Abstract
While large epidemiological datasets can inform research on the etiology and development of borderline personality disorder (BPD), they rarely include BPD measures. In some cases, however, proxy measures can be constructed using instruments already in these datasets. In this study we developed and validated a self-report measure of BPD from the Multidimensional Personality Questionnaire (MPQ). Items for the new instrument—the Minnesota BPD scale (MBPD)—were identified and refined using three large samples: undergraduates, community adolescent twins, and urban substance users. We determined the construct validity of the MBPD by examining its association with (1) diagnosed BPD, (2) questionnaire reported BPD symptoms, and (3) clinical variables associated with BPD: suicidality, trauma, disinhibition, internalizing distress, and substance use. We also tested the MBPD in two prison inmate samples. Across samples, the MBPD correlated with BPD indices and external criteria, and showed incremental validity above measures of negative affect, thus supporting its construct validity as a measure of BPD.
Keywords: Borderline Personality Disorder, Scale Development, Multidimensional Personality, Questionnaire, Validity
Borderline personality disorder (BPD) is a severe and persistent form of psychopathology characterized by pervasive affective, cognitive, interpersonal, and behavioral dysfunction, including emotional lability, interpersonal disturbances, impulsive and risky behaviors, and transient episodes of dissociation or paranoia (APA, 1994; Linehan et al., 1993; Gunderson, 2001, Skodol, 2002). Individuals with BPD often engage in dangerous behavior, including deliberate self-harm and suicidal gestures, drug and alcohol abuse, unsafe sexual practices, and misuse of prescription medications (APA, 1994; Gunderson, 2001; Frankenburg & Zanarini, 2004; Links et al., 1995; Skodol et al., 2002, 2005; Trull et al., 2000; Zanarini et al., 1998a). Such individuals have poor longitudinal outcomes, including low life satisfaction, academic and occupational difficulties, and elevated mental health service utilization (Winograd, Cohen, & Chen, 2008).
Traditionally, BPD research has been conducted in clinical samples consisting mainly of Caucasian, female, upper-middle class, psychiatric inpatients hospitalized for recent suicide attempts (e.g., Silk, Lee, Hill, & Lohr, 1995; Zanarini et al, 2002; Zanarini, Frankenburg, Khera, & Bleichmar, 2001). Research on psychiatric samples has provided valuable information about the correlates and comorbidity of BPD. Yet, there is a great deal about the etiology of BPD that cannot be understood from the study of clinic-based samples alone. For instance, much remains unknown about the epidemiology, genetics, onset, and course of BPD. Answering such questions requires the statistical power and methodology provided by large, representative samples that are followed longitudinally.
Longitudinal datasets such as the Dunedin Multidisciplinary Health and Development Study (Langley, Moffitt, & Silva, 1997; the Iowa development projects (Iowa Family Transitions Project, Iowa Youth and Families Project, Iowa Single Parent Project; Donnellan, Assad, Robins & Conger, 2007; Donnellan, Conger, & Burzette, 2007; Ge & Conger, 1999; Kim, Conger, Lorenz, & Elder, 2001); the Minnesota Study of Twins Reared Apart (Bouchard, Lykken, McGue, Segal, & Tellegen, 1990) and the Minnesota Twin and Family Study (Iacono et al, 1999) (to name some of the more known ones) contain a wealth of developmental, genetic, and psychophysiological information critical to understanding personality and psychopathology. Unfortunately, these large datasets lack direct assessment of BPD. However, if BPD can be measured using inventories of normal personality that are routinely administered in such large-scale investigations, however, the data collected could be used to answer questions about the disorder that are difficult or impossible to test in smaller, clinically ascertained cross-sectional samples. Such investigations can then inform more targeted projects that are specifically designed for BPD research.
This approach has been successfully utilized in previous research. Indeed, multiple studies have shown that BPD can be mapped from several continuous personality measures such as the Five Factor Model (FFM; Costa & McCrae, 1992; Saulsman, & Page, 2004; Clarkin, Hull, Cantor, & Sanderson, 1993), the Temperament and Character Inventory (Cloninger, Svrakic, & Przybeck, 1993; Ball, Tennen, Poling, Kranzler, & Rounsaville, 1997), and the Schedule for the Nonadaptive and Adaptive Personality (SNAP; Clark, 1993; Reynolds & Clark, 2001). For example, Trull and colleagues (2003) have utilized the NEO-Personality Inventory Revised (NEO-PI-R), a measure of the Five-factor model (FFM) of personality, to develop a new measure of BPD based on the congruence between NEO-PI–R scores and an expert rating profile of prototypical BPD traits. Similarly, Miller and colleagues (2001) utilized the NEO-PI-R to develop a measure of psychopathy. The BPD and psychopathy profiles were subsequently validated against several external correlates, including childhood trauma, parental psychopathology, and poor social functioning. Such results provide confidence that inventories of normal personality can be used to index personality disorders in general and BPD in particular.
A key consideration in developing a novel measurement of psychopathology are the existing instruments available for validation purposes. Fortunately, there are several well-established measures of borderline personality symptoms. These include the Personality Assessment Inventory – Borderline Subscale (PAI-BOR, Morey, 1991), the Personality Disorder Questionnaire-4 (Hyler, 1994), the Borderline Symptom List (Bohus et al., 2001), and the Zanarini Rating Scale For Borderline Personality Disorder (Zanarini et al, 2003). The PAI-BOR is one of the more widely-used measures and has demonstrated excellent psychometric properties in prior published work, including strong convergence with diagnostic measures of BPD (Trull, 1995). Moreover, Trull et al (2003) found that the PAI-BOR demonstrated high correlations with the FFM BPD prototype profile. Additionally, several recent studies indicate that self-report questionnaires are practical and valid alternatives to interview-based approaches (Hopwood et al., 2008; Jacobo, Blais, Baity, & Harley, 2007; Stein, Pinkster-Aspen, & Hilsenroth, 2007). Also, recent data indicate that the effectiveness of interview and self-report varies depending on the symptom being assessed. For example, Hopwood and colleagues (2008) reported that self-report instruments show higher validity when measuring experiential symptoms (i.e., identity disturbance and chronic emptiness) whereas interview-based methods showed higher validity in relation to observable and behavioral symptoms such as deliberate self-harm and impulsive acts.
Overview of Current Investigation
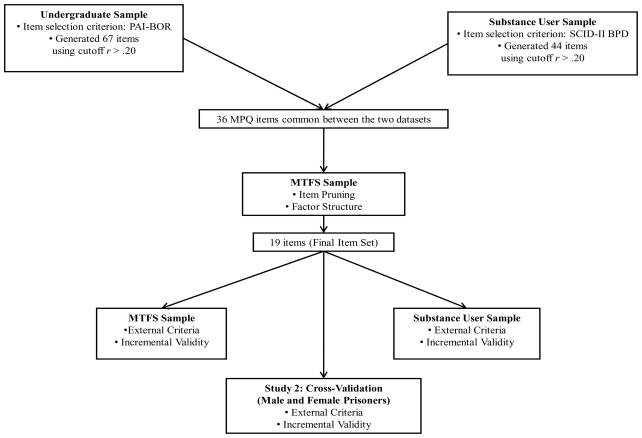
Inspired by the success of previous efforts to index personality syndromes using normal personality measures (Trull et al, 2003; Benning et al, 2005a,b; Miller et al., 2001), the current investigation utilized the Multidimensional Personality Questionnaire (MPQ, Tellegen, 1982, 1988, Patrick et al., 2002), a broadband inventory of normal-range personality traits. As such, our goal was to derive an index of BPD from a personality inventory that is commonly administered in epidemiological data sets. In other words, our goal was not to create a new measure of BPD symptoms and traits (a process in which new items would be generated and refined through multiple rounds of data collection). Rather, we aimed to develop a valid measure of BPD tendencies from the MPQ, an existing omnibus personality inventory, now available in the popular brief form (Patrick et al., 2002), that has been in wide-ranging use for several decades in key studies (e.g., Ben-Porath et al, 1995; Bouchard, et al, 1990; Caspi et al, 1997; Church, & Burke, 1994; Donnellan, et al, 2007; Markon, et al, 2005; Donnellan, et al, 2007; Ge & Conger, 1999; Kim, et al, 2001). To develop and validate the MPQ-derived BPD scale, we capitalized on two community and two clinical datasets. In the first study, we identified candidate items for the novel measure in a) a large sample of mixed-gender undergraduate students using the PAI-BOR scale as the criterion, and b) a sample of mixed-gender urban substance users using a diagnosis of BPD as the criterion. After identifying this pool of candidate items, we selected the final set of items using an epidemiological sample of adult youth recruited from the community. Next, we tested the association between our new scale—the Minnesota Borderline Personality Disorder Scale (MBPD)—and external correlates empirically associated with BPD, such as childhood trauma, behavioral disinhibition, and substance use. (See Figure 1 for a graphical depiction of these validation procedures.)
