Abstract
Birch-allergic patients often experience oral allergy syndrome upon ingestion of vegetables and fruits, most prominently apple, that is caused by antibody cross-reactivity of the IgE antibodies in patients to proteins sharing molecular surface structures with the major birch pollen group 1 allergen from Betula verrucosa (Bet v 1). Still, to what extent two molecular surfaces need to be similar for clinically relevant antibody cross-reactivity to occur is unknown. Here, we describe the grafting of a defined conformational antibody epitope from Bet v 1 onto the surface of the homologous apple allergen Malus domestica group 1 (Mal d 1). Engineering of the epitope was accomplished by genetic engineering substituting amino acid residues in Mal d 1 differing between Bet v 1 and Mal d 1 within the epitope defined by the mAb BV16. The kinetic parameters characterizing the antibody binding interaction to Bet v 1 and to the mutated Mal d 1 variant, respectively, were assessed by Biacore experiments demonstrating indistinguishable binding kinetics. This demonstrates that a conformational epitope defined by a high affinity antibody-allergen interaction can successfully be grafted onto a homologous scaffold molecule without loss of epitope functionality. Furthermore, we show that increasing surface similarity to Bet v 1 of Mal d 1 variants by substitution of 6–8 residues increased the ability to trigger basophil histamine release with blood from birch-allergic patients not responding to natural Mal d 1. Conversely, reducing surface similarity to Bet v 1 of a Mal d 1 variant by substitution of three residues abolished histamine release in one patient reacting to Mal d 1.
Keywords: Antigen, Epitope Mapping, Immunology, Mutant, Protein Structure, Allergy, Antibodies, Epitope, Epitope Grafting, Oral Allergy Syndrome
Introduction
Type 1 hypersensitivity, i.e. IgE-mediated allergy, is a substantial health problem in countries having adapted to Western lifestyle (1, 2). Grass pollen and house dust mites are the most important allergen sources world wide (3), but on a regional basis local pollen may be the cause of even higher prevalences of sensitization. In Scandinavia, inhalation allergy to birch pollen is among the most prevalent (4). Patients allergic to birch pollen most often also react to pollens of the related trees alder and hazel (5) prolonging the season with symptom load. Hazel pollinates in February-March, alder typically in March, and birch in April-May. Birch is the quantitatively dominating species reaching average pollen counts in the peak season of about 500 grains per m3, which is about 10 times the level of hazel and alder, and consequently most patients are sensitized to birch pollen. Birch pollen-allergic patients have an increased risk of symptoms upon ingestion of foods, such as nuts and certain vegetables and fruits, for example apple (6, 7). Symptoms induced by the foods are typically mild and restricted to the region around the mouth, for example itching and swelling of lip or tongue and throat irritation. This phenomenon is referred to as the oral allergy syndrome (OAS)2 (8, 9).
Analysis of serum IgE from allergic patients by crossed immunoelectrophoresis has revealed that all birch pollen-allergic patients have IgE directed to the major allergen Bet v 1 (4). Although patients may occasionally react to other allergens, IgE to Bet v 1 accounts for more than 90% of the IgE directed toward birch pollen allergens (4). Molecular studies have shown the presence of major allergens homologous to Bet v 1 in extracts of hazel and alder pollen. The current model for cross-reactivity is that the major allergens with ≥75% sequence identity have common molecular structures (i.e. epitopes) on their surfaces, which are recognized by the same patient IgE antibodies (10). Also, more distantly related species, such as apple, contain molecules homologous to Bet v 1(11, 12). Mal d 1, the major allergen in apple, is a 14-kDa protein that shares 55–65% amino acid sequence identity with Bet v 1. The molecular mechanism underlying OAS upon ingestion of apple is thought to be the same as those responsible for antibody cross-reactivity in general. Sequence similarity between Mal d 1 and Bet v 1 is obviously reduced compared with the more closely related species (hazel and alder), but studies comparing the molecular surfaces of Bet v 1 and Mal d 1 suggest that the OAS is indeed caused by IgE binding to epitopes that are shared between Bet v 1 and Mal d 1 (13). Still, the conserved surface areas between Bet v 1 and Mal d 1 are smaller compared with conserved surface areas between Bet v 1 and Aln g 1, the major allergen of alder pollen, and consequently, only a fraction of birch-allergic patients have IgE directed to the conserved surface areas in Mal d 1 and therefore display OAS upon ingestion of apple.
The dynamics of the processes taking place at the surface of mast cells and basophils have been described in some detail. IgE molecules are anchored to the cell surface through high affinity FcϵRI receptors with the ability to float freely over the cell surface. Effector cell activation occurs after simultaneous binding of the same allergen molecule by two or more IgE antibodies (14). As shown in a recent article (15), using a panel of recombinant allergen-specific IgE antibodies, activation of signal transduction requires that the first interaction is of medium to high affinity to withhold the allergen near the cell surface. The receptor-bound IgE molecules then float to the vicinity of the complex facilitating the second interaction. A consequence of this cooperativity is that if the first interaction is of high affinity then the affinity of the second interaction is not critical, and even low affinity interactions may play a significant role in cross-linking and also effector cell activation. This suggests that an IgE-allergen interaction through a single high affinity antibody may manifest into clinically significant cross-reactivity in the presence of an additional IgE-allergen interaction of any affinity. Still, the degree of similarity of molecular surface structures on related but nonidentical allergens needed to support relevant cross-reactivity in relation to allergy and OAS is still uncertain. Here, a well characterized conformational B-cell epitope from the major birch pollen allergen Bet v 1 was re-created onto the surface of Mal d 1, and the kinetic parameters characterizing antibody-epitope interactions were measured using Biacore technology. Furthermore, the allergenicity of several mutated Mal d 1 variants was investigated in IgE binding assays with birch patient serum IgE and in basophil histamine release experiments with blood from birch-allergic patients to investigate the effects on cross-reactivity of increasing or reducing surface similarity to Bet v 1 of Mal d 1 variants.
EXPERIMENTAL PROCEDURES
Cloning of Constructs
Generation of rMal d 1 variants was initiated on a previously cloned DNA construct (13) coding for Mal d 1 isoform (GenBankTM accession number Q8L6K9) inserted into the Escherichia coli expression vector pMAL-c (New England Biolabs, Hertfordshire, UK). First, nucleotides targeted for mutation that were located close together in the DNA sequence were mutated by PCR-based overlap extension using sense and antisense mutation-specific oligonucleotide primers accommodating each mutation along with sense and antisense oligonucleotide primers accommodating either upstream or downstream neighbor mutations or the N/C terminus of Mal d 1, respectively. Second, the PCR products were purified, mixed, and used as templates in a PCR assembling reaction with oligonucleotide primers accommodating the N and C termini of rMal d 1. The N-terminal primer included nucleotides coding for a Factor Xa cleavage site for generation of rMal d 1 with authentic N terminus. Both oligonucleotide primers contained nucleotide overhang for in-frame directional cloning into the multiple cloning site of pMAL-c. After transformation into E. coli K12, the strain DH5α correct nucleotide sequence of inserts was verified on both DNA strands by DNA sequencing.
