Abstract
Objective
To identify shared risk and protective factors for purging, binge eating, and overweight in a large sample of adolescents.
Design
Prospective cohort study.
Setting
Self-report questionnaires.
Participants
Females (n = 6022) and males (n= 4518), aged 11 to 17 years in 1998, in the ongoing Growing Up Today Study (GUTS). Main exposures were putative risk and protective factors within the psychological, behavioral, and socio-environmental domains.
Main outcome measures
Using laxatives or vomiting (purging), binge eating, and overweight. Due to the low prevalence of purging, we did not examine shared risk or protective factors for this behavior among males.
Results
In 1998, 219 (3.7%) females and 30 (0.7%) males reported purging behaviors, 426 (7.1%) females and 90 (2.0%) males reporting binge eating, and 1019 (17.4%) females and 1040 (24.6%) males were overweight. Over the 3-year follow-up period (1999-2001), 331 (7.8%) females initiated purging behaviors, 503 (11.8 %) females and 132 (4.5%) males initiated binge eating behaviors, and 424 (10.0 %) females and 382 (13.6 %) males became overweight. Concern for weight was significantly directly associated with all three weight-related problems among both males and females. Among females, dieting, parental weight-related teasing, and family meal frequency had a shared effect on the weight-related problems examined.
Conclusions
Factors within the psychological, behavioral, and socio-environmental domains may have a shared effect on purging, binge eating, and overweight. Further research is needed to determine if an intervention designed to address these shared risk and protective factors is effective in simultaneously reducing these weight-related problems.
INTRODUCTION
Weight-related problems, including purging, binge eating, and overweight/obesity (hereafter overweight), are prevalent among adolescents1-3 and have adverse consequences for health.4-8 Research suggesting that weight-related problems may co-occur in an individual and that individuals may transition from one problem to another has prompted researchers in the fields of eating disorders and obesity prevention to propose an integrated approach that addresses the spectrum of weight-related problems within a single intervention.9-13 However, limited knowledge about shared risk factors for these weight-related problems is a roadblock to developing interventions using this integrated approach.
Few studies have examined shared risk factors for weight-related problems. A study of over 1000 adult twins found that parental comments about weight, assessed retrospectively, was a shared risk factor for binge eating and purging.14 Possible differential recall of comments from parents is an important inferential limitation of this study. Additionally, overweight wasn’t examined. Previous analyses with GUTS have examined risk factors for binge eating and purging, but these analyses did not examine shared factors for purging, binge eating, and overweight.15
Neumark-Sztainer et al.,16 examined shared risk factors for overweight, binge eating, and weight control behaviors, including purging, among 2500 adolescents and found that, among females, weight concern, weight-related teasing, and dieting predicted all three outcomes. Among males, weight concern and weight control behaviors were associated with all three outcomes. Neumark-Sztainer et al.16 examined the association between each risk factor and each weight-related problem in separate models. Thus, the relative contribution of these factors in relation to the others explored is unknown. Examining the relative contribution would help identify the most potent factors on which to intervene. Additionally, Neumark-Sztainer et al.’s analyses didn’t account for the correlation between these outcomes,16 possibly causing the standard error estimates of the effects to be too small which can result in p-values that overstate the significance of observed associations. Our study addresses limitations of previous research by modeling these weight-related outcomes jointly allowing for appropriate estimation of p-values and for assessing whether risk factors are associated differentially with purging, binge eating, and overweight.
We aimed to identify shared risk factors for overweight and disordered eating behaviors that could serve as targets for integrated prevention interventions. To achieve this aim, we examined cross-sectional and prospective associations between a range of psychological, behavioral, and socio-environmental factors and purging, binge eating, and overweight among a large sample of adolescents. We hypothesized that factors within the psychological, socio-environmental, and behavioral domains will jointly predict purging, binge eating, and overweight.
METHODS
Theoretical Model
The putative risk factors of weight-related outcomes examined in this study are derived theoretically based on the Social Cognitive Theory (SCT; Figure 1).17, 18 Many have been examined previously in etiologic studies of overweight or disordered eating.16, 19
Figure 1.
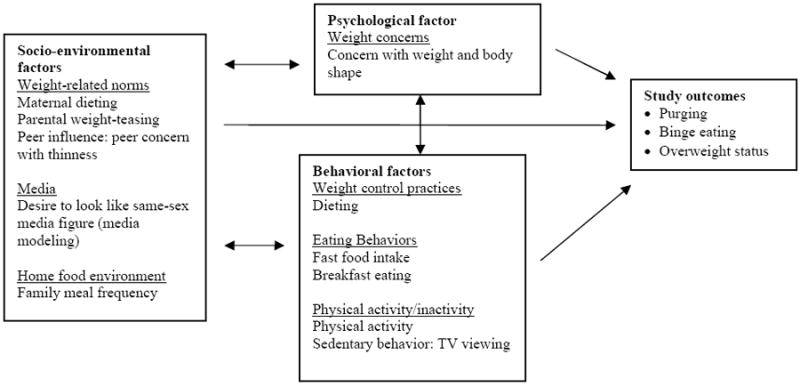
Putative socio-environmental, behavioral, and psychological risk and protective factors for purging, binge eating, and overweight status among adolescents
Study Population
GUTS is a prospective cohort study of adolescents residing throughout the US. Participants are offspring of participants in the Nurses’ Health Study II (NHS II). Participants in NHS II provided consent to invite their child to participate in GUTS. In 1996, we mailed GUTS participants an explanatory letter and a questionnaire. Returning the questionnaire constituted assent. The Human Subjects Committee at Brigham and Women’s Hospital approved this study.
