Abstract
Hypoxia during exercise augments blood flow in active muscles to maintain the delivery of O2 at normoxic levels. However, the impact of hyperoxia on skeletal muscle blood flow during exercise is not completely understood. Therefore, we tested the hypothesis that the hyperemic response to forearm exercise during hyperbaric hyperoxia would be blunted compared with exercise during normoxia. Seven subjects (6 men/1 woman; 25 ± 1 yr) performed forearm exercise (20% of maximum) under normoxic and hyperoxic conditions. Forearm blood flow (FBF; in ml/min) was measured using Doppler ultrasound. Forearm vascular conductance (FVC; in ml·min−1·100 mmHg−1) was calculated from FBF and blood pressure (in mmHg; brachial arterial catheter). Studies were performed in a hyperbaric chamber with the subjects supine at 1 atmospheres absolute (ATA) (sea level) while breathing normoxic gas [21% O2, 1 ATA; inspired Po2 (PiO2) ≈ 150 mmHg] and at 2.82 ATA while breathing hyperbaric normoxic (7.4% O2, 2.82 ATA, PiO2 ≈ 150 mmHg) and hyperoxic (100% O2, 2.82 ATA, PiO2 ≈ 2,100 mmHg) gas. Resting FBF and FVC were less during hyperbaric hyperoxia compared with hyperbaric normoxia (P < 0.05). The change in FBF and FVC (Δ from rest) during exercise under normoxia (204 ± 29 ml/min and 229 ± 37 ml·min−1·100 mmHg−1, respectively) and hyperbaric normoxia (203 ± 28 ml/min and 217 ± 35 ml·min−1·100 mmHg−1, respectively) did not differ (P = 0.66–0.99). However, the ΔFBF (166 ± 21 ml/min) and ΔFVC (163 ± 23 ml·min−1·100 mmHg−1) during hyperbaric hyperoxia were substantially attenuated compared with other conditions (P < 0.01). Our data suggest that exercise hyperemia in skeletal muscle is highly dependent on oxygen availability during hyperoxia.
Keywords: skeletal muscle blood flow
during dynamic exercise there is an increased metabolic demand that is matched closely by increases in skeletal muscle blood flow and O2 delivery. In conditions in which O2 availability is compromised, such as hypoxia, there is local vasodilation and an increased blood flow that ensures delivery of O2 to respiring tissues under metabolic stress. The combination of the two conditions (hypoxia and exercise) elicits a greater vasodilator response and thus an augmented blood flow response (3, 5, 6, 24, 25, 34, 35). The augmented hypoxic exercise hyperemia is proportional to the hypoxia-induced fall in arterial O2 content, thus preserving muscle O2 delivery and ensuring it is matched to demand.
Conversely, under hyperoxic conditions muscle blood flow at rest in humans is reduced (2, 13, 22, 37). Moreover, there is some evidence that suggests that muscle blood flow is reduced during and after hyperoxic exercise compared with normoxic conditions (11, 22, 31). Reich and colleagues (22) demonstrated that postexercise calf blood flow is reduced at hyperbaric pressures while breathing 100% O2. However, these findings are limited by the delay (∼30 s) in blood flow measurements following contractions and the uncertain effects of increased atmospheric pressure per se. Measurements made during exercise (i.e., thermo- and dye-dilution techniques) have demonstrated that leg blood flow is reduced during leg kicking and cycle exercise when comparing normobaric hyperoxia [fraction of inspired O2 (FiO2) = 100% O2] with normobaric normoxia, without any difference in O2 consumption and delivery between the two conditions (11, 31). However, these studies only examined the leg blood flow response to small increases (< 10%) in arterial O2 content. Therefore, the aim of the current study was to investigate the blood flow response in the exercising forearm to larger increases in estimated arterial and venous O2 content via hyperbaric hyperoxia. We hypothesized that there will be a reduction in exercise blood flow that mirrors the estimated increase in O2 content.
METHODS
Subjects.
A total of eight young healthy subjects (7 men and 1 woman) volunteered to participate in the study. Subjects completed written, informed consent and were nonobese (body mass index < 28 kg/m2), nonsmokers, and not taking any medications. A detailed history and physical exam directed toward hyperbaric O2 therapy risks was performed by a board-certified Undersea and Hyperbaric Medicine Physician (P. L. Claus) before each subject's study day. Additionally, chest X-rays and a 12-lead electrocardiogram were performed as part of the standard screening procedures for exposure to hyperbaric oxygenation. Studies were performed after an overnight fast, and the subjects refrained from exercise and caffeine for at least 24 h before the study. The female subject was studied during the early follicular phase of the menstrual cycle. All study protocols were approved by the Institutional Review Board and were performed according to the Declaration of Helsinki.
