Abstract
Background:
Managing cerebrovascular risk factors is complex and difficult. The objective of this program evaluation was to assess the effectiveness of an outpatient Multidisciplinary Stroke Clinic model for the clinical management of veterans with cerebrovascular disease or cerebrovascular risk factors.
Methods:
The Multidisciplinary Stroke Clinic provided care to veterans with cerebrovascular disease during a one-half day clinic visit with interdisciplinary evaluations and feedback from nursing, health psychology, rehabilitation medicine, internal medicine, and neurology. We conducted a program evaluation of the clinic by assessing clinical care outcomes, patient satisfaction, provider satisfaction, and costs.
Results:
We evaluated the care and outcomes of the first consecutive 162 patients who were cared for in the clinic. Patients had as many as six clinic visits. Systolic and diastolic blood pressure decreased: 137.2 ± 22.0 mm Hg versus 128.6 ± 19.8 mm Hg, P = 0.007 and 77.9 ± 14.8 mm Hg versus 72.0 ± 10.2 mm Hg, P = 0.004, respectively as did low-density lipoprotein (LDL)-cholesterol (101.9 ± 23.1 mg/dL versus 80.6 ± 25.0 mg/dL, P = 0.001). All patients had at least one major change recommended in their care management. Both patients and providers reported high satisfaction levels with the clinic. Veterans with stroke who were cared for in the clinic had similar or lower costs than veterans with stroke who were cared for elsewhere.
Conclusion:
A Multidisciplinary Stroke Clinic model provides incremental improvement in quality of care for complex patients with cerebrovascular disease at costs that are comparable to usual post-stroke care.
Keywords: clinical management of stroke, cost, blood pressure management, clinical outcome
Introduction
Approximately 780,000 people sustain a stroke in the United States each year.1 More specifically, it is estimated that at least 15,000 veterans have a stroke annually.2 Stroke is a leading cause of serious disability and is the third leading cause of death.3–6 The majority of stroke survivors are discharged from the acute care setting, and return home with mild or moderate physical, cognitive, or emotional deficits that require ongoing care and medical attention.7
Coordinated multidisciplinary inpatient stroke care, such as that provided by stroke teams in stroke units, has been shown to improve mortality and functional recovery post-stroke.8,9 Multidisciplinary outpatient clinical programs have been shown to improve patient outcomes in cardiovascular care, pain, and rehabilitation settings.10–12 Although post-stroke outpatient clinics have been described in the literature,10–13 there are few data about the use or effectiveness of a multidisciplinary approach to stroke care in the outpatient setting.
Based on the robust evidence regarding multidisciplinary care in the inpatient stroke setting and in the outpatient setting for other chronic conditions, we developed and evaluated the use of a multidisciplinary stroke program in the outpatient setting. The objective of this program evaluation was to assess the effectiveness of an outpatient Multidisciplinary Stroke Clinic model (referred to as the Clinic) for the clinical management of veterans with cerebrovascular disease. We include an assessment of: 1) clinical care, 2) patient satisfaction, 3) primary care provider satisfaction, and 4) Veteran Affairs (VA) costs.
Methods
We used the Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines in the preparation of this Clinic program evaluation.14 The SQUIRE guidelines were developed as a standard for reporting quality improvement studies in health care.
Setting and patients
The Clinic program was a clinic within the VA Connecticut Healthcare System. All patients cared for by the Clinic program received outpatient care for cerebrovascular disease and/or cerebrovascular risk factors. Most patients received primary care from one of the VA Connecticut Healthcare System’s primary care clinics. However, some patients were from VA Connecticut outpatient clinics and other veterans received primary care from VA sites in other states: Rhode Island, New Hampshire, and Maine.
The intervention: the Clinic program
Rationale
The Clinic program was designed as an outpatient clinical program, not as a research project. The VA Connecticut Healthcare System had robust primary care and general neurology services in place, and this new program was designed to complement the existing services to deliver nuanced medical care to the most complex patients with cerebrovascular disease. Specifically, the program was designed to ensure that patients who were hospitalized with a stroke received appropriate post-discharge care and that patients with a history of stroke or cerebrovascular risk factors received optimal care in the outpatient setting.