Details of initial recruitment are available elsewhere.20 The baseline 1996 sample included 8843 females and 7696 males, age 9-14 years. Participants were mailed follow-up questionnaires annually from 1997-2001 and biannually since 2003. For the current study, we explored cross-sectional associations among risk factors and purging, binge eating, and overweight in 1998 when participants were aged 11-17 years. We examined these associations in 1998 because all predictor variables of interest were assessed that year and because most of the participants would have entered puberty by that time. Puberty has been shown to be associated with the development of weight-related problems.21 In our prospective analyses, we explored the association between factors assessed in 1998 and cumulative incidence of overweight, binge eating, and purging behaviors in 1999, 2000 and 2001. We selected these 3 years, which are the most proximal to when the predictor variables were measured, to help reduce the noise from other factors that may influence these outcomes. In our cross-sectional (1998) analyses we excluded 107 females and 73 males with medical conditions possibly interfering with growth, 1128 females and 1417 males missing data on all 3 outcome variables and 1586 females and 1688 males missing any of the 1998 predictor variables of interest. Our final sample for our cross-sectional analyses was 6022 females and 4518 males. In order to identify development of weight-related problems subsequent to the predictors of interest, only participants who were not overweight and were not engaging in any of the relevant disordered eating behaviors in 1998 were eligible for the prospective analysis. Thus, we excluded 1597 females and 1389 males who reported purging, binge eating, or who were overweight in 1998. We also excluded 163 females and 219 males missing data on all 3 outcome variables across the follow-up years. Our final sample for prospective analyses was 4262 females and 2910 males.
Measures
Purging
We assessed purging with validated questions:22, 23, 24 “During the past year, how often did you make yourself throw up to keep from gaining weight?” and “How often did you take laxatives to keep from gaining weight?” Response options ranged from “never” to “daily.” We defined purging as reporting vomiting or laxative use in the past year.
Binge eating
We assessed binge eating with validated questions.22, 23 Participants first reported the frequency during the past year of eating “so much food in a short period of time that you would be embarrassed if others saw you (binge-eating).” Response options ranged from “never” to “more than once a week.” Respondents reporting any episodes of overeating were directed to a follow-up question asking whether “you felt out of control during these episodes, like you could not stop even if you wanted to.” We defined binge eating as having at least one episode of overeating in the past year and feeling out of control during the episode.
Overweight
Adolescents self-reported their height and weight. Previous studies report high validity for self-reported heights and weights in adolescents.25,26, 27 We classified children as overweight or obese based on the International Obesity Task Force cut-offs,28 which are age- and sex-specific BMI values for ages <18 years that correspond with a BMI of 25 kg/m2 at 18 years. Thus, the IOTF cut off points provide comparability in assessing overweight in adolescents and adults.
Psychological Factor
Weight concern
We assessed weight concern using items from the McKnight Risk Factor Survey.29 Males are more likely than females to want to increase muscle tone, rather than be thin,30 thus, to make the questions appropriate for males, we replaced the questions on thinness with questions about the importance of not being fat in the surveys sent to male participants.
Behavioral Factors
Dieting
We assessed dieting with the question: “During the past year, how often did you diet to lose weight or to keep from gaining weight?” Response options ranged from “never” to “always on a diet.” For these analyses, participants were considered dieters if they reported any dieting.
Fast food intake
We assessed fast food intake with the question “How often do you eat fried foods away from home (like french fries)?” Response items range from “never/less than once per week” to “daily.” This item is moderately correlated with a question asking about frequency of eating at a fast food restaurant.31
Breakfast
We assessed frequency of breakfast with the question “How many times each week (including weekdays and weekends) do you eat breakfast?” Response options ranged from “never or almost never” to “5 or more times per week”
Physical activity
We assessed mean hours of physical activity per week using the 18-item Youth/Adolescent Activity Questionnaire, which is based on the validated assessment tool developed for the NHS II questionnaire.32
TV viewing
We assessed TV viewing with the question: “How many hours per week do you spend watching TV?” Response options ranged from “never” to “31+ hours per week.” Separate questions were asked for weekends and weekdays and the values were summed and averaged to create the hours per day variable.
