Abstract
In Nigeria, over 900,000 children under the age of five years die every year. Early neonatal death is responsible for a little over 20% of these deaths. Prematurity remains a significant cause of these early neonatal deaths. In some series, it is reported to be responsible for 60–70% of these deaths. This study aimed to determine the prevalence and determinants of pre-term deliveries at the University of Ilorin Teaching Hospital, Ilorin. This was a prospective cohort study conducted over a 9-month period at the University of Ilorin Teaching Hospital. Records of deliveries and data on maternal socio-biological and antenatal variables were collected during this period in order to determine the prevalence and determinants of pre-term deliveries. Out of the 2,489 deliveries that took place over a 9-month period, there were 293 pre-terms, giving a pre-term delivery rate of 120 per 1,000 deliveries. Of the total deliveries, 1,522 singleton deliveries that satisfied inclusion criteria were recruited; 185 of them were pre-term deliveries giving a case:control ratio of 1:7. Significant determinants of pre-term delivery identified were previous pre-term delivery (P=0.001; OR=3.55; 95% CI=1.71–7.30), antepartum hemorrhage (P=0.000; OR=8.95; 95%CI=4.06–19.78), premature rupture of the membranes (P=0.000; OR=6.48; 95%CI=4.33–9.67), maternal urinary tract infection (P=0.006; OR=5.89; 95%CI=1.16–27.57), pregnancy induced hypertension (P=0.007; OR=3.23; 95%CI=2.09–4.99), type of labor (P=0.000; OR=6.44; 95%CI=4.42–9.38) and booking status (P=0.000; OR=4.67; 95%CI=3.33–6.56). The prevalence of pre-term delivery was 120 per 1,000 live births. Factors significantly associated with pre-term delivery were low socio-economic class, previous pre-term delivery, antepartum hemorrhage, premature rupture of fetal membranes, urinary tract infection, pregnancy induced hypertension, induced labor, and booking elsewhere outside the teaching hospital.
Key words: pre-term, prevalence, deliveries, Ilorin, Nigeria.
Introduction
Pre-term deliveries remain a significant perinatal challenge, with pre-term babies accounting for 5–25% of all deliveries and up to 75% of all perinatal mortality in some series.1–3 While only 0.87% of all live births occur at a gestational age less than 31 weeks, births below this gestational age are responsible for 84% of the neonatal mortalities among infants of all gestational ages in the developed world.4 In Nigeria, pre-term babies account for 40–60% of all perinatal deaths.5–7
The survival of these pre-term infants is a function of both their biological maturity and technological advancement.8 The latter has continued to improve in most developed countries, with continuing progress in neonatal intensive care, shifting the limit of viability towards younger gestational ages, with greater than 80% survival at 28 weeks gestation.8–11 Such improvements are also being seen in some developing countries, especially in Asia with survival rates of 50–60% being recorded at 26–27 weeks gestation.12 The same cannot be said for most African countries with poor health infrastructure, heavy debt burden, conflicts and endemic poverty. A previous study in Benin City recorded mortality of 92.6% in babies of less than 28 weeks gestation.13
Thus, the most rational way of reducing the impact of these deliveries on neonatal mortality is by reducing their incidence. This will be guided by a proper understanding of the risk factors associated with these deliveries.
Many factors have been associated with these deliveries. These include history of previous pre-term birth, severe maternal hypertension, spontaneous pre-term rupture of fetal membranes, maternal age over fifty years, urinary tract infection, maternal anemia, maternal illness during pregnancy, previous abortion, nulliparity and low body mass index.14, 15–19 The direct cause is, however, usually not apparent.15 Most available data come from Europe, North America and Asia, with few data from Africa.14–19
Hence this study was conducted to estimate the prevalence of pre-term delivery and identify associated factors.
Materials and Methods
The study was conducted at the Maternity Hospital Wing of the University of Ilorin Teaching Hospital, Ilorin. This wing of the hospital provides secondary and tertiary health-care services in neonatology, obstetrics and gynecology. It attends to both booked and unbooked emergency cases. The annual delivery rate is 2,000 to 2,500. Deliveries are both vaginal (spontaneous and assisted) and operative. The neonatal intensive care unit (NICU) provides level II care to both inborn and outborn neonates. It admits between 1,000 and 1,200 patients annually.