Program description
In this Clinic, patients were evaluated by staff from nursing, health psychology, physical therapy, internal medicine, and neurology in a single afternoon. Each patient’s case was discussed by all of the providers, who then developed and implemented a multidisciplinary care plan. Clinic providers reviewed the plan with patients and caregivers in person and communicated the plan with the primary care clinicians via the VA’s electronic medical record.
Patients received standardized screenings and assessments every visit to the Clinic (Table 1). Patients and their caregivers were encouraged to attend monthly support groups and educational sessions about stroke and stroke risk factors. Nursing staff helped patients complete the screening questionnaires, performed bilateral arm and orthostatic blood pressure (BP) measurements, and obtained ankle brachial indices. Health psychology staff conducted a brief cognition evaluation that: focused upon memory; screened for affective disorders (eg, depression), social isolation, stress, pain, tobacco use, alcohol or substance abuse; and inquired about exercise and diet. The physical therapist assessed functional status, equipment needs, and fall risk, and queried about exercise and made recommendations as appropriate. Clinicians from internal medicine and neurology performed medical histories and physical examinations. Residents in internal medicine and neurology as well as post-doctoral fellows in health psychology rotated through the Clinic weekly. A general internist and a stroke neurology attending supervised the Clinic.
Table 1.
Standardized screenings and assessments for patients and caregivers
| Patients | Caregivers |
|---|---|
| History | |
| Difficulties taking medications | Caregiving tasks |
| Number of blood pressure medications | Caregiver burden |
| Habits: self-report exercise, tobacco | Resources needed |
| Stroke knowledge | Self-reported health |
| Swallowing difficulties | |
| Sexual functioning problems | |
| Falls history | |
| Assessments and clinical tests | |
| Functional status (Functional Independence Measure)20,21 | Depression (Patient Health Questionnaire-2)19 |
| Blood pressure, manual reading (in supine, sitting, and standing) | |
| Ankle brachial index | |
| Depression (Patient Health Questionnaire-2)19 | |
| Cognition (Montreal Cognitive Assessment)18 | |
| Stroke severity (NIH Stroke Scale)16,17 | |
| Daytime sleepiness (The Epworth Sleepiness Scale)24 | |
| Pain, self-report 0–10 Numeric Rating Scale25 | |
| LDL-cholesterol | |
| Hemoglobin A1c |
Abbreviations: LDL, low-density lipoprotein; NIH, National Institute of Health.
Patients
Veterans were referred to the Clinic if they had cerebrovascular disease (eg, stroke or transient ischemic attack [TIA]) or cerebrovascular risk factors (eg, carotid stenosis). Because the VA Connecticut Healthcare System also had a general neurology clinic that provided ongoing care to veterans post-stroke, the patients who were most likely to be referred to the Clinic where those who were: thought to require care from multiple services (eg, stroke patients with concomitant affective disorders); might benefit from coordinated care (eg, frail stroke patients with concomitant medical and neurological needs); when clinical questions crossed traditional specialty boundaries (eg, anticoagulation management in patients with intracerebral hemorrhage); and/or when patients with stroke or TIA were being discharged from the hospital but who were not already enrolled in VA Primary Care. The patients seen in the Clinic were therefore, in general, more complex (eg, greatest disease severity and greatest comorbidity burden) than patients cared for in the general neurology clinic.
Planning the study of the intervention
This program evaluation was designed as a general evaluation of the effectiveness of the Clinic, including the following four domains: 1) clinical care, 2) patient satisfaction, 3) primary care provider satisfaction, and 4) VA costs. Data were collected in two manners: retrospectively for the chart review-based clinical care and economic evaluations, and cross-sectionally for the satisfaction surveys. The external audits of the medical records were performed by someone not associated with the Clinic (JK). Moreover, an external program evaluator implemented the patient and provider satisfaction surveys and interviews (EJM).