Socio-environmental Factors
Maternal dieting
We assessed adolescent perception of maternal dieting with the question “In the past year, how often has your mother tried to lose weight?” Response options ranged from “never” to “always.” For these analyses, mothers were considered dieters if their child reported any maternal dieting.33
Parental weight-teasing
We assessed parental weight-teasing with the question “In the past year, how often has your mother made a comment about your weight or eating that made you feel bad?” (similar question for father). Response options ranged from “never” to “always.”
Peer concern with thinness
We assessed peer concern with the following questions: 1) “How often have your friends talked about wanting to lose weight?” 2) “How important has it been to your friends that they not be fat?” 3) “How important has it been to your friends that you not be fat?” We used the mean score of these questions to create the peer influence variable.
Desire to look like same-sex media figure
We assessed desire to look like media figures with the question: “In the past year, how often have your tried to look like the girls or women you see on television, in movies, or in magazines?” (similar question for males). Response options ranged from “not at all” to “totally.”
Family meal frequency
We assessed family dinner with the question: “How often do you sit down with other members of your family to eat dinner or supper?” Response options ranged from “never” to “every day.”
Other covariates
We calculated child’s age from his or her birth date and the date each questionnaire was returned.
Statistical Analyses
We used generalized estimating equations34, 35 to jointly model the effects of the predictors on purging, binge eating, and overweight. These models assume that there is some correlation among the outcomes and adjusts standard errors to account for this correlation. We first assessed whether different effects for each predictor were necessary. To do this, we included each predictor as a main effect plus interaction terms between outcome type (i.e., purging, binge eating, overweight) and each predictor. Specifically, we included a row for each outcome for each participant. An indicator variable for outcome (purging, binge eating, overweight) is included in this row, as well as an interaction term between the indicator variable and each predictor. The test to examine whether different odds ratios are required for each outcome is a 2 df test of whether that interaction is significant. If the interaction terms were statistically significant (p < .05) then we retained them in the model and show the distinct odds ratios for each outcome associated with the predictor. If the interaction terms were not significant, we removed them from the model and we present the homogenous main effect of the predictor on the outcomes as a single odds ratio, which applies to all of the outcomes. All analyses were stratified by gender and conducted using SAS version 9.1.36
We conducted sensitivity analyses for the cross-sectional and prospective analyses to examine how our decisions regarding inclusion and exclusion of participants may have influenced our results. We ran our models two different ways; 1) excluding any participants who had missing data on any outcome variable of interest; and 2) including all participants in the models regardless of how many outcomes of interest were missing. There were no substantive differences in results for the model options. We chose to use results from the second model, which kept all available data by including all participants in the models regardless of how many outcome variables of interest were missing.
RESULTS
Participant Characteristics
In 1998, 219 (3.7%) females and 30 (0.7%) males reported purging and 426 (7.1%) females and 90 (2.0%) males reported binge eating (Table 1). Additionally, 1019 (17.4%) females and 1040 (24.6%) males were overweight. Given the small number of males reporting purging, we did not include purging in our examination of shared factors for males. Over the 3-year follow-up period, 331 (7.8%) females initiated purging, while 503 (11.8 %) females and 132 (4.5%) males initiated binge eating. In addition, 424 (10.0 %) females and 382 (13.6 %) males became overweight.
Table 1.
1998 outcomes, predictors and covariates of Growing Up Today Study participants (4518 males and 6022 females)
| Females | Males | |||
|---|---|---|---|---|
| Outcomes | N | % | N | % |
| Purging | 219 | 3.7 | 30 | 0.7 |
| Binge eating | 426 | 7.1 | 90 | 2.0 |
| Obese/Overweight | 1019 | 17.4 | 1040 | 24.6 |
| Predictors | Mean | SD | Mean | SD |
| Psychological | ||||
| Weight concern | 2.4 | 1.1 | 1.6 | 0.8 |
| Behavioral | ||||
| Dieting (N, % yes) | 2316 | 38.5 | 719 | 15.9 |
| Fast food (svg/wk) | 1.2 | 1.3 | 1.5 | 1.5 |
| Breakfast (times/wk) | 4.8 | 2.0 | 5.2 | 1.7 |
| Physical activity (hr/day) | 1.8 | 1.1 | 2.1 | 1.2 |
| TV viewing (hr/day) | 1.4 | 1.1 | 1.8 | 1.3 |
| Socio-environmental | ||||
| Maternal dieting (N, % yes) | 4104 | 68.2 | 2746 | 60.8 |
| Weight-teasing parents | 1.3 | 0.6 | 1.2 | 0.6 |
| Importance of thinness to peers | 1.9 | 0.7 | 1.3 | 0.5 |
| Look like media figure | 1.7 | 1.0 | 1.4 | 0.7 |
| Family meal frequency | 3.1 | 0.8 | 3.2 | 0.8 |
| Other variables | ||||
| Race/ethnicity (N, %) | ||||
| Non-white | 375 | 6.3 | 306 | 6.8 |
| White | 5625 | 93.8 | 4201 | 93.2 |
| Age (in years) | 13.9 | 1.6 | 13.8 | 1.5 |
Cross-sectional Results
Tables 2 and 3 present the cross-sectional multivariable adjusted odds ratios (ORs) of purging (females only), binge eating, and overweight associated with psychological, behavioral and socio-environmental factors among females and males, respectively. If we found that the effect estimates for a predictor were similar for all three outcomes, i.e. the interaction term of outcome type and the predictor variable of interest was not significant, we present the single homogeneous main effect of the predictor variable on the outcomes. If we found that the effect estimates for a predictor were significantly different for the three outcomes, i.e. the interaction term was significant, we present the individual effect of the predictor variable and each outcome.
