Summary
Non-communicable diseases are rapidly overtaking infectious, perinatal, nutritional and maternal diseases as the major causes of worldwide death and disability. It is estimated that within the next 10-15 years, the increasing burden of chronic diseases and the ageing of the population will expose the world to an unprecedented burden of chronic diseases. Preventing the potential ramifications of a worldwide epidemic of chronic non-communicable diseases in a sustainable manner requires coordinated, collaborative efforts. Herein we present our collaboration's strategic plan to understand, treat and prevent chronic cardiovascular and pulmonary disease in Western Kenya which builds on a two decade partnership between academic universities in North America and Kenya; the Academic Model Providing Access to Healthcare (AMPATH). We emphasize the importance of training Kenyan clinician-investigators who will ultimately lead efforts in cardiovascular and pulmonary disease care, education and research. This penultimate aim will be achieved by our five main goals. Our goals include creating an administrative core capable of managing operations, develop clinical and clinical research training curricula, enhancing existing technology infrastructure and implementing relevant research programs. Leveraging a strong international academic partnership with respective expertise in cardiovascular medicine, pulmonary medicine and medical informatics we have undertaken to understand and counter cardiovascular and pulmonary disease in Kenya by addressing patient care, teaching and clinical research.
Introduction
Chronic non-communicable cardiovascular and pulmonary diseases are rapidly overtaking infectious diseases as the major cause of death and disability in the developing world (Figure 1). In 2002, it was estimated that 29% of deaths worldwide were due to cardiovascular disease (CVD) and that 43% of the global morbidity and mortality was attributable to CVD.1 By 2015, 41 out of 64 million deaths will be due to chronic diseases and 80% of deaths from chronic diseases will occur in low- and middle-income countries.1-3 Compounding this problem, these deaths typically occur at earlier ages than in high-income countries.4 Chronic obstructive pulmonary disease represents the major burden of chronic pulmonary disease worldwide. In two large multinational studies, the prevalence of chronic obstructive pulmonary disease (COPD) in developing countries was twice that of North America.5, 6 While worldwide, tobacco smoking remains the most important cause of COPD, the World Health Organization (WHO) estimates that in low and middle income countries, 35% of people with COPD developed the disorder after exposure to biomass fuels.7 Death and disability in middle age due to preventable cardiovascular and pulmonary disease (CVPD) have major social and economic consequences, depriving families of parents, workplaces of employees, patients of healthcare workers and communities of leaders, not to mention increased competition for limited health care funds. Herein we describe a sustainable model to counter this epidemic based on the Academic Model Providing Access to Healthcare (AMPATH) consortium of universities from North America and Kenya.
Figure 1.
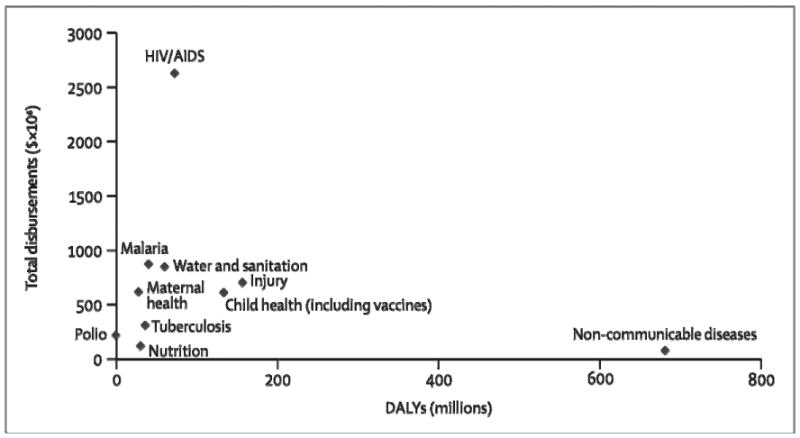
2001 disability-adjusted life years (DALYs) versus 2005 disbursements of World Bank, US Government, Bill & Melinda Gates Foundation, Global Fund to fight HIV/AIDS, Tuberculosis and Malaria. From Sridhar and Batniji. Misfinancing global health: a case for transparency in disbursements and decision making. Lancet (2008) vol. 372 (9644) pp. 1185-91.
