Abstract
OBJECTIVE:
The main aim of the study was to analyze the outcomes of clavicle fractures in adults treated non-surgically and to evaluate the clinical effects of displacement, fracture patterns, fracture location, fracture comminution, shortening and fracture union on shoulder function.
METHODS:
Seventy clavicle fractures were non-surgically treated in the Orthopedics Department at the Tuanku Ja'afar General Hospital, a tertiary care hospital in Seremban, Malaysia, an average of six months after injury. The clavicle fractures were treated conservatively with an arm sling and a figure-eight splint for three weeks. No attempt was made to reduce displaced fractures, and the patients were allowed immediate free-shoulder mobilization, as tolerated. They were prospectively evaluated clinically and radiographically. Shoulder function was evaluated using the Constant scoring technique.
RESULTS:
There were statistically significant functional outcome impairments in non-surgically treated clavicle fractures that correlated with the fracture type (comminution), the fracture displacement (21 mm or more), shortening (15 mm or more) and the fracture union (malunion).
CONCLUSION:
This article reveals the need for surgical intervention to treat clavicle fractures and improve shoulder functional outcomes.
Keywords: clavicle, fracture, conser vative surgical, functional
INTRODUCTION
Clavicle fractures are commonly found in all age groups.1 These fractures account for 5 to 10% of all fractures1,2 and represent 45 to 50% of all shoulder girdle injuries.1,3 Clavicle fractures are common, and reports have noted that their annual incidence varies from 29 to 64 per 100,000 individuals, and they account for. Most fractures occur in the middle third of the clavicle; this location accounted for 76 to 80% of clavicle fractures in a large study.1,3-6 Fractures in the most lateral portion of the clavicle principally occur after falls onto the tip of the shoulder, with an injury mechanism similar to that of acromioclavicular joint dislocations.7
In our clinical practice, we encounter clavicle fracture patients who often complain that their shoulders feel inadequate after a given treatment period. Their shoulder strength and motion are reduced compared to their pre-injury condition and to their contralateral shoulder. In certain situations, the patients were unable to perform the same activities they performed before their injuries. All these problems result from nonunion, malunion and shortening of the clavicle. As far as the literature is concerned, there are no quantitative data indicating that clavicle fractures should be treated surgically.
The Malaysian Orthopaedic Association meeting (held in June 2008 in Kuala Lumpur) concluded that there is a need to operate on certain clavicle fractures. Neer (1960) reported 3 nonunions out of 2,235 fractures that were treated with the closed method,8 whereas Rowe and Corr (1968) reported 4 nonunions out of 566 that were treated with the closed method.9 The main aim of this study was to determine the functional outcomes of clavicle fractures in non-surgically treated patients and to evaluate the clinical impacts of displacement, fracture patterns, fracture location, fracture comminution, shortening and fracture union on shoulder function in a tertiary hospital in Malaysia.
METHODS
This prospective cohort study was performed between May 2008 and April 2010 in the Orthopedics Department at the Tuanku Ja'afar General Hospital, a tertiary hospital in Seremban, Malaysia. Patients who presented with clavicle fractures and had completed at least 6 months of follow-up were included. All clavicle fractures were treated non-surgically. The shoulder functional outcomes of the clavicle fractures were measured using the Constant scoring technique.
The Constant scoring technique refers to a scoring system consisting of four variables that assess shoulder function, based on the guidelines of the European Society for Shoulder and Elbow Surgery (ESSES).10,11
Devices for measuring strength:
Strength was measured using a standard Salter pocket balance (Salter Co., UK) with a maximum weight of 25 kg.
Range of motion was measured using a goniometer (JAMAR Co., Pakistan).
The outcomes of the different end-points 6 months after the injury were explored using the chi-squared test and Pearson's χ-squared test. A p-value <0.05 was considered to be statistically significant. Selected subgroups of patients were compared after 6 months using estimated relative risks with 95% confidence intervals.