This was a prospective cohort study conducted over nine months. All deliveries during the period of subject recruitment were recorded in order to provide a denominator for calculating the incidence of pre-term delivery and for use as controls in determining the maternal socio-biological characteristics associated with pre-term deliveries. All deliveries in the hospital during the study period were recruited, except those of mothers unsure of their LMP, those with discrepancy greater than two weeks between gestational age determined by LMP and that from Ballard assessment, and those with multiple gestations. Also excluded were those mothers whose babies had gross congenital malformations and those with post-term deliveries. Subjects were recruited consecutively once they fulfilled the inclusion criteria. Following recruitment, the subjects were grouped into pre-term and term babies. Pre-term babies were defined as those babies whose delivery occurred between gestational age 28 weeks and 37 completed weeks while term babies were those whose delivery occurred at or beyond a gestational age of 37 completed weeks but before 42 completed weeks.
A structured study proforma was completed by all subjects recruited. Data collected on maternal profile included maternal age, tribe, height, parity, antenatal status, ante-partum hemorrhage, previous pre-term delivery, previous abortion and drug intake during pregnancy. Data on weight at first antenatal care visit, packed cell volume and pregnancy induced or associated hypertension was obtained from the mother's hospital records. Socio-economic index scores were awarded to the subjects based on the occupations and educational attainments of their parents or caregivers using the Oyedeji socio-economic classification scheme.20
All recruited subjects were thoroughly examined to identify any congenital malformations. Two methods of estimating gestational age were employed; the date of the mother's last menstrual period (LMP) and the Ballard score.21 For uniformity, the gestational age derived from the Ballard score was used for analysis. Subjects were excluded when the mother was unsure of the date of her last menstrual period or when there was an irreconcilable discrepancy in the gestational age by LMP and Ballard of more than two weeks.
Data analysis
Data from the proforma were entered into a personal computer using SPSS version 15.0 for Windows software. The data was cleaned before analysis. Frequency distribution tables for variables were generated. Prevalence of pre-term delivery was determined. Potential determinants of prematurity were cross tabulated and odd ratios with their 95% confidence interval determined. χ2 test (with Yates correction where applicable) and Fisher's exact test were used to test for significance of the differences between categorical variables. The contribution of multiple independent variables to pre-term delivery were determined using linear regression analysis. Level of significance was put at P<0.05.
Results
A total of 2,489 women delivered 2,589 babies over a 9-month period. Of these, 2,025 (81.4%) of the women delivered at term, 293 (11.8%) delivered pre-term and 171 (6.8%) delivered post-term. Ninety-seven of the women who delivered pre-term had early pre-term deliveries.
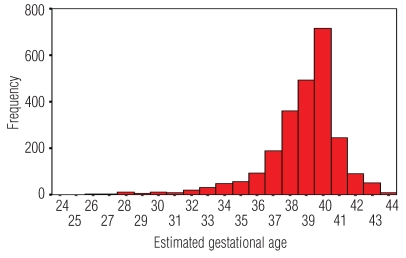
The pre-term delivery rate (<37 wks) was 120 per 1,000 deliveries. Early pre-term delivery rate (<34 wks) was 40 per 1,000 deliveries as shown in Figure 1.
Figure 1.
Distribution of all deliveries by estimated gestational age.
For the purpose of comparative analysis, a total of 1,522 subjects who met inclusion criteria were recruited into the study. One hundred and eighty-five of them were delivered pre-term and were recruited as subjects while 1,337 were term deliveries recruited as controls. The ratio of cases to controls is 1:7. This is to reflect the proportionate contribution of pre-term birth to the total delivery.
Of the various maternal socio-demographic characteristics studied as potential determinants of pre-term delivery, maternal age of 35 years or over, social class and parity were found to be significantly associated as shown in Table 1. Antenatal characteristics significant as determinants of pre-term delivery were previous pre-term delivery, febrile illness, antepartum hemorrhage, prolonged rupture of membrane and premature rupture of membrane. Others included urinary tract infection chorioamnionitis, pregnancy induced hypertension, type of labor and booking status as shown in Table 2.