Protein Expression and Purification
Expression vector pMAL-c containing inserts coding for rBet v 1 (Z80104), rMal d 1 (Q8L6K9), or rMal d 1 variants were overexpressed in E. coli K12, strain DH5α yielding fusion proteins with N-terminal maltose-binding protein. Purified molecules with authentic N terminus were obtained by amylose-affinity purification followed by Factor Xa cleavage (Protein Engineering Technology APS, Denmark) and size exchange chromatography as described previously in yields of 3–5 mg/liter (16). Protein concentrations were determined by UV absorption at 280 nm in a Shimadzu UV-1601PC (Columbia, MD) spectrophotometer. All purified protein preparations appeared as single bands with an apparent molecular mass of 17.5 kDa after silver-stained SDS-PAGE (data not shown).
Circular Dichroism Spectroscopy
Circular dichroism spectra were obtained using an OLIS DSM 10 CD spectrophotometer (On Line Instrument Systems, Bogart, GA), equipped with cylindrical (31-Q-1/CD) or square (21-Q-1/CD) 0.1-cm light path quartz cuvettes (Starna, Hainault, UK). The spectra were recorded from 260 to 184 nm collecting data at every second nm, 38 data points per spectrum. The temperature of the cuvette was maintained constant using a Julabo model F30-C bath/circulator temperature control module (Julabo Labortechnik, Seelbach, Germany). Spectra were obtained in 0.01 m sodium phosphate buffer, pH 7.2, at a concentration of 0.2 mg of protein per ml. Each spectrum represents the arithmetic mean of four determinations corrected for buffer absorption and normalized to Δϵ = 0 at 260 nm. The millidegree recorded was transformed to Δϵ using Δϵ = millidegree/(32,980·c·l) Aunits/(m·cm), where millidegree is the circular dichroism signal; c is the concentration in mol/liter as measured by amino acid analysis, and l is the length of the light path in cm.
Biacore Experiments
Biacore experiments were set up according to the manufacturer's recommendations (Biacore® 2000 Instrument Handbook, January 2001; Getting started Biacore® 3000, October, 1998), and in brief, the monoclonal antibody BV16 (1–10 μg/ml in HBS-EP Biacore buffer) was injected into the four flow channels on the Biacore Sensor Chip CM5 for 300 s at a flow rate of 30 μl/min (charging phase), followed by a 150-s flow (30 μl/min) of HBS-EP buffer (equilibrium phase). The antigen, i.e. rBet v 1 (Z80104), rMal d 1 (Q8L6K9), or one of the rMal d 1 variants, was injected for 180 s (association phase), followed by an HBS-EP buffer flow (30 μl/min) for up to 1000 s (dissociation phase), and the flow channels were regenerated by a pulse of 10 mm glycine solution, pH 1.8, for 30 s at a flow rate of 30 μl/min. The data used to estimate k1 (m−1·s−1), k−1 (s−1), and Kd (m) values were obtained from runs performed with five different antigen concentrations (1–150 μg/ml).
Specific Human Serum IgE Inhibition Assay
Individual patient sera or serum pools of equal volume of 10 sera from birch pollen-allergic patients was used for specific serum IgE inhibition assays. All patients had a clinical history of birch pollinosis and were radioallergosorbent test class 2 or more against birch extract. Information with respect to clinical history of apple allergy was not available. rBet v 1 was biotinylated at a molar ratio of 1:5 (rBet v 1:biotin). The inhibition assay was performed on ADVIA Centaur System (Bayer, Kgs. Lyngby, Denmark) as follows. A serum sample (25 μl) was incubated with paramagnetic beads (solid phase) coated with a monoclonal mouse anti-human IgE antibody (ALK-Abelló, Hørsholm, Denmark), washed, resuspended, and incubated with a mixture of biotinylated rBet v 1 and inhibitor (nonbiotinylated molecules, i.e. rBet v 1, rMal d 1, or derivate molecules) in dilution series. The amount of biotinylated rBet v 1 bound to the serum IgE on the solid phase was estimated from the measured relative light units after incubation with acridinium ester-labeled streptavidin. The degree of binding was calculated as the ratio between the relative light units obtained using buffer and rBetv 1, rMal d 1, or derivatives as inhibitor.
Histamine Release in Human Basophils
Heparinized blood (20 ml) was drawn from birch pollen-allergic patients with a history of seasonal hay fever, stored at room temperature, and used within 4 h. 100 μl of Pipes buffer, pH 7.4, or 100 μl of allergen dilutions in Pipes buffer, pH 7.4, 1, 3, 10, 30, 100, and 1000 ng of rBet v 1 (Z80104), rMal d 1 (Q8L6K9), or mutated rMal d 1 variants were added to 96-well plates in triplicate. Plates were preheated to 37 °C before 100 μl of preheated (37 °C) blood, diluted 1:5 with Pipes buffer, pH 7.4, was added to wells with different allergen dilutions or Pipes buffer. Plates were incubated 30 min at 37 °C before centrifuging for 10 min at 800 × g in a centrifuge with a plate rotor. Supernatants from each of the wells were transferred to wells in new microtiter plates that were covered and sealed with sealing tape before incubating at −20 °C. All histamine release experiments were performed in triplicate.
Histamine ELISA
Histamine release in each sample was measured using the ELISA-based enzyme immunoassay kit ref. 2015 (Immunotech, France) following the recommendations of the supplier. 100 μl of sample or standard solutions were acylated with 25 μl of acylation buffer and 25 μl of acylation reagent to permit later binding to anti-histamine antibodies. 50 μl of acylated histamine samples, standards, or negative controls were then added to anti-histamine antibody-coated wells along with 200 μl of alkaline phosphatase-conjugated histamine and incubated 2 h at 4 °C with shaking at 250 rpm. Plates were rinsed three times with diluted wash solution before 200 μl of para-nitrophenyl phosphate substrate solution was added to the plates that were incubated for 30 min at room temperature with shaking at 250 rpm before 50 μl of stop solution were added. The ability of the histamine samples and histamine standards (1, 3, 10, 30, 100, and 1000 nm) to inhibit binding of alkaline phosphatase-conjugated histamine to anti-histamine antibody-coated wells was measured as relative absorbance at 405 nm.