Forearm exercise.
Subjects performed rhythmic forearm exercise with a handgrip device by the right arm at 20% of each subject's maximal voluntary contraction (mean, 44 ± 3 kg; and range, 25–57 kg), determined at the beginning of each experiment. The weight was lifted 4 to 5 cm over a pulley at a duty cycle of 1 s contraction and 2 s relaxation (20 contractions/min) using a metronome to ensure correct timing. The average weight used for forearm exercise was 8.8 ± 0.7 kg.
Arterial catheterization.
A 20-gauge, 5-cm catheter (model RA-04020, Arrow International, Reading, PA) was placed in the brachial artery of the exercising arm under aseptic conditions after local anesthesia (2% lidocaine) for measurement of arterial pressure and was continuously flushed (3 ml/h) with heparinized saline.
Heart rate and systemic blood pressure.
Heart rate (HR) was recorded via continuous three-lead ECG. A pressure transducer connected to the arterial catheter measured beat-to-beat blood pressure (Cardiocap/5, Datex-Ohmeda, Louisville, CO). Beat-to-beat stroke volume was calculated from the brachial arterial pulse pressure wave by model flow analysis. Model flow computes an aortic waveform based on nonlinear pressure-volume, pressure-compliance, and pressure-characteristic impedance equations, incorporating age, sex, height, and body mass (32). Cardiac output was calculated as the average stroke volume multiplied by the HR.
Forearm blood flow.
Brachial artery mean blood velocity was determined with a 4-MHz pulsed-Doppler probe (model 500 V, Multigon, Mt. Vernon, NY) proximal to the catheter insertion site. A linear 15-MHz Doppler ultrasound probe (M-Turbo, SonoSite, Bothell, WA) was placed immediately proximal to the velocity probe to measure brachial artery diameter. Brachial artery blood velocity was measured throughout each condition with a probe insonation angle of 60°. Brachial artery diameter measurements were obtained at end diastole between contractions during steady-state conditions. Forearm blood flow (FBF) was calculated as the product of mean blood velocity (in cm/s) and brachial artery cross-sectional area (in cm2) and expressed as milliliters per minute (ml/min).
Experimental protocol.
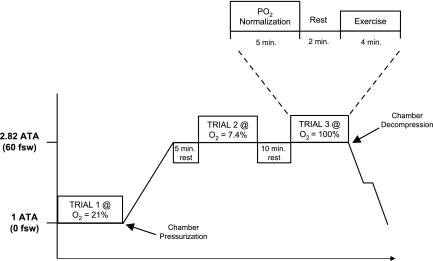
A schematic diagram of the general experimental design is illustrated in Fig. 1. Each trial included a Po2 normalization period (5 min), followed by a resting baseline condition (2 min), and then by rhythmic forearm exercise (4 min) at 20% maximal voluntary contraction. All studies were performed in a hyperbaric chamber at ∼1,000 ft above sea level with the subjects supine and consisted of three separate exercise trials. Ambient temperature in the hyperbaric chamber during the study trials was maintained at approximately thermoneutral with a climate control system.
Fig. 1.
Detailed hyperbaric exposure timeline. Hyperbaric exposure is shown in atmospheres absolute pressure (ATA) units. Trial 1 (normoxia) was performed at 1 ATA while breathing normoxic gas (air; 21% O2). Trials 2 and 3 took place at 2.82 ATA while breathing 7.4% and 100% O2, respectively. Breathing 7.4% O2 at a depth of 2.8 ATA is the equivalent to breathing room air at sea level and served as a “pressure control” trial. Breathing 100% O2 at a depth of 2.82 ATA served as the hyperoxic trial. Each trial consisted of a Po2 normalization period (5 min), rest (2 min), and exercise (4 min). fsw, feet of sea water.