Table 1. Maternal socio-demographic characteristics vs pre-term delivery.
| Parameter | Babies studied | Odd ratio | P | |
|---|---|---|---|---|
| Pre-term (%) | Term (%) | |||
| Age (years) | ||||
| <20 | 5 (16.7) | 25 (83.3) | 1.64 (0.48–4.46)! | 0.002* |
| 20–34 | 137 (10.9) | 1125 (89.1) | 1.91 (1.29–2.82)∧ | S |
| ≥35 | 43 (18.9) | 185 (81.1) | ||
| Social class | ||||
| Low(III,IV,V) | 103 (15.7) | 551 (84.3) | 1.82 (1.32–2.52) | 0.000* |
| High(I and II) | 80 (9.3) | 780 (90.7) | S | |
| Marital status | ||||
| Single | 5 (15.2) | 28 (84.8) | 1.30 (0.39–3.47) | 0.588# |
| Married | 180 (12.1) | 1309 (87.9) | NS | |
| Parity | ||||
| 0 | 5 (7.7) | 60 (92.3) | 0.64 (0.20–1.62)∼ | 0.001* |
| 1–4 | 154 (11.5) | 1184 (88.5) | 2.30 (1.40–3.76)° | S |
| ≥5 | 26 (23.0) | 87 (77.0) | ||
χ2 test;
Fisher's's exact test;
S, significant; NS, not significant;
Odd ratio for low maternal age;
Odd ratio for low maternal age;
Odd ratio for primiparity;
Odd ratio for grandmultiparity.
Table 2. Maternal antenatal and delivery characteristics vs pre-term delivery.
| Parameter | Babies studied | Odd ratio | P | |
|---|---|---|---|---|
| Pre-term (%) | Term (%) | |||
| Packed cell volume(%) | ||||
| <30 | 19 (8.2) | 212 (91.8) | 1.09 (0.62–1.92) | 0.745 |
| ≥30 | 62 (7.6) | 756 (92.4) | NS | |
| Previous abortion | ||||
| Yes | 53 (13.2) | 350 (86.8) | 1.14 (0.80–1.63) | 0.449* |
| No | 131 (11.7) | 987 (88.3) | NS | |
| Previous uterine curettage | ||||
| Yes | 31 (12.9) | 209 (87.1) | 1.09 (0.71–1.68) | 0.671* |
| No | 153 (11.9) | 1128 (88.1) | NS | |
| Previous pre–term delivery | ||||
| Yes | 13 (31.7) | 28 (68.3) | 3.55 (1.71–7.30) | 0.001# |
| No | 171 (11.6) | 1309 (88.4) | S | |
| Febrile illness | ||||
| Yes | 11 (22.9) | 37 (77.1) | 2.22 (1.05–4.62) | 0.020* |
| No | 174 (11.8) | 1300 (88.2) | S | |
| Antepartum hemorrhage | ||||
| Yes | 16 (53.3) | 14(46.7) | 8.95 (4.06–19.78) | 0.000# |
| No | 169 (11.3) | 1323(88.7) | S | |
| Prolonged rupture of membrane | ||||
| Yes | 43 (43.0) | 57 (57.0) | 6.80 (4.32–10.71) | 0.000* |
| No | 142 (10.0) | 1280 (90.0) | S | |
| Premature rupture of membrane | ||||
| Yes | 56 (40.0) | 84 (60.0) | 6.48 (4.33–9.67) | 0.000* |
| No | 129 (9.3) | 1253 (90.7) | S | |
| Urinary tract infection | ||||
| Yes | 4 (44.4) | 5 (55.6) | 5.89 (1.16–27.57) | 0.016# |
| No | 181 (12.0) | 1332 (88.0) | S | |
| Chorioamnionitis | ||||
| Yes | 6 (42.9) | 8 (57.1) | 5.57 (1.16–27.57) | 0.004# |
| No | 179 (11.9) | 1329 (88.1) | S | |
| Pregnancy induced hypertension | ||||
| Yes | 37 (27.8) | 96 (72.2) | 5.57 (1.57–18.50) | 0.000* |
| No | 148 (10.7) | 1241 (89.3) | S | |
| Type of labor | ||||
| Medically induced | 66 (38.4) | 106 (61.6) | 6.44 (4.42–9.38) | 0.000* |
| Spontaneous | 119 (8.8) | 1231 (91.2) | S | |
| Booking status | ||||
| Elsewhere | 84 (29.4) | 202 (70.6) | 4.67 (3.33–6.56) | 0.000* |
| UITH | 101 (8.2) | 1135 (91.8) | S | |
χ2 test;
Fisher's exact test;
S, significant; NS, not significant.
