Abstract
Objective
To understand what contributes to good collaborative physician working relationships through identifying the factors that affect working relationships between generalist physicians and specialists.
Design
Qualitative study using in-depth interviews.
Setting
University and community hospital inpatient family practice settings in Edmonton, Alta.
Participants
Eleven physicians from various specialties who graduated between 1977 and 2001.
Methods
A grounded-theory approach, including constant comparison and creation of memorandums, helped to conceptualize the main concern and generated a framework for how the main concern was being resolved. A semistructured interview guide was developed and individual, in-depth interviews were audiotaped. Purposeful and theoretical sampling techniques were used. Three researchers participated in the analysis.
Main findings
The findings suggested that when generalist physicians perceived that work had been imposed on them by specialists without negotiation, they felt overwhelmed by the workload. Differing priorities determined whether physicians were left holding the bag or sharing the load. In a system that valued technology and specialized knowledge and skills, the specialists were better able to control resources, set boundaries, and influence learners. This precipitated a culture of protecting valuable specialty resources, increasing physician isolation, and generalists feeling that they were left holding the bag. In order to reverse this cycle, it was important for physicians to develop good working relationships based on accessibility to needed expertise and tests, with negotiated agreements on how to share resources; mutual empowerment, including negotiation of roles and responsibilities to develop flexible relationships with a clear understanding of roles; and concern for fairness by sharing the load.
Conclusion
Medical systems that value technology and focused interests might lead to someone being left holding the bag, contributing to generalists feeling overwhelmed and isolated within the system. A comprehensive system that values relationships might help to resolve issues created through perceived inequities in workload, disempowerment, and lack of understanding of roles.
Résumé
Objectif
Définir ce qui contribue à une bonne collaboration de travail entre médecins en identifiant les facteurs qui ont un effet sur les relations entre médecins généralistes et spécialistes.
Type d’étude
Étude qualitative à l’aide d’entrevues en profondeur.
Contexte
Département de médecine familiale d’un hôpital universitaire et communautaire d’Edmonton, Alberta.
Participants
Onze médecins de diverses spécialités ayant obtenu leur diplôme entre 1977 et 2001.
Méthodes
L’utilisation d’une théorie basée sur des faits, incluant une comparaison constante et la prise de notes, a aidé à se faire une idée des principales préoccupations et a généré un cadre permettant de voir comment la préoccupation principale pouvait être résolue. On a développé un guide d’entrevue semi-structurée et enregistré des entrevues en profondeur individuelles sur ruban magnétique. On a utilisé des techniques d’échantillonnage raisonné et théorique. Trois chercheurs ont participé à l’analyse.
Principales observations
Les résultats laissent entendre que quand ils avaient l’impression que les spécialistes leur imposaient du travail sans négociation, les généralistes se sentaient dépassés par la charge de travail. Différentes priorités permettaient de déterminer si les médecins étaient confinés à un rôle secondaire ou participaient aux tâches. Dans un système qui valorise la technologie et des connaissances et habiletés spécialisées, les spécialistes sont plus à même de contrôler les ressources, d’établir des limites et d’influencer les apprenants. Cela a créé une culture qui protège les ressources spécialisées valables, augmente l’isolement des médecins et amène les généralistes à penser qu’ils ne jouent qu’un rôle de second plan. Afin de renverser ce cycle, il était important que les médecins développent de bonnes relations de travail basées sur une accessibilité adéquate à l’expertise et aux examens requis, incluant des ententes quant au partage des ressources; une responsabilisation mutuelle avec négociation des rôles et responsabilités afin de développer des relations flexibles avec une compréhension claire des rôles; et une préoccupation à l’égard d’un partage équitable des tâches.
Conclusion
Les systèmes médicaux qui valorisent la technologie et les intérêts particuliers risquent d’aboutir à ce que certains estiment jouer un rôle de second plan, contribuant ainsi au fait que les généralistes se sentent débordés et isolés dans le système. Un système global qui valorise les relations pourrait aider à résoudre les problèmes qui résultent de cette perception d’iniquité dans le partage de la tâche de travail, d’une déresponsabilisation et d’une mauvaise compréhension des rôles.