Sequence Analysis and Molecular Surface Illustrations
BLAST searches with the amino acid sequence of Mal d 1 (Q8L6K9) were performed at the internet server of the National Center for Biotechnology Information (www.ncbi.nlm.nih.gov) and at the Swiss Institute of Bioinformatics. Three-dimensional structure models of Mal d 1 and mutated variants were obtained using the program Deepview/Swiss-pdb-viewer version 4.0.1 and the SWISS-MODEL Comparative Protein Modeling Server (17) using the Protein Data Bank coordinates for Bet v 1 (1BV1) as template and the amino acid sequences of respective Mal d 1 molecules or Mal d 1 variants. The program DS ViewerPro version 5.0 was used for depiction of the water-accessible molecular surfaces. Unless stated otherwise, amino acid residues conserved between Bet v 1 and Mal d 1 were colored red, and conservative substitutions were colored blue in all models shown. Substitution of amino acid residues within the following groups were considered conservative: Val-Leu-Ile-Met, Ser-Thr-Cys, Phe-Tyr-Trp, Asp-Glu, Asn-Gln, and Lys-Arg-His.
RESULTS
Serum IgE Antibody Cross-reactivity
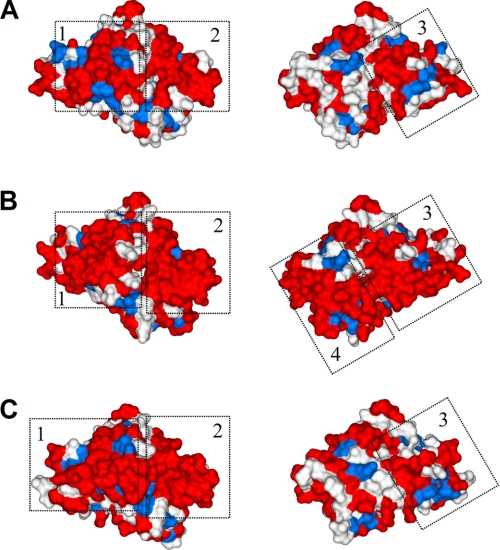
To visualize the basis for birch-allergic serum IgE antibody cross-reactivity toward the apple allergen Mal d 1, the amino acid sequences of 77 published different Mal d 1 isoforms were analyzed with respect to sequence identity to Bet v 1. Structural similarities between Bet v 1 and Mal d 1 enabled modeling of the three-dimensional structure of Mal d 1 isoforms upon combining amino acid sequence information of the different Mal d 1 isoforms with the Protein Data Bank coordinates from the known structure of Bet v 1 (18). In Fig. 1, A–C, the modeled water-accessible molecular surfaces of Mal d 1 isoforms have been color-coded with respect to amino acid identity to Bet v 1. In Fig. 1A, red indicates amino acid residues in Mal d 1 that in ≥90% of available sequences of Mal d 1 isoforms are identical to the corresponding residues found in Bet v 1, and blue indicates naturally occurring conservative substitutions. Fig. 1, B and C, shows the actual conservation of molecular surface structures to Bet v 1 of Mal d 1 isoforms (GenBankTM accession number Q43550 and P43211) having highest (65%) and lowest (55%) amino acid identity, respectively, to Bet v 1 among available sequences. Fig. 1A points out three surface patches that are well conserved between Bet v 1 and most Mal d 1 isoforms. These surface patches vary in shape and size in the molecules in Fig. 1, B and C. Interestingly, Fig. 1B shows an additional patch (Patch 4) that only exists in a subgroup of published Mal d 1 isoforms represented by Mal d 1 (Q43550). Patch 4 is not present in the subgroup represented by Mal d 1 (P43221) shown in Fig. 1C.
FIGURE 1.
Modeled molecular surfaces of Bet v 1 (Z80104) and two Mal d 1 isoforms (Q43550 and P43211) having 65 and 55% amino acid sequence identity to Bet v 1 (Z80104), respectively. Front and back views (turned 180° on vertical axes) are shown. A, red color indicates residues shared between Bet v 1 and ≥90% of available Mal d 1 sequences. Blue color indicates residues that in ≥90% of Mal d 1 isoforms are either shared with Bet v 1 or conservatively substituted. Three surface patches are framed that are shared between Bet v 1 and 9 of10 Mal d 1 isoforms. Patch 1 contains 28 residues, Glu-42, Ile-44, Glu-45, Gly-46, Gly-48, Gly-49, Gly-51, Thr-52, Thr-53, Lys-55, Tyr-66, Val-67, Lys-68, Arg-70, Val-71, Asp-72, Ser-84, Val-85, Ile-86, Glu-87, Gly-88, Ile-91, Leu-95, Glu-96, Lys-97, Ile-98, Ser-99, and His-121. Patch 2 contains 19 residues, Leu-24, Asp-25, Asp-27, Asn-28, Leu-29, Pro-31, Lys-32, Val-33, Ala-34, Pro-35, Gln-36, Ala-37, Glu-148, Tyr-150, Leu-151, Asp-156, Ala-157, Tyr-158, and Asn-159. Patch 3 contains 11 residues, Tyr-5, Glu-6, Glu-8, Glu-127, Val-128, Lys-129, Glu-131, Val-133, Lys-134, Lys-137, and Glu-138. B shows residues shared between Bet v 1 and Mal d 1 isoform Q43550. Red (identity) and blue (conservatively substituted residues). Four surface patches shared between Bet v 1 and Mal d 1 (Q43550) are framed. C shows residues shared between Bet v 1 and Mal d 1 isoform P43211. Red (identity) and blue (conservatively substituted residues). Three surface patches shared between Bet v 1 and Mal d 1 P43211 are framed.
Epitope Grafting
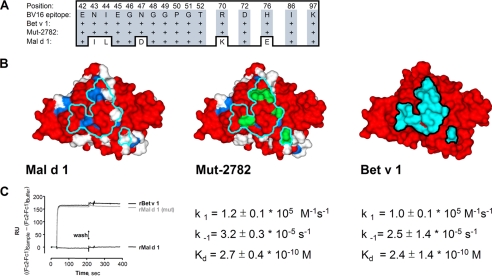
The mAb BV16 binds an epitope on Bet v 1. Previously, the precise epitope was identified from the crystal structure of the Bet v 1-BV16 Fab complex (19), and a clear inhibition of birch-allergic serum IgE by mAb BV16 was shown (19) illustrating the relevance of the BV16-defined epitope on Bet v 1 for IgE binding. Here, the requirements for Bet v 1-specific antibody cross-reactivity between Bet v 1 and Mal d 1 were investigated in further detail in a model system, including anti-Bet v 1 mAb BV16 together with rBet v 1, rMal d 1, and variants of Mal d 1 (Table 1). The x-ray structure of the complex revealed 16 amino acid residues (Fig. 2A) in rBet v 1 that constitute a 931-Å2 conformational B-cell epitope on the Bet v 1 surface. Fig. 2B (right model, Bet v 1) depicts the footprint of the BV16 epitope on rBet v 1. Five residues within the antibody footprint are different between rBet v 1 and rMal d 1 (Q8L6K9), seen as blue- or white-colored residues in the left model, depicting Mal d 1. The center model illustrates the grafting of the “BV16 epitope” into the Mal d 1 variant (Mut-2782) through substitution of these five residues to residues found in corresponding positions in Bet v 1. Fig. 2C shows a Biacore diagram illustrating the interaction between the mAb BV16 and each of the three molecules. The BV16 antibody did not bind Mal d 1 with any measurable strength. Kinetic parameters for the interaction with Bet v 1 and the Mal d 1 variant with the grafted BV16 epitope are displayed below the respective models. The very similar kinetic parameters characterizing antibody binding to Bet v 1 and Mut-2782 as both being of high affinity show full recognition of the grafted epitope on the engineered Mal d 1 variant Mut-2782 by BV16.