Methods of evaluation
Clinical care evaluation
We conducted a complete medical record review of all of the patients cared for in the Clinic during the period 2002–2005 (n = 162). This was completed in order to describe the patient characteristics and the management recommendations that were made at the time of the first Clinic visit. No data were excluded from analyses based on number of visits or demographics; however, some analyses included only people with more than one visit.
Patient characteristics included: demographics, past medical history, and social history (including tobacco, alcohol, exercise, and diet). Medication data included: the number of antihypertensive medications; the World Health Organization (WHO)-defined daily dose (DDD);15 antihypertensive agents; and any medication (antihypertensive and other medication classes) additions, deletions, or dose changes. Physical examination data included: BP; presence of orthostasis; ankle-brachial index (ABI); and stroke severity measured by the National Institute of Health Stroke Scale (NIHSS).16,17 Laboratory data included low- density lipoprotein (LDL)-cholesterol and glycosylated hemoglobin (HbA1c) values. Cognition was assessed using the Montreal Cognitive Assessment18 and was categorized as normal or impaired. Depression was screened for by using the PHQ-2 and was also categorized as normal or impaired.19 Fall risk was measured using: a fall history, direct observation of mobility, and focused physical examination by the physical therapist. Fall risk was classified as present or absent. Functional status was measured using the functional independence measure (FIM).20,21
Caregivers (when present) were asked to complete a questionnaire that included items regarding basic caregiver demographics, care provided to the patient (including activities of daily living [ADLs] and instrumental activities of daily living [IADLs]), and caregiver depression, self-reported health status, and burden.
To determine the clinical effectiveness of the Clinic, we evaluated the change in patient outcomes for patients with either a stroke or TIA. We compared the first and last visit scores for: LDL-cholesterol, HbA1c, number of antihypertensive medications and the WHO DDD for anti-hypertensive medications, existence of orthostasis (defined as systolic pressure decreased by 20 mm Hg or diastolic pressure decreased by 10 mm Hg or orthostatic symptoms, systolic and diastolic BP, stroke severity (NIHSS), functional status (FIM), depression, pain, cognition, and frequencies of exercising and smoking. To evaluate the change in antihypertensive medications, we included all of the patients with stroke or TIA cared for in the Clinic during the study period. For the rest of the clinical effectiveness analyses we included only patients who attended the Clinic on more than one occasion. Management recommendations were evaluated by measuring the number and type of: 1) new diagnoses that were made by the Clinic team, 2) tests or procedures that were ordered, 3) referrals made to other services, and 4) assistive devices that were issued or ordered.
Patient satisfaction survey
Patients who visited the Clinic during the period July 2002–August 2004 were contacted at least three times to participate in a patient satisfaction survey. Multiple attempts were made via phone call and mailed letter to contact patients for this survey. The survey was an in-person or by-telephone 42-item survey that included both open-ended questions and questions with Likert-scale responses. The survey was used to assess the patients’ satisfaction with their clinical care. Specifically, we asked if the patients liked the clinic, whether they valued being evaluated by multiple disciplines at one session, and whether they understood why the visit took a whole afternoon, as opposed to the usual 30 minute clinic visit. The survey was also used to assess the stroke educational programs and hence included questions about stroke risk factors and stroke warning signs.
Primary care provider survey
The primary care provider survey sought to assess providers’ opinions regarding satisfaction with clinical services, clinical management recommendations, and with the communication between the Clinic and the provider.
Cost assessment
The authors of the Heart Disease Stroke Statistics 2011 Update indicate stroke and cardiovascular disease to be a continued high cost disease, with spending near US$300 billion a year.1 We therefore conducted two economic evaluations of the Clinic. For these evaluations, we used total annual VA health care costs (including inpatient, outpatient, physician, pharmacy, procedure, and other costs). First, among patients who had been seen in the Clinic in fiscal year 2003 who had 2 years of cost data before their first Clinic visit (2001–2003) and 2 years of cost data after their Clinic visit (2003–2005), we compared the trend in costs before versus after being seen in the Clinic.
Second, among all patients who had been admitted to the VA Connecticut Healthcare System, West Haven Medical Center for an ischemic stroke (based on discharge diagnosis International Classification of Disease (ICD-9-CM) codes 434.X and 436) in the period 2002–2005, we compared the post-discharge total annual health care costs for those veterans who were cared for in the Clinic versus those who were not cared for in the Clinic.