Trial 1 was performed at 1 atmospheres absolute (ATA) (unpressurized chamber) while breathing normoxic gas (air) [21% O2; inspired Po2 (PiO2) ≈ 150 mmHg]. The hyperbaric chamber was then pressurized to 2.82 ATA over 5–10 min. Trial 2 was performed at 2.82 ATA while breathing hyperbaric normoxic gas (7.4% O2; PiO2 ≈ 150 mmHg). Trial 3 was performed at 2.82 ATA while breathing hyperoxic gas (100% O2; PiO2 ≈ 2,100 mmHg). Breathing 7.4% O2 at 2.82 ATA is equivalent to breathing air at 1 ATA and served as a pressure control trial to confirm that any changes in blood flow are independent of pressure changes. The 100% O2 at 2.82 ATA served as the hyperoxic trial and was used to study the blood flow response during markedly increased levels of arterial and venous O2 content. Inspired gas (air, 7.4% O2, and 100% O2) was supplied at ambient pressure via a tight-fitting, nonrebreathing, silicone oronasal mask connected to a demand regulator. The fit of the mask was adjusted by tightening the mask until no air leaks were apparent to the subject during inhalation against a closed valve. The total time of the hyperbaric exposure was limited to 49 min to prevent the need for decompression for study personnel who breathed air throughout the study. Additionally, 2.82 ATA was selected for chamber pressurization based on the time required (Fig. 1) to complete the exercise trials without the need for decompression for study personnel. The hyperbaric chamber was depressurized at a rate of 0.9 ATA min−1 while all personnel breathed 100% O2 with a 2-min safety (decompression) stop at 1.6 ATA.
Data analysis and statistics.
Data were collected at 200 Hz, stored on a computer, and analyzed off-line with signal processing software (WinDaq, DATAQ Instruments, Akron, OH). Mean arterial pressure (MAP) was determined from the brachial artery pressure waveform, and HR was determined from the electrocardiogram. FBF, arterial pressure, and HR were determined by averaging values from second minute of rest and the fourth minute of exercise. Forearm vascular conductance (FVC) was calculated as (FBF/arterial pressure) × 100 (expressed in ml·min−1·100 mmHg−1). To account for differences in resting FBF and FVC across trials, the change (Δ) in FBF and FVC (from rest to steady-state exercise) was calculated for each condition.
All values are expressed as means ± SE. To determine the effect of hyperoxia, differences in absolute FBF and FVC (at rest and during exercise) and ΔFBF and ΔFVC (from rest to exercise) were determined via repeated-measures ANOVA. Hemodynamic variables were compared via repeated-measures ANOVA to detect differences between responses during hyperoxia at rest and during exercise. Tukey post hoc analysis determined where statistical differences occurred. Statistical difference was set a priori at P < 0.05.
Estimated arterial O2 content (CaO2) was calculated under each condition as:
| (1) |
where SaO2 is arterial saturation, PaO2 is the partial pressure of arterial O2, 1.36 is the O2 capacity of hemoglobin, and 0.003 is the solubility of O2 in plasma. A hemoglobin value of 14 g/dl was used across trials and is based on average values observed in young male subjects from our previous studies (4–6). PaO2 values were derived from the Alveolar Air Equation:
| (2) |
where PB is the barometric pressure, PH2O is the water vapor pressure in the airways (47 mmHg), PaCO2 is the partial pressure of arterial CO2 (estimated to be 40 mmHg), and 0.8 represents the assumed respiratory quotient. The average PB on the study days was 733 ± 1 mmHg (range, 729–737), and this was used in the calculations of PaO2 for the normobaric trial. PB for the hyperbaric trials was consistent among all trials (2.82 ATA or 2,143 mmHg). The PaO2 was estimated from PAO2 based on a previously reported arterial-to-alveolar Po2 ratio of 0.9 (29). It is important to note that the arterial-to-alveolar Po2 ratio did not vary between normobaric normoxia and various levels of hyperbaric hyperoxia (1.2–3 ATA) in that study.
RESULTS
Seven (6 men and 1 woman) of the eight subjects completed the study protocol. One subject did not complete the protocol because of ear pain associated with the pressurization of the chamber. Those subjects completing the study were 25 ± 1 yr of age, 180 ± 4 cm in height, and 78 ± 4 kg in weight (body mass index, 24 ± 1 kg/m2).
Systemic hemodynamic responses.
The group data for systemic hemodynamic responses to combined forearm exercise and pressurization with each inspired O2 level are presented in Table 1. Resting HR was slightly lower at 2.82 ATA (for both 7.4 and 21% O2) compared with 1 ATA (P < 0.05). However, the change in HR from rest to exercise did not differ between trials (P = 0.20). Pressurization of the chamber to 2.82 ATA resulted in higher MAP at rest and during exercise. Hyperoxia (2.82 ATA at 100% O2) produced a greater increase in MAP during exercise compared with both the normoxia (1 ATA at 21% O2; P < 0.01) and hyperbaric normoxia (2.82 ATA at 7.4% O2; P < 0.05) trials. Cardiac output at rest (P = 0.75) and during exercise (P = 0.87) was not different between trials.
Table 1.