Good physician relationships are required for good patient care,1–4 hence generalist and specialist interactions have implications for the health care system. Tensions between the 2 medical approaches have been described since the origins of the medical profession in the Greek schools of Cos and Cnidos. The school of Cos focused on the treatment of the patient as a whole, according to Hippocrates, while Cnidos focused on the science, that is, the organs and disease.5 Generalists and specialists might have difficulty relating and understanding each other’s roles owing to spectrum bias,6 as each sees a different aspect of the disease spectrum. Fundamental differences in how generalists and specialists approach diagnosis and clinical problem solving7 could also contribute to misunderstandings. The literature describes environments characterized by misunderstanding and lack of respect,4,8,9 as well as instances of effective, respectful working relationships between generalists and specialists.4 Tensions between these groups are occasionally observed in other arenas, such as complaints to regulatory bodies, as evidenced by the Alberta Registrar’s report of February 2006.10 Physicians’ working relationships also affect learners and contribute to the hidden curriculum. Negative attitudes of specialists toward family physicians might have played a role in declining enrolment in family medicine.11,12
There is a need for both specialist and generalist approaches in medicine,13,14 and discussion papers explore how to promote good collegial physician working relationships.3,15 Unfortunately, research focused on the development of a framework to promote collegial physician-physician relationships is lacking.3 This is not the case with the doctor-patient relationship, as the patient-centred model14,16,17 provides a framework that blends generalist and specialist approaches in the doctor-patient relationship. Understanding barriers and contributors to good collaborative physician working relationships could help improve patient care and our learning and working environments. The purpose of this study was to establish an understanding of the interactions or processes involved in the development of good working relationships between generalists and specialists.
METHODS
Design
To understand the main concern encountered by physicians in their working relationships and to develop a model for resolution of this concern, grounded-theory approach was used.18,19 Grounded theory is best for research questions that ask “what are the interactions or processes going on here?”18 Grounded theory was developed in sociology and uses a constant comparative method.20 Our aim was to develop an understanding of the working relationships between family physicians and other physicians.
The study received ethical approval from the Health Research Ethics Board of the University of Alberta.
Setting and study sample
The research team consisted of a family physician, a psychologist, a researcher with expertise in grounded theory, and an infectious disease specialist. Ideally, researchers using grounded theory should do so without preconceived ideas of the subject under study. This was not the case in our study, as the family physician identified respect from specialists as a concern for family physicians in previous research,8,9 the psychologist dealt with problematic physician working relationships, and the specialist thought there was a need to model ideal family physician and specialty working relationships for learners. The team was cognizant of these potential biases and attempted to seek findings other than those supporting their preconceived ideas.
The research setting included 2 inpatient family practice units located in Edmonton, Alta. Both units involved academic family physicians. One was a tertiary care hospital with 12 family physicians, and the other was a community hospital with 15 to 18 family physicians. In these settings family physicians work closely with nurses, nurse practitioners, and specialist consultants. Learners included occasional medical students, family medicine residents, and specialty residents whose preceptors were consulted about particular patients.
Purposeful sampling identified key informants to represent junior and senior family physicians, residents, general internists, and other physicians who worked closely with each unit. The researchers interviewed a family physician from each unit to obtain an understanding of the working environment in each unit and to help identify potential participants. Potential informants were invited to participate, and all those who were approached agreed to participate. They were given an information letter describing the project.
The 11 participants graduated from medical school between 1977 and 2001 (Table 1). This physician sample varied in sex, age, years in practice, and specialty and was selected using maximum variation sampling to identify and describe common patterns that transcended a focused sample, providing themes that were common to all.21,22 As an understanding of physician working relationships emerged, theoretical sampling23 was used to inform the selection of informants and collect information from relevant sources not previously considered. We assumed that emergency physicians and general internists would perceive themselves to be specialists; however, we found that they perceived themselves to be generalists, as they treated undifferentiated illness and, like other generalists, were frustrated with the specialist approach. Hence, theoretical sampling23 was used to identify a subspecialist with a focus on specific organ systems. Theoretical saturation was obtained at the sixth interview, as new information did not provide further insight in the categories of information obtained.22
Table 1.