Ethical issues
Human subjects approval was received.
Statistical analysis
All statistical analyses were completed with SAS (version 9.1; SAS Institute Inc., Cary, NC). Descriptive statistics were used to describe the baseline characteristics of the patients cared for in the Clinic, the clinical care evaluation, the patient satisfaction survey, the primary care provider survey, and the caregiver questionnaire. We used paired t-tests for continuous data and chi-square or Fisher’s exact tests for ordinal data, to compare outcomes between first and last visits. For the cost assessment, we used the Wilcoxon’s rank-sum test to compare the median costs of patients who were cared for in the Clinic versus patients who were not cared for in the Clinic.
Results
The demographic and stroke characteristics of the first 162 consecutive patients cared for in the Clinic are presented in Table 2. The average age was 69 (± 11) years, most of the veterans were male (97%) and white (72%), and the majority had a history of stroke (68%). Patients had multiple comorbidities, with 70 (43%) having six or more comorbidities.
Table 2.
Patient baseline characteristics and changes to care
| Patient characteristic | N = 162 |
|---|---|
| Age (years), range 44–100, mean ± SD | 69 ± 11 |
| Male gender: N (%) | 157 (97%) |
| Race, white | 117 (72%) |
| Primary diagnosis | |
| Stroke | 110 (68%) |
| Transient ischemic attack | 31 (19%) |
| Carotid stenosis | 30 (19%) |
| Other | 31 (19%) |
| Functional Independence Measure score, range 27–126 (n = 137) | 106.47 ± 20.614.0 |
| National Institute of Health Stroke Scale score, range 0–14, mean ± SD | 2.5 ± 3.4 |
| Total number of Stroke Clinic visits per patient | |
| 1 | 94 (58%) |
| 2 | 41 (25%) |
| ≥3 | 27 (17%) |
| Number of comorbid conditions | |
| 1 | 2% |
| 2 or 3 | 16% |
| 4 or 5 | 39% |
| ≥6 | 43% |
| Comorbid conditions | |
| Stroke | 108 (67%) |
| Transient ischemic attack | 37 (23%) |
| Hypertension | 130 (80%) |
| Hyperlipidemia | 105 (65%) |
| Ischemic heart disease | 66 (41%) |
| Depression | 57 (35%) |
| Diabetes mellitus | 47 (29%) |
| Prostatic hypertrophy | 36 (22%) |
| Peripheral vascular disease | 33 (20%) |
| Peptic ulcer disease | 31 (19%) |
| Congestive heart failure | 16 (10%) |
| Sleep apnea | 14 (9%) |
| New symptom or diagnosis | |
| Impaired cognition | 88 (54%) |
| Pain | 64 (40%) |
| Depression | 56 (35%) |
| Impaired sexual functioning | 45 (28%) |
| Fall risk | 60 (37%) |
| Falls | 29 (18%) |
| Dysphagia | 25 (15%) |
| Obstructive sleep apnea | 12 (7%) |
| Osteopenia/osteoporosis | 10 (6%) |
| Peripheral neuropathy | 9 (6%) |
| Clinical care changes | |
| Service referral made | 90% |
| Any rehabilitation | 64 (40%) |
| Any psychological therapy | 32 (20%) |
| BP clinic | 39 (21%) |
| Primary care clinic | 16 (10%) |
| Smoking cessation | 22 (14%) |
| Pulmonary/sleep study | 51 (31%) |
| Diagnostic testing ordered | 88% |
| Equipment issued | 48% |
| Medication information | |
| Medications added | 71 (44%) |
| Contraindications to a medication present | 48 (30%) |
| Medication dose changed | 43 (27%) |
| Medications discontinued | 25 (15%) |
| Able to name a stroke sign or symptom at last visit | 10% |
Abbreviations: BP, blood pressure; SD, standard deviation.