The clinical outcomes of the non-surgically treated clavicle fractures were evaluated after 6 months of follow-up using the Constant scoring technique developed by Constant and Murley. Only the researchers performed the physical examinations and recorded the data and scores to minimize any inter-observer error. These data were analyzed using SPSS (version 15.0).
RESULTS
1. Shoulder function treated non-surgically after clavicle fracture
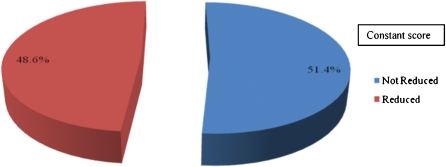
Chart 1 shows the frequency and percentage of shoulder function after clavicle fracture. The results showed that 34 patients (48.6%) had reduced shoulder function on the affected side, whereas 36 patients (51.4%) reported no reduction following clavicle fracture.
Chart 1.
Shoulder status after a non-surgical treatment of a clavicle fracture.
2. Fracture location and constant score
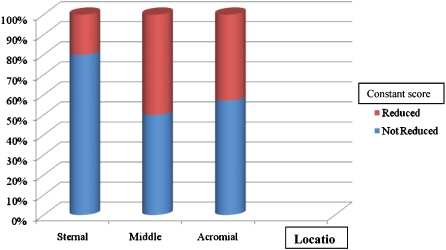
Figure 1 shows the clavicle fracture location and the Constant score (chi-squared = 1.720, df = 2, sig = .423>.05). These values indicate that there was no significant correlation between the clavicle fracture location and Constant score. In other words, the clavicle fracture location did not affect shoulder function. In addition, the low standardized residual (0.2 to 0.9) shows that the observed frequency and expected frequency were too small to allow us to reject the null hypothesis.
Figure 1.
Clavicle fracture location and Constant score.
3. Clavicle fracture type and constant score
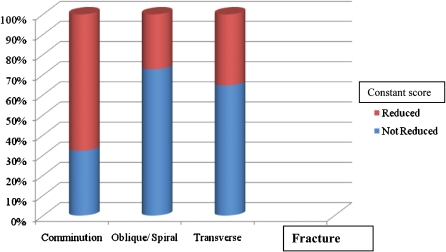
The Pearson chi-squared results in Figure 2 have a chi-square value of 9.722 (df = 2, sig = .008<.05), indicating that there was a significant correlation between the fracture type and the Constant score. The findings indicate that more patients with comminution fractures had reduced shoulder function compared to patients with other types of fractures (oblique/spiral and transverse). The counted reduced Constant score for comminution fractures was 21 (expected count = 14.6 and std. residual = 1.7). Other types yielded smaller values (see Table 3a).
Figure 2.
Clavicle fracture type and Constant score.
4. Clavicle fracture displacement and constant score
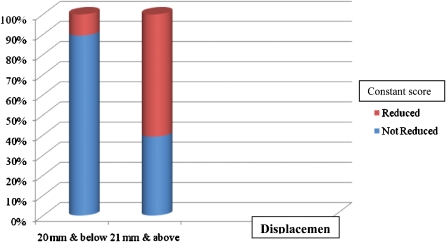
Figure 3 shows the relationship between the clavicle fracture displacement and the Constant score. The result of the chi-squared test for fractured bone displacement and Constant score revealed a significant correlation (chi-squared = 14.032, df = 1, p = .000 <.05). These findings indicate that patients whose fractured bones were displaced 21 mm or more had lower Constant scores than those with fractured bones that were displaced by less than 20 mm. The Constant score for a bone displacement of 21 mm or more was 31 (expected count = 24 and std. residual = 1.4), while bone displacements of 20 mm or less yielded lower values.
Figure 3.
Clavicle fracture displacement and Constant score.
In this study, analyses were made to determine how severely displacement affects shoulder function. The chi-squared values revealed a significant difference between displacement and shoulder function (chi-squared value = 23.386, df = 4, p = .000<.05). Although a displacement of 0.50 cm could affect shoulder function in this study, this effect was not statistically significant.