Description of study sample
| DEMOGRAPHIC CHARACTERISTIC | PROPORTION (N) |
|---|---|
| Sex | |
| • Female | 36 (4) |
| • Male | 64 (7) |
| Setting | |
| • Community hospital | 18 (2) |
| • Academic hospital | 55 (6) |
| • Both community and academic hospital | 27 (3) |
| Specialty | |
| • Family physician | 36 (4) |
| • Family medicine resident | 9 (1) |
| • General internist | 27 (3) |
| • Subspecialist | 9 (1) |
| • Emergency physician | 18 (2) |
Data collection
Two guiding questions and a semistructured interview guide were developed based on the research team’s collective experience, the related literature, and discussions with other physicians (Box 1). These were presented at a Department of Family Medicine Research Forum to solicit further input and feedback from academic family physicians.
Box 1. Guiding questions and interview guide.
Two main guiding questions:
Please reflect on your experience on this unit and the physicians’ working relationships.
We are interested in the working relationships between the family physician and other physicians (family physicians, consultants, and specialists) on this unit. Could you describe these to us?
We are also interested in the effects the working relationships between the family physician and other physicians (family physicians, consultants, and specialists) on this unit have on learners. Could you describe the effects these relationships have on learners?
Probing questions (if needed):
Part 1
What are the working relationships on the unit?
What is your understanding of the relationships and how they work together?
Has your experience on the unit provided you with a realistic view of how various physician specialties can work together to provide efficient, comprehensive continuity of care to patients? If not, how could it be improved?
What are effective working relationships between physicians?
How are effective working relationships between physicians developed?
How are effective working relationships between physicians maintained?
Is there anything that could be done differently to improve the situation?
How different or similar are the working relationships on this unit compared with other settings you have worked in?
Part 2
Do you think the relationships on this unit have an effect on learners? In what way?
How have the relationships on this unit affected your attitude toward family physicians?
How have the relationships on this unit affected your attitude toward specialists?
Is this learning environment relevant to family practice? Please explain your answer.
Based upon your experience on the academic unit, do you think learners developed an understanding of the relationships between various physicians?
How does this unit compare with other settings you have worked in (with regards to effects on learning)?
[For medical students] Have you decided which residency program discipline you plan to pursue? Has your experience influenced your decision about which specialty you would like to pursue?
Individual semistructured interviews were conducted by the family physician and psychologist to obtain candid, unencumbered information from each informant.22 The interviews took 1 to 1.5 hours to conduct, in order to obtain each informant’s detailed story, and they were audiotaped and transcribed verbatim. The interview guide helped to ensure that key areas were discussed, and it was modified as interviews progressed to accommodate emerging questions. Field notes were recorded immediately after each interview, including descriptions of where the interview was held; reflections on how the interview went, including visual cues such as body language; and memorandums on possible relationships or issues to consider exploring in future interviews.
Journal entries were made throughout the project. These included memorandums or comments about possible linkages or relationships between data, ideas on emerging themes or areas that need further exploration, the researchers’ evolving perceptions and understandings, potential biases, and contradictory information that needed further exploration.
Data analysis
Analysis involved coding and categorizing the transcribed information. This was initially done manually, then with the use of NVivo software. The transcripts and memorandums were read and reread. Initially, open coding was used, with each idea given a code name (a word or phrase summarizing the main idea). Two investigators (D.M. and L.B.) coded approximately 5 pages of the document independently and then met to discuss and develop consensus on the coding.
The codes were grouped according to their properties and types, and they were grouped into categories. Through coding and developing categories, relationships between different ideas began to emerge and these were written as memorandums. Sorting the memorandums helped to clarify themes and, through theoretical coding, a framework emerged. This model followed Glaser’s description of a grounded-theory approach.19,23
Rigour of the study
Several methods were used to ensure the study was rigorous and trustworthy. Coding was initially done independently by 2 researchers. Regular meetings were held with team members to review the evolving understanding. Varied perspectives from the research team challenged preconceived ideas. The grounded-theory concept of interchangeability of indicators20 was achieved, as various indicators described in the discussion could be interchanged and still lead to the same core variable. Feedback was solicited from participants, a social worker, and a palliative care physician.
Our work addressed Glaser’s23 4 criteria for doing and judging grounded theory: fit (the concept expressed fit the pattern in the data), workability (the conceptualization obtained accounts for how the main concern is resolved), relevance (the study deals with the real concern of physicians feeling overwhelmed), and modifiability (the theory can be modified).
