valcheva V, Mokrousov I, Narvskaya O, Rastogi N, Markova N. Utility of new 24-locus variable-number tandem-repeat typing for discriminating Mycobacterium tuberculosis clinical isolates collected in Bulgaria. J Clin Microbiol. 2008;46:3005–3011. doi: 10.1128/JCM.00437-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abadia E, Sequera M, Ortega D, Mendez MV, Escalona A, et al. Mycobacterium tuberculosis ecology in Venezuela: epidemiologic correlates of common spoligotypes and a large clonal cluster defined by MIRU-VNTR-24. BMC Infect Dis. 2009;9:122. doi: 10.1186/1471-2334-9-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Spoligotyping pattern and drug-resistant pattern and genetic mutation of drug-resistant MTB isolates with non-Beijing family. Note: SIT, Spoligotyping International Type; wt, wide type. aSpotclust program-assigned clade. bProbaiblity that the Spoligotyping pattern belongs to the clades. cSequence of drugs was Isoniazid, Rifampin, Streptomycin, Ethambutol; R, resistant; S, susceptible.
(DOC)