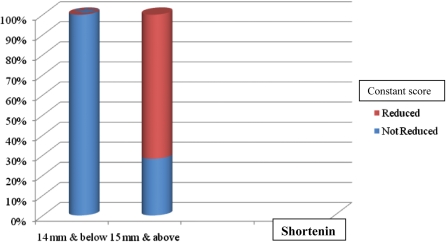
5. Clavicle fracture shortening and constant score
Figure 4 shows the relationship between clavicle fracture shortening and the Constant score. A chi-squared value of 32.57 (df = 1, p = .000 <.05) indicates a significant correlation between shortening (in the AP view) and the Constant score. Patients with shortening (in the AP view) of 15 mm or more yielded a count value (33) greater than the expected count (21.7), while patients with shortening (in the AP view) of 14 mm or more yielded a count value of 0. This means that shortening (in the AP view) of 15 mm or more had an effect on reducing the Constant score.
Figure 4.
Clavicle fracture shortening and Constant score.
A shortening of 1.20 cm (12 mm) could affect shoulder function in this study, but this effect was not statistically significant.
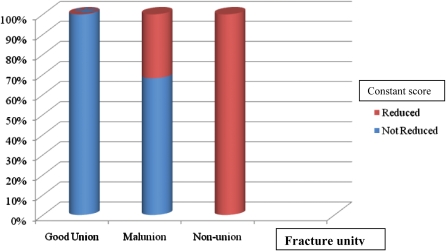
6. Clavicle fracture unity (fracture union ) and constant score
Figure 5 shows the clavicle fracture unity and the Constant score. A Pearson's chi-squared test value of 31.693 (df = 2, sig = .000 <.05) reveals a significant correlation between the fracture unity and the Constant score. This finding implies that more patients with fracture malunions (count = 30, expected count = 20.7 and std. residual = 2.0) had reduced shoulder function compared to patients with fracture nonunions (count = 3, expected count = 1.4 and std. residual = 1.3), while patients with good fracture unions had no reductions in their Constant scores (count = 0, expected count = 10.8 and std. residual = −3.3).
Figure 5.
Clavicle fracture unity and Constant score.
DISCUSSION
Clavicle fractures represent 45% of all shoulder girdle injuries.1 Although clavicle fractures usually unite uneventfully with treatment, they can be associated with difficult early and late complications. Fractures in the middle third of the clavicle represent 80% of all clavicular fractures.1,3 Traditionally, clavicle fractures are treated conservatively, and surgical treatment has been associated with an increased complication rate. Indications for primary open fixation include significant displacement, fracture comminution and skin tenting that threatens the skin's integrity and fails to respond to closed reduction.
Based on the 70 patients in this study, our results showed that 34 patients (48.6%) had reduced shoulder function on the affected side, whereas 36 patients (51.4%) did not experience reduced shoulder function. The Constant shoulder score varied from 39 to 94, with a mean of 77.19.
Our results showed no statistically significant correlation between clavicle fracture location and the Constant score. The clavicle fracture location did not appear to affect shoulder function. The current recommendation for an unstable distal clavicle fracture is surgery; however, the number of distal clavicle fractures in our sample was small (7 patients). A larger sample may have altered the results. Krüger–Franke et al. (2001) reported very good outcomes in a series of 41 patients with lateral clavicle fractures who were treated with the K-wire stabilization with cerclage and AO-plate osteosynthesis. An 8-year follow-up revealed good or very good outcomes in 97% of these subjects.12 Surgical treatment is recommended for unstable distal clavicular fractures, and several surgical methods have been proposed, including extraarticular or transarticular K-wire fixation, coracoclavicular screw fixation, tension band wiring and clavicular plate fixation.13 Khashif Khan et al. (2009) also reported that shaft fractures occur most often in young adults, while medial and lateral end fractures are more common in older age groups.14