Figure 1.
In study 2, we explored the utility of the MBPD scale in two samples of male and female prison inmates. In this study, we examined associations of the MBPD with several external measures and scale scores from a number of normal personality inventories. The use of urban substance users and prison inmates capitalizes on the expectation that they may be especially vulnerable to the development of BPD, given their heightened risk for many of the hypothesized risk factors for BPD, including BPD-relevant personality traits (e.g., impulsivity; Casillas & Clark, 2002; Moeller et al., 2002; Patton et al, 1995), environmental adversity (e.g., abuse, neglect, disruptions in attachment, and exposure to violence; see Fleming et al., 1998; Jasinski et al., 2000; Schwartz et al., 2005, Romero-Daza et al., 2003, Verona, Hicks, & Patrick, 2005), and behaviors associated with BPD itself including deliberate self-harm and suicidal behavior (Verona et al, 2001; Verona et al, 2005; Fulwiler, Forbes, Santangelo, & Folstein, 1997; Evren, Sar, Evren, & Dalbudak, 2008; Cottler, Campbell, Krishna, Cunningham-Williams, & Abdallah, 2005). Earlier studies suggest elevated rates of BPD among both drug users and prison inmates (Jordan, Schlenger, Fairbank, & Caddell, 1996; Zlotnick, 1997; Hochhausen, Lorenz, & Newman, 2002). Together, these findings support the utility of research with drug users and prison inmates for evaluating the performance of a novel BPD measure.
Scale construction and validation requires stipulating the expected correlates of BPD and then evaluating the extent to which a new measure exhibits predicted patterns of association with these external criteria. Behavioral disinhibition (Siever & Davis, 1991; Skodol et al., 2002) and affective dysregulation (Siever & Davis, 1991; Siever, Torgersen, Gunderson, Livesley, & Kendler, 2002; Skodol et al., 2002; Linehan, 1993; Livesley, Jackson, & Schroeder, 1992; Livesley, Jang, & Vernon, 1988) are considered to be two core temperamental liabilities for the development of BPD with clear links to models of normal-range personality (Trull et al, 2003; Costa & McCrae, 1990). BPD is also associated with a history of childhood trauma, adult victimization, and subsequent posttraumatic stress disorder (Zanarini et al, 1997, 2000; Linehan, 1993). Finally, individuals with BPD exhibit substantial psychiatric comorbidity, with elevated rates of mood and anxiety disorders (Zanarini et al, 1997; Zanarini et al, 1998a), substance use disorders (Zanarini et al, 1998a), and antisocial behavior (Paris, 1997).
Relying on previous research, we formulated four hypotheses for the current study. We predicted that MBPD scores would be associated with (1) childhood abuse and symptoms of PTSD; (2) disinhibitory behaviors, including impulsivity, criminal and antisocial behavior, substance use, and suicidal behavior; (3) indices of internalized distress such as depression, anxiety, and fear; and (4) personality traits such as neuroticism and stress reaction. Given that some (albeit somewhat inconsistent) evidence suggests gender differences in both the rates and clinical presentation of BPD (Paris, 1997), we examined our predictions separately for male and female samples.
STUDY 1. CREATING AN MPQ ITEM-BASED SCALE
Method
As noted above, Study 1 included three separate samples evaluated with different sets of instruments and procedures. All participants provided written consent after written and oral assurances of confidentiality. The current study was approved by the University of Minnesota Institutional Review Board.
Sample 1:Undergraduate Students
Participants
Participants were 288 (57% female) students recruited from the “Introduction to Psychology” subject pool. The mean age for the sample was 20.5 years (SD = 2.9 years). Eighty-six percent of the participants were non-Hispanic White.
Study questionnaires were administered and monitored by research assistants in classrooms and auditoriums. Participants were compensated with extra class credit or a $10 payment. Items from the target measures (see below) were randomly included with items from other questionnaires to offset order effects.
Measures
To document and ensure reliability, across the many measures used in the current report, we examined four reliability indices. Diagnostic reliability was calculated from the kappa coefficient, scale internal consistency was evaluated using Cronbach’s α, and the reliability of a composite measure composed of multiple scales was determined by examining mean inter-scale correlations Finally, mean inter-item correlations were used to index correlations among categorical items (e.g., experience of some type of negative life event such as rape) composing a scale.
MPQ-Brief Form (MPQ-BF; Patrick et al., 2002)
The MPQ is a self-report personality inventory that was developed through factor analysis to assess normal personality functioning. The MPQ-BF is a 155-item version of the original 300-item MPQ (Tellegen, 1982), developed to assess a variety of personality traits and temperamental dispositions. Items have a dichotomous, “true” or “false” response format. MFQ-BF includes 11 primary trait scales which load onto three higher-order factors. The traits of Well-Being, Achievement, Social Closeness, and Social Potency load onto the higher-order factor of Positive Emotionality (predisposition to experiencing positive affect); the traits of Stress Reactivity, Alienation, and Aggression make up the higher-order factor of Negative Emotionality (the predisposition to experiencing negative affect); the traits of Control, Harm Avoidance, and Traditionalism load on the higher-order factor of Constraint (predisposition to behavioral self-control, the converse of disinhibition); and the trait of Absorption does not load preferentially on any of the higher-order factors. Scores from the traits scales of the MPQ-BF are highly correlated with the equivalent trait scales from the original MPQ (r’s ranged from .92 to .96) and have demonstrated high internal consistency (α’s range from .74 to .84; Patrick et al., 2002).
PAI-BOR (Morey, 1991)
BPD features were assessed by self-report using the PAI-BOR. The PAI-BOR consists of 24 items rated on a 4-point scale ranging from 1 (false) to 4 (very true). The measure has four subscales: Affective Instability, Identity Problems, Negative Relationships, and Self-Harm (Morey, 1991). The PAI-BOR exhibits good internal consistency (α = .84; Morey, 1991), high test-retest reliability over a 3- to 4-week time period (r = .86; Morey, 1991), and good convergent and discriminant validity (Stein, Pinsker-Aspen, & Hilsenroth, 2007; Trull, 1995). Item and scale loadings are similar across age and gender (DeMoor et al, 2009). Cronbach’s α in the current sample was .85.
Sample 2: Urban Drug Users
Participants
We enrolled 146 inpatient residents in a drug and alcohol abuse treatment center in Northeast Washington, D. C. Treatment residency ranges from 30 to 180 days. Program admission required complete abstinence from alcohol and drugs (including methadone) except for caffeine and nicotine. Regular drug testing was mandated and substance use was grounds for dismissal. If needed, detoxification took place prior to program admission. Aside from authorized outside activities (e.g., group retreats, physician visits), residents could not leave the center grounds during treatment.
Study participants ranged in age from 18 to 67 years, with a mean age of 42.0 years (SD = 9.2 years). Sixty-five percent were male; 92% self-identified as African-American, 6.3% as non-Hispanic white, 0.6% as Hispanic, and 1.1% as other. Among the sample, 21.1% had not completed high school or earned a GED, 42.9% had completed high school or received a GED, and 36.1% had enrolled in college or a technical school. Most participants were single (69.0%) and unemployed (68.0%). Residents were asked to participate in the study within one week of arriving at the treatment center.
Measures
In addition to the MPQ-BF, all participants completed a battery of self-report questionnaires to determine associations between the MBPD scales and external correlates. Structure interviews and measures were randomly sequenced across participants to limit order effects. The instruments are discussed below within each domain of interest.
Assessment of BPD
We used the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II) to determine BPD diagnostic status (First et al., 1997). Interviews were conducted by Dr. Bornovalova, who was trained in administration of the SCID-II. These interviews were conducted with no knowledge of participant scores on others study measures. Twenty-five percent of these interviews were reviewed by another PhD-level clinician. In the three cases where a discrepancy existed, a consensus was reached. Based on SCID-II results, 37% of the women (n = 19) and 11% of the men (n = 10) had diagnosis of BPD. Participants also completed the self-report Inventory for Interpersonal Problems-BPD scale (IIP-BPD) which uses two of the five IIP scales: interpersonal sensitivity and aggression (Lejuez et al, 2003; Pilkonis, Kim, Proietti, & Barkham, 1996). These subscales, theoretically and empirically associated with BPD, are related to central features of the disorder in non-clinical samples of college students and of substance users (Lejuez et al., 2003). Cronbach’s α for the IIP-BPD in the current sample was .91.
Substance dependence
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First et al., 1996) was used to assess dependence on alcohol, cannabis, crack/cocaine, heroin, and hallucinogens. (Administration protocol mirrored the SCID-II above.) We also administered a self-report measure assessing past year use of alcohol, marijuana, crack/cocaine, heroin, and PCP.