FINDINGS
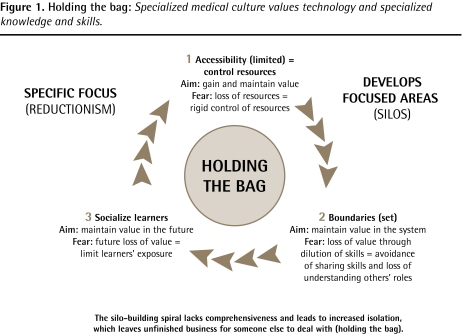
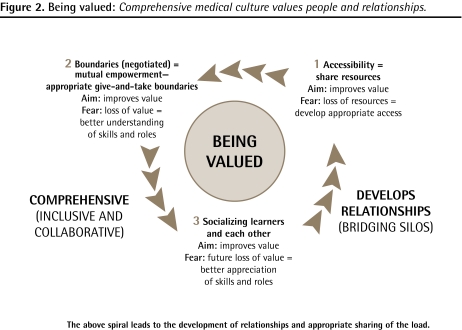
Medical cultures
Two distinct cultures emerged from the analysis: a specialist culture and a generalist or comprehensive culture. Distinctions in knowledge, skills, and values between the 2 cultures could be summarized as focused versus comprehensive. A specialized medical culture delineated areas of focus and expertise by limiting access to valued resources, setting boundaries, and socializing others according to their areas of expertise. The main concern generalists identified was feeling that they were left holding the bag—that they felt overwhelmed when they perceived specialists to be imposing work on them without negotiation. A comprehensive medical culture valued people and relationships, bridging silos by being accessible, developing mutual empowerment through negotiation of boundaries, and socializing others about everyone’s roles and responsibilities.
Specialist medical culture
The specialists focused on technology, concepts, and specific details of diseases and organs. For example, one participant indicated a preference for “Focusing more on specific things in medicine; I liked that.” (Interview 11)
A specialist culture was clearly identified at the tertiary care hospital, which valued technology and specialized knowledge and skills with a disease and organ focus: “[W]e’ve been promoting people based on research productivity and research [that] is basically disease based.” (Interview 4) The faculty sought physicians with specialized skills in focused areas to bring prestige to the university.
Comprehensive medical culture
The generalists’ focus was comprehensive, treating both differentiated and undifferentiated illnesses. The relationships that these physicians developed were integral to their work. “We are generalists, which means we are focused on patients, not disease.” (Interview 4)
A comprehensive medical culture was prominent in the community hospital setting, where comprehensive clinical skills and service were the primary focus: “Their mission statement isn’t clouded by issues of research or other issues. Largely it’s purely patient care.” (Interview 6)
An overwhelmed medical system
An overwhelmed medical system was described as lacking the resources to deal with the large number of patients. Many problems that physicians dealt with were not medical in nature but were the result of deficiencies in the system, such as the inability to move patients out of the hospital into long-term care beds.
Yeah, you can’t get them off the ward, so it all funnels down to emergency eventually; and we’re hearing that there’s difficulty and even fear about getting people transferred onto a long-term care bed.
(Interview 6)
Highly skilled specialists often lacked the skills to manage general medical and nonmedical problems, and having them manage these types of problems was seen as a poor use of their resources and time in the tertiary care hospital. Consequently, overworked generalists, who might be more familiar with managing systemic issues, felt obliged to provide comprehensive medical care to those who most required it. As the general medical and nonmedical problems did not go away, generalists often had to deal with them, leaving the generalists with a perception that work was imposed upon them without negotiation—that they were left holding the bag.
Holding the bag meant that generalists were left with the responsibility for patients specialists refused or were unable to provide care for, but they were unsure of their role. Were they responsible for providing comprehensive care for the specialists’ patients as consultants or as the responsible physicians?
In the specialist culture, the specialist was better able to control resources, set boundaries, and socialize learners to adopt these values, which often resulted in the generalists, once again, holding the bag (Figure 1).
Figure 1.
Holding the bag: Specialized medical culture values technology and specialized knowledge and skills.
In the comprehensive culture, a work culture that valued both the specialist and generalist was described. The organizational structure in the community hospital reinforced common values and facilitated the development of peer-to-peer working relationships, thus bridging the silos. The workload was negotiated, leading to a sense of sharing the load (Figure 2).
Figure 2.
Being valued: Comprehensive medical culture values people and relationships.