Systemic hemodynamic responses
| 1 ATA (21% O2) |
2.82 ATA (7.4% O2) |
2.82 ATA (100% O2) |
||||
|---|---|---|---|---|---|---|
| Rest | Exercise | Rest | Exercise | Rest | Exercise | |
| Heart rate, beats/min | 68 ± 1 | 68 ± 1 | 66 ± 1* | 68 ± 1 | 66 ± 1* | 66 ± 1*† |
| Mean arterial pressure, mmHg | 86 ± 2 | 90 ± 2 | 91 ± 3* | 94 ± 3* | 92 ± 2* | 98 ± 3*† |
| Cardiac output, l/min | 5.8 ± 0.2 | 5.8 ± 0.2 | 5.9 ± 0.3 | 5.9 ± 0.2 | 5.8 ± 0.2 | 5.8 ± 0.2 |
Values are means ± SE.
P < 0.05 vs. 1 atmospheres absolute (ATA) at 21% O2;
P < 0.05 vs. 2.82 ATA at 7.4% O2.
FBF and conductance.
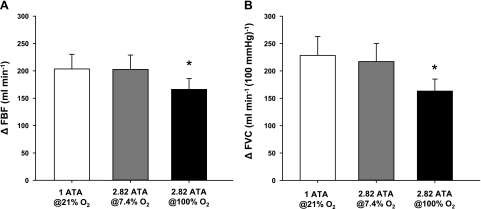
Presented in Table 2 are group data (means ± SE) forearm hemodynamics at rest and during exercise under each condition. FBF and FVC at rest and during exercise did not differ between normoxic (1 ATA at 21% O2) and hyperbaric normoxic (2.82 ATA at 7.4% O2) conditions. Hyperoxia (2.82 ATA at 100% O2) reduced resting FBF and FVC compared with hyperbaric normoxia (P < 0.05). Of particular interest to the current study, hyperoxic exercise caused a substantial reduction in FBF and FVC compared with the normoxic and hyperbaric normoxic exercise conditions (P < 0.01). The changes (Δ) in FBF and FVC (relative to resting values) were also reduced during hyperoxic exercise (Fig. 2, A and B).
Table 2.
Forearm hemodynamics at rest and with exercise during normoxia, hyperbaric normoxia, and hyperoxia
| 1 ATA (21% O2) |
2.82 ATA (7.4% O2) |
2.82 ATA (100% O2) |
||||
|---|---|---|---|---|---|---|
| Rest | Exercise | Rest | Exercise | Rest | Exercise | |
| Forearm blood flow, ml/min | 50 ± 12 | 254 ± 38 | 57 ± 12 | 261 ± 37 | 48 ± 10† | 214 ± 30* |
| Forearm vascular conductance, ml·min−1·100 mmHg−1 | 60 ± 16 | 288 ± 51 | 66 ± 17 | 284 ± 49 | 53 ± 12† | 217 ± 34* |
Values are means ± SE.
P < 0.01 vs. other exercise values;
P < 0.05 vs. 2.82 ATA at 7.4% O2.
Fig. 2.
Changes in forearm blood flow (ΔFBF) and forearm vascular conductance (ΔFVC) because of hyperoxic exercise. Rhythmic forearm exercise during hyperoxia (2.82 ATA at 100% O2; black bars) resulted in a reduced ΔFBF (A) and ΔFVC (B) compared with normoxic (1 ATA at 21% O2; white bars) and hyperbaric normoxic (2.82 ATA at 7.4% O2; gray bars) conditions. *P < 0.01 vs. normoxia and hyperbaric normoxia.
Estimated arterial O2 content.
The estimated PaO2 during the hyperbaric hyperoxia trial (1,773 mmHg) is substantially greater than during normobaric normoxia and hyperbaric normoxia trials (85 and 89 mmHg, respectively). The PaO2 during hyperbaric hyperoxia would result in a ∼25–30% increase in the estimated CaO2 compared with the other trials (24.4 vs. 18.9 ml O2/100 ml).
DISCUSSION
In the present study, we determined the impact of hyperbaric oxygenation on the blood flow and vasodilator response to rhythmic forearm exercise in young healthy adults. Our primary goal was to examine whether FBF and conductance would decrease in response to hyperoxic exercise to a similar magnitude to the increases previously observed during hypoxic exercise. The major observation in this study is that large increases in estimated systemic O2 content resulted in a substantial reduction in exercising FBF despite significantly higher perfusion pressures. Interestingly, the blunted ΔFVC during hyperoxic exercise (∼25% lower) mirrored the estimated increase in arterial O2 content (∼25–30%) in the present study. These findings parallel our previous findings in which hypoxic-mediated increases in ΔFVC during exercise mirrors the fall in O2 content (5, 6).