Antisocial behavior/behavioral disinhibition
Because previous studies indicated that BPD was correlated with behavioral problems and antisocial behavior (Frankenburg & Zanarini, 2004; Dougherty et al, 1999), we assessed conduct disorder (CD; childhood criteria for antisocial personality disorder) and antisocial personality disorder. Additionally, we administered two scales measuring trait-impulsivity, the UPPS Impulsive Behavior Scale (UPPS; Whiteside & Lynam, 2001), and the Barratt Impulsiveness Scale Version 10 (BIS-10; Barratt & Patton, 1983, Barratt, 1985). The UPPS is a 45-item self-report measure used to measure four impulsivity-related traits: Urgency, (lack of) Premeditation, (lack of) Perseverance, and Sensation Seeking. In the current study, all but the Sensation Seeking scale were administered to the sample of drug users (α = .88). The BIS-10 is a 34-item measure of impulsivity that also demonstrated excellent psychometric properties with this sample (α = .83). For the purposes of data reduction, we conducted a principal components analysis on the six utilized subscales from both measures. This analysis produced a one-factor solution, accounting for 59% of the variance in the construct. This factor (termed Impulsivity) was used as a criterion variable.
Internalizing distress
To assess internalizing distress, participants completed the Center for Epidemiological Studies – Depression Scale (CES-D; Radloff, 1977). This 22-item self-report scale is designed to measure affective components of depressive symptoms, including depressed mood, feelings of guilt and worthlessness, psychomotor retardation, feelings of helplessness and hopelessness, loss of appetite, and sleep disturbance during the past two weeks (sample α = .84).
Childhood trauma
Childhood abuse was assessed using the emotional, physical, and sexual abuse subscales of the Childhood Trauma Questionnaire-Short Form (CTQ-SF; Bernstein et al., 2003). The CTQ-SF is a 28-item measure that retrospectively assesses childhood maltreatment. Previous studies indicated excellent psychometric properties for this scale (Bernstein, Ahluvalia, Pogge, & Handelsman, 1997) which were also borne out for the current sample (α = .86).
Sample 3: Adult Youth Twins Recruited from the Community
Participants
The sample included 510 male and 622 female twins drawn from the Minnesota Twin Family Study (MTFS), a longitudinal investigation of the epidemiology of psychiatric and substance abuse disorders. Twins born in Minnesota between1972 to 1979 (according to public records) were recruited into this study the year the twins turned 17 years old. Participants were drawn from the general community subject to two exclusionary criteria. First, the families had to live within a day’s drive of the University of Minnesota laboratories. Second, neither twin could have a physical or mental handicap that would preclude participation in the day-long assessment (a full description of the design of the MTFS has been provided elsewhere; Iacono et al., 1999). The mean age for the sample was 17.5 years (SD = 0.5 years). Consistent with the demographics of Minnesota during the years the twins were born, 98% of the twins were non-Hispanic White.
The MTFS sample does not contain a diagnostic assessment of BPD, and thus, the rates of BPD in the sample cannot be estimated. However, participants in this sample receive a number of other diagnostic assessments for disorders that are known to be comorbid with a diagnosis of BPD. In particular, at age 17, the rates of lifetime adult antisocial behavior (AAB, adult criteria for antisocial personality disorder; 3.4% in men, 2.1% in women) alcohol dependence (9.7% in men, 6.7% in women), illicit drug dependence (3.8% in men, 3.5% in women), and major depressive disorder (12.1% in men, 23.0% in women) are similar to estimates from other large-scale studies (Grant et al, 2008). Given the high comorbidity of BPD with these disorders, it is likely that BPD is present at rates commonly found in epidemiological studies of young adults. All twins provided written informed consent or assent as appropriate (parents provided informed consent for twins under age 18).
Measures
Participants in the Minnesota Twin Family Study completed a 198-item version of the MPQ. The twins also completed several questionnaires and structured interviews to test construct validity of MBPD scores within several domains.
Substance Use and Abuse
Participants were interviewed for lifetime nicotine, alcohol, and illicit drug abuse and dependence, as defined by the Diagnostic and Statistical Manual of Mental Disorders (3rd ed Revised; DSM–III-R; American Psychiatric Association, 1987). Researchers used the Substance Abuse Module (SAM) of the Composite International Diagnostic Interview (Robins, Baber, Cottler, 1987). Kappa reliabilities were > .91 for each substance use disorder diagnosis. The nicotine use/dependence variable was calculated by taking the mean z-score of nicotine dependence symptoms, average number of days the participant used tobacco in a month (0 to 30), and the average number of cigarettes (or other tobacco products) used in a day. The alcohol use/dependence variable was calculated by taking the mean z-score of alcohol abuse and dependence symptoms, number of lifetime intoxications, and maximum number of drinks consumed in 24 hours. The drug use/dependence variable was calculated by taking the mean z-score of drug abuse and dependence symptoms, number of different illicit drug classes used, and number of lifetime marijuana and stimulant uses. The mean inter-scale correlations for the nicotine, alcohol, and drug-use composites were .76, .70, and .69, respectively.
Antisocial behavior/behavioral disinhibition
Conduct disorder (CD) and adult antisocial behavior (AAB) symptoms were assessed using a structured interview based on the Structured Clinical Interview for DSM-III-R-II. Kappa reliabilities for diagnoses of CD and AAB were .81 and .95, respectively. Non-diagnostic indicators of behavioral disinhibition were obtained from the Life Events Interview (Billing et al., 1996). A scale score was derived from these behaviors: history of suspension or expulsion from school; legal difficulties other than traffic violations; and sexual intercourse before the age of 17. Participants also completed the Delinquent Behavior Inventory, a 36-item (α = .95) inventory of antisocial acts committed during adolescence (DBI, Gibson, 1967). Participants also completed the Behavioral Disinhibition (BD) scale (Taylor et al., 2000), a 12-item (α = .68) subscale of the California Psychological Inventory-Socialization scale (Gough, 1957, 1960). Finally, multiple teacher ratings were obtained for most participants (76%) using for a 30-item (α = .92) scale of externalizing behavior. The teacher rating scale incorporates DSM-III-R criteria for conduct disorder and oppositional defiant disorder, as well as trait descriptors associated with externalizing behavior (e.g., impulsivity and aggressive).
A composite measure of antisocial behavior/behavioral disinhibition was calculated by taking the mean z-score for (1) symptoms of CD and AAB, (2) Life Events Interview behavioral disinhibition items, (3) DBI scores, (4) BD scale scores, and (5) teacher ratings of externalizing behavior (mean inter-scale correlation for composite = .43). An overall Externalizing (EXT) composite variable was then calculated by using the mean z-score of the composite antisocial behavior/behavioral disinhibition variable and the three substance use/dependence variables (mean inter-scale correlation = .60).
Internalizing distress
Modules from the Structured Clinical Interview for DSM-III-R were used to assess select mood and anxiety disorders. Specifically, participants were interviewed for lifetime incidence of major depressive disorder, social phobia, and simple phobia. Kappa reliabilities ranged from .78 to .89 for these disorders. Teacher ratings of students were obtained on a 12-item (α = .85) rating scale measuring overall internalizing distress. The INT variable was calculated by taking the mean z-score of the symptoms of the 3 disorders and the teacher rating of internalizing distress.
Analytic Approach and Results for Initial Development of the Minnesota Borderline Personality Disorder Scale (MBPD)
We conducted the initial development and item selection of the MBPD in the three samples described above. The initial items for the scale were selected using the undergraduate and the urban drug user samples as each included a measure designed to assess BPD traits or symptoms. The MTFS sample was then used to advantage for further refining and finalizing our item selection. By reserving the MTFS sample for the final step in scale refinement, we were able to reduce the number of items to a core set (Appendix A) the construct validity of which was supported by the work carried out below.
Appendix.
Final Items for the MBPD Scale (155/300 item versions)
| MPQ Scale | Item # (155/300 item versions) | Abbreviated Item |
|---|---|---|
| Stress Reaction | 125/292 | Unaccountably change from happy to sad. |
| 18/95 | Mood often fluctuates. | |
| 149/ 270 | Sometimes am “on edge” all day. | |
| 78/131 | Sometimes feel strong emotions without knowing why. | |
| 90/212 | Sometimes over-react to minor problems. | |
| Alienation | 42/ 147 | Mean things often said about me. |
| 54/238 | Often betrayed by friends. | |
| 126/ 250 | Often been lied to. | |
| 150/103 | Often have bad luck. | |
| Control | 86/ 41 | Often act impulsively. |
| 44/ 26 | Usually make decisions very carefully. | |
| 128/ 176 | Often not cautious enough. | |
| Aggression | 8/82 | Often want to hit someone when angry. |
| 127/293 | Sometimes like to hit someone. | |
| 151/ 158 | Sometimes enjoy saying mean things. | |
| Well-Being | 74/ 170 | Most mornings day seems bright. |
| 104/ 159 | Rarely feel happy. | |
| Absorption | --/76 | Sometimes experience a “different state of being.” |
| --/ 40 | My mind sometimes encompasses world. | |
| 71/ -- | Often “sense” people before seeing them. | |
| 130/-- | Sometimes feel presence of people not actually there. |
Note: There are actually several different versions of the MPQ: the 300 item version, and the 155 item version (a 198-item version has been used at the University of Minnesota previously as well, but this format is not used anywhere else). The 300 item version (very widely used) has both a 2- and a 4-point response format (true/false for 2-point response format; definitely true, probably true, probably false, and definitely false for 4-point response format), and the 198-item version has a 4-point response format only. The brief MPQ (155-item version) has a binary (True/False) format. Because some labs use the 300-item version and others use the 155-item version, we created an MBPD version for each full MPQ format. Therefore, MBPD scores can range from 19–76 when using the 300-item version of the MPQ, and from 0–19 when using the MPQ-BF. The double dash symbol shows which items did not have an equivalent between versions.