I’m hearing it’s sort of from the top down in terms of the organizational structure, where it’s got a clear mission that pretty well everyone agrees to and wants to work together, and they realize that these are long-term relationships.
(Interview 6)
Three themes emerged as key to either developing healthy balanced peer-to-peer relationships or leading to increased isolation. These were accessibility, negotiation of boundaries, and socializing learners and others.
Accessibility
Specialist culture: The specialist culture limited accessibility through control of resources. The valuing of technology and diseases provided some physicians with better control of resources, which helped them to maintain a valued position in the medical hierarchy: “The hierarchy comes in the toys that get used and the access to the toys.” (Interview 10)
Comprehensive culture: In the comprehensive culture accessible and approachable physicians were more likely to develop and maintain ongoing relationships. Appropriate accessibility was negotiated between the physicians, working out details such as when to consult and what workup should be done before a consultation. Being accessible led to the appropriate sharing of resources. “Radiology knows us by name. You know we phone them up or we go down there and review films. And I think that’s pretty unique.” (Interview 8)
Negotiating boundaries and mutual empowerment
Specialist culture: In the specialist culture the focus on naming and categorizing diseases of specific organs better enabled physicians to define their areas of expertise and limit their roles. Some subspecialists saw their roles as only focused on their diseases of interest and deferred care of the patient onto others without negotiation: “We now have a culture which thinks that in subspecialty medicine ... their real job is to look after the disease of the patient.” (Interview 4)
There was a lack of understanding of the role of generalists who treated undifferentiated illness or unnamed illnesses. They were sometimes devalued and perceived to treat nothing. One participant illustrated this point: “You know, well this person, there’s nothing really wrong with them; they should go to family practice.” (Interview 8)
Comprehensive culture: Appropriate boundaries were set when mutual empowerment occurred and physicians valued one another. There was concern and attention to fairness and justice within these shared power relations. These were described as give-and-take symbiotic relationships.
I mean, it’s certainly my point of view, but I think the majority of the department, you know, really does look at it as a symbiotic relationship, where ... there’s no way we could admit all these patients without the family practice physicians .... And one thing that I know our department has talked about a lot is, you know, just always trying to make sure that all the teams are equal as far as the workload.
(Interview 8)
Socializing learners and one another
Specialist culture: Learners immersed and mentored in a specialist culture were described as adopting the specialist culture and values. This was a concern when training generalists: “The problem is that we’re all trying to train generalists in a culture that is clearly partialization.” (Interview 4) Some students immersed in a specialist culture were described as valuing specialists over generalists. Some thought that “they were better than a family doctor because they’re going to be specialists.” (Interview 3)
Comprehensive culture: Understanding and experiencing one another’s roles led to valuing others’ potential contributions: “[P]erhaps from walking in shoes of other persons there would be greater collegiality.” (Interview 4) With recognition of the valuable role of both generalists and specialists, efforts were made to socialize learners in both cultures. One participant described it as being “like when you go to church or Sunday school, you learn what’s expected behaviour in that environment.” (Interview 6)
Consequences of the medical cultures
A specialized medical culture that limits accessibility through controlling resources, setting boundaries, and socializing learners and others to adopt these values can lead to increased isolation (Figure 1). This might have contributed to the development of silos and a sense of isolation in the tertiary care hospital. One participant commented, “We practise in stove pipe isolation. I come in and I give my [specialty] advice, cardiology comes in and gives their cardiology advice, and endocrine gives their diabetes advice.” (Interview 11)
Specialist physicians practising in isolation focused on being valued and on their boundaries in the hierarchical system, and they sometimes did not recognize others’ expertise or roles in the system, as one participant commented: “[T]he other specialists don’t necessarily recognize that we have that expertise.” (Interview 7)
Physicians sought to become valued in a specialist culture by adopting a specialized focus: “Now, family medicine hasn’t been immune from those pressures, because what’s happening in family medicine? There’s more and more specialization within family medicine.” (Interview 4) Generalists who specialized reduced the pool of generalists available to deal with the ever increasing undifferentiated, complex workload.
[The workload] just became overwhelming, you know, and actually [a number of doctors] gave up medicine privileges because of that. But then the hospital was left still with all the patients coming in, you know.