Forty-five caregivers completed the caregiver questionnaire; their average age was 62.6 (± 14) years. Fifty nine percent of the caregivers were married to the patient and 76% of the caregivers provided assistance with at least one ADL and IADL. On average, the caregivers provided assistance with 2.6 (± 2.7) ADLs and 3.3 (± 2.1) IADLs. Many caregivers reported feeling ‘satisfied’ with their caregiving experience (76%).
Clinical care evaluation
The number of visits to the Clinic ranged from one to six, but most patients visited the Clinic once (58%; Table 2). Demographics, stroke characteristics, and the changes in patients’ outcomes are provided in Table 3.
Table 3.
Selected Multidisciplinary Stroke Clinic outcomes, people with stroke or TIA
| Characteristic | Na | First visit | Last visit | P-value |
|---|---|---|---|---|
| History | ||||
| Number of BP medications at beginning of first visit, mean ± SDb | 140 | 1.53 (± 1.14)b | 1.74 (± 1.16)b | <0.001 |
| WHO DDD for BP medications at beginning of first visit, mean ± SDb | 140 | 1.87 (± 1.98)b | 2.01 (± 2.04)b | 0.001 |
| Increased exercise by last visit, yes, n (%) | 36 | 26 (72%) | ||
| Decreased frequency of smoking by last visit, yes, n (%) | 16 | 6 (40%) | ||
| Attempted to quit smoking by last visit, yes, n (%) | 16 | 12 (75%) | ||
| Successful in quitting smoking by last visit, yes, n (%) | 15 | 1 (7%) | ||
| At risk for falls, yes, n (%) | 21 | 16 (76%) | 17 (81%) | 0.707 |
| Assessments and clinical tests | ||||
| Functional Independence Measure, mean ± SD | 29 | 105.31 ± 19.98 | 105.76 ± 15.41 | 0.786 |
| Systolic blood pressure (mm Hg), mean ± SD | 58 | 137.21 ± 21.96 | 128.60 ± 19.80 | 0.007 |
| Diastolic blood pressure (mm Hg), mean ± SD | 58 | 77.88 ± 14.83 | 71.98 ± 10.20 | 0.004 |
| Orthostasis, yes, n (%)b | 24 | 6 (25%) | 4 (17%) | 0.035 |
| Depression, impaired, n (%) | 45 | 19 (42%) | 18 (40%) | 0.830 |
| Cognition, impaired, n (%)b | 45 | 31 (69%) | 26 (58%) | 0.274 |
| NIH Stroke Severity Scale, mean ± SD | 23 | 3.13 ± 3.24 | 3.00 ± 2.84 | 0.710 |
| Pain, present at time of initial clinic visit | 112 | 45 (40%) | ||
| LDL cholesterol (mg/dL), mean ± SD | 33 | 101.91 ± 23.10 | 180.61 ± 24.97 | 0.001 |
| Hemoglobin A1c (%), mean ± SD | 19 | 7.08 ± 1.36 | 6.95 ± 1.53 | 0.723 |
Notes:
Sample size changed accordingly for people with more than one visit;
Data regarding change from blood pressure medications from first visit only.
Abbreviations: BP, blood pressure; DDD, defined daily dose; LDL, low-density lipoprotein; NIH, National Institute of Health; SD, standard deviation; TIA, transient ischemic attack; WHO, World Health Organization.
Patients commonly received statistically significant increases in their antihypertensive regimens. Among patients with more than one Clinic visit, BP improved over time (Table 3). For example, the mean systolic BP decreased from the first visit (137.21 ± 21.96 mm Hg) to the last visit (128.60 ± 19.80 mm Hg; P = 0.007). Similarly, the mean diastolic BP decreased from the first visit (77.88 ± 14.83 mm Hg) to the last visit (71.98 ± 10.20 mm Hg; P = 0.004). Despite overall lowering in BP, fewer patients had orthostasis at the last visit 4/24 (17%) compared with the first visit 6/24 (25%; P = 0.035). Improvements were also observed in mean LDL-cholesterol values from the first visit (101.91 ± 23.10 mg/dL) to the last visit (80.61 ± 24.97 mg/dL; P = 0.001). Additionally, 72% of patients reported an increase in physical exercise by the last Clinic visit. Regarding cigarette smoking, 40% indicated a decrease in smoking, 75% reported an attempt to quit smoking, and 1 person (7%) was successful in smoking cessation by the last Clinic visit.