A linear regression analysis was carried out to exclude the relative contribution listwise of the identified significant determinants of pre-term delivery. Table 3 shows that after regression analysis, socio-economic class, previous pre-term delivery, antepartum hemorrhage, premature rupture of fetal membranes, urinary tract infection, pregnancy induced hypertension, type of labor and booking status remained significant. The model accounted for 19.6% of pre-term deliveries. Booking status was the strongest determinant of pre-term delivery.
Table 3. Linear regression of maternal socio-demographic and antenatal variables on pre-term deliveries.
| Beta coefficients | T | P | |
|---|---|---|---|
| Maternal age | −0.033 | −1.360 | 0.174 |
| Socio-economic class | −0.057 | −2.412 | 0.016 |
| Parity | −0.029 | −1.188 | 0.235 |
| Previous pre-term delivery | 0.081 | 3.488 | 0.001 |
| Febrile illness | 0.026 | 1.017 | 0.309 |
| Antepartum hemorrhage | 0.102 | 4.240 | 0.000 |
| Prolonged rupture of membranes | 0.051 | 1.285 | 0.199 |
| Premature rupture of membranes | 0.153 | 3.931 | 0.000 |
| Urinary tract infection | 0.066 | 2.746 | 0.006 |
| Chorioamnionitis | 0.013 | 0.480 | 0.632 |
| Hypertension in pregnancy | 0.068 | 2.702 | 0.007 |
| Type of labor | −0.167 | −6.408 | 0.000 |
| Booking status | −0.172 | −7.144 | 0.000 |
Discussion
The study has demonstrated that pre-term delivery remains a significant problem with a hospital based prevalence rate of 120 per 1,000 deliveries. This rate is higher than would be expected from a community based study because the study center is a tertiary center which attends to referrals from other primary and secondary centers. Most normal deliveries are taken in primary and secondary centers while more complicated deliveries, like pre-term labor, are referred to the teaching hospital. This reduces the denominator and thus exaggerates the pre-term delivery rate in teaching hospitals.
However, it is higher than pre-term delivery rates previously reported from Nigeria.13,22 Those reports were, however, from retrospective studies of admissions into the neonatal unit of a teaching hospital. These are not true estimates of pre-term delivery rate as many late unproblematic pre-term deliveries will not be admitted and thus, the absolute number of pre-term babies delivered will be under-reported. The absolute number of babies delivered will also be under-represented as many babies delivered without any problem will be discharged.
The prevalence rate reported in the current study was lower than those reported from Zimbabwe and Malawi.23,24 The study from Zimbabwe was also a hospital based study with a tendency for an exaggerated pre-term delivery rate while that of Malawi was a small community study in which the gestational age was allocated using second trimester ultrasound scan. The rate is, however, higher than the 5–10% reported by most European studies.3,25–29 Given the near 100% vital registration rate of most European countries, these rates will be similar to community based pre-term delivery rate. It is, however, similar to the 12.5% reported from the United States of America.29 The American report was also based on data from vital registration.
The current study identified many maternal socio-demographic and antenatal variables, including previous pre-term delivery, antepartum hemorrhage, premature rupture of membrane, urinary tract infection, pregnancy induced hypertension, type of labor and booking status, as determinants of pre-term delivery. The model used to identify the role of multiple independent variables on pre-term delivery could only account for 19% of the pre-term deliveries. This agrees with current knowledge that most cases of pre-term delivery are unexplained.15
Previous pre-term delivery was significantly associated with pre-term delivery in this study. Previous studies had demonstrated this association.14,17 This may be due to the persistence of unidentified factors in some women precipitating pre-term delivery.