(Interview 6)
A comprehensive medical culture with appropriate accessibility and sharing of resources, negotiation of boundaries that mutually empowers physicians, and socialization of learners to adopt these values might contribute to collaborative physician relationships that reduce isolation and overwork through bridging silos (Figure 2).
DISCUSSION
There is a need for both generalists, who provide first-contact and comprehensive personalized care, and specialists, with their specific expertise and skills, in the medical system.24 Our current medical culture arose from a disease-focused biomedical model and might be more representative of a specialist culture. This is reflected in our billing and classification systems that depend upon the International Classification of Disease codes. Much illness experience cannot be captured using this biomedical approach, and some argue that another model might be required.25
Much has been written about the importance of the doctor-patient relationship and the healing that can occur within healing relationships.26 Physician-physician relationships could be equally important. The need to develop relationships between family physicians and other specialists and for them to support each other’s roles was described in a Delphi survey.9
Our study suggests that a specialist culture affects physician relationships through controlled access to resources and increased ability of specialists to set boundaries around their work. This might lead to reductionism and isolation and decrease the quality of patient care, which could explain, in part, the increase in mortality observed in countries with higher specialist-to-population ratios.27 Stange has described how a health care crisis has been created by fragmentation through a disease-focused approach.28
Our current medical culture might also affect the socialization of learners and others. One qualitative study described how internists were socialized to avoid doctor-patient relationships.29 Learning environments that immerse learners in a culture of collaboration might better prepare future physicians. Programs, such as family health teams in Ontario, have been developed to address this concern.30 There is evidence that these innovative learning environments improve knowledge and attitudes needed in collaborative settings.31
Our study suggests that a comprehensive culture that values and cultivates relationships leads to increased collaboration. Just as accessibility, mutual empowerment, and understanding each other’s roles might be important in the doctor-patient relationship, these aspects might be equally vital in doctor-doctor relationships, and they might be critical for the effective delivery of care. A comprehensive medical culture with collaborative physician relationships could explain the observed reduced mortality, improved outcomes, and lower costs associated with adequate primary care.32–35
Limitations
Our project focused on inpatient family medicine units in a large urban centre. Participants consisted of physicians who worked within this Canadian setting in Alberta. Nonphysician clinicians, medical students, and administrative staff were not interviewed and might have perspectives worth exploring. The researchers involved in the project had preconceived ideas from their previous work, which could contribute to a biased perspective.
Conclusion
We found that a specialist culture that values technology and focused interests might lead to increased physician isolation and the development of silos, leaving generalists feeling overwhelmed. This might contribute to problems within the system. A comprehensive culture that values relationships might lead to increased collaboration through improved accessibility by negotiated access to resources, mutual empowerment with negotiation of roles and responsibilities, and improved socialization of learners and others to adopt these values.
Considerations for further research include exploring what is valued in various medical systems and how to shift from valuing focused interests to developing and valuing relationships; and research broadening the issue of working relationships and environments to include other health care providers, as well as addressing the effects on learners, is needed.
Acknowledgments
Financial support was provided by the CPDiQ (Issues of Quality and Continuing Professional Development) project, under the auspices of the Association of Faculties of Medicine of Canada. Health Canada made the project possible with grant funding from the Health Canada Primary Healthcare Transition Fund. The views expressed herein do not necessarily reflect the views of Health Canada.
EDITOR’S KEY POINTS
There is a need for both specialist and generalist approaches in medicine. Understanding barriers and contributors to good collaborative physician working relationships could help improve patient care and our learning and working environments.
The purpose of this study was to establish an understanding of the interactions or processes involved in the development of good working relationships between generalists and specialists.
The authors found that the main concern generalists identified was feeling that they were left holding the bag in a culture that valued specialization—they felt overwhelmed when they perceived specialists to be imposing work on them without negotiation. A comprehensive culture valued both specialists and generalists; the organizational structure reinforced common values and facilitated development of peer-to-peer working relationships. Further, workload was negotiated, leading to a sense of sharing the load.
POINTS DE REPÈRE DU RÉDACTEUR
En médecine, on a besoin des façons de faire des spécialistes comme des généralistes. Comprendre les facteurs qui font obstacle ou qui facilitent une bonne collaboration entre médecins pourrait aider à améliorer les soins des patients et le milieu d’apprentissage et de travail.
