Abstract
The rotator cuff musculature imparts dynamic stability to the glenohumeral joint. In particular, the balance between the subscapularis anteriorly and the infraspinatus posteriorly, often referred to as the rotator cuff “force couple,” is critical for concavity compression and concentric rotation of the humeral head. Restoration of this anterior-posterior force balance after chronic, massive rotator cuff tears may allow for deltoid compensation, but no in vivo studies have quantitatively demonstrated an improvement in shoulder function. Our goal was to determine if restoring this balance of forces improves shoulder function after two-tendon rotator cuff tears in a rat model. Forty-eight rats underwent detachment of the supraspinatus and infraspinatus. After four weeks, rats were randomly assigned to three groups: no repair, infraspinatus repair, and two-tendon repair. Quantitative ambulatory measures including medial/lateral forces, braking, propulsion, and step width were significantly different between the infraspinatus and no repair group and similar between the infraspinatus and two-tendon repair groups at almost all time points. These results suggest that repairing the infraspinatus back to its insertion site without repair of the supraspinatus can improve shoulder function to a level similar to repairing both the infraspinatus and supraspinatus tendons. Clinically, a partial repair of the posterior cuff after a two tendon tear may be sufficient to restore adequate function. An in vivo model system for two-tendon repair of massive rotator cuff tears is presented.
Introduction
Shoulder motion is dependent on a complex interplay of forces and moments around the glenohumeral joint. Because the shoulder lacks inherent bony restraint, the surrounding soft tissue and musculature provide much of the stability to the joint. In particular, the rotator cuff musculature imparts forces that, when balanced, provide the glenohumeral joint with adequate mobility and dynamic stability. The balance between the anterior subscapularis muscle and the posterior infraspinatus and teres minor muscles, often referred to as the rotator cuff “force couple”, has been proposed to be a critical component of this stability by providing concavity compression to the joint.1 Compression of the humeral head into the glenoid concavity provides a stable fulcrum for concentric rotation of the head in the glenoid.2–3 Even when the superior part of the rotator cuff musculature, the supraspinatus, is torn, this anterior-posterior force balance between the subscapularis and infraspinatus can provide concavity compression and resist superior translation of the head despite superior pull of the deltoid muscle during abduction.2; 4–5
Rotator cuff tears, among the most common musculoskeletal problems encountered in the aging population, 6–7 can cause disruption of normal shoulder kinematics by disrupting the force balance between the subscapularis and infraspinatus.1 Clinically, patients with irreparable rotator cuff defects can have preserved function,8–10 suggesting that a deficient cuff can be functionally intact if the integrity of the anterior-posterior force balance is maintained.11–12 However, if the tear progresses to involve the posterior cuff musculature, this balance of forces is often disrupted, concavity compression is lost, and a stable fulcrum for concentric rotation of the humeral head in the glenoid no longer exists.1; 13
Restoration of this anterior-posterior force balance in massive rotator cuff tears may allow for deltoid compensation and adequate arm elevation by the patient.1 However, these massive tears are often chronic in nature and characterized by fatty degeneration, tendon retraction and stiffening, and increased repair tension, making it difficult for the surgeon to adequately treat these tears.14–16 In vitro cadaver studies investigated the concept of a rotator cuff “force couple,”1; 13; 17–19 and clinical case series reported results on partial repair of only the infraspinatus after massive, two-tendon cuff tears20–21; these studies provide important information to our field. However, no in vivo studies have quantitatively demonstrated the importance of rotator cuff musculature balance or an improvement in shoulder function with partial repair of torn rotator cuff tendons in a controlled model system. Therefore, our objective was to use quantitative ambulatory measures in a rat rotator cuff model to determine if repair of the posterior cuff musculature and subsequent restoration of the balance of forces improves shoulder function after a chronic two-tendon rotator cuff tear. Our hypothesis was that restoring the balance of the anterior and posterior cuff forces by repair of the infraspinatus tendon only would be sufficient to improve shoulder function to a level similar to repairing both the supraspinatus and infraspinatus tendons.