Many patients had a new medical problem identified during their first Clinic visit, including: impaired cognition (54%), depression (35%), and pain (40%) (Table 2). All of the patients had at least one major change recommended in their care management (Table 2); in half of the cases, this change was related to inadequate hypertension management (data not shown). Additionally, 88% had a diagnostic test ordered (eg, neuropsychiatry testing, nerve conduction velocity testing, noninvasive peripheral vascular studies, Holter monitor), 48% had equipment issued (eg, walker, home BP monitor), 44% had medications added, and 40% received an order for a new radiologic procedure. In 90% of cases, an unmet clinical need was identified which required referral for additional services (eg, consultation to rehabilitation or urology) (Table 2).
Patient satisfaction survey
A total of 110 patients were potentially eligible for participation in the patient satisfaction survey: eight had died, five declined, 47 were unable to be contacted, and 50 completed the survey (Table 4). All of the patients rated the overall quality of visit “good” or “excellent”; the mean reported appointment duration was 2.5 hours and 76% stated that the visit was “about the right length of time”; and 90% liked being seen by multiple specialists during the same appointment.
Table 4.
Patient satisfaction survey and primary care provider satisfaction survey
| Survey items | |
|---|---|
| Patient satisfaction | N = 50 |
| Age (years): mean | 69.2 |
| White | 92% |
| Overall quality of visit “good” or “excellent” | 100% |
| Clinic was “organized” (yes) | 100% |
| Staff were “courteous” (yes) | 100% |
| Average appointment time | 2.5 hours |
| Visit was “about the right length of time” (yes) | 76% |
| Liked being seen by multiple specialists during same appointment (yes) | 90% |
| Primary care provider satisfaction | N = 14 |
| Primary care providers with ≥1 patient seen in clinic | N = 35 |
| Number of responses | 14/35 (40%) |
| How helpful has the Clinic been in your management of patients? | Mean score: 4.5 |
| 1 = Very unhelpful, 2 = Somewhat unhelpful, 3 = Neutral, 4 = Somewhat helpful, 5 = Very helpful | |
| How would you rate the quality of communication provided by the Clinic regarding patients seen at the clinic (eg, notes, email)? | Mean score: 4.5 |
| 1 = Poor, 2 = Somewhat unsatisfactory, 3 = Just OK, 4 = Good, 5 = Excellent |
Primary care provider survey
Among the 35 primary care providers with at least one patient seen in Clinic, 40% participated in the survey. Qualitative responses to open-ended questions identified a positive attitude about the Clinic and its role in clinical management (Table 4).
Cost assessment
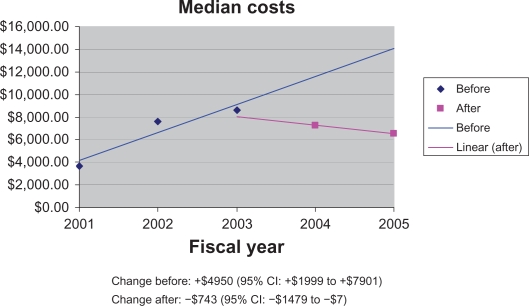
Among the 36 patients seen in the Clinic in 2003 who had health care cost data for the 2 years prior to and the 2 years after the visit, the trend in total VA health care costs before the first Clinic visit was +US$4950 (95% confidence interval [CI]: +US$1999 to +US$7901) and the trend after the Clinic visit was –US$743 (95% CI: –US$1479 to –US$7; see Figure 1).
Figure 1.
Median total health care costs before (2001, 2002, 2003) versus after Clinic use (2004, 2005). Currency = USD.
Abbreviation: CI, confidence interval.