Methods
The creation of this manuscript was supported in part by the National Heart Lung and Blood Institute Global Health Initiative's AMPATH Cardiovascular and Pulmonary Disease Center of Excellence (HV-09-12), the NIH Fogarty International Clinical Research Fellowship Program (R24TW007988) and the Dr. Joseph C. Greenfield Scholar Award in Cardiovascular Medicine at Duke University. The authors are solely responsible for drafting and editing of this paper.
The Need: An Epidemic of Cardiovascular and Pulmonary Disease in Developing Countries
It is well recognized that chronic non-communicable diseases exist to a significant degree in all regions of the world.8 Current estimates and projections on the burden of non-communicable diseases worldwide demonstrate that sub-Saharan Africa differs from the rest of the developing world as it relates to the rate at which these transitions are occurring (Figure 2). If projections of the burden of CVD are correct and the epidemiologic transition occurs in sub-Saharan Africa the way it has in other developing regions of the world, then a true opportunity for primary (and primordial) prevention exists in sub-Saharan Africa. Out of all six WHO regions, Africa stands to gain the most in life expectancy by enacting interventions now to lower cardiovascular risk.7, 9, 10 With regard to chronic non-communicable pulmonary diseases, the same is true regarding tobacco smoking, however, breathing air tainted by the burning of biomass fuels may be more important, especially among women.11
Figure 2.
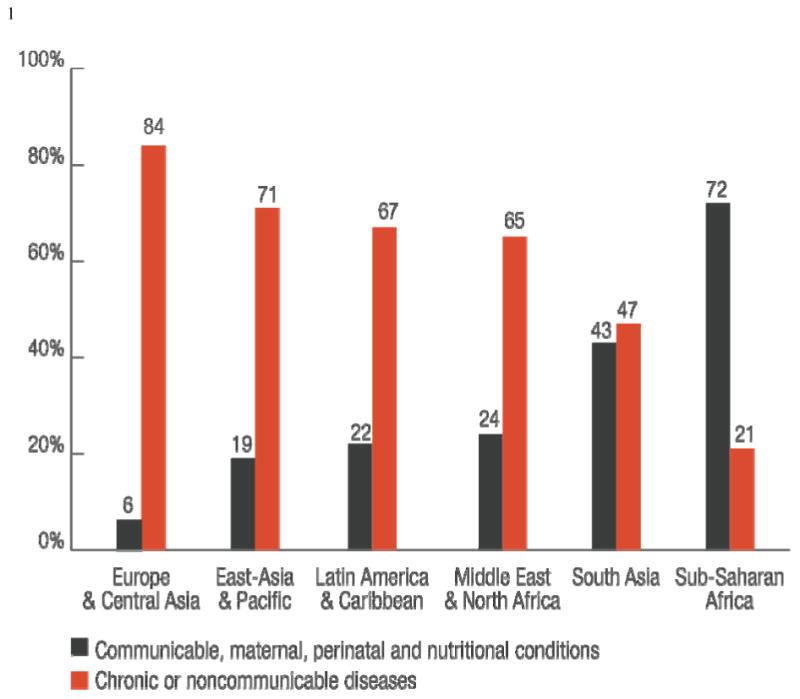
Worldwide share of deaths by cause and World Bank Region (excluding high-income countries, 2002). From Suhrcke Chronic Disease: An Economic Perspective. Oxford Health Alliance (2006) pp. 1-60
The landmark studies demonstrating the epidemiologic transition in sub-Saharan Africa have predominantly emanated from South Africa and Nigeria. Although often considered to be a homogeneous entity, the countries in the sub-Saharan Africa region are different and merit to be recognized accordingly. Research investigating cardiovascular and pulmonary diseases in the rest of the continent is lacking. This is in part due to critical health workforce shortages in sub-Saharan Africa. There is a dearth of both workforce and infrastructure capable of dealing with the burgeoning epidemic as well as clinician-investigators to ensure that research is relevant to local community health concerns.12, 13 As the Institute of Medicine reported in 2010, efforts to improve cardiovascular and pulmonary health in the developing world are more likely to succeed if they are carried out within existing global health missions.14
One Response: The AMPATH Cardiovascular and Pulmonary Disease Center of Excellence
In 2009, The National Heart, Lung, and Blood Institute in partnership with UnitedHealth Group established a network of collaborating Centers of Excellence (COE) characterized by academic collaborations between medical schools in the U.S. and partner institutions in developing countries.15, 16 These COEs have the ultimate goal of countering the burden of non-communicable CVPD in developing nations by enhancing the infrastructure and training necessary to conduct innovative and locally-relevant clinical research.15 One of the 11 initial NHLBI COEs is in western Kenya where Moi University School of Medicine (MUSOM) has a 22-year relationship with