Table 2.
1998 Cross-sectional associations between psychological, behavioral, and socio-environmental factors and weight-related outcomes: Femalesa,b,c
| Homogeneous Main Effect | Different Effect by Outcome | |||||||
|---|---|---|---|---|---|---|---|---|
| Purging | Binge Eating | Obese/Overweight | ||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Psychological | ||||||||
| Weight concern | 2.45 | 2.26, 2.67 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Behavioral | ||||||||
| Dieting | ------------ | ------------ | 3.37 | 2.03, 5.57 | 1.41 | 1.08, 1.85 | 1.58 | 1.31, 1.91 |
| Fast food | 0.99 | 0.95, 1.04 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Breakfast | 0.99 | 0.96, 1.01 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Physical activity | ------------ | ------------ | 1.27 | 1.13, 1.43 | 1.00 | 0.92, 1.10 | 0.81 | 0.75, 0.88 |
| TV viewing | ------------ | ------------ | 0.96 | 0.84, 1.10 | 1.00 | 0.92, 1.09 | 1.16 | 1.09, 1.23 |
| Socio-environmental | ||||||||
| Maternal dieting | 0.97 | 0.85, 1.11 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Parental weight-teasing | ------------ | ------------ | 0.96 | 0.81, 1.14 | 1.23 | 1.08, 1.41 | 2.05 | 1.82, 2.31 |
| Importance of thinness peers | ------------ | ------------ | 1.28 | 1.03, 1.58 | 1.03 | 0.86, 1.23 | 0.74 | 0.64, 0.84 |
| Look like media figure | ------------ | ------------ | 1.26 | 1.12, 1.42 | 1.10 | 0.99, 1.21 | 0.66 | 0.60, 0.72 |
| Family meal frequency | ------------ | ------------ | 0.76 | 0.63, 0.91 | 0.87 | 0.77, 1.00 | 1.01 | 0.92, 1.11 |
Multivariable model includes all psychological, behavioral, and socio-environmental factors
Multivariable model adjusted for age when questionnaire was returned
Bold represents statistically significant results (p ≤ 0.05)
Table 3.
1998 Cross-sectional associations between psychological, behavioral, and socio-environmental factors and weight-related outcomes: Males a,b,c
| Homogeneous Main Effect | Different Effect by Outcome | |||||
|---|---|---|---|---|---|---|
| Binge Eating | Obese/Overweight | |||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Psychological | ||||||
| Weight concern | ------------ | ------------ | 2.10 | 1.64, 2.70 | 3.52 | 3.04, 4.07 |
| Behavioral | ||||||
| Dieting | ------------ | ------------ | 1.09 | 0.60, 1.98 | 2.61 | 2.07, 3.30 |
| Fast food | 1.01 | 0.96, 1.06 | ------------ | ------------ | ------------ | ------------ |
| Breakfast | 0.97 | 0.93, 1.01 | ------------ | ------------ | ------------ | ------------ |
| Physical activity | 0.96 | 0.90, 1.02 | ------------ | ------------ | ------------ | ------------ |
| TV viewing | 1.12 | 1.06, 1.18 | ------------ | ------------ | ------------ | ------------ |
| Socio-environmental | ||||||
| Maternal dieting | 1.08 | 0.92, 1.27 | ------------ | ------------ | ------------ | ------------ |
| Parental weight-teasing | 1.31 | 1.15, 1.50 | ------------ | ------------ | ------------ | ------------ |
| Importance of thinness peers | ------------ | ------------ | 1.26 | 0.93, 1.72 | 0.69 | 0.55, 0.85 |
| Look like media figure | ------------ | ------------ | 1.32 | 1.06, 1.63 | 0.67 | 0.57, 0.78 |
| Family meal frequency | 1.00 | 0.90, 1.11 | ------------ | ------------ | ------------ | ------------ |
Multivariable model includes all psychological, behavioral, and socio-environmental factors
Multivariable model adjusted for age when questionnaire was returned
Bold represents statistically significant results (p ≤ 0.05)
Females
Among females, weight concern was directly associated with all three weight-related problems and the direction and magnitude of the effect was similar for all three outcomes (homogeneous effect OR = 2.45, 95% CI 2.26, 2.67). Of the five behavioral factors examined, only dieting was found to be significantly associated with all three weight-related problems. The magnitude of the effect differed across the three outcomes, with dieting being most strongly associated with purging. Physical activity was significantly associated with purging and overweight, however, the direction of the effect differed; physical activity was directly associated with purging and inversely associated with overweight. Fast food intake, breakfast, and television viewing did not have a shared effect on the weight-related problems examined.