Previous attempts at examining the effect of hyperbaric O2 on exercising blood flow have been limited to measuring postexercise flows (via plethysmography). Along these lines, postexercise calf blood flow following foot ergometry under hyperbaric conditions (3 ATA at 100% O2) was shown to be significantly reduced (22). Studies that have examined blood flow responses to acute hyperoxia during dynamic exercise have been limited to small increases in PiO2 using 100% O2 under normobaric conditions. Kaijser (16) originally reported that arterial-venous O2 difference in the arm increased during hyperoxic exercise, thus suggesting a decreased muscle blood flow. However, FBF was not directly measured. Direct measurements of flow indicate that there is an ∼8–10% reduction in leg blood flow in response to a ∼10% increase in arterial O2 content during hyperoxic (FiO2 = 100% O2) exercise (9, 11, 31). As noted earlier, these findings are limited to small increases in O2 content. Therefore, our data are the first evidence to demonstrate that hyperbaric oxygenation decreases blood flow and vasodilation in active muscle groups during exercise.
Potential mechanisms for reduced blood flow during hyperoxic exercise.
A greater increase in MAP without a change in cardiac output and a reduction in FVC indicates that vascular resistance was increased during hyperoxic exercise (relative to the other trials). Hyperoxia reduces muscle sympathetic nerve activity at rest (14, 26, 37); however, the impact of hyperoxia during exercise is less clear. During isometric forearm exercise hyperoxia enhances metaboreflex sensitivity, which results in a greater sympathetic and blood pressure reactivity (14). However, hyperoxia does not appear to enhance the magnitude of change in sympathetic nerve activity to nonactive skeletal muscle during dynamic exercise (26). Therefore, it is unclear whether a greater amount of sympathetic vasoconstrictor activity contributed to the reduced FBF and vasodilation during hyperbaric exercise. Furthermore, we cannot rule out the possibility that increased O2 levels may have attenuated functional sympatholysis and therefore enhanced vasoconstriction in the contracting forearm (12). Finally, the increase in vascular resistance under hyperoxic exercise conditions may be a direct vasoconstrictor action of O2 on the arterial and arteriolar wall. Along these lines, some evidence suggests that the vascular response (i.e., constriction) to hyperoxia in the hindlimbs of dogs is not mediated by the autonomic nervous system but rather direct action of high arterial O2 tension (1).
A decreased release or responsiveness to local vasodilators within the contracting muscle under hyperoxic conditions could also promote a shift in the vasoconstrictor/vasodilator balance and consequently alter vascular tone. In this context, prostaglandin-mediated vasodilation following isometric exercise is reduced during hyperoxia (36). Additionally, vasoconstriction via a reduction in basal nitric oxide (NO) production has been observed in porcine coronary arteries exposed to elevated levels of O2 (21). Along the same lines, an increase in free radical production (i.e., superoxide anions) during hyperbaric oxygenation causes vasoconstriction in the cerebral circulation of rats via inactivation of NO (39). However, recent evidence suggests that NO metabolites are unaffected in humans during normobaric hyperoxic exercise (9).
Accumulating evidence suggests that erythrocytes have the ability not only to sense changes in O2 but also to modulate vascular tone (via release of ATP and/or NO), thus leading to appropriate changes in blood flow and matching O2 delivery with metabolic need (10). Under conditions of hemoglobin desaturation and mechanical deformation, ATP is released from erythrocytes and is thought to contribute to the augmented blood flow during hypoxic exercise (15, 27, 28). Therefore, an attenuated release of ATP in response to large increases in O2 may have blunted the blood flow response to exercise via these or related mechanisms.
Experimental considerations.
There are four potential limitations to our study that should be mentioned. First, in the present study, despite our efforts, we were unable to directly measure arterial and venous blood gases because of maximal Po2 limits (999 mmHg) of our commercially available arterial blood gas analyzers. Additionally, the blood gas analyzers are not able to be used in the hyperbaric chamber and blood samples obtained under pressure are subject to supersaturation and bubbling of O2 upon decompression for analysis, which can result in significant reading errors (7). Therefore, our estimated increase (∼25–30%) in arterial O2 content during hyperoxia is based on calculated values of arterial Po2 as described in methods. The estimated O2 tensions from the current study are similar to those previously reported using direct measurements of PaO2 (i.e., micro-O2 electrode or arterial blood sample) in subjects exposed to hyperbaric O2 (8, 19, 29, 30). Additionally, we were not able to calculate or determine whether O2 consumption in the active forearm was different between trials. However, previous studies have demonstrated that O2 consumption of an active limb is not different between normoxic and hyperoxic conditions (23, 31).