TABLE 1.
Mutated recombinant Mal d 1 variants
| Mutated variants | Amino acid substitutionsa |
|---|---|
| Mut-2782b,c,d | I43N, L44I, D47N, K70R, E76H |
| Mut-2781b,d,e,f | I43N, L44I, D47N, G65K, K70R, E76H |
| Mut-2762b,f,g | E12V, P16A, S107T, G108P, +109D, S110G, K152L, P155S |
| Mut-2760f,h | N28T, K32Q, E45S |
a Amino acid substitutions were introduced into Mal d 1 (Q8L6K9).
b Residues in Mal d 1 were substituted to residues present in corresponding positions in Bet v 1.
c All five mutations in Mut-2782 are located within the BV16 antibody footprint illustrated in Fig. 2.
d Mut-2781 and Mut-2782 were tested along with rBet v 1 and rMal d 1 in Biacore experiments with mAb BV16.
e In addition to the five mutations located within the BV16 antibody footprint, Mut-2781 contains an additional mutation G65K located outside the footprint as shown in Fig. 3B.
f Mut-2781, Mut-2762, and Mut-2760 were tested along with rBet v 1 and rMal d 1 in IgE-binding experiments with birch-allergic patient sera and in histamine release assays with blood from birch-allergic patients.
g (+109D) refers to the insertion of aspartic acid extending the length of the mutated molecule to 159 amino acid residues.
h Residues in Mal d 1 were substituted to residues not present in corresponding positions in Bet v 1.
FIGURE 2.
A, amino acid sequence alignment of residues present within the epitope defined by the binding of the mAb BV16 to Bet v 1 in Bet v 1, Mal d 1, and the mutated Mal d 1 variant Mut-2782. Five residues within the antibody footprint are not shared between Mal d 1 and Bet v 1. All 16 residues within the antibody footprint are shared between Bet v 1 and Mut-2782. B, modeled molecular surfaces of Mal d 1, Mut-2782 with the BV16 epitope grafted onto its surface, and Bet v 1. Amino acid residues are color-coded according to amino acid identity (red) to Bet v 1 and (blue) indicates naturally occurring conservative substitutions. Right model shows Bet v 1 (Z80104) with 16 amino acid residues colored cyan that make up the BV16 epitope. Left model shows Mal d 1 (Q8L6K9) with the antibody footprint visible in cyan. Center model shows Mut-2782 with the antibody footprint visible in cyan and mutated amino acid residues colored in green. C, kinetic parameters for the binding of mAb BV16 are shown below each model. No binding to Mal d 1 could be detected, whereas very similar kinetic parameters characterize BV16 antibody binding to Bet v 1 and Mut-2782 were found.
With the aim to further investigate the structural basis for antibody cross-reactivity from birch-allergic patients with Mal d 1, additional Mal d 1 variants were engineered (Table 1). An amino acid sequence alignment of Bet v 1, Mal d 1, and all mutated variants is shown in Fig. 3A. Mut-2782 (Fig. 2B), Mut-2781 (Fig. 3B), and Mut-2762 (Fig. 3C) all illustrate Mal d 1 variants with increased surface similarity to the Bet v 1 allergen. Mut-2762 was designed with the intention to increase surface similarity to Bet v 1 in a surface area on Mal d 1 clearly separated from the epitope defined by mAb BV16. As seen from Fig. 3C, Mut-2762 contains a surface area shared with Bet v 1 that is very similar to “Patch 4” shown in Fig. 1B, which is shared between a subgroup of naturally occurring isoforms of Mal d 1 and Bet v 1. In Mut-2781, Mut-2782, and Mut-2762, mutations are located in surface areas that on naturally occurring Mal d 1 isoforms are specific to Mal d 1, and all targeted residues were substituted to residues that are present in the corresponding positions in Bet v 1. In contrast, Fig. 3D displays the modeled molecular surface of Mut-2760 that contains mutations intended to reduce surface similarity to Bet v 1. Here, three residues Asn-28, Lys-32, and Glu-45 shared between Mal d 1 and Bet v 1 were substituted with residues differing from the ones found in the corresponding positions of known Bet v 1 isoforms. These residues were chosen for substitution based on previous data showing that they are critical residues in Bet v 1 for binding birch-allergic patients serum IgE antibodies (20).
FIGURE 3.
A, B, C, and D, amino acid residues identical with residues in Bet v 1 or conservatively substituted are shown in red and blue colors, respectively. A, amino acid sequence alignment of Bet v 1, Mal d 1, and mutated variants. Symbols #, X, @, and $ mark positions of introduced point mutations in Mut-2781, Mut-2782, Mut-2762, or Mut-2760, respectively. Amino acid residue positions in Bet v 1 are shown with numbers above aligned sequences. For the C-terminal part of Mal d 1, residue positions are shown below aligned sequences. B, modeled molecular surfaces of Mal d 1, Mut-2781, and Bet v 1 (front views). Green color shows the positions of six introduced point mutations in Mut-2781 that increases surface similarity to Bet v 1 within (five mutations) and around (1 mutation) the epitope defined by the BV16 antibody. C, modeled molecular surfaces of Mal d 1, Mut-2762, and Bet v 1 (back views). Frame marks Patch 4 previously defined in Fig. 1B. Green color shows the positions of eight introduced point mutations in Mut-2762 that increases surface similarity to Bet v 1 within Patch 4. D, modeled molecular surfaces of Mal d 1, Mut-2760, and Bet v 1 (front views). Frame marks Patch 2 previously defined in Fig. 1A. Yellow color shows the positions of three introduced point mutations in Mut-2760 of which two mutations decrease surface similarity to Bet v 1 within Patch 2. E, CD spectra. All spectra of mutated molecules Mut-2781 (□), Mut-2762 (Δ), and Mut 2760 (♢) recorded at 15 °C are similar to spectra of wild type molecules rBetv 1 (●) and rMal d 1 (▴) recorded at 15 °C that are different from the spectrum of denatured rBet v 1 (×) recorded at 90 °C.