The association between antepartum hemorrhage and pre-term delivery was also significant. In the current study, most of the women with antepartum hemorrhage were medically induced to deliver. Of all cases of antepartum hemorrhage among the subjects, 56.7% were medically induced to deliver. This was higher among pre-term subjects where 62.5% were medically induced to deliver.
Premature rupture of membranes, as in other studies,30,31 was identified as a determinant of pre-term delivery in the current study. It has also been associated with subclinical chorioamninitis30 and chlamydia vaginitis,31 both of which have also been associated with pre-term delivery. Its role is, therefore, inconclusive in that it is not clear whether premature rupture of membrane is the primary event that leads to pre-term delivery or whether there is an underlying problem like subclinical chorioamninitis that leads to both premature rupture of membrane and pre-term delivery. Subclinical chorioamnionitis can initiate labor by stimulating the production of interleukin-1.32 Interleukin-1 is known to indirectly serve as a signal for the initiation of labor in cases of intrauterine or systemic infection by inducing prostaglandin production by intrauterine tissues.33
Urinary tract infection was significantly associated with pre-term delivery. Urinary tract infection is favored by the morphological and functional changes that take place in pregnancy. Relative stasis of urine due to pregnancy-induced changes in the urinary tract is one such factor predisposing to urinary tract infection. Infection stimulates the production of cytokines among which is interleukin-1, a known stimulant of labor through the production of prostaglandins from uterine tissue.32,33 Previous studies have shown that urinary tract infection increases the risk of pre-term labour.15
Pregnancy induced hypertension has been associated with pre-term delivery in previous studies.17,19 This study also found an association between pregnancy induced hypertension and pre-term delivery. Reduced placental perfusion may be the mechanism that induces pre-term labor. Many patients with pregnancy induced hypertension, however, are medically induced to deliver either vaginally or operatively. In this study, 46.6% of all subjects with pregnancy induced hypertension were medically induced to deliver. This percentage increased to 75.7% among pre-term subjects with pregnancy induced hypertension. These associations were significant with a P value of less than 0.05. Thus, the role of pregnancy induced hypertension in pre-term delivery in this study has more to do with medical intervention than with a direct causal relationship.
Studies have shown that many pre-term deliveries are due to medical intervention either for maternal or fetal reasons26,34–35 and this is confirmed in this study. Those maternal reasons identified to be predominant causes of medical intervention in this study were pregnancy induced hypertension and antepartum hemorrhage. Booking status of subjects was also identified as the strongest determinant of pre-term delivery. A problem, with a potential to result in pre-term delivery, in a woman with a booked and well supervised pregnancy is likely to be detected early. Such a woman, with appropriate management, may have her pregnancy managed to term. A similar problem in a woman with a pregnancy that is either not booked or poorly supervised, will likely be identified late. This increases the chances of spontaneous or medically induced premature delivery. In this study, there was no significant difference between spontaneous and medically induced delivery among all recruited pre-term subjects based on booking status (P=0.531).