None of the socio-environmental factors were significantly associated with all three weight-related problems. However, a number of socio-environmental factors were associated with two of the three weight-related problems, suggesting a shared effect. Parental weight-related teasing was directly associated with binge eating and overweight. Family meal frequency was inversely associated with purging and binge eating. Desire to look like same-sex media figures and importance of thinness to peers were also significantly associated with two of the weight-related problems; however, the direction of these associations differed across outcomes. Desire to look like same-sex media figures was directly associated with purging and inversely associated with overweight. Importance of thinness to peers was directly associated with binge eating and inversely associated with overweight. Maternal dieting did not have a shared effect on the weight-related problems examined.
Males
Among males, concern with weight was directly associated with binge eating and overweight; the magnitude of effect differed across the two outcomes, with weight concern being more strongly associated with overweight. Of the five behavioral factors examined, only TV viewing was significantly associated with both binge eating and overweight. TV viewing was directly associated with both outcomes (homogenous effect OR= 1.12, 95% CI 1.06, 1.18). Dieting, fast food intake, breakfast, and physical activity did not have a shared effect on binge eating and overweight among males.
Parental weight-related teasing was directly associated with binge eating and overweight (homogenous effect OR = 1.31, 05% CI 1.15, 1.50). Importance of thinness to peers was significantly associated with binge eating and overweight: however, the direction of these associations differed across outcomes. Importance of thinness to peers was directly associated with binge eating and inversely associated with overweight. Desire to look like same-sex media figures was also directly associated with binge eating and inversely associated with overweight. Maternal dieting and family meal frequency did not have a shared effect on binge eating and overweight.
Prospective Results
Tables 4 and 5 present the prospective multivariable adjusted odds ratios (ORs) of incident cases of purging (females only), binge eating, and overweight status associated with risk factors among females and males, respectively.
Table 4.
Prospective associations between psychological, behavioral, and socio-environmental factors assessed in 1998 and incident weight-related outcomes in 1999-2001: Femalesa,b,c
| Homogeneous Main Effect | Different Effect by Outcome | |||||||
|---|---|---|---|---|---|---|---|---|
| Purging | Binge Eating | Obese/Overweight | ||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Psychological | ||||||||
| Weight concern | 1.56 | 1.42, 1.71 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Behavioral | ||||||||
| Dieting | 1.48 | 1.25, 1.74 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Fast food | 1.02 | 0.97, 1.07 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Breakfast | ------------ | ------------ | 0.97 | 0.92, 1.03 | 1.03 | 0.98, 1.09 | 0.92 | 0.88, 0.97 |
| Physical activity | 1.05 | 1.00, 1.11 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| TV viewing | 1.01 | 0.95, 1.08 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Socio-environmental | ||||||||
| Maternal dieting | 0.89 | 0.77, 1.02 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
| Parental weight-teasing | ------------ | ------------ | 1.10 | 0.89, 1.37 | 1.29 | 1.08, 1.55 | 1.64 | 1.36, 1.96 |
| Importance of thinness peers | ------------ | ------------ | 1.17 | 0.96, 1.44 | 1.08 | 0.92, 1.27 | 0.74 | 0.61, 0.89 |
| Look like media figure | ------------ | ------------ | 1.14 | 1.01, 1.29 | 1.04 | 0.93, 1.16 | 0.78 | 0.69, 0.88 |
| Family meal frequency | 0.90 | 0.83, 0.98 | ------------ | ------------ | ------------ | ------------ | ------------ | ------------ |
Multivariable model includes all psychological, behavioral, and socio-environmental factors
Multivariable model adjusted for age when questionnaire was returned
Bold represents statistically significant results (p ≤ 0.05)
Table 5.