Materials and Methods
Forty-eight adult Sprague-Dawley rats (400–450 g) were used in this study, which was approved by the University of Pennsylvania Institutional Animal Care and Use Committee. All rats underwent detachment of the supraspinatus and infraspinatus and were then allowed cage activity for 4 wks to simulate a chronic, massive two-tendon tear.22 After the 4 wks, the rats were randomly assigned to three groups based on treatment: no repair (n=16), infraspinatus only repair (n=16), and infraspinatus and supraspinatus repair (n=16), referred to as the “no repair,” “infraspinatus repair,” and “two-tendon repair” groups, respectively.
Detachment Technique
All procedures were performed on the left shoulder. With the arm in external rotation, a 2 cm skin incision was made, followed by blunt dissection down to the rotator cuff musculature. The rotator cuff was exposed, and the tendons were visualized at their insertion on the humerus. The supraspinatus was identified as the tendon passing underneath the acromion, and the infraspinatus was identified as the tendon posterior and inferior to the supraspinatus. Suture was passed under the acromion to apply upward traction for further exposure, and the supraspinatus was separated from the other rotator cuff tendons before sharp detachment at its insertion on the greater tuberosity using an 11-blade. A 5-0 nylon suture was used to mark the tendon edge, and the tendon was allowed to freely retract. The infraspinatus was detached and marked in a similar manner. The muscle incision was closed in a layered fashion, the skin was closed with staples, and the rats were allowed unrestricted cage activity.
Repair Technique
A surgical repair technique was developed to test the effects of one- and two-tendon repairs. This repair surgery was performed on the 28th day after detachment surgery. For all treatment groups, a similar dissection and exposure to approach the rotator cuff musculature was used, with increased medial dissection to allow for identification of retracted tendons. Any scar tissue or attachments between the tendon and insertion were removed regardless of treatment group. To recreate the supraspinatus and infraspinatus insertion sites, any remaining fibrocartilage at the insertion site was removed using a high-speed burr. Two crossing 0.5 mm drill holes were made through the humerus, with entrance and exit holes corresponding to the edges of the anatomic footprint of the supraspinatus and infraspinatus (Fig. 1). After the drill holes were created, the surgeon was notified of the treatment group.
Figure 1.
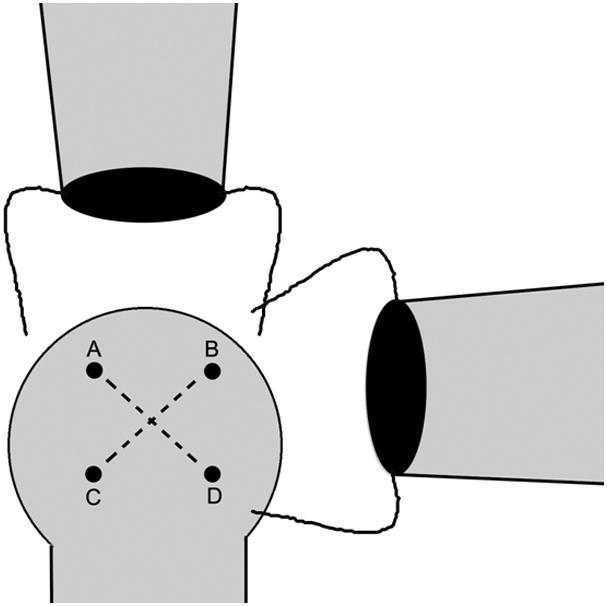
Surgical repair technique with crossed bone tunnels. Drill hole A represents the anterior footprint of the supraspinatus, B represents the intersection of the posterior supraspinatus and superior infraspinatus footprints, and D represents the inferior footprint of the infraspinatus. Drill hole C represents a point on the lateral humeral head roughly equidistant from points A and D. Holes are drilled from A to D then from B to C. The use of these bone tunnels and a modified Mason-Allen stitch allows for repair of both tendons to their respective anatomic footprints on the humeral head.
For a two-tendon repair, scar tissue was dissected until the supraspinatus and infraspinatus tendon edges were identified by the marking suture. Scar tissue surrounding the tendons was dissected to allow for mobilization of the tendon edge to the appropriate insertion site. The edges were grasped with a modified Mason-Allen technique using 4-0 braided polyester suture. The sutures were passed through the drill holes, and the tendons were reapposed to their insertion sites. Five suture knots were tied, and the incision was closed.