Testing the Structural Relationship of MPQ Subscales with Measures of BPD (Undergraduate and Urban Drug User Samples)
First, to determine if the MPQ shows the same structural relationship to the two measures of BPD available in the undergraduate and urban drug user samples, the PAI-BOR and BPD diagnostic symptom counts were regressed onto the 11 primary MPQ scales. Table 1 provides the bivariate correlations and beta weights of the MPQ primary scales with PAI-BOR scores and BPD diagnostic symptom counts. Both the PAI-BOR scores and symptom counts were strongly associated with Stress Reaction and moderately associated with Alienation, low Control, Aggression, and low Well-being scores (gender differences and contrast zs for the MPQ scales are also presented in Table 1). The multiple Rs were .85 and .71 (undergraduates and urban drug users, respectively), which are similar tothe reliability of the PAI-BOR total score. The fact that the MPQ has a similar structural relationship with two different BPD measures and in the two different samples attests to the potential of a scale derived from MPQ items to serve as a valid estimate of BPD tendencies.
Table 1.
Correlations and Regression Coefficients between MPQ Scores and PAI-BOR (Undergraduate Student Sample, N = 288; males = 124; females = 164) and BPD symptom count (Urban Drug User Sample, N = 146; males = 94; females = 52).
| BPD Diagnostic Symptom Count | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PAI-BOR | Total Sample | r Men | r Women | Contrast Z | Total Sample | r Men | r Women | Contrast Z | ||
| MPQ Scale | β | r | β | r | ||||||
| Well-being | −.10† | −.29** | −.22† | −.38** | 1.47 | −.11 | −.19* | −.04 | −.37** | 1.97* |
| Social Potency | .05 | .03 | .01 | .05 | −.33 | .18* | .04 | .10 | .01 | .51 |
| Achievement | −.01 | −.04 | −.06 | −.03 | −.25 | .01 | −.21* | −.21* | −.17** | −.23 |
| Social Closeness | .06 | −.18* | −.18 | −.25* | .61 | .06 | −.32** | −.29** | −.32* | .19 |
| Stress Reaction | .55** | .74** | .72** | .75** | −.54 | .47** | .62** | .57** | .65** | −.72 |
| Alienation | .24** | .62** | .56** | .66** | −1.33 | .25** | .49** | .39** | .52** | −.93 |
| Aggression | .12** | .37** | .40** | .42** | −.20 | .09 | .35** | .41** | .36* | .33 |
| Control | −.19** | −.32** | −.23* | −.41** | 1.67 | −.13 | −.42** | −.42** | −.41** | −.07 |
| Harm Avoidance | −.03 | −.11 | −.04 | −.25* | 1.79 | .08 | −.04 | .05 | −.12 | .96 |
| Traditionalism | −.01 | −.17* | −.22† | −.16† | −.52 | .01 | −.01 | .01 | −.06 | .40 |
| Absorption | .09† | .40** | −.43** | −.36** | −.69 | −.02 | .12 | .12 | .02 | .57 |
| Multiple R | .85 | .71 | ||||||||
| MPQ Superfactors | ||||||||||
| Agentic Positive Emotionality | −.05 | −.15† | −.16 | −.15 | −.09 | −.11¥ | −.22* | −.15 | −.28† | |
| Communal Positive Emotionality | −.02 | −.20* | −.18† | −.27* | .79 | |||||
| Negative Emotionality | .74** | .77** | .76** | .79** | −.60 | .59** | .62** | .59** | .62** | |
| Constraint | −.18** | −.29** | −.23† | −.41** | 1.67 | −.03 | −.29** | −.03 | −.29** | |
| Multiple R | .80 | .63 | ||||||||
p < .05;
p < .01;
p < .001;
A general negative emotionality estimate was computed for this sample
Identifying a Pool of Candidate Items for the MBPD Scale (Undergraduate and Urban Drug User Samples)
As described above, the undergraduate sample contains the PAI-BOR, and the urban drug user sample provides the diagnosis of BPD. To identify candidate items, we took items from each sample that a) correlated greater than .2 with the PAI-BOR and with the diagnosis of BPD, and b) overlapped across the two samples. We identified 67 MPQ items in the undergraduate sample and 44 MPQ items in the substance user sample. The items that overlapped between the two samples (36 items) were then further examined using the MTFS sample. These items correlated well with the criterion BPD measures (median value = .33; range = .20–.62).
Final Item Selection (MTFS Sample)
The final item selection took place in the MTFS sample. First, because the MTFS sample lacks an explicit measure of BPD, the regression weights derived from regressing the 11 MPQ subscales on PAI-BOR and BPD symptom count scores in the analyses above were used to provide anchor measures (termed PAI-BOR-est. and BPD symptoms-est.) for the MTFS sample. Next, we noted that many of the items identified above focused on general distress or dysphoria (i.e., several items from the Stress Reaction scale). To ensure that the MBPD scale would not simply be a measure of stress reaction, we conducted a principal components analysis of the 36 items identified above. Next, each item was individually entered into a regression equation with Stress Reaction, predicting 1) PAI-BOR-est. and 2) BPD symptoms-est. Items were retained only if they exhibited incremental predictive utility over scores on the Stress Reaction scale. This refinement process generated 19 items with a Cronbach’s α = .83 (see Appendix for brief item descriptions). The sum of these items correlated .90 with the PAI-BOR-est. and .86 with BPD symptoms-est.
Concurrent Validity
In the undergraduate sample, the correlation between scores on the 19-item MBPD scale and the PAI-BOR was .80, matching the internal consistency reliability of the MBPD (α = .81). MBPD scores correlated moderately to strongly with all PAI-BOR subscales, including Affective Instability (r = .73), Identity Problems (r = .64), Negative Relationships (r = .51), and Self-Harm (r = .52). As such, the MBPD scale appeared to provide adequate content coverage of the BPD construct.
In the substance user sample, we examined associations between the MBPD (α = .78 for this group) and SCID-II diagnoses of BPD, along with continuous scale measures of BPD tendencies. Results are reported in Table 2. As BPD diagnosis is a categorical variable, biserial correlations were calculated. For both male and female participants, there was a strong association between MBPD scores and the BPD diagnosis. MBPD scores also strongly correlated with IIP-BPD scores and multiple BPD symptoms on the SCID-II.
Table 2.
Zero-Order Correlations and Gender Differences between the MBPD and External Correlates in the Male (N = 94) and Female (N = 52) Inner-City Substance Users
| MPQ-BPD | Gender Difference | ||
|---|---|---|---|
| Male | Female | ||
| Criterion Variable | Contrast Z | ||
| BPD Status | .69** | .60** | .87 |
| Number of SCID-II BPD | .19 | ||
| Symptoms | .65** | .63** | |
| IIP-BPD | .59** | .62** | −.27 |
| Conduct Disorder | .32** | .49** | −1.15 |
| Adult Antisocial Behavior | .33** | .42** | −.59 |
| Impulsivity Composite | .63** | .51** | 1.01 |
| Substance Use Frequency | .23* | .05 | 1.04 |
| Number of Substance Dependence | .70 | ||
| Diagnoses | .25* | .13 | |
| Depression Symptoms (CES-D) | .44** | .37** | .47 |
| Childhood Abuse Score | .30** | .48** | −1.20 |
p < .05;
p < .01.
Mean Differences and External Correlates of the MBPD
Females scored significantly higher than men on the MBPD among the substance user sample. The mean (SD) was 8.24 (4.10) for males and 10.35 (3.84) for females (Cohen’s d = −.53, p < .01). Table 2 includes correlations between MBPD scores and external criterion variables. For both genders, MBPD scores were moderately to highly correlated with Conduct Disorder, Adult Antisocial Behavior, and the Impulsivity composite. MBPD scores correlated to substance use and substance dependence diagnoses in men only. There was a moderate association with depression severity and childhood abuse for both men and women. While women substance users exhibited slightly higher MBPD scores, there were no significant gender differences in terms of correlations with external variables (see Table 2 for contrast z statistics).