Second, the present study could not differentiate between changes in muscle and skin circulation. Along these lines, normobaric hyperoxia causes cutaneous vasoconstriction under resting normothermic conditions (38). However, the blood flow measured by Doppler techniques during normobaric forearm exercise is largely influenced by the active muscles rather than changes in skin circulation (18). Therefore, it is likely that the reduction in flow during hyperbaric hyperoxic exercise in the present study mainly reflects changes in skeletal muscle blood flow.
Third, the calculated cardiac output values in the present study did not differ between trials at rest or during exercise. These findings are in contrast to previous reports that suggest resting cardiac output is reduced during hyperbaric hyperoxia (17, 20, 30, 33). This discrepancy may be explained by the stroke volume being derived from the beat-to-beat brachial arterial pulse pressure wave using model flow analysis in the current study, whereas other studies have relied on thermal and indicator dilution methods. Along these lines, estimating cardiac output from pulse contour analysis may not be sensitive enough to detect changes and/or may not be accurate under the experimental conditions of the current protocol.
Finally, the trial order (normoxia vs. hyperoxia) used in the present study was not randomized. The effects of hyperbaric hyperoxia on the recovery of skeletal muscle blood flow following exercise (i.e., time to return to resting baseline values) are unknown. The time limits on the hyperbaric exposure to ensure safety prevented us for allowing for long (>10 min) recovery periods. Therefore, to minimize the effect of hyperoxia on subsequent trials, we performed the hyperbaric hyperoxic trial last in all studies. It is important to note that the blood flow and vasodilator responses during normoxic and hypoxic forearm exercise are highly reproducible across multiple trials and therefore the effect of not randomizing the interventions should have been minimal (4).
Conclusions.
This study demonstrates that hyperbaric oxygenation reduces FBF and vasodilation during rhythmic exercise in humans compared with normoxic and hyperbaric normoxic control conditions but that estimated O2 delivery remains constant. Taken together with our previous work, our data suggest that exercise hyperemia in skeletal muscle is highly dependent on O2 availability during hyperoxia as well as hypoxia.
GRANTS
This research was supported by the National Institutes of Health Research Grants AR-55819 (to D. P. Casey) and HL-46493 (to M. J. Joyner) and by Clinical and Translational Science Award RR-024150. The Caywood Professorship via the Mayo Foundation also supported this research.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
ACKNOWLEDGMENTS
We are grateful to the study volunteers for participating. We thank Maureen Bigelow, William Fuqua, Jon R. Balgeman, Branton Walker, Christopher Johnson, John Roger Shepherd, Nancy Meyer, and the Hyperbaric & Altitude Medicine staff for technical assistance.
REFERENCES
- 1.Bachofen M, Gage A, Bachofen H. Vascular response to changes in blood oxygen tension under various blood flow rates. Am J Physiol 220: 1786–1792, 1971 [DOI] [PubMed] [Google Scholar]
- 2.Bird AD, Telfer AB. The effect of oxygen at 1 and 2 atmospheres on resting forearm blood flow. Surg Gynecol Obstet 123: 260–268, 1966 [PubMed] [Google Scholar]