Maintained Structural Integrity of rBet v 1, rMal d 1, and Mutated rMal d 1 Variants
To confirm the structural integrity of wild type and mutated molecules, the presence of secondary structure elements were analyzed by circular dichroism (CD) spectroscopy. Fig. 3E shows an overlay of CD spectra obtained at 15 °C. A CD spectrum of heat-denatured rBet v 1 obtained at 90 °C is included for comparison. The spectra of rBet v 1, rMal d 1, and mutated variants all have negative and positive amplitudes at 212–216 and 192–194 nm, respectively, characteristic for nBet v 1. All five spectra are different from the CD spectrum of heat-denatured rBet v 1, which is characterized by negative and positive amplitudes at 200 and 186 nm, respectively. This suggests that the containment of secondary structure elements is unaffected by the introduced point mutations and that all of the molecules have maintained structural integrity. CD spectroscopy was not applied to Mut-2782. However, BV16 binds a conformational epitope on Mut-2781 and Mut-2782 with identical kinetics strongly indicating identical folding patterns. Therefore, in this study the reported effects of introducing mutations was in all cases caused by local changes in surface topography and charge distribution and was not caused by loss of overall structure integrity.
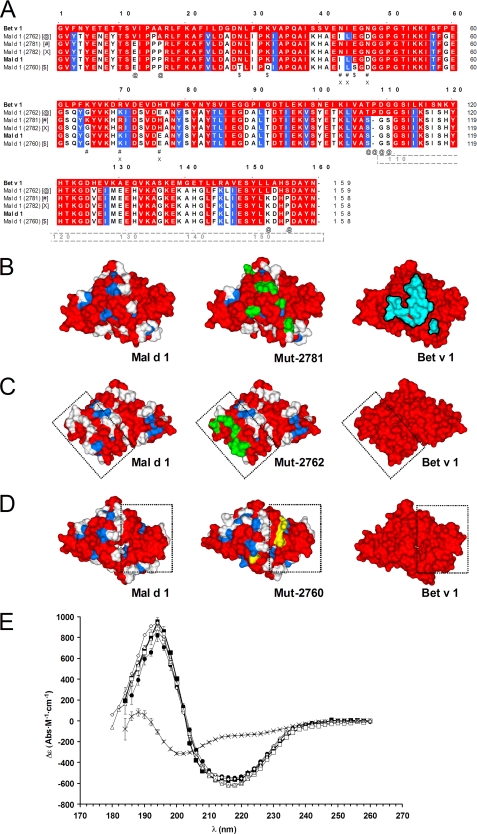
Increasing Surface Similarity to Bet v 1 of Mal d 1 Variants Increased Binding of Birch Allergic Serum IgE
Compared with wild type rMal d 1, the mutated variants Mut-2781 and Mut-2762 with point mutations that increase surface similarity to Bet v 1 showed increased binding of pooled serum IgE from patients with birch allergies. Fig. 4 (left column) shows the binding of human serum IgE to biotinylated rBet v 1 inhibited by rBet v 1, rMal d 1 or mutated Mal d 1 variants, respectively. Fig. 4, A and B, shows the degree of inhibition when testing serum pools A and B, respectively. Serum pool A is a pool of sera from 10 birch pollen-allergic patients tested positive for IgE against Bet v extract (ALK-Abelló, Magic Lite®, class 3) and Mal d extract (GE Healthcare, CAP®, class 2–4). Serum pool B is a pool of 10 sera from patients tested positive for IgE against Bet v extract (Magic Lite®, class 3) but negative against Mal d extract (CAP®, class 0). Fig. 4, C and D, shows the degree of inhibition when testing individual patient sera. In all four graphics, rBet v 1 shows full inhibition at the highest inhibitor concentration, whereas wild type rMal d 1 inhibits IgE binding poorly. Compared with rMal d 1, the two mutated Mal d 1 variants with increased surface similarity to Bet v 1 inhibit IgE-binding to Bet v 1 to a larger extent.
FIGURE 4.
IgE inhibition (left column) and histamine release (right column). For IgE inhibition assay, graphs A–D show the binding of serum IgE (individual sera or serum pools) to biotinylated rBet v 1 upon inhibition with rBet v 1 (●), rMal d 1 (▾), or mutated rMal d 1 variants Mut-2781 (□) and Mut-2762 (Δ) with increased surface similarity to Bet v 1. Serum pool A, 10 sera sensitive to Bet v and Mal d extracts. Serum pool B, 10 sera sensitive to Bet v extract solely. In all graphs full inhibition is obtained with rBet v 1 as inhibitor. Compared with rMal d 1 that shows very little inhibition, the mutated variants Mut-2781 and Mut2762 inhibit binding of serum IgE to biotinylated rBet v 1 to a larger degree. For histamine release assay, graphs E, F, and G show the results of histamine release with blood from three individual birch-allergic patients. No histamine release is obtained with rMal d 1 (▾), whereas histamine release is seen with rBet v 1 (●) as well as with the mutated rMal d 1 variants Mut-2781 (□) and Mut-2762 (Δ) with increased surface similarity to Bet v 1.
Increasing Surface Similarity to Bet v 1 of Mal d 1 Variants Increased the Ability to Trigger Histamine Release in Birch Allergic Basophils
Recombinant Bet v 1, rMal d 1, Mut-2781, and Mut-2762 were tested in standard basophil histamine release assays. Fig. 4 (right column) shows the results of three histamine release experiments (E, F, and G) with blood drawn from three individual birch-allergic patients not reacting to apple. The increased surface similarity to Bet v 1 of the Mal d 1 variants mut-2781 and mut-2762 enabled both molecules to trigger basophil histamine release with blood from these patients.