In the MTFS sample, there were no gender differences in MBPD scores [mean (SD) = 43.60 (7.67) for males and 42.7 (8.76) for females (Cohen’s d = .11, p > .1). We also examined the MBPD’s associations with theoretically relevant external criterion variables in the MTFS sample. Table 3 lists the correlations between MBPD scores and composite measures of substance use and abuse, behavioral disinhibition, and internalizing distress. For both men and women, MBPD scores were positively and significantly (all ps < .001) correlated with each composite variable including nicotine use/dependence, alcohol use/dependence, drug use/dependence, antisocial behavior/behavioral disinhibition, EXT, and INT. We also examined gender differences in mean-level MBPD scores and in the strength of the correlations across all variables in the current large sample. Results indicated that there were no significant gender differences in mean MBPD scores or in the magnitude of correlations with external criterion variables (see Table 3 for contrast z statistics).
Table 3.
Zero-Order Correlations between the MBPD and Clinical Variables in the MTFS Male (N = 505) and Female (N = 628) Samples
| MPQ-BPD | Gender Difference | ||
|---|---|---|---|
| Male | Female | ||
| Criterion variable | Contrast Z | ||
| Nicotine Use/Dependence | .22*** | .34*** | −1.54 |
| Alcohol Use/Dependence | .20*** | .31*** | −1.39 |
| Drug Use/Dependence | .20*** | .23*** | −.37 |
| Antisocial Behavior/ | .32*** | .41*** | −1.22 |
| Behavioral Disinhibition | |||
| Externalizing | .31*** | .40*** | −1.21 |
| Internalizing | .18*** | .29*** | −1.37 |
p < .05;
p < .01;
p < .001.
None of the differences in the magnitude between the correlations across gender were significant.
Incremental Validity of MBPD
Incremental validity was determined by testing whether the MBPD accounted for variance in the criterion variables beyond negative affectivity as measured by the Negative Emotionality superfactor of the MPQ (Tellegen, 1982). We also tested for gender differences. Specifically, we conducted a series of hierarchical regressions with Negative Emotionality scores and gender entered in the first step and MBPD scores entered in the second step with the external correlates of BPD (e.g., EXT, INT) as the criterion. In the substance user sample, MBPD scores were incrementally predictive of depression symptoms (R2Δ = .059, p < .001), impulsivity (R2Δ = .159, p < .001), and number of substance dependence diagnoses (R2Δ = .027, p < .05). However, MBPD scores did not predict childhood trauma (R2Δ = .004, p = .38), antisocial personality disorder status (OR = 1.10, p = .29), or conduct disorder (OR = 1.07, p = .45) when controlling for Negative Emotionality and gender. Finally, the MBPD scores were incrementally predictive of BPD diagnostic symptom count (R2Δ = .039, p < .01), BPD diagnosis (OR = 1.29, p < .05), and IIP-BPD scores (R2Δ = .049, p < .01).
In the community sample, the MBPD scores predicted nicotine use/dependence (Δ R2 = .054, p < .001), alcohol use/dependence (Δ R2 = .051, p < .001), drug use/dependence (Δ R2 = .044, p < .05), and antisocial behavior/behavioral disinhibition (Δ R2 = .081, p < .001). The new measure predicted EXT (Δ R2 = .081, p < .001) but not INT (Δ R2 = .001, p = .52). (This result is not surprising, given that the conceptual constructs of INT and Negative Emotionality strongly overlap). Taken together, these results support the construct validity of MBPD scores.
Mean Differences between Community and Clinical Samples
When examining mean-level differences across sample populations, we expected the substance user group would have higher MBPD scores than the community and undergraduate samples. Because of slight response option differences across samples, we dichotomized the 4-point response option for the MTFS sample to be on a similar scale as the other samples. With no significant differences between the undergraduate and twin samples (p > .1), MBPD scores were collapsed these into one sample. A 2 × 2 ANOVA – with sample group and gender entered as independent variables, age as a covariate, and MBPD scores as the dependent variable – revealed an effect of age [F(1, 1539) = 7.56; p < .01; lower age related to higher BPD traits], sample [F(2, 1539) = 26.95; p <.01; undergraduate twin sample < drug user sample], gender [F(1, 1539) = 8.38, p < .01; females > males], and sample X gender interaction [F(1, 1539) = 9.35; p <.01]. The sample X gender interaction effect indicated that females had higher levels of BPD traits than males in the drug user sample but not in the combined undergraduate/twin sample. Each of these effects is consistent with the general literature that also reports higher BPD traits in females compared to males, clinical compared to community samples, and younger compared to older participants (Grant et al, 2008; Segal, Hook, & Coolidge, 2001; Widiger & Weissman, 1991). This provides additional evidence that the MBPD is behaving in a way the larger BPD construct does.
Study 1 Discussion
Overall, the observed pattern of associations for MBPD scores is consistent with both theoretical conceptualizations and the empirical literature, and provides an initial step in the validation of the scale. The evidence also suggests that this measure is an index of something beyond just negative affect – a finding that adds to its construct validity. Thus, the initial validation results provide ground for cautious optimism about the validity of the MBPD scale.
Next, we examined the validity of the MBPD scale in two samples characterized by elevated levels of personality pathology: male and female prison inmates. As noted previously, a number of studies have shown that prisoners demonstrate both an elevated rate of BPD (Zlotnick, 1997; Hochhausen, Lorenz, & Newman, 2002) and behaviors associated with BPD such as substance use, violence, and deliberate self-injury (e.g., Verona et al, 2005). As such, prison inmates are an excellent sample in which our novel scale can be validated. In this study we examined the construct validity of the MBPD by delineating the associations between MBPD scores and expected external correlates including childhood trauma, behavioral disinhibition, substance use, and internalizing distress. As in Study 1, associations with normal personality traits were also examined. Consistent with the theoretical and empirical literature (Trull et al, 2003), we predicted that the MBPD scores would be positively correlated with measures of behavioral disinhibition and negative affectivity, and negatively correlated with measures of socialization and positive affect.
STUDY 2: PRISON INMATES: ASSOCIATION WITH PSYCHOPATHOLOGY AND NORMAL PERSONALITY
Method
Participants
The sample consisted of 240 male and 226 female inmates recruited from two medium security federal prisons in Florida. Among the males, the racial/ethnic composition was 47% non-Hispanic white, 40% African American, and 13% Hispanic. Among females, the distribution was 57.1% African American, 29.6% non-Hispanic White, 10.6% Hispanic, and 2.6% other. For men, the mean age was 32.7 years old (SD = 7.8 years); for women, 31.9 years old (SD = 6.8). Participants were recruited randomly from a master prison roster and contacted if they met inclusion criteria: a) absence of severe and persistent mental illness; b) release date not imminent; c) conversational competency in English, and d) ability to read the study description aloud. The study protocol received approval by an internal review board. All participants provided written informed consent prior to completing the structured interview and self-report questionnaires described below. (See Table 4 for measures administered in the male and female inmates, which were treated as separate samples). All participants also completed the MPQ. Cronbach’s α for the MBPD in the males was .81 and in the females .82.
Table 4.
Zero-Order Correlations and Gender Differences between the MBPD and External Variables in the Male (N = 240) and Female (N = 226) Prison Inmates.
| MPQ-BPD | Gender-Difference | ||
|---|---|---|---|
| Males | Females | ||
| Criterion Variable | Contrast Z | ||
| Conduct disorder | .18** | .42*** | −2.85** |
| Adult antisocial behavior | .23*** | .37*** | −1.65 |
| Charges before age 17 | −.02 | .28*** | −3.30** |
| Age of 1st charge | −.08 | −.29*** | 2.34** |
| Criminal variety index | .12 | .19** | −.77 |
| Violent behavior composite | .21** | .36*** | −1.76 |
| Survey of Alcohol and Drug Use | .21** | .25*** | −.45 |
| Drinking Motives Questionnaire | |||
| Social | .06 | .23** | −1.87 |
| Coping | .16* | .39*** | −2.68** |
| Enhancement | .09 | .29*** | −2.23** |
| Alcohol dependence scale | .42*** | .42*** | .00 |
| Short Drug Abuse Screening Test | .29*** | .25*** | .46 |
| Mental health treatment | .36*** | ||
| History of suicide attempts | .25*** | .31*** | −.70 |
| Beck depression inventory | .48*** | ||
| Penn State Worry scale | .48*** | ||
| FEQ Total anxiety | .54*** | ||
| Fear Survey Schedule | |||
| Total | .32*** | ||
| Social fears | .32*** | ||
| Agoraphobia fears | .27*** | ||
| Fears of bodily injury, death, & illness | .18* | ||
| Fears of sexual & aggression scenes | .23** | ||
| Fears of harmless animals | .15 | ||
| Traumatic life events - assaults | .34*** | ||
| Traumatic life events - total | .27*** | ||
| PTSD symptoms | .56*** | ||
| NEO-FFI Five Factor Inventory | |||
| Neuroticism | .64*** | ||
| Extraversion | −.35*** | ||
| Openness | −.22** | ||
| Agreeableness | −.46*** | ||
| Conscientiousness | −.44*** | ||
| EASI Temperament Inventory | |||
| Emotionality: Distress | .55*** | ||
| Emotionality: Fearfulness | .38*** | ||
| Emotionality: Anger | .39*** | ||
| Activity | .04 | ||
| Sociability | −.20* | ||
| Impulsivity | .32*** | ||
| PANAS Positive Affect | −.39*** | ||
| PANAS Negative Affect | .47*** | ||
| CPI Socialization scale | −.57*** | ||
| Anger expression questionnaire | .59*** | ||
| Sensation Seeking Scale | |||
| Total | .08 | ||
| Thrill and Adventure Seeking | −.17* | ||
| Experience Seeking | −.04 | ||
| Boredom Susceptibility | .31*** | ||
| Disinhibition | .26** | ||
p < .05;
p < .01;
p < .001.