more than a dozen US medical schools lead by Indiana University. This collaboration, named USAID AMPATH has the stated goal to build upon an academic foundation that supports all three academic missions of service, teaching, and research. AMPATH's Kenyan partner institutions include Moi Teaching and Referral Hospital (Kenya's second national referral hospital) and Moi University School of Medicine that provide care, teach, and perform research in networks of urban and rural Ministry of Health hospitals and health centers in western Kenya. AMPATH delivers a comprehensive, community-based care program that initially focused on patients infected with HIV but has since been expanded to provide primary care and chronic disease management to an assigned catchment population of nearly 2 million persons. The history, organizational structure, and health programs of USAID AMPATH have been described elsewhere.17, 18 AMPATH emphasizes partnership between regional Kenyan leadership and a diverse consortium of providers. To date, more than 115,000 HIV-infected patients have been enrolled in AMPATH and more than 70,000 are currently receiving care. AMPATH is now the largest HIV/AIDS care program in Kenya and one of the largest in all of sub-Saharan Africa.
Implementing a transnational, multi-institution collaboration between academic medical centers focused on combating CVPD presents unique challenges. In addition to the challenges presented by physical and temporal separation, the inequalities in infrastructure, resources and administrative capacity had to be addressed and overcome. A first step was building relationships. Counterpart relationships at the individual and departmental level are the cornerstone of the AMPATH partnerships.19 These relationships have resulted in the bidirectional exchange of over 1000 faculty members, postgraduate trainees and students. Reliable and varied modes of communication also had to be developed. Training of clinicians, nurses, researchers, data and laboratory technicians and administrative staff are necessary in order to build a sustainable program that addresses clinical care, public health and training of the next generation of clinician scientists. Adopting the infrastructure which has served the endeavors within HIV care to fit the unique demands of a non-communicable disease focused program has posed its own challenges in terms of data acquisition, care models, care protocol development and screening. Within each of these facets, communication with the community at large helped to forge the relationships upon which we would build a successful large-scale chronic disease management program.
The AMPATH CVPD COE aligns the existing strengths of AMPATH with specific needs relevant to CVPD in order to achieve goals across five domains. The 5 main goals of the AMPATH CVPD COE, selected strengths of the AMPATH program, specific needs and examples of steps we have taken to achieve these goals are shown in the Table. Although these goals, strengths, needs and implementation examples are presented distinctly, many of these principles apply to more than one goal. It is our plan that the effects of each implementation support the overall efforts of the AMPATH CVPD COE synergistically.
Table. Goals of the AMPATH Cardiovascular and Pulmonary Disease Center of Excellence with Existing Strengths, Necessary Enhancements and Examples of Implementation for each goal.