Among all the veterans who were hospitalized for ischemic stroke at VA Connecticut, the median post-discharge total VA healthcare costs for patients cared for in the Clinic was US$13,876 compared with US$18,169 for the patients of comparable demographics and diagnoses who did not receive care in the Clinic (P = 0.26). While costs were not significantly different, we are able to see that the veterans in the Clinic had better care with improved outcomes at comparable costs.
Discussion
We found that this multidisciplinary outpatient model of stroke care effectively improved care and outcomes for patients with cerebrovascular disease and risk factors in a VA clinical setting. Improvements in care may have been due to the implementation of standard screening procedures that efficiently identified potential problems for patients. Certainly, the standard screening procedures resulted in the identification of new problem areas for the majority of patients.
Stroke clinics have traditionally been embedded in neurology clinics, and the evaluation of these programs have only demonstrated improved hypertension control.22 Allen et al demonstrated success with an initial post-stroke home assessment and team-based approach.22 There is little data about the use or effectiveness of a multidisciplinary approach to stroke care in the outpatient setting, particularly for more potentially complicated patients. In the Allen et al clinical program, one health care provider entered the home and completed all assessments, and the team evaluated the results of the home assessment, identified problems, and developed an individualized treatment plan. The treatment plan was then sent to the patient’s primary care provider who was responsible for new referrals and the patient’s overall health care. The program resulted in improvements across multiple domains including: neuromotor function, severe complications, quality of life, management of risk for common post-stroke complications and recurrent stroke, and stroke knowledge. Although the Multidisciplinary Clinic demonstrated improvements in several domains, responses to the patient education questions indicated that either our patient education program was not effective or the questions we used asking about stroke risk factors and stroke signs and symptoms were not well-understood by our patients.
Limitations
Several limitations require attention. First, the overall sample size was small, and there was a relatively poor response rate from providers and patients for the surveys. Patients or providers who were unhappy with the care may have been less likely to respond to the surveys; however, we received both positive and negative responses to the surveys, suggesting that at least some respondents felt comfortable providing constructive feedback. Second, we are not able to compare these study participants who did not receive care in this Clinic. Third, all care was provided at one clinical site from within the VA health care system. Such regional data are likely not representative of national patterns.23 Therefore these results may not be generalizable to other settings or to nonveteran populations or other national settings. Specifically, given that the VA uses an electronic medical record that allows for enhanced communication with primary care physician, these results may not be applicable to health care settings without an electronic medical record. Furthermore, the population analyzed was predominately white male. Finally, the patients cared for in the Clinic had many complex comorbidities; therefore, this sample may not represent the typical stroke population cared for in the outpatient setting.
Conclusion
A multidisciplinary outpatient stroke program can fill critical gaps in the care of veterans with cerebrovascular disease and improve outcomes without added costs. Given that the vast majority of VA medical centers have the staff who participated in this multidisciplinary program, it would be feasible to implement a multidisciplinary outpatient clinic across the spectrum of VA medical centers.
Acknowledgments
This project was supported by a Locally Initiated Project (LIP) grant from the Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) Stroke Quality Enhancement Research Initiative (QUERI) program. Dr Bravata was supported by an advanced career development award from the VA HSR&D Service and a Robert Wood Johnson Generalist Physician Faculty Scholars Award. Dr Schmid is supported by a career development award from the VA Rehabilitation Research and Development (RR&D CDA-2, D6174W). Service. The authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics – 2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Department of Veterans Affairs Stroke QUERI strategic plan. 2010. Available from http://www.queri.research.va.gov/about/strategic_plans/str.pdf. Accessed March 21, 2011.