Le but de cette étude était de mieux comprendre les interactions ou les processus qui jouent un rôle dans le développement de bonnes relations de travail entre généralistes et spécialistes.
Les auteurs ont trouvé que la préoccupation principale des généralistes était le sentiment d’avoir un rôle de second ordre dans une culture qui valorise la spécialisation – ils se sentaient accablés quand ils sentaient que les spécialistes leur imposaient du travail sans négociation. Une compréhension mutuelle valorisait spécialistes et généralistes; la structure organisationnelle renforçait les valeurs communes et facilitait le développement de relations d’égal à égal au travail. De plus, la tâche de travail était négociée, ce qui entraînait l’impression de partager le travail.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Dr Manca conceived and designed the study, developed the guiding questions, performed interviews, analyzed and interpreted the data, organized meetings of the investigators, and wrote the manuscript. Dr Breault assisted with the concept and design of the study, developing the guiding questions, performing interviews, analyzing and interpreting the data, and writing the manuscript. Dr Wishart assisted with the design of the study, analyzing and interpreting the data, and writing the manuscript. All authors reviewed and approved the manuscript for publication.
Competing interests
None declared
References
- 1.Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA. 1995;273(13):1026–31. [PubMed] [Google Scholar]
- 2.Langley GR, Minkin S, Till JE. Regional variation in nonmedical factors affecting family physicians’ decisions about referral for consultation. CMAJ. 1997;157(3):265–72. [PMC free article] [PubMed] [Google Scholar]
- 3.College of Family Physicians, Royal College of Physicians and Surgeons of Canada . Family physicians and other specialists: working and learning together. Conjoint discussion paper. Mississauga, ON: College of Family Physicians of Canada; 2006. Available from: www.cfpc.ca/English/cfpc/communications/health%20policy/published%20Reports/default.asp?s=1. Accessed 2009 May 13. [Google Scholar]
- 4.Marshall MN. How well do GPs and hospital consultants work together? A survey of the professional relationship. Fam Pract. 1999;16(1):33–8. doi: 10.1093/fampra/16.1.33. [DOI] [PubMed] [Google Scholar]
- 5.Crookshank FG. Theory of diagnosis. Lancet. 1926;208(5384):939–42. [Google Scholar]
- 6.Jelinek M. Spectrum bias: why generalists and specialists do not connect. Evid Based Med. 2008;13(5):132–3. doi: 10.1136/ebm.13.5.132. [DOI] [PubMed] [Google Scholar]
- 7.Rosser WW. Approach to diagnosis by primary care clinicians and specialists: is there a difference? J Fam Pract. 1996;42(2):139–44. [PubMed] [Google Scholar]
- 8.Manca DP, Varnhagen S, Brett-MacLean P, Allan GM, Szafran O, Ausford A, et al. Rewards and challenges of family practice. Web-based survey using the Delphi method. Can Fam Physician. 2007;53:278–86. [PMC free article] [PubMed] [Google Scholar]
- 9.Manca D, Varnhagen S, Brett-MacLean P, Allan GM, Szafran O. RESPECT from specialists. Concerns of family physicians. Can Fam Physician. 2008;54:1434–5.e1–5. Available from: www.cfp.ca/cgi/reprint/54/10/1434. Accessed 2011 Mar 21. [PMC free article] [PubMed] [Google Scholar]
- 10.Theman T. Registrar’s report. The Messenger. 2006;124:3–4. Available from: www.cpsa.ab.ca/Resources/Messenger/Messenger_Archives.aspx. Accessed 2010 Feb 24. [Google Scholar]
- 11.Hearst N, Shore WB, Hudes ES, French L. Family practice bashing as perceived by students at a university medical center. Fam Med. 1995;27(6):366–70. [PubMed] [Google Scholar]
- 12.Hunt DD, Scott C, Zhong S, Goldstein E. Frequency and effect of negative comments (“badmouthing”) on medical students’ career choices. Acad Med. 1996;71(6):665–9. doi: 10.1097/00001888-199606000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Biggart JH. Cnidos v. Cos. Ulster Med J. 1971;41(1):1–9. [PMC free article] [PubMed] [Google Scholar]