Our findings revealed a statistically significant correlation between the fracture type and shoulder function. Our results showed that patients with comminuted clavicle fractures had reduced shoulder function compared to patients with other types of fractures (oblique/spiral and transverse). This finding is consistent with an earlier report by Wiesel et al. (2006), who used multivariate analysis to identify a lack of cortical apposition and the presence of comminution as risk factors for nonunion in diaphyseal clavicle fractures that lead to reduced shoulder function.15
Our fracture displacement results showed that a bone displacement of 20 mm or more can negatively impact shoulder function, but this effect was not statistically significant. However, a displacement of 21 mm or more was significant associated with reduced shoulder function. In another study, a fracture displacement of 20 mm or more was associated with unsatisfactory outcomes.16 This is because an initial displacement of 20 mm or more is associated with a higher risk of nonunion and a poor clinical outcome.14,17
Clavicle fracture patients with shortening (in the AP view) of 14 mm had no reduction in shoulder function, but shortening of 15 mm or more was statistically associated with affected shoulder function. This finding agrees with earlier studies by Goss and Constant et al. (1993), who reported that shortening of more than 15 mm was associated with shoulder discomfort and dysfunction.16,18 Previous research has reported that shortening of more than 14 mm is associated with unsatisfactory results.19 A biomechanical assessment revealed that shortening of 15 mm or more is associated with reduced muscular strength during the extension, adduction and internal rotation of the humerus, with reduced peak abduction in the injured shoulder.20
We found a significant correlation between the fracture unity and the Constant score. Patients with fracture malunions had reduced shoulder function compared to patients with fracture nonunions. In contrast, patients with good fracture unions had no reductions in their Constant scores. Malunions and nonunions lead to further shortening, which affects shoulder function.18,20
CONCLUSION
Clavicle fracture treatment continues to progress. Based on our findings, we conclude that a comminuted fracture, a fracture displacement of 21 mm or more, a shortening of 15 mm or more and fractures complicated by malunion and nonunion may lead to further shortening and can reduce shoulder function.
We recommend treating fractures with a displacement of more than 21 mm, a shortening of more than 15 mm, symptomatic nonunions and malunions primarily with open reduction and internal fixation with plates and screws. Sometimes, augmentation with bone grafting can enhance the outcome, especially after a comminuted fracture. We recommend that further studies be performed with longer follow–ups because late complications can arise after a clavicle fracture. We also believe that a longer study time frame and more patients could produce more accurate results. Admittedly, a limitation of this study was the difficulty of calling back patients for assessments 6 or more months after their injuries, especially when they felt that their injuries did not cause any significant disability.
ACKNOWLEDGEMENTS
We are indebted to the following dedicated individuals who willingly offered their expertise and valuable time to provide their guidance, opinions and reviews of this article: Associate Prof. Srijit Das and Associate Prof. Rizal.
REFERENCES
- 1.Keener JD, Dahners LE. Percutaneous Pinning of Displaced Midshaft Clavicle Fractures. Techniques Shoulder & Elbow Surgery. 2006;7:175–81. 10.1097/01.bte.0000235402.67223.41 [Google Scholar]
- 2.Collinge C, Devinney S, Herscovici D, DiPasquale T, Sanders R. Anterior-inferior Plate Fixation of Middle-third Fractures and Nonunions of the Clavicle. J Orthop Trauma. 2006;20:680–6. doi: 10.1097/01.bot.0000249434.57571.29. 10.1097/01.bot.0000249434.57571.29 [DOI] [PubMed] [Google Scholar]