- 3.Stineman MG, Maislin G, Fiedler RC, Granger CV. A prediction model for functional recovery in stroke. Stroke. 1997;28:550–556. doi: 10.1161/01.str.28.3.550. [DOI] [PubMed] [Google Scholar]
- 4.O’Sullivan SB. Stroke. In: O’Sullivan SB, Schmitz TJ, editors. Physical Rehabilitation: Assessment and Treatment. Philadelphia: FA Davis Company; 2001. pp. 519–582. [Google Scholar]
- 5.AHCPR . Clinical Practice Guidelines: Post-stroke Rehabilitation. US Department of Health and Human Services; 1995. [Google Scholar]
- 6.Han B, Haley WE. Family caregiving for patients with stroke – review and analysis. Stroke. 1999;30:1478–1485. doi: 10.1161/01.str.30.7.1478. [DOI] [PubMed] [Google Scholar]
- 7.Yates JS, Lai SM, Duncan PW, Studenski S. Falls in community-dwelling stroke survivors: an accumulated impairments model. J Rehabil Res Dev. 2002;39:385–394. [PubMed] [Google Scholar]
- 8.Kwan J, Sandercock P. In-hospital care pathways for stroke: a Cochrane systematic review. Stroke. 2003;34:587–588. doi: 10.1161/01.str.0000054673.28010.1b. [DOI] [PubMed] [Google Scholar]
- 9.Dow RS, Dick HL, Crowell FA. Failures and successes in a stroke program. Stroke. 1974;5:40–47. doi: 10.1161/01.str.5.1.40. [DOI] [PubMed] [Google Scholar]
- 10.Kasper EK, Gerstenblith G, Hefter G, et al. A randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. J Am Coll Cardiol. 2002;39:471–480. doi: 10.1016/s0735-1097(01)01761-2. [DOI] [PubMed] [Google Scholar]
- 11.Vliet Vlieland TP. Multidisciplinary team care and outcomes in rheumatoid arthritis. Curr Opin Rheumatol. 2004;16:153–156. doi: 10.1097/00002281-200403000-00015. [DOI] [PubMed] [Google Scholar]
- 12.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44:810–819. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 13.Joseph LN, Babikian VL, Allen NC, Winter MR. Risk factor modification in stroke prevention: the experience of a stroke clinic. Stroke. 1999;30:16–20. doi: 10.1161/01.str.30.1.16. [DOI] [PubMed] [Google Scholar]
- 14.Davidoff F, Batalden P, Stevens D, Ogrinc G, Mooney S. Publication guidelines for improvement studies in health care: evolution of the squire project. Ann Intern Med. 2008;149:670–676. doi: 10.7326/0003-4819-149-9-200811040-00009. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization Defined Daily Dose. 2009.
- 16.Albanese MA, Clarke WR, Adams HP, Jr, Woolson RF. Ensuring reliability of outcome measures in multicenter clinical trials of treatments for acute ischemic stroke. The program developed for the trial of org 10172 in acute stroke treatment (toast) Stroke. 1994;25:1746–1751. doi: 10.1161/01.str.25.9.1746. [DOI] [PubMed] [Google Scholar]
- 17.Lyden P, Brott T, Tilley B, et al. Improved reliability of the NIH Stroke Scale using video training. NINDS TPA Stroke Study Group. Stroke. 1994;25:2220–2226. doi: 10.1161/01.str.25.11.2220. [DOI] [PubMed] [Google Scholar]
- 18.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montréal Cognitive Assessment (MOCA): a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 19.Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (phq-2) J Psychosom Res. 2005;58:163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 20.The State University of New York . Guide for the uniform data set for medical rehabilitation, version 5.1. Buffalo: State Univ New York; 1997. [Google Scholar]
- 21.Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD. Performance profiles of the functional independence measure. Am J Phys Med Rehabil. 1993;72:84–89. doi: 10.1097/00002060-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Allen KR, Hazelett S, Jarjoura D, et al. Effectiveness of a postdischarge care management model for stroke and transient ischemic attack: a randomized trial. J Stroke Cerebrovasc Dis. 2002;11:88–98. doi: 10.1053/jscd.2002.127106. [DOI] [PubMed] [Google Scholar]
- 23.Andresen EM, Diehr PH, Luke DA. Public health surveillance of low-frequency populations. Annu Rev Public Health. 2004;25:25–52. doi: 10.1146/annurev.publhealth.25.101802.123111. [DOI] [PubMed] [Google Scholar]
- 24.Johns MW. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth sleepiness scale. Chest. 1993;103:30–36. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 25.Jensen M, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk D, Melzack R, editors. Handbook of Pain Assessment. New York: Guilford Press; 2001. pp. 15–34. [Google Scholar]