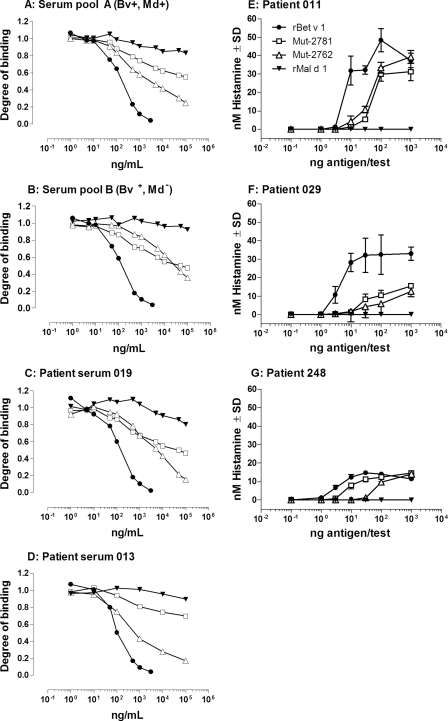
Reduction of Surface Similarity to Bet v 1 of a Mal d 1 Variant Affected Histamine Release from Individual Basophils Differently
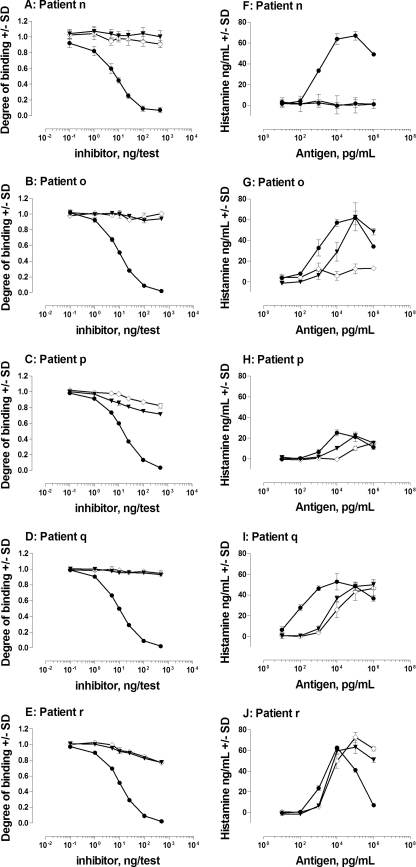
rBet v 1, rMal d 1, and the mutated variant Mut-2760 were tested in IgE inhibition experiments with individual sera from five birch pollen allergic patients and biotinylated Bet v 1 (Fig. 5, left column). rBet v 1 inhibits binding fully at maximum inhibitor concentration, whereas rMal d 1 and Mut-2760 inhibited poorly the binding of serum IgE from different patients to biotinylated rBet v 1. Blood obtained from the same five individual patients was used in basophil histamine release assays (Fig. 5, right column). Here, rBet v 1 triggered strong histamine release responses with basophils from all patients, whereas notable patient-to-patient variations were seen with rMal d 1. In basophils from patient (n), no histamine release occurred within the measured antigen concentration range. In basophils from patients o, p, and q, 10–100-fold higher concentrations of rMal d 1 were needed to initiate histamine release when compared with rBet v 1. In basophils from patient r, the difference was considerably less i.e. 0–3-fold. Still, rMal d 1 had the ability to reach histamine release levels (maximum release) equal to those obtained with rBet v 1 in basophils from four patients (o, p, q, and r). The Mal d 1 variant Mut-2760 with point mutations that reduce surface similarity to Bet v 1 affected histamine release in basophils from individual patients differently. As with wild type rMal d 1, no histamine release occurred within the measured antigen concentration range when testing basophils from patient n. With basophils from patient o, histamine release was abolished in the measured antigen concentration range. In basophils from patient p, a 10-fold reduced potency of Mut-2760 to trigger histamine release was seen compared with Mal d 1. In basophils from patients q and r, no difference was seen.
FIGURE 5.
IgE binding and histamine release experiments. For IgE inhibition assay, graphs A–E (left column) show binding of individual (n, o, p, q, and r) birch serum IgE samples to biotinylated rBet v 1 upon inhibition with rBet v 1 (●), rMal d 1 (▾), or a mutated rMal d 1 variant Mut-2760 (♢), with point mutations that decrease surface similarity to Bet v 1. In all graphs, binding of serum IgE is inhibited fully by rBet v 1, whereas little inhibition is caused by rMal d 1 or the variant Mut-2760. For histamine release assay, graphs F–J (right column) show the results of histamine release experiments using blood from the same panel of individual birch-allergic patients (n, o, p, q, and r). rBet v 1 triggered histamine release in basophils from all five patients, whereas notable patient-to-patient variations were seen with rMal d 1 and the variant Mut-2760. Interestingly, three mutations N28T, K32Q, and E45S that decrease surface similarity to Bet v 1 of variant Mut-2760 abolished histamine release in patient o.
DISCUSSION
Bet v 1 in complex with an antibody Fab fragment from the mAb BV16 raised against natural Bet v 1 has previously been crystallized (19). In this study, the molecular surface of Mal d 1, which shares 60% amino acid identity to Bet v 1 and is not recognized by mAb BV16, was altered by introduction of five point mutations. After these alterations, all of the 16 amino acid residues that constitute the BV16 epitope on the surface of rBet v 1 were present in the corresponding surface area on the Mal d 1 variant Mut-2782, as if the epitope had been grafted onto the molecular surface. The kinetics of the complex formation between BV16 and Mut-2782 and the complex formation between BV16 and Bet v 1 were nearly identical, which strongly indicates a perfect fit between epitope and paratope in both complexes, and confirm that full functionality of the assembled conformational epitope on the engineered Mal d 1 variant has been achieved. The identical CD spectra obtained here for Bet v 1 and Mal d 1 indicate equal folding patterns that must be assumed to be very important for the formation of this nonlinear epitope and in this case a prerequisite for epitope grafting. The allergen preparations used did not activate basophils passively sensitized with a monoclonal humanized recombinant IgE antibody form of BV16 (see supplemental Fig. E1), excluding possible oligomerization/aggregation of the allergen.
We have previously illustrated the molecular basis of birch-allergic patient antibody cross-reactivity to the group 1 allergen from apple by analysis of 17 Mal d 1 isoform sequences (13). Here, a total of 77 different Mal d 1 isoform sequences originating from 12 different apple varieties was analyzed with the purpose of identifying structurally identical surface patches on Bet v 1 and Mal d 1 large enough to accommodate antibody binding. Available crystal structures of antibody-antigen interactions suggest that a typical epitope covers ∼600–900 Å2 on the surface of the antigen (21, 22). Here, four such patches of sufficient sizes (Fig. 1) on Mal d 1 were identified where birch-allergic patient serum IgE may bind. Surprisingly, despite the dominance of conserved residues in the models in Fig. 1, our IgE binding data show that the large majority of specific IgE antibodies from birch-allergic patients fails to bind Mal d 1 in a competition assay with biotinylated Bet v 1 (Fig. 4). This indicates that few IgE antibody specificities in IgE repertoires from patients bind surface areas with high affinity that are conserved between Bet v 1 and Mal d 1. Still, it is tempting to suggest that the presence of IgE directed against the surface patches conserved among Bet v 1 and Mal d 1 increases the risk of cross-allergic reactions as those seen with OAS. Furthermore, serum pool A, with IgE reactivity to birch and apple (Fig. 4A), and serum pool B, with IgE reactivity to only birch (Fig. 4B), only showed modest differences in IgE binding capacities to rMal d 1 implying that even small differences among birch-allergic IgE repertoires may determine the ability to potentiate allergic reactions to apple and may determine whether or not a particular patient experiences OAS.