Abbreviations: FEQ, Fenz-Epstein Questionnaire; PTSD, post-traumatic stress disorder; NEO-FFI, Neuroticism-Extraversion-Openness Five Factor Inventory; EASI, Emotionality-Activity-Sociability-Impulsivity Temperament Survey; PANAS, Positive and Negative Affect Schedule; CPI, California Psychological Inventory.
Male Prisoners
Externalizing behavior
Antisocial behavior was assessed via structured interviews and a review of the prison file. Interview items covered Conduct Disorder and Antisocial personality disorder (adult criteria) as defined by Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; APA, 1994). All interviews, conducted by trained research assistants, were videotaped and independently reviewed by two diagnosticians. The diagnostic inter-rater reliability, assessed via the intraclass correlation (ICC), was .85 and .91 for the adult and history of child symptoms, respectively. Measures of criminal behavior included age of first criminal charge and number of charges before age 17. Based on records and self-report, a criminal variety index detailed a prisoner’s engagement in different types of crime. Finally, a violent behavior composite incorporated the number of child and adult fights, history of domestic violence, and number of violent crimes (mean inter-item correlation = .20).
Substance use and abuse
Alcohol and drug use were determined using self-report questionnaires. The Survey of Alcohol and Drug Use (SADU) assessed quantity and frequency of use for nicotine, alcohol, and seven drug classes (Bachman, Johnston, & O’Malley, 1991). An overall substance use score was calculated utilizing the mean z-score across the different substances (mean inter-item correlation = .25). Symptoms of alcohol dependence, including severe miscues, were assessed using the 29-item Alcohol Dependence Scale (ADS; Skinner & Allen, 1982; α = .91), emphasizing the more severe manifestations of alcohol misuse. Additionally, the Drinking Motives Questionnaire (DMQ; Cooper, Russell, Skinner, & Windle, 1992) was administered to assess distinct alcohol use patterns. A 15-item self-report measure, the DMQ includes three drinking motive scales: Social (drink to socialize and interact with others) (α = .90), Coping (drink to cope with emotional and other problems) (α = .89), and Enhancement (drinking to augment positive feelings) (α = .89). Participants also completed the Short Drug Abuse Screening Test (SDAST; Skinner, 1982), a 20-item questionnaire (α = .86) that assesses symptoms of drug abuse and dependence.
Internalizing distress
Inmates completed the Beck Depression Inventory (BDI; Beck et al., 1961), a 21-item questionnaire (α = .86) that measures depression symptomology during the last 2 weeks. Participants also completed the Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990), a 16-item scale (α = .88) assessing subjective worry that correlates with other self-report anxiety measures (Hopko et al., 2003). Additionally, inmates completed the muscular tension, autonomic arousal, and feelings of anxiety scales of the Fenz-Epstein Questionnaire (FEQ; Fenz & Epstein, 1965) that provided prison researchers with a total anxiety score (α = .86). Participants also completed the 52-item Fear Survey Schedule III (FSS-III; Arrindell, Emmelkamp, & van der Ende, 1984), which yields a total score (α = .94) and five subscale scores: social fears; agoraphobia; fears of bodily injury, death, and illness; fears of sexual and aggressive scenes; and fears of harmless animals. Finally, we determined if there was a history of suicide attempts from the clinical interview and prison files.
Normal personality functioning
We examined associations between MBPD scores and normal personality trait constructs via six well-validated self-report measures:
Neuroticism-Extraversion-Openness Five Factor Inventory (NEO-FFI). The 60-item NEO-FFI (Costa & McCrae, 1992) assesses the “Big Five” model of normal personality. This instrument provides scores on five trait constructs: Neuroticism (α = .79), Extraversion (α = .63), Openness (α = .68), Agreeableness (α = .70), and Conscientiousness (α = .82).
Emotionality-Activity-Sociability-Impulsivity Temperament Survey (EASI). The 25-item EASI was developed by Buss and Plomin (1975) to measure their model of temperament traits. Emotionality (subscales Distress, Fearfulness, Anger; α = .80, .55, .58, respectively) encompasses a person’s sensitivity and reaction to negative emotions. Activity (α = .56) refers to the pace of a person’s life. Sociability (α = .56) measures an individual’s fondness for personal interactions. Impulsivity (α = .53) identifies a tendency to act before thinking.
Positive and Negative Affect Schedule (PANAS)-Trait Version. This instrument (Watson, Clark, & Tellegen, 1988) examines the frequency various mood states are experienced. PANAS Positive Affect scores (α = .84) measure pleasurable states in a person’s life, while PANAS Negative Affect scores (α = .84) quantify negativity.
Anger Expression Questionnaire (AEQ). This 20-item inventory (α = .78; Spielberger, 1988) assesses anger expression and regulation.
Socialization (So) scale. This 54-item instrument is a subscale of the California Psychological Inventory (α = .68; Gough, 1957, 1960). This measure of antisocial tendencies sorts individuals in a stepwise fashion on a spectrum from model citizens to incarcerated offenders.
Sensation Seeking Scale (SSS). This 40-item measure (Zuckerman, 1979) examines behavioral disinhibition and risk-taking tendencies. The SSS yields a total score and four subscale scores: Disinhibition (α = .59), Boredom Susceptibility (α = .64), Thrill and Adventure Seeking (α = .81), and Experience Seeking (α = .80).
Measures Administered To Female Prisoners
The female inmates completed the very similar self-report measures of substance use and abuse to that filled out by the male inmates. All women received the self-report measures of substance use and abuse (SADU, DMQ, ADS, and SDAST), and indices of antisocial, criminal, and violent behavior (CD, AAB, criminality, violence composite) that were derived from the clinical interview and from a review of prison file data available for each participant. The ICCs for AAB and CD diagnoses were .85 and .91, respectively. History of suicide attempts (coded as present or absent) was also assessed from the interview and review of the prison file (Verona et al., 2005). The mean inter-item correlations for the violence composite and the SADU were both .26. Cronbach’s alphas for the female sample were as follows: ADS (α = .93); DMQ-social (α = .88); DMQ-coping (α = .92); DMQ-enhancement (α = .94); SDAST (α = .93).
Two additional instruments were also administered to assess trauma and symptoms of posttraumatic stress disorder (PTSD). Lifetime exposure to traumatic events was assessed using the Life Events Checklist (Gray et al., 2004). Given that traumatic events related to abuse and assaults are most relevant to BPD, we computed an overall index of traumatic events as the sum of all endorsed events on the checklist, as well as scores for subscales reflecting only the abuse and assault items (i.e., childhood physical or sexual abuse, and physical or sexual assault as an adult; mean inter-item correlation = .32). Symptoms of PTSD were assessed using the civilian version of the PTSD Checklist (α = .92; Weathers et al, 1993), a self-report questionnaire in which participants rated the extent to which each of the 17 symptoms of PTSD was experienced during the past month. Finally, mental health treatment history was collected from prisoner interviews and prison files. A composite treatment measure was calculated by summing the presence (yes = 1, no = 0) of the following indicators: treatment outside prison, treatment inside prison, history of psychiatric hospitalization, and history of taking medications for anxiety (mean inter-item correlation = .25).
Results for Male Prisoners
Table 4 lists the correlations between MBPD and the criterion variables for all prisoners. For males, MBPD scores exhibited modest associations with CD, AAB, and the violent behavior composite. MBPD scores also exhibited small to moderate associations with scores on the SADU, ADS, SDAST, and the DMQ Coping scale. For measures of internalizing distress, MBPD scores exhibited moderate to large associations with scores on the BDI, PSWQ, FEQ, most FSS subscales, particularly the Social Fears and Agoraphobia scales, and a history of suicide attempts.