- 3.Calbet JA, Boushel R, Radegran G, Sondergaard H, Wagner PD, Saltin B. Determinants of maximal oxygen uptake in severe acute hypoxia. Am J Physiol Regul Integr Comp Physiol 284: R291–R303, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Casey DP, Curry TB, Wilkins BW, Joyner MJ. Nitric oxide-mediated vasodilation becomes independent of β-adrenergic receptor activation with increased intensity of hypoxic exercise. J Appl Physiol 110: 687–694, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casey DP, Madery BD, Curry TB, Eisenach JH, Wilkins BW, Joyner MJ. Nitric oxide contributes to the augmented vasodilatation during hypoxic exercise. J Physiol 588: 373–385, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casey DP, Madery BD, Pike TL, Eisenach JH, Dietz NM, Joyner MJ, Wilkins BW. Adenosine receptor antagonist and augmented vasodilation during hypoxic exercise. J Appl Physiol 107: 1128–1137, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cherry AD, Forkner IF, Frederick HJ, Natoli MJ, Schinazi EA, Longphre JP, Conard JL, White WD, Freiberger JJ, Stolp BW, Pollock NW, Doar PO, Boso AE, Alford EL, Walker AJ, Ma AC, Rhodes MA, Moon RE. Predictors of increased PaCO2 during immersed prone exercise at 4.7 ATA. J Appl Physiol 106: 316–325, 2009 [DOI] [PubMed] [Google Scholar]
- 8.Clark JM, Lambertsen CJ. Alveolar-arterial O2 differences in man at 0.2, 10, 20, and 35 Ata inspired Po2. J Appl Physiol 30: 753–763, 1971 [DOI] [PubMed] [Google Scholar]
- 9.Dufour SP, Patel RP, Brandon A, Teng X, Pearson J, Barker H, Ali L, Yuen AH, Smolenski RT, Gonzalez-Alonso J. Erythrocyte-dependent regulation of human skeletal muscle blood flow: role of varied oxyhemoglobin and exercise on nitrite, S-nitrosohemoglobin, and ATP. Am J Physiol Heart Circ Physiol 299: H1936–H1946, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ellsworth ML, Ellis CG, Goldman D, Stephenson AH, Dietrich HH, Sprague RS. Erythrocytes: oxygen sensors and modulators of vascular tone. Physiology 24: 107–116, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonzalez-Alonso J, Olsen DB, Saltin B. Erythrocyte and the regulation of human skeletal muscle blood flow and oxygen delivery: role of circulating ATP. Circ Res 91: 1046–1055, 2002 [DOI] [PubMed] [Google Scholar]
- 12.Hansen J, Sander M, Hald CF, Victor RG, Thomas GD. Metabolic modulation of sympathetic vasoconstriction in human skeletal muscle: role of tissue hypoxia. J Physiol 527: 387–396, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hansen M, Madsen J. Estimation of relative changes in resting muscle blood flow by 133Xe washout: the effect of oxygen. Scand J Clin Lab Invest 31: 133–139, 1973 [DOI] [PubMed] [Google Scholar]
- 14.Houssiere A, Najem B, Cuylits N, Cuypers S, Naeije R, van de Borne P. Hyperoxia enhances metaboreflex sensitivity during static exercise in humans. Am J Physiol Heart Circ Physiol 291: H210–H215, 2006 [DOI] [PubMed] [Google Scholar]
- 15.Jagger JE, Bateman RM, Ellsworth ML, Ellis CG. Role of erythrocyte in regulating local O2 delivery mediated by hemoglobin oxygenation. Am J Physiol Heart Circ Physiol 280: H2833–H2839, 2001 [DOI] [PubMed] [Google Scholar]
- 16.Kaijser L. Limiting factors for aerobic muscle performance. The influence of varying oxygen pressure and temperature. Acta Physiol Scand Suppl 346: 1–96, 1970 [PubMed] [Google Scholar]
- 17.Kenmure AC, Murdoch WR, Hutton I, Cameron AJ. Hemodynamic effects of oxygen at 1 and 2 Ata pressure in healthy subjects. J Appl Physiol 32: 223–226, 1972 [DOI] [PubMed] [Google Scholar]
- 18.Krix M, Weber MA, Krakowski-Roosen H, Huttner HB, Delorme S, Kauczor HU, Hildebrandt W. Assessment of skeletal muscle perfusion using contrast-enhanced ultrasonography. J Ultrasound Med 24: 431–441, 2005 [DOI] [PubMed] [Google Scholar]
- 19.McDowall DG, Ledingham IM, Tindal S. Alveolar-arterial gradients for oxygen at 1, 2, and 3 atmospheres absolute. J Appl Physiol 24: 324–329, 1968 [DOI] [PubMed] [Google Scholar]
- 20.McMahon TJ, Moon RE, Luschinger BP, Carraway MS, Stone AE, Stolp BW, Gow AJ, Pawloski JR, Watke P, Singel DJ, Piantadosi CA, Stamler JS. Nitric oxide in the human respiratory cycle. Nat Med 8: 711–717, 2002 [DOI] [PubMed] [Google Scholar]
- 21.Pasgaard T, Stankevicius E, Jorgensen MM, Ostergaard L, Simonsen U, Frobert O. Hyperoxia reduces basal release of nitric oxide and contracts porcine coronary arteries. Acta Physiol (Oxf) 191: 285–296, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Reich T, Tuckman J, Naftchi NE, Jacobson JH. Effect of normo- and hyperbaric oxygenation on resting and postexercise calf blood flow. J Appl Physiol 28: 275–278, 1970 [DOI] [PubMed] [Google Scholar]