For the infraspinatus repair group, the technique was similar, including the bone tunnels, except that the supraspinatus was not dissected out or repaired back to its insertion site. For the no repair group, neither the suprapinatus nor the infraspinatus tendon edge was dissected free. However, to control for the trauma caused by the surgery, any scar tissue between the tendon and humeral head was removed, bone tunnels were drilled, and suture without any tendon attachments was passed through the bone tunnels and tied down.
Quantitative Ambulatory Assessment
Forelimb gait and ground reaction forces were quantified using an instrumented, stationary walkway as described previously.23 Briefly, two 6 degree-of-freedom force/torque cells (nano17, ATI Industrial Automation, Apex, NC) were mounted to clear, acrylic force plates and incorporated into a walkway. Mirrors were placed along the sides of the walkway, and a digital camera (A601 fc, Basler Vision Tech., Ahrensburg Germany) underneath the walkway captured ventral and sagittal (left and right) images of the animal at 60 frames-per-second.
Rats were acclimated to walk freely along the instrumented walkway over a period of 2 wks prior to formal recording of ambulatory data. For all groups, data were collected one day prior to detachment surgery to obtain average baseline, uninjured ambulatory values. Data were then collected at days −1 (1 d prior to repair surgery), 3, 7, 10, 14, 21, and 28 post-repair surgery. Kinetic data were analyzed using MATLAB (Version 7.7.0, MathWorks, Inc., Natick, MA).
Ground reaction force data were analyzed by using both ventral and sagittal views to determine when the left paw was in contact with the plate of interest. Medial/lateral (±x direction, respectively), braking (−y direction), propulsion (+y direction), and vertical (+z direction) forces were determined. At each time point, at least two walks were recorded per animal, along with the animal’s body weight. These parameters were averaged across walks on a given day for each animal and normalized to the animal’s body weight for that day.
Paw print analysis was achieved by creating a mask for each paw using the apex of each toe from calibrated ventral images. The step width was calculated by determining the centroids for the left and right forepaw. The step width reveals gait disturbances, with decreasing step width indicating the need for compensatory contralateral limb stabilization during gait. By moving the uninjured contralateral limb medially towards the center of the body or “tripoding,” the animal can compensate for lack of shoulder function on the injured side.24
Statistical analysis
All ground reaction force and step width data were compared using a one-way ANOVA followed by Fisher’s PLSD multiple comparison test to study the effect of group at each given time point. Because our objective was to determine the level of shoulder function after an infraspinatus only repair, comparisons of interest were infraspinatus repair to no repair, and infraspinatus repair to a two-tendon repair. Therefore, to correct for multiple comparisons, significance was set at p<0.025. Also, each kinetic parameter from each day post-repair was compared to the baseline, uninjured data using two-sided paired t-tests with significance set at p<0.05.
Results
Baseline kinetic data collected at day −1 were not significantly different between any of the groups for any ambulatory parameter.
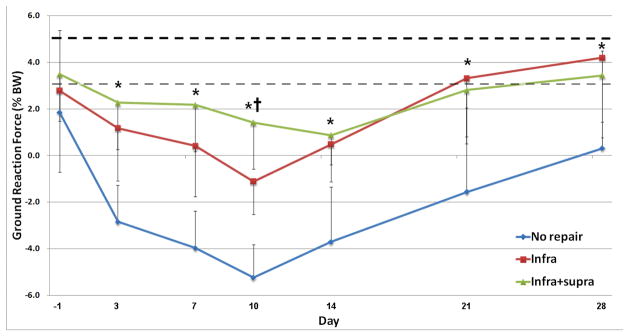
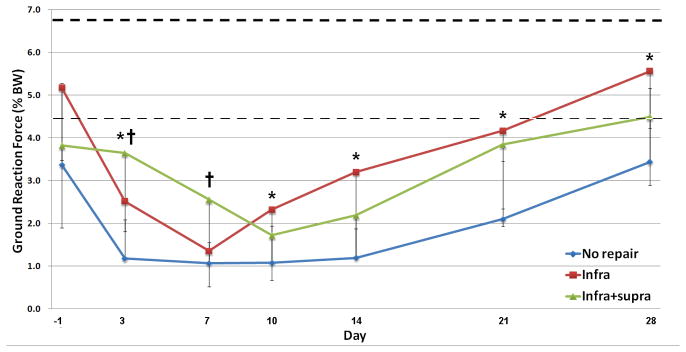
Medial/lateral forces were significantly different (p<0.001) between the no repair group and the infraspinatus repair group at all time points (Fig. 2A). No differences were seen between the infraspinatus only repair group and the two-tendon repair group at any time point except day 10. Rats in the infraspinatus and two-tendon repair groups placed predominantly medial forces on the affected extremity, while rats in the no repair group had larger lateral forces. Medial/lateral forces were not significantly different compared to baseline, uninjured values at days 21 and 28 in the infraspinatus only and two-tendon repair groups. The no repair group was significantly different than baseline values at all time points.