Prospective associations between psychological, behavioral, and socio-environmental factors assessed in 1998 and incident weight-related outcomes in 1999-2001: Males a,b,c
| Homogeneous Main Effect | Different Effect by Outcome | |||||
|---|---|---|---|---|---|---|
| Binge Eating | Obese/Overweight | |||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Psychological | ||||||
| Weight concern | ------------ | ------------ | 1.65 | 1.27, 2.13 | 2.41 | 2.00, 2.91 |
| Behavioral | ||||||
| Dieting | 0.94 | 0.65, 1.34 | ------------ | ------------ | ------------ | ------------ |
| Fast food | ------------ | ------------ | 1.12 | 1.00, 1.24 | 0.93 | 0.87, 1.00 |
| Breakfast | ------------ | ------------ | 1.06 | 0.94, 1.19 | 0.94 | 0.87, 1.00 |
| Physical activity | 1.06 | 0.99 1.15 | ------------ | ------------ | ------------ | ------------ |
| TV viewing | 1.01 | 0.94, 1.09 | ------------ | ------------ | ------------ | ------------ |
| Socio-environmental | ||||||
| Maternal dieting | 1.14 | 0.94, 1.40 | ------------ | ------------ | ------------ | ------------ |
| Parental weight-teasing | 1.07 | 0.88, 1.29 | ------------ | ------------ | ------------ | ------------ |
| Importance thinness | 0.92 | 0.72, 1.17 | ||||
| peers | ------------ | ------------ | ------------ | ------------ | ||
| Look like media figure | 0.95 | 0.82, 1.11 | ------------ | ------------ | ------------ | ------------ |
| Family meal frequency | 0.89 | 0.78, 1.01 | ------------ | ------------ | ------------ | ------------ |
Multivariable model includes all psychological, behavioral, and socio-environmental factors
Multivariable model adjusted for age when questionnaire was returned
Bold represents statistically significant results (p ≤0.05)
Females
As in our cross-sectional analyses, concern with weight was directly associated with all three weight-related problems in our prospective analyses and the direction and magnitude of the effect was similar for all three outcomes (homogeneous effect OR = 1.56, 95% CI 1.42, 1.71). Dieting was also directly associated with the three outcomes (homogeneous effect OR = 1.48, 95% CI 1.25, 1.74). Unlike our cross-sectional results which found that physical activity was directly associated with purging and inversely associated with overweight, our prospective analyses showed that physical activity did not have a shared effect on the weight-related outcomes. Prospectively, fast food intake, breakfast, and television viewing did not have a shared effect on the weight-related problems, similar to our cross-sectional findings.
As we found in our cross-sectional analyses, parental weight-related teasing was directly associated with binge eating and overweight, but not purging prospectively. Also similar to our cross-sectional analyses, desire to look like same-sex media figures was associated with more than one weight-related problem prospectively, but the direction of this effect differed across outcomes; it was directly associated with purging and inversely associated with overweight. Prospectively, family meal frequency was inversely associated with all three weight-related outcomes (homogenous effect OR = 0.90, 95% CI 0.83, 0.98). Maternal dieting and importance of thinness to peers did not have a shared effect on the weight-related problems.
Males
As we found in our cross-sectional analyses, concern with weight was directly associated with both binge eating and overweight prospectively; the effect’s magnitude differed across the two outcomes, with weight concern being more strongly associated with overweight. Unlike our cross-sectional results, which found that television was directly associated with both binge eating and overweight, prospectively TV viewing did not have a shared effect on obesity and binge eating. Dieting, fast food, breakfast, and physical activity also did not have a shared effect on binge eating and overweight among males. Prospectively, none of the five socio-environmental factors had a shared effect on binge eating and overweight among males.
COMMENT
Using analytic methods that account for the correlation between the three weight-related outcomes, we examined shared risk factors of purging, binge eating, and overweight in a large cohort of adolescents. Identification of shared risk factors for these weight-related problems can inform development of interventions to promote maintenance of healthful weight and decrease risk of disordered eating.
We found that weight concern was the most robust shared risk factor for purging (females only), binge eating and overweight among both male and female adolescents. Among females, dieting was a shared risk factor for purging, binge eating, and overweight. Two socio-environmental factors, weight-related teasing by parents and family meal frequency, had a shared effect on weight-related problems. Weight-related teasing was a risk factor for binge eating and overweight and family meal frequency was a protective factor for all three weight-related outcomes. These findings are consistent with previous research showing that dieting37, 38 and weight-related teasing39, 40 are associated with increased risk of disordered eating and obesity and that family meals41-44 may reduce adolescents’ risk of engaging in disordered eating behaviors.
Our finding that female adolescents who reported wanting to look like same-sex media figures were less likely to become overweight, but were more likely to initiate purging behaviors underscores the importance of examining the influence of risk factors on a range of weight-related problems. By looking only at the influence of wanting to look like media figures on obesity risk, researchers and public health practitioners may inadvertently promote an obesity prevention strategy, i.e., emulating media figures, that could increase disordered eating risk among adolescents.45
Among males, none of the behavioral or socio-environmental factors were consistently associated with binge eating and overweight. Our results are consistent with the finding by Neumark-Sztainer et al.16 that, compared to females, substantially fewer risk factors had a shared effect on weight-related problems among males. It is possible that our relatively null findings among males may be due to the fact that our measures of the behavioral or socio-environmental factors do not adequately capture the experiences of males. For example, we did not assess performance (vs. appearance) related pressures to achieve an ideal body weight, which may have a strong influence on weight-related problems among males.46 Further research is needed to elucidate shared factors of weight-related problems among males.
This study’s strengths include prospective data collection, the breadth of theoretically-driven risk factors examined, and the use of analytic methods that account for the correlation among the weight-related outcomes examined. This study also had limitations. Although study participants reside throughout the US, our cohort is not a representative sample of US adolescents. Participants are children of registered nurses and the cohort is >90% white, which may reduce the generalizability of our findings. However, our findings are similar to those found by Neumark-Sztainer,16 who examined shared risk factors in a racially and socio-economically diverse population. Another limitation was the necessity of collecting data from youth by self-report questionnaires. All three self-report outcome measures have been previously validated22, 23, 47 and the resulting measurement error should be random.