For normal personality traits, MBPD scores evidenced associations with scores on measures of negative affect, including NEO-FFI Neuroticism; EASI Distress, Fearfulness, and Anger subscales; PANAS Negative Affect; and the Anger Expression Questionnaire. MBPD scores were negatively correlated with measures of positive affect, including PANAS Positive Affect, NEO-FFI Extraversion, and EASI Sociability. There were small to moderate positive correlations with indices of behavioral disinhibition, including EASI Impulsivity and SSS Boredom Susceptibility and Disinhibition scales. Similarly, the MBPD was negatively associated with measures of socialization, including NEO-FFI Agreeableness, NEO-FFI Conscientiousness, and CPI Socialization. In sum, as expected, the MBPD correlated with antisociality, alcohol and drug use, behavioral disinhibition, negative affect, suicidality, and boredom susceptibility.
Results for Female Prisoners and Gender Differences
With regard to mean-level gender differences, females scored significantly higher than men. For males the mean (SD) was 6.32 (4.04); for females it was 8.03 (4.24) (Cohen’s d = −.41, p < .01). Table 4 lists the correlations between MBPD scores and criterion variables in the female prisoner sample. In addition to results that generally parallel those obtained for the men for measures both samples had in common, MBPD scores exhibited moderate associations with history of mental health treatment and trauma exposure (total trauma count and assaults) as well as a strong association with symptoms of PTSD.
Finally, we examined gender differences in mean scores and the strength of the correlations between MBPD scores and external criterion variables. There was a significant gender difference in MBPD mean scores, with women scoring higher than men [F(1,454) = 19.31, p < .001)]. As seen in Table 4, women also exhibited significantly higher correlations between MBPD scores and Conduct Disorder symptoms, criminal charges before age 17, age of first offense, and the DMQ Coping and Enhancement scales (all ps < .01) (see Table 4 for contrast z statistics). There were trend level differences (in the same direction) for the violent behavior composite and the DMQ Social scale (ps = .08 and .06, respectively).
Incremental Validity of MBPD
As with the substance user sample, we examined whether MBPD scores explained anything beyond negative affectivity. We conducted a series of hierarchical regressions with gender and Negative Emotionality scores entered in the first step, MBPD scores entered in the second step, and the external correlates of BPD entered as criterion variables. Given the sheer number of variables in the two prison samples, we used only variables that conceptually overlapped with Study 1 (i.e., AAB child and adult symptoms, indices of EXT, and drug and alcohol misuse). MBPD scores were incrementally predictive of CD symptoms (R2Δ = .009, p < .01), the ADS (R2Δ = .023, p < .01), the SDAST (R2Δ = .014, p < .01), and a history of suicide attempts (OR = 1.18, p < .001). However, the MTSD-BPD was not predictive of AAB symptoms (R2Δ = .001, p = .21).
Some variables—including PTSD and indices of INT—were only assessed among male or female prisoners. We conducted similar incremental analyses because of the theoretical relevance of such variables (although these analyses controlled for negative emotionality only). We examined the incremental validity of MBPD scores on PTSD symptoms among women and on BDI (as an index of INT) among men. MBPD scores were predictive of PTSD symptoms (R2Δ = .027, p < .01) and of the BDI (R2Δ = .056, p < .01). These results provide additional evidence of incremental validity beyond measures of negative affect.
Study 2 Discussion
Consistent with previous evidence documenting the correlates of BPD in psychiatric and substance user samples (Bornovalova et al, 2006; Gratz et al, 2008; Zanarini et al, 1997, 1998a, 1998b), MBPD scores were associated with externalizing behavior, internalizing distress, substance use frequency and severity, and traumatic experiences. Associations between MBPD scores and normal range personality traits also mirrored previous results (Trull et al, 2003; Costa & McCrae, 1990), including measures of negative affectivity, poor socialization, and behavioral disinhibition across a number of personality inventories. Thus, the MBPD scale exhibited good convergent validity with relevant external correlates in the prisoner sample. MBPD scores also predicted measures of psychopathology and maladaptive behavior, even when controlling for negative emotionality. These results validate the utility of the MBPD in samples at elevated risk for BPD.
General Discussion
The current study developed and tested the construct validity of a new self-report measure of BPD, the MBPD. To restate a crucial point, the ultimate goal of this scale development study was pragmatic, in that we aimed to develop an index of BPD traits from a measure that is in common use (the MPQ), including in several important epidemiological investigations. By incorporating data from multiple large samples, spanning a diverse range of participants, and employing criterion measures of various types, the current pair of studies provided for a rigorous assessment of the validity of this new self-report BPD scale. In turn, the development of this novel scale allows researchers to calculate an index of BPD and answer questions that, for practical and financial considerations, cannot be answered in general BPD studies – for instance, questions about the longitudinal course, heritability, or genomic markers associated with BPD.
Construct Validity and Incremental Validity
First, our results indicated that the MBPD has strong internal consistency reliability across all the samples in this study (average α = .81). Second, it strongly correlated with other self-report BPD measures and moderately correlated with diagnosed BPD. The incremental validity analyses suggest the MBPD provides valuable clinical information beyond measuring negative emotionality, because across the study samples, the MBPD accounted for significant variance beyond MPQ Negative Emotionality.
External Correlates of MBPD
Consistent with previous research and our study hypotheses, results for the MBPD indicate significant association with indices of behavioral disinhibition, including measures of antisocial behavior, criminality, violence, substance abuse, and disinhibitory personality traits. The MBPD scores also correlated with measures of internalizing psychopathology and childhood and adult trauma. As a whole, then, scores on the MBPD scale behaved in a manner consistent with how the BPD construct as indexed by DSM criteria is known to behave; as such, the current data provide strong evidence for the construct validity of MBPD as a measure of the larger BPD construct.
Gender Differences
Notably, the current study also examined gender differences in the strength of associations of MBPD with external criterion variables. Although gender differences were not observed in the sample of community adult youth, there were gender differences within the two samples of prisoners (and the substance user sample was too small to detect differences). These disparate results are not surprising given the equivocality in the research literature about the linkage between gender and BPD correlates (Golomb, Fava, Abraham, & Rosenbaum, 1995; Grilo, 2002; Johnson et al, 2003; Zlotnick, Rothschild, & Zimmerman, 2002; Zanarini et al, 1998a). Since the studies that found gender differences in the correlates of BPD generally used adult clinical samples, the disparity across (our) samples might stem from differences in sample characteristics (age, SES, and prevalence of clinical disorders including substance use problems) as well.
Despite the multiple strengths of the study, several limitations should also be acknowledged. First, we do not claim that the MBPD scale, specifically created for the use in existing studies that included the MPQ, would necessarily work as well as a scale constructed from scratch using a clinical BPD group. Second, because the MTFS and prisoner studies lacked a direct measure of BPD, we utilized correlations with relevant criterion variables to infer validity of the MBPD scale. Third, as suggested by Dulit et al (1990), a diagnosis of BPD in the urban drug user sample might be confounded by long-standing substance use. Nevertheless, Dulit et al. found that even after accounting for substance abuse symptoms that overlapped with BPD symptoms, the rate of BPD among substance abusers remained high (67%), adding confidence that a diagnosis of BPD in such individuals is not wholly attributable to substance misuse. Finally, the study analyses also did not examine the discriminant validity or the test-retest reliability of the MBPD – a clear direction for follow-up work.
Despite the above limitations, the current study successfully developed a new self-report measure of BPD tendencies that demonstrated good validity across several conceptually and clinically relevant criteria. This work provides a basis for researchers to index BPD tendencies using items from a broadband inventory of normal personality that has been administered in large-scale longitudinal epidemiological studies (Iacono et al., 1999; Krueger et al., 1998; Silva, 1990; Roberts, Caspi, & Moffitt, 2001). Using the MPQ-based BPD scale developed here, follow-up investigations can answer a number of interesting questions. First, employing data from existing large-scale studies can be used to examine such questions as longitudinal change in BPD levels, the influence of co-occurring psychopathology (e.g., substance use) on temporal stability and change, and the relationship of BPD tendencies early in life to psychological adjustment and adaptive functioning in later years. Moreover, the current study sets the stage for novel work that draws on the unique features in the longitudinal datasets that administer the MPQ. For instance, the MTFS includes monozygotic and dizygotic twin and family data, as well as molecular genetic information. The MBPD scale then will allow for quantitative genetic and molecular genetic studies of BPD. Work of this kind is likely to contribute substantially to knowledge of the etiology of BPD, and in turn, to methods for preventing and treating this very serious and debilitating disorder.
Acknowledgments
This work was supported by National Institute on Drug Abuse grant DA05147, National Institute on Alcohol Abuse and Alcoholism grants AA09367 and AA015621, and National Institutes on Mental Health grants MH072850, MH089727, and T32 MH017069.