- 3.Pope R. Clavicle fracture management conservative versus operative. J Bone Joint Surg (Br) 2002:84-B Suppl III: 214. [Google Scholar]
- 4.Celestre P, Roberston C, Mahar A, Oka R, Meunier M, Schwartz A. Biomechanical Evaluation of Clavicle Fracture Plating Techniques: Does a Locking Plate Provide Improved Stability. J Orthop Trauma. 2008;22:241–7. doi: 10.1097/BOT.0b013e31816c7bac. 10.1097/BOT.0b013e31816c7bac [DOI] [PubMed] [Google Scholar]
- 5.Canadian Orthopaedic Trauma Society. Nonoperative Treatment Compared with Plate Fixation of Displaced Midshaft Clavicular Fractures: A Multicenter, Randomized Clinical Trial. J Bone Joint Surg (Am) 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 6.Zlowodzki M, Zelle B, Cole P, Jeray K, McKee MD. Treatment of Acute Midshaft Clavicle Fractures: Systematic Review of 2144 Fractures: On behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19:504–7. doi: 10.1097/01.bot.0000172287.44278.ef. 10.1097/01.bot.0000172287.44278.ef [DOI] [PubMed] [Google Scholar]
- 7.Edelson G, Saffuri H, Vigder F, Obid E, Nudelman A. Case Reports: Unusual Lateral Clavicle Fracture Dislocation: Case Reports and Museum Specimens. Clin Orthop Rel Res. 2005;439:274–9. doi: 10.1097/01.blo.0000176555.05105.df. 10.1097/01.blo.0000176555.05105.df [DOI] [PubMed] [Google Scholar]
- 8.Neer CS. Non union of the clavicle. J Am Med Assoc. 1960 doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 9.Rowe CR Corr. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop. 1968;58:29–42. [PubMed] [Google Scholar]
- 10.Constant CR. Murley AHG. A Clinical Method of Functional Assessment of the Shoulder. Department of Orthopaedics Surgery, Addenbrooke's Hospital. Cambridge, England. February 26, 1985.
- 11.Conboy VB, Morris RW, Kiss J, Carr AJ. An Evaluation of the Constant-Murley Shoulder Assessment. J Bone Joint Surg (Br) 1996;78-B:229–32. [PubMed] [Google Scholar]
- 12.Krüger–Franke M, Kohne G, Rosemeyer B. Results of operatively treated lateral clavicle fracture. J Orthop Trauma. 2001;15:149. 10.1097/00005131-200102000-00019 [Google Scholar]
- 13.Kashii M, Inui H, Yamamoto K. Surgical Treatment of Distal Clavicle Fractures Using the Clavicular Hook Plate. Clin Orthop Rel Res. 2006;447:158–64. doi: 10.1097/01.blo.0000203469.66055.6a. 10.1097/01.blo.0000203469.66055.6a [DOI] [PubMed] [Google Scholar]
- 14.Khashif Khan LA, Bradnock TJ, Scott C, Robinson CM. Current Concepts Review: Fracture of the Clavicle. J Bone Joint Surg (Am) 2009;91:447–60. doi: 10.2106/JBJS.H.00034. 10.2106/JBJS.H.00034 [DOI] [PubMed] [Google Scholar]
- 15.Wiesel BB, Getz CL. Current concepts in clavicle fractures, malunions and nonunions. Curr Opin Orthop. 2006;17:325–30. 10.1097/01.bco.0000233727.26139.cc [Google Scholar]
- 16.Goss TP. Double disruptions of superior shoulder suspensory complex. J Orthop Trauma. 1993;7:99–106. doi: 10.1097/00005131-199304000-00001. 10.1097/00005131-199304000-00001 [DOI] [PubMed] [Google Scholar]
- 17.Robinson CM. Fractures of the clavicle in the adult: Epidemiology and Classification. J Bone Joint Surg (Br) 1998;80-B:476–84. doi: 10.1302/0301-620x.80b3.8079. 10.1302/0301-620X.80B3.8079 [DOI] [PubMed] [Google Scholar]
- 18.Constant CR, Murley AH. A Clinical method of functional assessment of the shoulder. Clin Orthop Rel Res. 1987;214:160–4. [PubMed] [Google Scholar]
- 19.Lazarides S, Foukas A Zafiropoulos. Conservative Management of Middle-Third Clavicular Fractures-The Relevance of Shortening and Clinical Outcome. J Bone Joint Surg (Br) 2005;87-B:333–4. [Google Scholar]
- 20.Ledger M, Leeks N, Ackland T, Wang A. Short malunions of the clavicle: An Anatomic and Functional Study. J Shoulder Elbow Surg. 2005;14:349–54. doi: 10.1016/j.jse.2004.09.011. 10.1016/j.jse.2004.09.011 [DOI] [PubMed] [Google Scholar]