Here, we show that changing the allergen epitope composition by increasing or reducing the surface similarity to Bet v 1 in confined surface areas on Mal d 1 variants has a huge impact on the histamine release patterns obtained with basophils from birch-allergic individuals. Amino acid residues Glu-45, Pro-108, Asn-28, and Lys-32 all present in surface structures on Bet v 1 that are conserved among the group 1 Fagales allergens have previously been demonstrated to be critical residues for binding of birch-allergic patient serum IgE to Bet v 1 (23). In later studies with the homologous protein from cherry, Pru av 1, residues Glu-45 (24) and Asn-28 (25) have likewise been identified as critical residues for IgE binding. Here, we show (Fig. 5) notable differences between birch-allergic patient basophil histamine release profiles upon testing of wild type rMal d 1 and the mutated variant Mut-2760 (N28T, K32Q, E45S) with point mutations that decrease surface similarity to Bet v 1. This result illustrates that IgE repertoires from allergic patients can be expected to vary from patient to patient and that different IgE antibodies binding different epitopes on Mal d 1 may be responsible for OAS in individual patients. In addition, the unresponsiveness toward Mut-2760 seen with blood from patient o suggests that histamine release in this patient caused by wild type rMal d 1 is because of the presence of few or as little as two different IgE-binding epitopes. This result may explain why some birch-allergic patients suffer from OAS to apple despite the result in Fig. 4 showing effectively no inhibition of serum IgE binding to Bet v 1 by Mal d 1.
In addition, the classical view states that the minimum requirements for basophil and mast cell activation involves cross-linking of antigen by two receptor-bound IgE antibodies that bind two nonoverlapping epitopes on the same antigen. However, it has been hypothesized (26) that one high affinity IgE antibody on the surface of an effector cell may act as a stable surface anchor hereby facilitating binding to a second IgE antibody even if the second antibody involved binds the antigen with very poor affinity. This theory was recently supported by data from basophil activation experiments with a panel of humanized recombinant IgE antibodies binding the house dust mite allergen rDer p 2 with low, medium, or high affinity (15). Here, the combination of a single high affinity IgE specificity combined with a single low affinity IgE specificity was almost as effective as the combination of two high affinity IgE specificities, and both combinations resulted in potent histamine release responses. Therefore, whether or not an individual suffers from OAS may be determined by the existence of a single IgE antibody specificity binding a single “birch-like epitope” present on Mal d 1 with medium to high affinity causing effector cell activation through cross-linking of antigen in complexes with low affinity IgE antibodies. Together, this indicates that the number of birch-like epitopes in Mal d 1 bound by high affinity IgE that is responsible for antibody cross-reactivity in a particular birch-allergic patient may be few and interestingly that low affinity IgE antibodies may play an important role in cross-allergies.
Specific immunotherapy (SIT) is a highly effective treatment of allergic disease that reduces both the immediate allergic symptoms as well as late phase responses (27). Current treatment depends on the use of standardized allergen extracts administered to patients for a period of 3–5 years. SIT based on subcutaneous injection of allergen extract is associated with a small but significant risk of inducing systemic allergic adverse reactions. Several concepts for the improvement of vaccines for subcutaneous SIT have therefore been proposed. Most concepts aim for a reduction in the anaphylactic potential of the vaccine component either through disruption of the tertiary structure of the allergen, e.g. allergen-derived peptides (28, 29), or through disruption of epitopes by substitution of surface-exposed single amino acid residues on structurally intact allergens (20, 23). A vaccine for SIT based on allergen-derived peptides focuses solely on a modulation of the existing T-cell response, whereas the latter concept also focuses on maintaining surface structures for the induction of so-called blocking IgG antibodies (30, 31) reactive with the native allergen. The approach, however, is hampered by the heterogeneity of responses from allergic patients, and the concept may be dependent on the introduction of mutations in numbers leading to structural destabilization of the resulting molecule.
Conceptually, a novel approach to rational allergy vaccine engineering might be based on epitope grafting, i.e. the building of allergen-specific antibody-binding epitopes into a stable homologous scaffold molecule that, with respect to binding IgE antibodies from allergic patients, ideally should be inert. The idea is to generate a vaccine with reduced anaphylactic potential by splitting the allergen surface onto separate vaccine molecule components. Ideally, the size of the surface graft on each scaffold molecule should allow for several overlapping epitopes to exist but be restricted in size to allow only one IgE antibody to bind within the surface graft at the same time. Potentially, such a multicomponent-based vaccine will be unable to activate effector cells as this would require specific IgE antibodies to bind two or more nonoverlapping epitopes on the same scaffold molecule. The vaccine, however, would be able to generate blocking IgG antibodies directed against all the overlapping epitopes present within the grafted surface areas present on the different vaccine components. In line with the results of other studies (32, 33), we have demonstrated reactivity with Mal d 1 of Bet v 1-specific T-cell lines, and in addition, the T-cell recognition of rMal d 1 variants was not influenced by the mutations investigated in this study (see supplemental Fig. E2). Still, a scaffold molecule that is very distantly related but structurally similar to the allergen in question would probably lack most if not all allergen-specific T-cell epitopes. Grafting of both specific B-cell epitopes as well as specific T-cell epitopes might therefore be necessary to obtain a suited vaccine candidate. The grafting of the BV16 epitope from Bet v 1 to Mal d 1 performed in this study was a first attempt to follow such a strategy, and this study shows that it is possible to shape a conformational B-cell epitope onto the surface of a homologous scaffold molecule having 60% amino acid identity to Bet v 1 and maintain epitope functionality. Further work is needed to show whether a conformational epitope can be grafted onto a homologous scaffold molecule that is exceedingly more distantly related to Bet v 1.
Supplementary Material
Acknowledgments
We thank Jeanette Haugel-Nielsen, Lise Hansen, Jette Skovsgaard, Annette Giselsson, Michael G. Jensen, Lotte Friberg, Gitte Grauert, and Lotte Heerfordt for excellent technical assistance.

The on-line version of this article (available at http://www.jbc.org) contains supplemental Figs. E1 and E2.
- OAS
- oral allergy syndrome
- SIT
- specific immunotherapy.