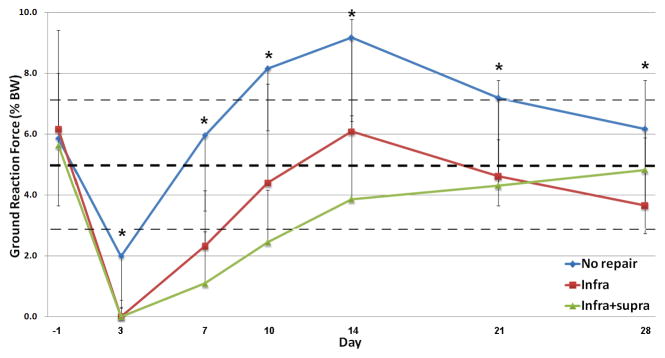
Figure 2.
(A) Medial/lateral, (B) braking, (C) propulsion, and (D) vertical ground reaction forces across the three groups showing significant differences between the infraspinatus repair group and no repair group at most time points, and similarities between the infraspinatus repair group and two-tendon repair group (*p<0.05 infraspinatus repair vs. no repair, †p<0.05 between infraspinatus repair vs. two-tendon repair). The thick dotted line represents average baseline values for all animals obtained before detachment surgery; the thin dotted line represents one standard deviation from the baseline average.
Braking forces were significantly higher (p<0.002) in the infraspinatus only repair group compared to the no repair group at all time points except day 7 (Fig. 2B). Braking forces in the two-tendon repair and the infraspinatus only repair groups were significantly different at early time points (day 3 and 7), but not at time points after day 7. Braking forces were significantly different than baseline, injured values at all time points in all groups.
Propulsion forces were significantly different (p<0.025) in the infraspinatus only repair group compared to the no repair group at all time points (Fig. 2C). No significant differences were found between the infraspinatus only repair and two-tendon repair groups at any time point. The infraspinatus only and two-tendon repair groups were not significantly different compared to baseline, uninjured values at days 10 through 28 and days 14 through 28, respectively. The no repair group was not significantly different compared to baseline, uninjured values at days 7 and 28.
The vertical ground reaction force (the amount of weight the rat places on the extremity) was not significantly different between the groups at any time point except day 14, where a small but significant difference between the two-tendon repair group and infraspinatus only repair group was observed (Fig. 2D). In all groups at all time points, the vertical ground reaction forces were significantly different than baseline, uninjured values.
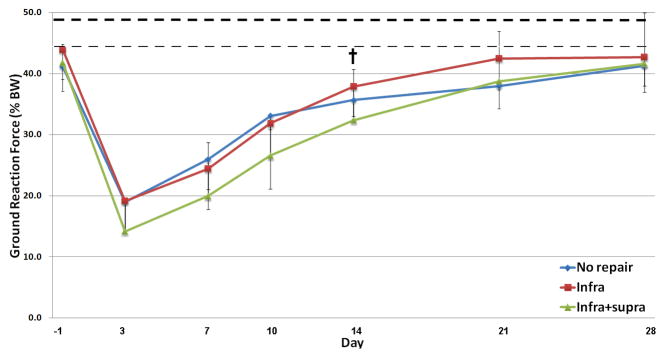
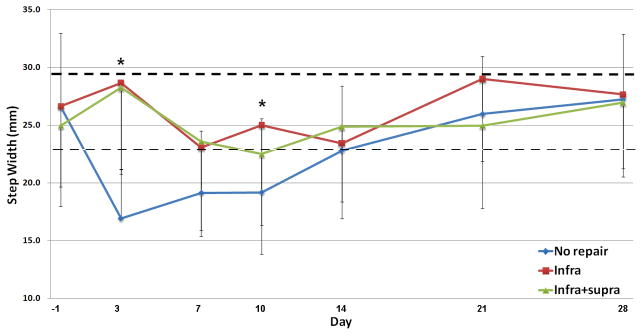
The step width in the no repair group was significantly lower at early time points (day 3, 7, and 10) and was significantly lower than the infraspinatus only repair group up to 10 days after repair surgery (p<0.01) (Fig. 3). No difference was found between the infraspinatus only repair and two-tendon repair groups at any time point. At day 3, step width of the infraspinatus only and two-tendon repair groups were not significantly different compared to baseline, uninjured values. All groups were significantly different than baseline at days 7 through 14, then returned to baseline values at days 21 and 28, except for a small but significant difference between the two-tendon repair group and baseline, uninjured values at day 21.