| Goal 1. Organize an administrative core for CVPD clinical care, training and research | ||
|
| ||
| Existing Strengths* | Desired Outcome | Implementation Examples |
|
|
|
| Goal 2. Develop and implements a competency-based clinical training curriculum | ||
|
| ||
| Existing Strengths | Desired Outcome | Implementation Examples |
|
|
|
| Goal 3. Establish a CVPD clinical research training program | ||
|
| ||
| Existing Strengths | Desired Outcome | Implementation Examples |
|
|
|
| Goal 4. Adopt and enhance AMPATH's existing data management and laboratory infrastructure and research network for CVPD | ||
|
| ||
| Existing Strengths | Desired Outcome | Implementation Examples |
|
|
|
| Goal 5. Implement research programs to address prevalence, prevention and treatment of CVPD that afflict citizens of western Kenya | ||
|
| ||
| Existing Strengths | Desired Outcome | Implementation Examples |
|
|
|
These strengths are applicable across goals and are not limited in their utility to one specific goal
Actionable Data: a good place to start
It is widely believed that sub-Saharan Africa is in the early stages of the epidemiologic transition, however, these conclusions are largely based on data from a small number of countries. In Kenya, population or community-based data on the burden of CVPDs and their risk factors are lacking. We will collect surveillance data on cardiovascular and pulmonary diseases and risk factors through pilot projects (community- and hospital-based) and through enhancements to the elements routinely collected through the AMPATH clinical care program. One of our pilot projects is a community-based assessment of the prevalence of hypertension and CVD risk factors – the leading risk factor for myocardial infarction in sub-Saharan Africa.20 This endeavor will ultimately involve a home-based screening program for hypertension and diabetes carried out with the aid of teams of community health workers and community-owned resource persons who will do the screening. Data acquisition will occur with the aid of smart phones that will send data securely using wireless technology to a main server thereby limiting the need for paper forms, travel from remote sites, and will decrease delays in data entry. To date, our home-based screening program has focused mostly on HIV and tuberculosis and has achieved a high level (>90%) of acceptance in most communities. We have signed a memorandum of understanding with the Kenyan Ministry of Health to expand our program to include screening for chronic non-communicable diseases.
In addition to community-level screening, our clinical research program is also focused on training clinician investigators. The clinical training program will expose our trainees to the preventive as well as the therapeutic aspects of cardiovascular and pulmonary medicine and, as such, will include exposure to advanced diseases at our referral hospital. During the initial funding period, we have chosen to thematically link our investigative program to chronic dyspnea and the clinical syndrome of heart failure: its recognition, systematic assessment, documentation, etiologic characterization, prevention, and management. We have begun a series of dyspnea-related investigative programs utilizing enhanced data collection and diagnostic tools that will be implemented in parallel with our clinical and research training efforts. While these programs each target separate research questions, clinical skills, and patient and clinician cohorts, unifying research methodologies will be employed. These include: 1) retrospective analyses of the AMPATH electronic medical record system, 2) a protocol-based approach to diagnostic testing among patients with dyspnea or hypoxemia, 3) prospective observational cohort studies, and 4) interventional studies. Causes of dyspnea are investigated by enhancements in the pulmonary and cardiac laboratories (i.e., spirometry and echocardiography). Highlighting the importance of these different methodologies and building upon available resources, the AMPATH CVPD COE has begun a series of pilot studies. Building on the theme of dyspnea, these pilot studies focus on the epidemiology of CHF and the cardiopulmonary sequelae of indoor air pollution. These initiatives will energize future clinicians and investigators and build a culture of cyclical evidence-based quality improvement - plan, do, study, and act - and an appreciation of evidence-based care necessary to transform chronic CVPD prevention and treatment in Western Kenya. Understanding the epidemiology of CVPDs and their risk factors is an important first step that will inform our future efforts. Lastly, the AMPATH program, as it moves to include chronic non-HIV disease management, has expanded the scope of information that clinicians routinely collect on all patients during a clinical outpatient encounter. Data collection, data entry and information technology forms and processes are being enhanced to routinely collect surveillance on dietary salt intake, detailed tobacco use, indoor air pollution, physical activity and family history of cardiovascular and pulmonary diseases.