References
- 1.Demissie K, Rhoads GG, Ananth CV, et al. Trends in preterm birth and neonatal mortality among blacks and white in the United States of America from 1989 to 1997. Am J Epidemiol. 2001;154:307–15. doi: 10.1093/aje/154.4.307. [DOI] [PubMed] [Google Scholar]
- 2.Ezechukwu CC, Ugochukwu EF, Egbuonu I, Chukwuka JO. Risk factors for neonatal mortality in a regional tertiary hospital in Nigeria. Nig J Clin Pract. 2004;7:50–2. [Google Scholar]
- 3.Steer P. The epidemiology of preterm labour. Br J Obstet Gynaecol. 2005;112:1–3. doi: 10.1111/j.1471-0528.2005.00575.x. [DOI] [PubMed] [Google Scholar]
- 4.Usher R. Extreme prematurity. In: Avery GB, editor. Neonatology pathophysiology and management of the Newborn. Philadelphia: JB Lippincott(Publ); 1987. pp. 264–264. [Google Scholar]
- 5.Chike-Obi U. Preterm delivery in Ilorin; multiple and teenage pregnancies major aetiologic factors. West Afr J Med. 1993;12:228–30. [PubMed] [Google Scholar]
- 6.Njokanma OF, Olanrewaju DM. A study of neonatal deaths at the Ogun State University Teaching Hospital, Sagamu, Nigeria. J Trop Paediatr. 1995;98:155–60. [PubMed] [Google Scholar]
- 7.Njokanma OF, Sule Odu OA, Akesode FA. Perinatal mortality at the Ogun State University Teaching Hospital, Sagamu, Nigeria. J Trop Paediatr. 1994;40:78–81. doi: 10.1093/tropej/40.2.78. [DOI] [PubMed] [Google Scholar]
- 8.Breborowicz GH. Limit of fetal viability and its enhancement. Early Pregnancy. 2001;5:49–50. [PubMed] [Google Scholar]
- 9.Lorenz JM. The outcome of extreme prematurity. Semin Perinatol. 2001;25:348–59. doi: 10.1053/sper.2001.27164. [DOI] [PubMed] [Google Scholar]
- 10.Allen MC, Donohue PK, Dusman AE. The limit of viability-neonatal outcome of infants born at 22 to 25 weeks gestation. N Engl J Med. 1993;329:1597–601. doi: 10.1056/NEJM199311253292201. [DOI] [PubMed] [Google Scholar]
- 11.Dunn PM, Stirrat GM. Capable of being born alive? Lancet. 1984;1:553–5. doi: 10.1016/s0140-6736(84)90943-7. [DOI] [PubMed] [Google Scholar]
- 12.Sehgal A, Telang S, Passah SM, Jyothi MC. Maternal and neonatal profile and immediate outcome in extremely low birthweight babies in Delhi. Trop Doct. 2004;34:165–8. doi: 10.1177/004947550403400315. [DOI] [PubMed] [Google Scholar]
- 13.Ibhanesebhor SE, Afadapa MA. Epidemiology of preterm delivery in Benin City. Nig J Paediatr. 1996;23:27–32. [Google Scholar]
- 14.Mokuolu AO, Abdul IF, Adesiyun O. Maternal factors associated with early spontaneous singleton preterm delivery in Nigeria. Trop J Obstet Gynaecol. 2002;19:32–5. [Google Scholar]
- 15.Harlow BL, Frigoletto FD, Cramer DW, et al. Determinants of preterm delivery in low risk pregnancies. The RADIUS study group. J Clin Epidemiol. 1996;49:441–8. doi: 10.1016/0895-4356(95)00566-8. [DOI] [PubMed] [Google Scholar]
- 16.Olsen P, Laara E, Rantakallio P, et al. Epidemiology of preterm delivery in two birth cohorts with an interval of twenty years. Am J Epidemiol. 1995;142:1184–93. doi: 10.1093/oxfordjournals.aje.a117577. [DOI] [PubMed] [Google Scholar]
- 17.Wildschut HI, Petus TJ. Determinants of preterm birth in Curacao, Netherlands Antilles. Int J Gynaecol Obstet. 1991;36:23–7. doi: 10.1016/0020-7292(91)90173-3. [DOI] [PubMed] [Google Scholar]
- 18.Meda N, Soula G, Dabis F, et al. Risk factors in prematurity and intra uterine growth retardation in Burkina Faso. Rev Epidemiol Sante Publique. 1995;43:215–24. [PubMed] [Google Scholar]
- 19.Sehgal A, Telang S, Passah SM, Jyothi MC. Maternal and neonatal profile and immediate outcome in ELBW babies. Indian Pediatr. 2003;10:991–5. [PubMed] [Google Scholar]