Figure 3.
Step width across the three groups demonstrating a decrease in step width at early time points in the no repair group (*p<0.05 infraspinatus repair vs. no repair, †p<0.05 between infraspinatus repair vs. two-tendon repair). The thick dotted line represents average baseline values for all animals obtained before detachment surgery; the thin dotted line represents one standard deviation from the baseline average.
Discussion
This study investigated the effects of restoring the balance of anterior and posterior cuff forces on shoulder function in a chronic rat rotator cuff tear model and is the first to investigate repair of two-tendon rotator cuff tears in an animal model. Using quantitative ambulatory measures, we found that the kinetics of an infraspinatus only repair mirrored that of a two-tendon repair and were significantly different than the kinetics of a simulated chronic tear in which neither tendon was repaired (Table 1). These results support our hypothesis and other clinical observations that restoring the balance of anterior-posterior forces by repair of the infraspinatus only is sufficient to improve shoulder function to a level similar to repairing the supraspinatus and infraspinatus together.
TABLE 1.
Comparison of kinetic variables between groups.
| Infraspinatus-only repair vs. | ||
|---|---|---|
| Kinetic variable | Two-tendon repair | No repair |
| Medial/lateral force | NS except day 10 | p<0.025 at all time points |
| Braking force | NS except day 3, 7 | p<0.025 except day 7 |
| Propulsion force | NS at all time points | p<0.025 at all time points |
| Vertical force | NS except day 10 | NS at any time point |
| Step width | NS at all time points | p<0.025 at early time points |
NS – no significance.
At nearly every time point post-repair surgery, the medial/lateral, braking, and propulsion forces of the infraspinatus only repair animals were significantly different than those forces of the no repair group. Furthermore, kinetics of the infraspinatus repair group mirrored that of the two-tendon repair group, with differences found at only a minimal number of time points. Propulsion and braking forces, which are measured in the forward flexion plane in the rat, correlate to human abduction due to differences in the orientation of the scapula. This is often used as an objective measurement of shoulder function in humans. We observed no differences between the infraspinatus repair and two-tendon repair groups for these ambulatory parameters, and by day 10 to 14, saw no differences between the braking and propulsion values for the two repair groups and baseline ambulatory values measured before repair surgery. This suggests that a partial repair of the infraspinatus only would be adequate to provide a clinically significant improvement in shoulder function for both repair groups. These differences persisted until the last time point recorded after repair surgery.
The step width can be used as an indicator of shoulder function by quantifying the amount of contralateral limb compensation to provide stability for the injured limb. The step widths of the infraspinatus only repair and two-tendon repair groups were no different than baseline at any point after surgery and were significantly higher than the no repair group up to 10 days after repair surgery. The decreased step width in the animals in which no tendon was repaired indicates “tripoding” and decreased shoulder function, while the step widths of the infraspinatus repair and two-tendon repair groups were no different than baseline values. Previous studies investigating the ambulatory parameters in animals undergoing acute repair of supraspinatus detachments showed no difference in step width at any time point when compared to uninjured controls.23 These results indicate that in the no repair group, animals needed more contralateral limb compensation and stabilization during the gait cycle compared to the repair groups.