CONCLUSION
We found that weight concern was the most robust shared risk factor for overweight and disordered eating among adolescents. Among females, we found that dieting, weight-related teasing, and family meal frequency had a shared effect on these weight-related problems. Interventions that aim to prevent multiple weight-related problems should test strategies that address these factors to determine if such efforts can reduce the high prevalence of overweight and disordered eating behaviors among youth.
Acknowledgments
This study was supported by grants from the National Institutes of Health (DK46834, DK59570, DK072117), the Kellogg Company, and the Canadian Institutes of Health Research (200510MFE-154556-10955). Dr. Haines had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Curr Opin Psychiatry. 2006;19(4):389–394. doi: 10.1097/01.yco.0000228759.95237.78. [DOI] [PubMed] [Google Scholar]
- 3.Keel PK, Heatherton TF, Dorer DJ, Joiner TE, Zalta AK. Point prevalence of bulimia nervosa in 1982, 1992, and 2002. Psychol Med. 2006;36(1):119–127. doi: 10.1017/S0033291705006148. [DOI] [PubMed] [Google Scholar]
- 4.Johnson JG, Cohen P, Kasen S, Brook JS. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. Am J Psychiatry. 2002;159(3):394–400. doi: 10.1176/appi.ajp.159.3.394. [DOI] [PubMed] [Google Scholar]
- 5.Strauss CC, Smith K, Frame C, Forehand R. Personal and interpersonal characteristics associated with childhood obesity. Journal of Pediatric Psychology. 1984;10:337–343. doi: 10.1093/jpepsy/10.3.337. [DOI] [PubMed] [Google Scholar]
- 6.Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: An epidemiologic review and a public health perspective. Journal of Pediatrics. 2000;136(5):664–672. doi: 10.1067/mpd.2000.105141. [DOI] [PubMed] [Google Scholar]
- 7.Herzog DB, Keller MB, Sacks NR, Yeh CJ, Lavori PW. Psychiatric comorbidity in treatment-seeking anorexics and bulimics. J Am Acad Child Adolesc Psychiatry. 1992;31(5):810–818. doi: 10.1097/00004583-199209000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Zipfel S, Lowe B, Reas DL, Deter HC, Herzog W. Long-term prognosis in anorexia nervosa: lessons from a 21-year follow-up study. Lancet. 2000;355(9205):721–722. doi: 10.1016/S0140-6736(99)05363-5. [DOI] [PubMed] [Google Scholar]
- 9.Neumark-Sztainer D. Obesity and eating disorder prevention: An integrated approach? Adolescent Medicine: State of the Art Reviews. 2003;14:159–173. [PubMed] [Google Scholar]
- 10.Irving LM, Neumark-Sztainer D. Integrating primary prevention of eating disorders and obesity: Feasible or futile? Prev Med. 2002;34(3):299–309. doi: 10.1006/pmed.2001.0997. [DOI] [PubMed] [Google Scholar]
- 11.Smolak L, Striegel-Moore RH. Future directions in eating disorder and obesity research. In: Thompson JK, editor. Handbook of Eating Disorders and Obesity. Hoboken, New Jersey: John Wiley & Sons, Inc.; 2004. pp. 738–754. [Google Scholar]
- 12.Austin SB. Prevention research and eating disorders: Theory and new directions. Psychol Med. 2000;30(6):1249–1262. doi: 10.1017/s0033291799002573. [DOI] [PubMed] [Google Scholar]
- 13.Brownell KD, Fairburn CG. Eating disorders and obesity: A comprehensive handbook. New York: Guilford Press; 1995. [Google Scholar]
- 14.Wade TD, Treloar S, Martin NG. Shared and unique risk factors between lifetime purging and objective binge eating: a twin study. Psychol Med. 2008;38(10):1455–1464. doi: 10.1017/S0033291708002791. [DOI] [PubMed] [Google Scholar]
- 15.Field AE, Javaras KM, Aneja P, et al. Family, peer, and media predictors of becoming eating disordered. Arch Pediatr Adolesc Med. 2008;162(6):574–579. doi: 10.1001/archpedi.162.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neumark-Sztainer DR, Wall MM, Haines JI, Story MT, Sherwood NE, van den Berg PA. Shared risk and protective factors for overweight and disordered eating in adolescents. Am J Prev Med. 2007;33(5):359–369. doi: 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 18.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 19.Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res. 2006;21(6):770–782. doi: 10.1093/her/cyl094. [DOI] [PubMed] [Google Scholar]
- 20.Gillman MW, Rifas-Shiman SL, Camargo CA, Jr, et al. Risk of overweight among adolescents who were breastfed as infants. JAMA. 2001;285(19):2461–2467. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- 21.Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002;128(5):825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- 22.Field AE, Taylor CB, Celio A, Colditz GA. Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. Int J Eat Disord. 2004;35(1):86–92. doi: 10.1002/eat.10220. [DOI] [PubMed] [Google Scholar]