- 20.Araoye MO. Subject selection and sample size determination. In: Araoye MO, editor. Research methodology with statistics for health and social sciences. Nathadex Publishers; 2003. pp. 115–20. [Google Scholar]
- 21.Ballard JL, Novak KK, Driver M. A simplified score for assessment of foetal maturity of newborn infants. J Pediatr. 1979;95:769–769. doi: 10.1016/s0022-3476(79)80734-9. [DOI] [PubMed] [Google Scholar]
- 22.Omene JA, Okolo AA, Imoedehme D, Omu AE. Trend in perinatal mortality rates at the University of Benin Teaching Hospital, Nigeria. East Afr Med J. 1984;61:461–9. [PubMed] [Google Scholar]
- 23.Feresu SA, Harlow SD, Welch K, Gillespie BW. Incidence of and sociodemographic risk factors for stillbirth, preterm birth and low birthweight among Zimbabwean women. Paediatr Perinat Epidemiol. 2004;18:154–63. doi: 10.1111/j.1365-3016.2003.00539.x. [DOI] [PubMed] [Google Scholar]
- 24.Van den Broek N, Ntonya C, Kayira E, et al. Preterm birth in rural Malawi: high incidence in ultrasound-dated population. Human Reprod. 2005;20:3235–7. doi: 10.1093/humrep/dei208. [DOI] [PubMed] [Google Scholar]
- 25.Bibby E, Stewart A. The epidemiology of preterm birth. Neuro Endocrinol Lett. 2004;25:43–7. [PubMed] [Google Scholar]
- 26.Morken NH, Kallen K, Hagberg H, Jacobsson B. Preterm birth in Sweden 1973–2001: rate, subgroups, and effect of changing patterns in multiple births, maternal age, and smoking. Acta Obstet Gynecol Scand. 2005;84:558–65. doi: 10.1111/j.0001-6349.2005.00765.x. [DOI] [PubMed] [Google Scholar]
- 27.Wisborg K, Henriksen TB, Hedegaard M, Secher NJ. Smoking during pregnancy and preterm birth. Br J Obstet Gynaecol. 1996;103:800–5. doi: 10.1111/j.1471-0528.1996.tb09877.x. [DOI] [PubMed] [Google Scholar]
- 28.Grjibovski AM, Bygren LO, Yngve A, Sjostrom M. Large social disparities in spontaneous preterm birth rates in transitional Russia. Public Health. 2005;119:77–86. doi: 10.1016/j.puhe.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 29.Donna LH, Mathews TJ, Menacker F, et al. Annual Summary of Vital Statistics: 2004. Pediatrics. 2006;117:168–83. doi: 10.1542/peds.2005-2587. [DOI] [PubMed] [Google Scholar]
- 30.Romero R, Sirtori M, Oyarzun E, et al. Infection and labour, V: Prevalence, microbiology and significance of intraamniotic infection in women with preterm labour and intact membrane. Am J Obstet Gynaecol. 1989;161:817–24. doi: 10.1016/0002-9378(89)90409-2. [DOI] [PubMed] [Google Scholar]
- 31.Martin DH, Koutsky L, Eschenbach DA, et al. Prematurity and perinatal mortality in pregnancy complicated by maternal Chlamydia trachomatis infection. JAMA. 1982;247:1585–8. [PubMed] [Google Scholar]
- 32.Buckley Rebecca H. The T-, B-, and NK-Cell Systems. In: Behrman RE, Kliegman RM, Jenson HB, editors. INelsons Textbook of Paediatrics. 17th edition. WB Saunders Co (Publ); 2004. pp. 683–700. [Google Scholar]
- 33.Romero R, Mazor M, Wu YK, et al. Infection in the pathogenesis of preterm labour. Semin Perinatol. 1988;12:262–79. [PubMed] [Google Scholar]
- 34.Philip Steer, Caroline Flint. ABC of labour care: Preterm labour and premature rupture of membranes. Br Med J. 1999;318:1059–62. doi: 10.1136/bmj.318.7190.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ananth CV, Vintzileos AM. Maternal-fetal conditions necessitating a medical intervention resulting in preterm birth. Am J Obstet Gynaecol. 2006;195:1557–63. doi: 10.1016/j.ajog.2006.05.021. [DOI] [PubMed] [Google Scholar]