REFERENCES
- 1. Linneberg A., Gislum M., Johansen N., Husemoen L. L., Jørgensen T. (2007) Clin. Exp. Allergy 37, 1137–1142 [DOI] [PubMed] [Google Scholar]
- 2. Jõgi R., Janson C., Björnsson E., Boman G., Björkstén B. (1998) Clin. Exp. Allergy 28, 1072–1080 [DOI] [PubMed] [Google Scholar]
- 3. Larsen J. N., Houghton C. G., Løwenstein H., Lombardero M. (2004) Clin. Allergy Immunol. 18, 433–455 [PubMed] [Google Scholar]
- 4. Ipsen H., Løwenstein H. (1983) J. Allergy Clin. Immunol. 72, 150–159 [DOI] [PubMed] [Google Scholar]
- 5. Ipsen H., Bøwadt H., Janniche H., Nüchel Petersen B., Munch E. P., Wihl J. A., Løwenstein H. (1985) Allergy 40, 510–518 [DOI] [PubMed] [Google Scholar]
- 6. Hannuksela M., Lahti A. (1977) Contact Dermatitis 3, 79–84 [DOI] [PubMed] [Google Scholar]
- 7. Vieths S., Scheurer S., Ballmer-Weber B. (2002) Ann. N.Y. Acad. Sci. 964, 47–68 [DOI] [PubMed] [Google Scholar]
- 8. Amlot P. L., Kemeny D. M., Zachary C., Parkes P., Lessof M. H. (1987) Clin. Allergy 17, 33–42 [DOI] [PubMed] [Google Scholar]
- 9. Ausukua M., Dublin I., Echebarria M. A., Aguirre J. M. (2009) Med. Oral Patol. Oral Cir. Bucal. 11, 568–572 [DOI] [PubMed] [Google Scholar]
- 10. Ipsen H., Wihl J. A., Petersen B. N., Løwenstein H. (1992) Clin. Exp. Allergy 22, 391–399 [DOI] [PubMed] [Google Scholar]
- 11. Ebner C., Birkner T., Valenta R., Rumpold H., Breitenbach M., Scheiner O., Kraft D. (1991) J. Allergy Clin. Immunol. 88, 588–594 [DOI] [PubMed] [Google Scholar]
- 12. Aalberse R. C., Akkerdaas J., van Ree R. (2001) Allergy 56, 478–490 [DOI] [PubMed] [Google Scholar]
- 13. Holm J., Baerentzen G., Gajhede M., Ipsen H., Larsen J. N., Løwenstein H., Wissenbach M., Spangfort M. D. (2001) J. Chromatogr. B Biomed. Sci. Appl. 756, 307–313 [DOI] [PubMed] [Google Scholar]
- 14. Alam R. (2009) in Allergy and Allergic Diseases (Kay A. B., Kaplan A. P., Bousquet J., Holt P. G. eds) 2nd Ed., Vol. 1., pp. 203–213, Wiley-Blackwell, London, UK [Google Scholar]
- 15. Christensen L. H., Holm J., Lund G., Riise E., Lund K. (2008) J. Allergy Clin. Immunol. 122, 298–304 [DOI] [PubMed] [Google Scholar]
- 16. Spangfort M. D., Ipsen H., Sparholt S. H., Aasmul-Olsen S., Larsen M. R., Mørtz E., Roepstorff P., Larsen J. N. (1996) Protein Expr. Purif. 8, 365–373 [DOI] [PubMed] [Google Scholar]
- 17. Arnold K., Bordoli L., Kopp J., Schwede T. (2006) Bioinformatics 22, 195–201 [DOI] [PubMed] [Google Scholar]
- 18. Gajhede M., Osmark P., Poulsen F. M., Ipsen H., Larsen J. N., Joost van Neerven R. J., Schou C., Løwenstein H., Spangfort M. D. (1996) Nat. Struct. Biol. 3, 1040–1045 [DOI] [PubMed] [Google Scholar]
- 19. Mirza O., Henriksen A., Ipsen H., Larsen J. N., Wissenbach M., Spangfort M. D., Gajhede M. (2000) J. Immunol. 165, 331–338 [DOI] [PubMed] [Google Scholar]
- 20. Holm J., Gajhede M., Ferreras M., Henriksen A., Ipsen H., Larsen J. N., Lund L., Jacobi H., Millner A., Würtzen P. A., Spangfort M. D. (2004) J. Immunol. 173, 5258–5267 [DOI] [PubMed] [Google Scholar]
- 21. Davies D. R., Padlan E. A., Sheriff S. (1990) Annu. Rev. Biochem. 59, 439–473 [DOI] [PubMed] [Google Scholar]
- 22. Braden B. C., Cauerhff A., Dall'Acqua W., Fields B. A., Goldbaum F. A., Malchiodi E. L., Mariuzza R. A., Poljak R. J., Schwarz F. P., Ysern X., et al. (1995) Ann. N.Y. Acad. Sci. 764, 315–327 [DOI] [PubMed] [Google Scholar]
- 23. Spangfort M. D., Mirza O., Ipsen H., Van Neerven R. J., Gajhede M., Larsen J. N. (2003) J. Immunol. 171, 3084–3090 [DOI] [PubMed] [Google Scholar]
- 24. Neudecker P., Lehmann K., Nerkamp J., Haase T., Wangorsch A., Fötisch K., Hoffmann S., Rösch P., Vieths S., Scheurer S. (2003) Biochem. J. 376, 97–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wiche R., Gubesch M., König H., Fötisch K., Hoffmann A., Wangorsch A., Scheurer S., Vieths S. (2005) Biochem. J. 385, 319–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aalberse R. C., Kleine Budde I., Stapel S. O., van Ree R. (2001) Allergy 56, 27–29 [DOI] [PubMed] [Google Scholar]
- 27. Bousquet J., Lockey R. F., Malling H. J. (1998) Allergy 53, (Suppl. 44) 1–42 [Google Scholar]
- 28. Norman P. S., Ohman J. L., Jr., Long A. A., Creticos P. S., Gefter M. A., Shaked Z., Wood R. A., Eggleston P. A., Hafner K. B., Rao P., Lichtenstein L. M., Jones N. H., Nicodemus C. F. (1996) Am. J. Respir. Crit. Care Med. 154, 1623–1628 [DOI] [PubMed] [Google Scholar]
- 29. Alexander C., Ying S. B, Kay A., Larché M. (2005) Clin. Exp. Allergy 35, 52–58 [DOI] [PubMed] [Google Scholar]
- 30. Lichtenstein L. M., Holtzman N. A., Burnett L. S. (1968) J. Immunol. 101, 317–324 [PubMed] [Google Scholar]
- 31. Flicker S., Valenta R. (2003) Int. Arch. Allergy Immunol. 132, 13–24 [DOI] [PubMed] [Google Scholar]
- 32. Fritsch R., Bohle B., Vollmann U., Wiedermann U., Jahn-Schmid B., Krebitz M., Breiteneder H., Kraft D., Ebner C. (1998) J. Allergy Clin. Immunol. 102, 679–686 [DOI] [PubMed] [Google Scholar]
- 33. Jahn-Schmid B., Radakovics A., Lüttkopf D., Scheurer S., Vieths S., Ebner C., Bohle B. (2005) J. Allergy Clin. Immunol. 116, 213–219 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.