- 23.Brener ND, Collins JL, Kann L, Warren CW, Williams BI. Reliability of the Youth Risk Behavior Survey Questionnaire. Am J Epidemiol. 1995;141(6):575–580. doi: 10.1093/oxfordjournals.aje.a117473. [DOI] [PubMed] [Google Scholar]
- 24.Kann L, Warren CW, Harris WA, et al. Youth Risk Behavior Surveillance--United States, 1995. Morbidity and Mortality Weekly Report CDC Surveillance Summaries. 1996;45(4):1–84. [PubMed] [Google Scholar]
- 25.Shannon B, Smiciklas-Wright H, Wang MQ. Inaccuracies in self-reported weights and heights of a sample of sixth-grade children. J Am Diet Assoc. 1991;91(6):675–678. [PubMed] [Google Scholar]
- 26.Strauss RS. Comparison of measured and self-reported weight and height in a cross-sectional sample of young adolescents. Int J Obes Relat Metab Disord. 1999;23(8):904–908. doi: 10.1038/sj.ijo.0800971. [DOI] [PubMed] [Google Scholar]
- 27.Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106:52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- 28.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shisslak CM, Renger R, Sharpe T, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. Int J Eat Disord. 1999;25(2):195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 30.McCabe MP, Ricciardelli LA, Finemore J. The role of puberty, media and popularity with peers on strategies to increase weight, decrease weight and increase muscle tone among adolescent boys and girls. J Psychosom Res. 2002;52(3):145–153. doi: 10.1016/s0022-3999(01)00272-0. [DOI] [PubMed] [Google Scholar]
- 31.Taveras EM, Berkey CS, Rifas-Shiman SL, et al. Association of consumption of fried food away from home with body mass index and diet quality in older children and adolescents. Pediatrics. 2005;116(4):e518–524. doi: 10.1542/peds.2004-2732. [DOI] [PubMed] [Google Scholar]
- 32.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23(5):991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 33.Field AE, Austin SB, Striegel-Moore R, et al. Weight concerns and weight control behaviors of adolescents and their mothers. Arch Pediatr Adolesc Med. 2005;159(12):1121–1126. doi: 10.1001/archpedi.159.12.1121. [DOI] [PubMed] [Google Scholar]
- 34.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 35.Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 36.SAS. Version 9.1. Cary, NC: SAS Institute, Inc.; 2002. computer program. [Google Scholar]
- 37.Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? J Am Diet Assoc. 2006;106(4):559–568. doi: 10.1016/j.jada.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 38.Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. Journal of Consulting and Clinical Psychology. 1999;67(6):967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- 39.Taylor CB, Bryson S, Celio Doyle AA, et al. The adverse effect of negative comments about weight and shape from family and siblings on women at high risk for eating disorders. Pediatrics. 2006;118(2):731–738. doi: 10.1542/peds.2005-1806. [DOI] [PubMed] [Google Scholar]
- 40.Keery H, Boutelle K, van den Berg P, Thompson JK. The impact of appearance-related teasing by family members. J Adolesc Health. 2005;37(2):120–127. doi: 10.1016/j.jadohealth.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 41.Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents: longitudinal findings from project EAT. Arch Pediatr Adolesc Med. 2008;162(1):17–22. doi: 10.1001/archpediatrics.2007.9. [DOI] [PubMed] [Google Scholar]
- 42.Ackard D, Neumark-Sztainer D. Family mealtime while growing up: Associations with symptoms of bulimia nervosa. Eating Disorders: The Journal of Treatment and Prevention. 2001;9:239–249. doi: 10.1080/10640260127551. [DOI] [PubMed] [Google Scholar]
- 43.Sen B. Frequency of family dinner and adolescent body weight status: evidence from the national longitudinal survey of youth, 1997. Obesity (Silver Spring) 2006;14(12):2266–2276. doi: 10.1038/oby.2006.266. [DOI] [PubMed] [Google Scholar]
- 44.Veugelers PJ, Fitzgerald AL. Prevalence of and risk factors for childhood overweight and obesity. CMAJ. 2005;173(6):607–613. doi: 10.1503/cmaj.050445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Taveras EM, Rifas-Shiman SL, Field AE, Frazier AL, Colditz GA, Gillman MW. The influence of wanting to look like media figures on adolescent physical activity. J Adolesc Health. 2004;35(1):41–50. doi: 10.1016/j.jadohealth.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 46.Cafri G, van den Berg P, Thompson JK. Pursuit of muscularity in adolescent boys: relations among biopsychosocial variables and clinical outcomes. J Clin Child Adolesc Psychol. 2006;35(2):283–291. doi: 10.1207/s15374424jccp3502_12. [DOI] [PubMed] [Google Scholar]
- 47.Field AE, Aneja P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity (Silver Spring) 2007;15(9):2357–2364. doi: 10.1038/oby.2007.279. [DOI] [PubMed] [Google Scholar]