Making it back to the bedside
Research and training without a comprehensive clinical care model will not affect cardio-pulmonary morbidity or mortality in sub-Saharan Africa. We do not believe that the presence of outstanding researchers and carefully trained doctors automatically translates into improved clinical care for Africans. We do believe that a sustainable approach outlined at the outset of our endeavor will help. We can take lessons learned during rapid anti-retroviral therapy expansion under the President's Emergency Plan For AIDS Relief funding. The United States' emergency response to the HIV/AIDS epidemic was focused on getting antiretroviral therapy quickly to those most in need, demonstrating the feasibility of protocol-driven treatment and monitoring programs, and showing progress in meeting enrollment and treatment targets. By any measure, PEPFAR has made tremendous gains in providing life-saving treatment to people infected with HIV.21 However, it has also offered important lessons on the limitations of a strictly vertical approach and to its credit has incorporated a number of these lessons as it has developed. One such lesson is the importance of linking knowledge, training and programs with the system of care providers in resource-limited settings and interfacing with these providers in an ongoing manner.
In Kenya, most patients are cared for by clinical officers (equivalent to a physician assistant's level of training) rather than physicians. We will include both physician scientists as well as clinical officers into our training model and prospectively assess this mixed clinical officer/physician care model on the processes and outcomes of care. In satellite clinics in remote parts of the region, we currently provide computer-based decision support to clinical officers via clinical summaries provided during patient visits and prospective computer reminders to reinforce clinical algorithms for HIV. We will expand these tools into chronic non-communicable CVPD. The AMPATH medical record system is a key factor in our ability to practice evidence-based medicine and translate what is learned from retrospective and prospective studies to inform the care model and the training we will provide to both physicians and non-physician health workers so that cardiovascular morbidity and mortality are reduced.
Summary
The epidemic of cardiovascular and pulmonary diseases that is burgeoning in the developing world is causing disproportionate morbidity and mortality. In India, East Asia and Eastern Europe, for example, mortality rates due to ischemic heart disease are already increasing22-25. The sub-Saharan African region is distinct in that there is mounting evidence of an epidemiologic transition although the mortality effects of the epidemiologic transition are yet to become apparent. Thus, there exists at least a region of the world where preventive medicine may truly be primarily preventive of chronic CVPD. Whereas much of the data representing the sub-Saharan African region have come from South Africa and Nigeria, more data are emerging from other sub-Saharan countries. Within Kenya, a fertile infrastructure exists by virtue of the AMPATH program's established infrastructure and academic partners.
Although AMPATH has traditionally been involved in HIV/AIDS care, the need for expansion into primary care and preventive medicine is apparent. Herein we have presented a new paradigm for how US and Kenyan academic medical centers can work together to treat and control chronic CVPDs. Consortium partners — Moi University, Duke University, Brown University and Indiana University — are recent recipients of one of eleven contracts with the NHLBI and UnitedHealth group to create a cardiovascular Center of Excellence in developing countries. Building upon the AMPATH foundation, the AMPATH CVPD COE is uniquely poised to rapidly impact cardio-pulmonary care in Western Kenya and, eventually, in the rest of sub-Saharan Africa. Our approach is timely and congruent with suggestions from a recent Institute of Medicine report that calls for expansion of existing major global initiatives to promote better primary health care to meet a range of health needs.14 We will draw upon the inherent power of the academic medical center and transnational, multi-institutional academic partnerships to effect real change in the health of all persons, especially persons who heretofore did not have access to health care. Our ultimate goal is to impact the health of the region immediately with care and training and sustainably by informing evidence-based health policy with research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mathers CD, Lopez AD, Stein C, et al. Deaths and Disease Burden by Cause: Global Burden of Disease Estimates for 2001 by World Bank Country Groups. 2005. Disease Control Priorities Project Working Paper No. 18; pp. 1–213. [Google Scholar]
- 2.WHO WHO Fact Sheet Number 317: Cardiovascular diseases (CVDs) [July 27, 2010];2009 September; http://www.who.int/mediacentre/factsheets/fs317/en/index.html.