- 23.Richardson RS, Grassi B, Gavin TP, Haseler LJ, Tagore K, Roca J, Wagner PD. Evidence of O2 supply-dependent V̇o2max in the exercise-trained human quadriceps. J Appl Physiol 86: 1048–1053, 1999 [DOI] [PubMed] [Google Scholar]
- 24.Roach RC, Koskolou MD, Calbet JA, Saltin B. Arterial O2 content and tension in regulation of cardiac output and leg blood flow during exercise in humans. Am J Physiol Heart Circ Physiol 276: H438–H445, 1999 [DOI] [PubMed] [Google Scholar]
- 25.Rowell LB, Saltin B, Kiens B, Christensen NJ. Is peak quadriceps blood flow in humans even higher during exercise with hypoxemia? Am J Physiol Heart Circ Physiol 251: H1038–H1044, 1986 [DOI] [PubMed] [Google Scholar]
- 26.Seals DR, Johnson DG, Fregosi RF. Hyperoxia lowers sympathetic activity at rest but not during exercise in humans. Am J Physiol Regul Integr Comp Physiol 260: R873–R878, 1991 [DOI] [PubMed] [Google Scholar]
- 27.Sprague RS, Ellsworth ML, Stephenson AH, Kleinhenz ME, Lonigro AJ. Deformation-induced ATP release from red blood cells requires CFTR activity. Am J Physiol Heart Circ Physiol 275: H1726–H1732, 1998 [DOI] [PubMed] [Google Scholar]
- 28.Sprague RS, Ellsworth ML, Stephenson AH, Lonigro AJ. Participation of cAMP in a signal-transduction pathway relating erythrocyte deformation to ATP release. Am J Physiol Cell Physiol 281: C1158–C1164, 2001 [DOI] [PubMed] [Google Scholar]
- 29.Weaver LK, Howe S. Normobaric measurement of arterial oxygen tension in subjects exposed to hyperbaric oxygen. Chest 102: 1175–1181, 1992 [DOI] [PubMed] [Google Scholar]
- 30.Weaver LK, Howe S, Snow GL, Deru K. Arterial and pulmonary arterial hemodynamics and oxygen delivery/extraction in normal humans exposed to hyperbaric air and oxygen. J Appl Physiol 107: 336–345, 2009 [DOI] [PubMed] [Google Scholar]
- 31.Welch HG, Bonde-Petersen F, Graham T, Klausen K, Secher N. Effects of hyperoxia on leg blood flow and metabolism during exercise. J Appl Physiol 42: 385–390, 1977 [DOI] [PubMed] [Google Scholar]
- 32.Wesseling KH, Jansen JR, Settels JJ, Schreuder JJ. Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol 74: 2566–2573, 1993 [DOI] [PubMed] [Google Scholar]
- 33.Whalen RE, Saltzman HA, Holloway DH, Jr, McIntosh HD, Sieker HO, Brown IW., Jr Cardiovascular and blood gas responses to hyperbaric oxygenation. Am J Cardiol 15: 638–646, 1965 [DOI] [PubMed] [Google Scholar]
- 34.Wilkins BW, Pike TL, Martin EA, Curry TB, Ceridon ML, Joyner MJ. Exercise intensity-dependent contribution of beta-adrenergic receptor-mediated vasodilatation in hypoxic humans. J Physiol 586: 1195–1205, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilkins BW, Schrage WG, Liu Z, Hancock KC, Joyner MJ. Systemic hypoxia and vasoconstrictor responsiveness in exercising human muscle. J Appl Physiol 101: 1343–1350, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Win TS, Marshall JM. Contribution of prostaglandins to the dilation that follows isometric forearm contraction in human subjects: effects of aspirin and hyperoxia. J Appl Physiol 99: 45–52, 2005 [DOI] [PubMed] [Google Scholar]
- 37.Yamauchi K, Tsutsui Y, Endo Y, Sagawa S, Yamazaki F, Shiraki K. Sympathetic nervous and hemodynamic responses to lower body negative pressure in hyperbaria in men. Am J Physiol Regul Integr Comp Physiol 282: R38–R45, 2002 [DOI] [PubMed] [Google Scholar]
- 38.Yamazaki F, Takahara K, Sone R, Johnson JM. Influence of hyperoxia on skin vasomotor control in normothermic and heat-stressed humans. J Appl Physiol 103: 2026–2033, 2007 [DOI] [PubMed] [Google Scholar]
- 39.Zhilyaev SY, Moskvin AN, Platonova TF, Gutsaeva DR, Churilina IV, Demchenko IT. Hyperoxic vasoconstriction in the brain is mediated by inactivation of nitric oxide by superoxide anions. Neurosci Behav Physiol 33: 783–787, 2003 [DOI] [PubMed] [Google Scholar]