Clinically, these results suggest that a patient with a chronic, two-tendon tear with retraction of the supraspinatus may benefit from a partial repair. Previous clinical case series showed improvements in shoulder function after partial repair.20–21 Burkhart et al demonstrated an improvement of an average of 90° of shoulder elevation (from 60 to 150°) after partial repair, with 13 of 14 patients satisfied with their results. They concluded that partial repair of massive irreparable cuff tears and creation of a “functional cuff tear” is mechanically superior to tendon transposition.21 Duralde et al similarly demonstrated an improvement in active elevation from 114 to 154° with 22 of 24 patients satisfied after partial repair of a massive rotator cuff tear.20 These clinical results suggest that shoulder elevation in the functional range can be restored with restoration of the posterior cuff; however, long term implications on repair integrity are unknown. Using ultrasound and standard radiographic evaluation, Keener et al demonstrated that a significantly greater amount of proximal humeral migration occurred in tears involving the infraspinatus than isolated tears of the supraspinatus, and tear size was the only independent predictor of proximal humeral migration25. These data support our results and suggest that massive tears that extend to involve the infraspinatus are more likely to disrupt normal glenohumeral kinematics.
Our study has several limitations. While we previously showed that biomechanical, geometric, and histological properties remain altered in this chronic rat rotator cuff model through the time points studied, it does not exactly replicate the human condition. Based on similar anatomy including tendon insertions and bony anatomy, the kinematics of the rat shoulder would most likely replicate the human most closely of all non-human primate animal models; however, in our study, improved rat shoulder function after partial repair may not necessarily translate to a similar degree of improved human shoulder function. Nonetheless, our results demonstrate the concept of functional consequences of these conditions. The tendon is acutely detached from its insertion site and therefore does not result from chronic degeneration that is usually seen in humans; therefore, the environment and healing potential of the repaired tendons in this model may be different. Also, scar tissue forms between the detached tendon edges and the insertion site, which is common among all animal models, but does not occur in humans. This scar tissue could account for the apparent improved kinetics seen in the group with no tendon repair. In addition, not all kinetic parameters reached uninjured values by the end of the study; therefore, the clinical significance of improved shoulder function that does not reach baseline can be questioned. Kinetic data only rather than kinematic data additionally were reported, as we were unable to track shoulder position with enough accuracy to discriminate between groups.
Future investigations include studies investigating the effect of activity after a partial repair. Although restoration of the balance of forces restored shoulder function in this study, the long-term implications of repairing only the posterior rotator cuff musculature are not well described. Previous studies showed that larger tears of the supraspinatus lead to progression of the tear anteriorly and/or posteriorly, but whether these data apply to a “functional rotator cuff tear” created by a partial repair is unknown.26–28 Other future studies may include developing methods to accurately track shoulder position to determine shoulder kinematics. Also, the effect of restoring the balance of rotator cuff forces on the glenoid cartilage and intact tendons, such as the long head of the biceps tendon, remain interesting questions to be further investigated.
This study demonstrates that restoring the balance of anterior-posterior rotator cuff forces is sufficient to restore shoulder function in a rat rotator cuff model of a chronic, massive two-tendon tear. Ground reaction forces and step width show that animals in which only the infraspinatus was repaired have improved function when compared to animals in which neither tendon was repaired. Additionally, the kinetic data from an infraspinatus-only repair were not different from those from a two-tendon repair, indicating that repairing the posterior cuff musculature restores shoulder function to a level similar to that of a two-tendon repair. These results support use of a partial repair after a two tendon tear when necessary to restore adequate shoulder function. We utilize a controlled in vivo model system to quantitatively demonstrate the importance of rotator cuff musculature balance. This animal model of a two-tendon repair model can be used in future studies investigating massive rotator cuff tears.
Acknowledgments
This study was supported by NIH/NIAMS.