- 14.McWhinney IR. Are we on the brink of a major transformation of clinical method? CMAJ. 1986;135(8):873–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Pearson SD. Principles of generalist-specialist relationships. J Gen Intern Med. 1999;14(Suppl 1):S13–20. doi: 10.1046/j.1525-1497.1999.00259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stewart M, Brown J, Levenstein J, McCracken E, McWhinney IR. The patient-centred clinical method. 3. Changes in residents’ performance over two months of training. Fam Pract. 1986;3(3):164–7. doi: 10.1093/fampra/3.3.164. [DOI] [PubMed] [Google Scholar]
- 17.Levenstein JH, McCracken EC, McWhinney IR, Stewart MA, Brown JB. The patient-centred clinical method. 1. A model for the doctor-patient interaction in family medicine. Fam Pract. 1986;3(1):24–30. doi: 10.1093/fampra/3.1.24. [DOI] [PubMed] [Google Scholar]
- 18.Rowan M, Huston P. Qualitative research articles: information for authors and peer reviewers. CMAJ. 1997;157(10):1442–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Glaser BG. Basics of grounded theory analysis: emergence vs. forcing. Mill Valley, CA: Sociology Press; 1992. [Google Scholar]
- 20.Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Hawthorne, NY: Aldine de Gruyter; 1967. [Google Scholar]
- 21.Kuzel A. Sampling in qualitative inquiry. In: Crabtree BF, Miller W, editors. Doing qualitative research in primary care: multiple strategies. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999. pp. 33–45. [Google Scholar]
- 22.Creswell JW. Qualitative inquiry and research design: choosing among five approaches. 2nd ed. Thousand Oaks, CA: Sage Publications; 2007. [Google Scholar]
- 23.Glaser BG. Doing grounded theory: issues and discussions. Mill Valley, CA: Sociology Press; 1998. [Google Scholar]
- 24.Stange KC. The generalist approach. Ann Fam Med. 2009;7(3):198–203. doi: 10.1370/afm.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wade DT, Halligan PW. Do biomedical models of illness make for good healthcare systems? BMJ. 2004;329(7479):1398–401. doi: 10.1136/bmj.329.7479.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scott JG, Cohen D, Dicicco-Bloom B, Miller WL, Stange KC, Crabtree BF. Understanding healing relationships in primary care. Ann Fam Med. 2008;6(4):315–22. doi: 10.1370/afm.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Starfield B, Shi L, Grover A, Macinko J. The effects of specialist supply on populations’ health: assessing the evidence. Health Aff (Millwood) 2005:W5-97–W5-107. doi: 10.1377/hlthaff.w5.97. (Suppl Web Exclusives): [DOI] [PubMed] [Google Scholar]
- 28.Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009;7(2):100–3. doi: 10.1370/afm.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mizrahi T. Getting rid of patients: contradictions in the socialisation of internists to the doctor-patient relationship. Sociol Health Illn. 1985;7(2):214–35. doi: 10.1111/1467-9566.ep10949079. [DOI] [PubMed] [Google Scholar]
- 30.Price D, Howard M, Hilts L, Dolovich L, McCarthy L, Walsh AE, et al. Interprofessional education in academic family medicine teaching units. A functional program and culture. Can Fam Physician. 2009;55:901–1.e1–5. Available from: www.cfp.ca/cgi/reprint/55/9/901. Accessed 2011 Mar 21. [PMC free article] [PubMed] [Google Scholar]
- 31.Remington TL, Foulk MA, Williams BC. Evaluation of evidence for inter-professional education. Am J Pharm Educ. 2006;70(3):66. doi: 10.5688/aj700366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shi L, Starfield B, Kennedy B, Kawachi I. Income inequality, primary care, and health indicators. J Fam Pract. 1999;48(4):275–84. [PubMed] [Google Scholar]
- 33.Forrest CB, Starfield B. Entry into primary care and continuity: the effects of access. Am J Public Health. 1998;88(9):1330–6. doi: 10.2105/ajph.88.9.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Franks P, Fiscella K. Primary care physicians and specialists as personal physicians. Health care expenditures and mortality experience. J Fam Pract. 1998;47(2):105–9. [PubMed] [Google Scholar]
- 35.Franks P, Clancy CM, Nutting PA. Gatekeeping revisited—protecting patients from overtreatment. N Engl J Med. 1992;327(6):424–9. doi: 10.1056/NEJM199208063270613. [DOI] [PubMed] [Google Scholar]