- 3.WHO . World Health Statistics 2008. Geneva: [July 27, 2010]. http://www.who.int/whosis/whostat/2008/en/index.html. [Google Scholar]
- 4.Reddy KS. Cardiovascular disease in non-Western countries. N Engl J Med. 2004;350(24):2438–40. doi: 10.1056/NEJMp048024. [DOI] [PubMed] [Google Scholar]
- 5.Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370(9589):741–50. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 6.Menezes AMB, Perez-Padilla R, Jardim JRB, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366(9500):1875–81. doi: 10.1016/S0140-6736(05)67632-5. [DOI] [PubMed] [Google Scholar]
- 7.Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–57. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 8.Beaglehole R, Bonita R. Global public health: a scorecard. Lancet. 2008;372(9654):1988–96. doi: 10.1016/S0140-6736(08)61558-5. [DOI] [PubMed] [Google Scholar]
- 9.WHO . Global Health Risks Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009. [Google Scholar]
- 10.Suhrcke M, Nugent RA, Stuckler D, et al. Chronic Disease: An Economic Perspective. London: Oxford Health Alliance; 2006. [Google Scholar]
- 11.Kurmi OP, Semple S, Simkhada P, et al. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65(3):221–8. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 12.Williams JR, Schatz EJ, Clark BD, et al. Improving public health training and research capacity in Africa: a replicable model for linking training to health and socio-demographic surveillance data. Global Health Action. 2010;3 doi: 10.3402/gha.v3i0.5287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen L, Evans T, Anand S, et al. Human resources for health: overcoming the crisis. Lancet. 2004;364(9449):1984–90. doi: 10.1016/S0140-6736(04)17482-5. [DOI] [PubMed] [Google Scholar]
- 14.Fuster V, Kelly BB, editors. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington, DC: Committee on Preventing the Global Epidemic of Cardiovascular Disease: Meeting the Challenges in Developing Countries; Institute of Medicine; 2010. [PubMed] [Google Scholar]
- 15.Nabel EG, Stevens S, Smith R. Combating chronic disease in developing countries. Lancet. 2009;373(9680):2004–6. doi: 10.1016/S0140-6736(09)61074-6. [DOI] [PubMed] [Google Scholar]
- 16.NHLBI National Heart Lung and Blood Institute Global Health Initiative. [July 27, 2010];2009 December 1; http://www.nhlbi.nih.gov/about/globalhealth/
- 17.Einterz RM, Kimaiyo S, Mengech HNK, et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007;82(8):812–8. doi: 10.1097/ACM.0b013e3180cc29f1. [DOI] [PubMed] [Google Scholar]
- 18.Mamlin JJ, Kimaiyo S, Nyandiko WM, et al. Perspectives and Practice in Antiretroviral Treatment. Geneva: World Health Organization; 2004. Academic Institutions Linking Access to Treatment and Prevention: Case Study. [Google Scholar]
- 19.Einterz RM, Kelley CR, Mamlin JJ, et al. Partnerships in international health. The Indiana University-Moi University experience. Infect Dis Clin North Am. 1995;9(2):453–5. [PubMed] [Google Scholar]
- 20.Steyn K, Sliwa K, Hawken S, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. 2005;112(23):3554–61. doi: 10.1161/CIRCULATIONAHA.105.563452. [DOI] [PubMed] [Google Scholar]
- 21.WHO . Progress Report. Geneva: 2009. Towards Universal Access: Scaling Up Priority HIV/AIDS Interventions in the Health Sector. [Google Scholar]
- 22.Joshi R, Chow CK, Raju PK, et al. Fatal and nonfatal cardiovascular disease and the use of therapies for secondary prevention in a rural region of India. Circulation. 2009;119(14):1950–5. doi: 10.1161/CIRCULATIONAHA.108.819201. [DOI] [PubMed] [Google Scholar]
- 23.Gaziano TA, Reddy KS, Paccaud F, et al. Cardiovascular Disease. In: Jamison DT, Breman J, Measham A, Alleyne G, Claeson M, Evans D, et al., editors. Disease Priorities in Developing Countries. 2nd. New York: Oxford University Press and World Bank; 2006. pp. 645–62. [Google Scholar]
- 24.He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet. 2009;374(9703):1765–72. doi: 10.1016/S0140-6736(09)61199-5. [DOI] [PubMed] [Google Scholar]
- 25.Mackay J, Mensah GA, Mendis S, et al. The Atlad of Heart Disease and Stroke. Geneva: WHO; 2004. [Google Scholar]