References
- 1.Thompson WO, Debski RE, Boardman ND, 3rd, et al. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24:286–292. doi: 10.1177/036354659602400307. [DOI] [PubMed] [Google Scholar]
- 2.Lippitt S, Matsen F. Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res. 1993:20–28. [PubMed] [Google Scholar]
- 3.Warner JJ, Bowen MK, Deng X, et al. Effect of joint compression on inferior stability of the glenohumeral joint. J Shoulder Elbow Surg. 1999;8:31–36. doi: 10.1016/s1058-2746(99)90051-4. [DOI] [PubMed] [Google Scholar]
- 4.Bassett RW, Browne AO, Morrey BF, An KN. Glenohumeral muscle force and moment mechanics in a position of shoulder instability. J Biomech. 1990;23:405–415. doi: 10.1016/0021-9290(90)90295-e. [DOI] [PubMed] [Google Scholar]
- 5.Karduna AR, Williams GR, Williams JL, Iannotti JP. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res. 1996;14:986–993. doi: 10.1002/jor.1100140620. [DOI] [PubMed] [Google Scholar]
- 6.Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77:296–298. [PubMed] [Google Scholar]
- 7.Yamaguchi K, Ditsios K, Middleton WD, et al. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699–1704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- 8.Rockwood CA, Jr, Williams GR, Jr, Burkhead WZ., Jr Debridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am. 1995;77:857–866. doi: 10.2106/00004623-199506000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Levy O, Mullett H, Roberts S, Copeland S. The role of anterior deltoid reeducation in patients with massive irreparable degenerative rotator cuff tears. J Shoulder Elbow Surg. 2008;17:863–870. doi: 10.1016/j.jse.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Liem D, Lengers N, Dedy N, et al. Arthroscopic debridement of massive irreparable rotator cuff tears. Arthroscopy. 2008;24:743–748. doi: 10.1016/j.arthro.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991:45–56. [PubMed] [Google Scholar]
- 12.Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992:144–152. [PubMed] [Google Scholar]
- 13.Parsons IM, Apreleva M, Fu FH, Woo SL. The effect of rotator cuff tears on reaction forces at the glenohumeral joint. J Orthop Res. 2002;20:439–446. doi: 10.1016/S0736-0266(01)00137-1. [DOI] [PubMed] [Google Scholar]
- 14.Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994:78–83. [PubMed] [Google Scholar]
- 15.Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998;33:163–170. doi: 10.1097/00004424-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Hersche O, Gerber C. Passive tension in the supraspinatus musculotendinous unit after long-standing rupture of its tendon: a preliminary report. J Shoulder Elbow Surg. 1998;7:393–396. doi: 10.1016/s1058-2746(98)90030-1. [DOI] [PubMed] [Google Scholar]
- 17.Aluisio FV, Osbahr DC, Speer KP. Analysis of rotator cuff muscles in adult human cadaveric specimens. Am J Orthop (Belle Mead NJ) 2003;32:124–129. [PubMed] [Google Scholar]
- 18.Halder AM, Zhao KD, Odriscoll SW, et al. Dynamic contributions to superior shoulder stability. J Orthop Res. 2001;19:206–212. doi: 10.1016/S0736-0266(00)00028-0. [DOI] [PubMed] [Google Scholar]
- 19.Payne LZ, Deng XH, Craig EV, et al. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25:801–808. doi: 10.1177/036354659702500612. [DOI] [PubMed] [Google Scholar]
- 20.Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14:121–127. doi: 10.1016/j.jse.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 21.Burkhart SS, Nottage WM, Ogilvie-Harris DJ, et al. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/s0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 22.Dourte LM, Perry SM, Getz CL, Soslowsky LJ. Tendon properties remain altered in a chronic rat rotator cuff model. Clin Orthop Relat Res. 468:1485–1492. doi: 10.1007/s11999-009-1206-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarver JJ, Dishowitz MI, Kim SY, Soslowsky LJ. Transient decreases in forelimb gait and ground reaction forces following rotator cuff injury and repair in a rat model. J Biomech. 43:778–782. doi: 10.1016/j.jbiomech.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perry SM, Getz CL, Soslowsky LJ. Alterations in function after rotator cuff tears in an animal model. J Shoulder Elbow Surg. 2009;18:296–304. doi: 10.1016/j.jse.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keener JD, Wei AS, Kim HM, et al. Proximal humeral migration in shoulders with symptomatic and asymptomatic rotator cuff tears. J Bone Joint Surg Am. 2009;91:1405–1413. doi: 10.2106/JBJS.H.00854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maman E, Harris C, White L, et al. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91:1898–1906. doi: 10.2106/JBJS.G.01335. [DOI] [PubMed] [Google Scholar]
- 27.Perry SM, Getz CL, Soslowsky LJ. After rotator cuff tears, the remaining (intact) tendons are mechanically altered. J Shoulder Elbow Surg. 2009;18:52–57. doi: 10.1016/j.jse.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cofield RH, Parvizi J, Hoffmeyer PJ, et al. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am. 2001;83-A:71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]