Footnotes
No conflict of interest exists for any of the authors.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Revised. 3. Washington, DC: 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington D. C: 1994. [Google Scholar]
- Arrindell WA, Emmelkamp PMG, van der Ende J. Phobic dimensions: I. Reliability and generalizability across samples, gender and nations. Advances in Behaviour Research and Therapy. 1984;6:207–245. [Google Scholar]
- Bachman JG, Johnston LD, O’malley PM. Monitoring the Future 1988. Ann Arbor: Institute for Social Research; 1991. [Google Scholar]
- Ball SA, Tennen H, Poling JC, Kranzler HR, Rounsaville BJ. Personality, temperament, and character dimensions and the DSM-IV personality disorders in substance abusers. Journal of Abnormal Psychology. 1997;106:545–553. doi: 10.1037//0021-843x.106.4.545. [DOI] [PubMed] [Google Scholar]
- Barratt E. Impulsive subtraits: Arousal and information processing. In: Spence JT, Izard CE, editors. Motivation, emotion, and personality. New York: Elsevier Science Publisher; 1985. pp. 137–146. [Google Scholar]
- Barratt ES, Pattonj H. Impulsivity: Cognitive, behavioral, and psychophysiological correlates. In: Zuckerman M, editor. Biological bases of sensation seeking, impulsivity and anxiety. Hillsdale, NJ: Erlbaum; 1983. pp. 77–116. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benning SD, Patrick CJ, Iacono WG. Psychopathy, startle blink modulation, and electrodermal activity in twin men. Psychophysiology. 2005;42:753–762. doi: 10.1111/j.1469-8986.2005.00353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benning SD, Patrick CJ, Blonigen DM, Hicks BM, Iacono WG. Estimating facets of psychopathy from normal personality traits: A step toward community-epidemiological investigations. Assessment. 2005;12:3–18. doi: 10.1177/1073191104271223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Porath YS, Almagor M, Hoffman-Chemi A, Tellegen A. A cross-cultural study of personality with the Multidimensional Personality Questionnaire. Journal of Cross-Cultural Psychology. 1995;26:360–373. [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Billing JP, Hershberger SL, Iacono WG, et al. Life events and personality in late adolescence: genetic and environmental relations. Behaviour Genetics. 1996;26:543–554. doi: 10.1007/BF02361227. [DOI] [PubMed] [Google Scholar]
- Bohus M, Limberger MF, Frank U, Sender I, Gratwohl T, Stieglitz RD. Entwicklung der Borderline-Symptom-Liste (Development of the borderline symptom list) Psychotherapy and Psychosomatic Medicine Psychology. 2001;51:201–211. doi: 10.1055/s-2001-13281. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Nick B, Delaney-Brumsey A, Lynch TR, Kosson D, Lejuez CW. A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. Journal of Psychiatric Research. 2008;42:717–26. doi: 10.1016/j.jpsychires.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Delany-Brumsey A, Paulson A, Lejuez CW. Temperamental and environmental risk factors for borderline personality disorder among inner-city substance users in residential treatment. Journal of Personality Disorders. 2006;20:218–231. doi: 10.1521/pedi.2006.20.3.218. [DOI] [PubMed] [Google Scholar]
- Bouchard TJ, Jr, Lykken DT, McGue M, Segal NL, Tellegen A. Sources of human psychological differences: The Minnesota Study of Twins Reared Apart. Science. 1990;250:223–228. doi: 10.1126/science.2218526. [DOI] [PubMed] [Google Scholar]
- Buss AH, Plomin R. A temperament theory of personality development. New York: Wiley Interscience; 1975. [Google Scholar]
- Casillas A, Clark LA. Dependency, impulsivity, and self-harm: Traits hypothesized to underlie the association between cluster B personality and substance use disorders. Journal of Personality Disorders. 2002;16:424–436. doi: 10.1521/pedi.16.5.424.22124. [DOI] [PubMed] [Google Scholar]
- Casillas A, Clark LA. Dependency, impulsivity, and self-harm: Traits hypothesized to underlie the association between cluster B personality and substance use disorders. Journal of Personality Disorders. 2002;16:424–436. doi: 10.1521/pedi.16.5.424.22124. [DOI] [PubMed] [Google Scholar]
- Caspi A, Begg D, Dickson N, Harrington H, Langley J, Moffitt TE, Silva PA. Personality differences predict health-risk behaviors in young adulthood: Evidence from a longitudinal study. Journal of Personality and Social Psychology. 1997;73:1052–1063. doi: 10.1037//0022-3514.73.5.1052. [DOI] [PubMed] [Google Scholar]
- Church AT, Burke PL. Exploratory and confirmatory tests of the Big Five and Tellegen’s three- and four-dimensional models of personality structure. Journal of Personality and Social Psychology. 1994;66:93–114. doi: 10.1037//0022-3514.66.1.93. [DOI] [PubMed] [Google Scholar]
- Clark LA. Manual for the Schedule for Nonadaptive and Adaptive Personality (SNAP) Minneapolis: University of Minnesota Press; 1993. [Google Scholar]
- Clarkin JF, Hull JW, Cantor J, Sanderson C. Borderline personality disorder and personality traits: a comparison of SCID-II BPD and NEO-PI. Psychological Assessment. 1993;5:472–476. [Google Scholar]
- Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Archives of General Psychiatry. 1993;50:975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4:23–132. [Google Scholar]
- Costa PT, McCrae RR. Personality disorders and the five factor model of personality. Journal of Personality Disorders. 1990;4:362–371. [Google Scholar]
- Costa PT, McCrae RR. Normal Personality Assessment in Clinical Practice: The NEO Personality Inventory. Psychological Assessment. 1992;4:5–13. [Google Scholar]
- Cottler LB, Campbell W, Krishna VAS, Cunningham-Williams RM, Ben Abdallah A. Predictors of high rates of suicidal ideation among drug users. Journal of Nervous and Mental Disease. 2005;193(7):431–437. doi: 10.1097/01.nmd.0000168245.56563.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Moor MHM, Distel MA, Trull TJ, Boomsma DI. Assessment of Borderline Personality Features in Population Samples: Is the Personality Assessment Inventory-Borderline Features Scale Measurement Invariant Across Sex and Age? Psychological Assessment. 2009;21:125–130. doi: 10.1037/a0014502. [DOI] [PubMed] [Google Scholar]
- Donnellan MB, Assad KK, Robins RW, Conger RD. Do negative interactions mediate the effects of negative emotionality, communal positive emotionality, and constraint on relationship satisfaction? Journal of Social and Personal Relationships. 2007;24:557–73. [Google Scholar]
- Donnellan MB, Conger RD, Burzette RG. Personality development from late adolescence to young adulthood: Differential stability, normative maturity, and evidence for the maturity-stability hypothesis. Journal of Personality. 2007;75:237–263. doi: 10.1111/j.1467-6494.2007.00438.x. [DOI] [PubMed] [Google Scholar]
- Donnellan MB, Assad KK, Robins RW, Conger RD. Do negative interactions mediate the effects of Negative Emotionality, Communal Positive Emotionality, and Constraint on relationship satisfaction? Journal of Social and Personal Relationships. 2007;24:557–573. [Google Scholar]
- Dougherty DM, Bjork JM, Huckabee HCG, Moeller FG, Swann AC. Laboratory measures of aggression and impulsivity in women with borderline personality disorder. Psychiatry Research. 1999;85:315–326. doi: 10.1016/s0165-1781(99)00011-6. [DOI] [PubMed] [Google Scholar]
- Dulit RA, Fryer MR, Haas GL, Sullivan T, Frances AJ. Substance use in borderline personality disorder. American Journal of Psychiatry. 1990;147:1002–1007. doi: 10.1176/ajp.147.8.1002. [DOI] [PubMed] [Google Scholar]
- Evren C, Sar V, Evren B, Dalbudak E. Self-mutilation among male patients with alcohol dependency: the role of dissociation. Comprehensive Psychiatry. 2008;49(5):489–495. doi: 10.1016/j.comppsych.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Fenz WD, Epstein S. Manifest anxiety: Unifactorial or multifactorial composition? Perceptual and Motor Skills. 1965;20:773–780. doi: 10.2466/pms.1965.20.3.773. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. User’s guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I Disorders: Non-patient edition (SCID-NP, v. 2.0) New York: NY State Psychiatric Institute; 1996. [Google Scholar]
- Fleming J, Mullen PE, Sibthorpe B, Attewell R, Bammer G. The relationship between childhood sexual abuse and alcohol abuse in women: a case control study. Addiction. 1998;93:1787–98. doi: 10.1046/j.1360-0443.1998.931217875.x. [DOI] [PubMed] [Google Scholar]
- Frankenburg FR, Zanarini MC. The association between borderline personality disorder and chronic medical illnesses, poor health-related lifestyle choices, and costly forms of health care utilization. Journal of Clinical Psychiatry. 2004;65:1660–1665. doi: 10.4088/jcp.v65n1211. [DOI] [PubMed] [Google Scholar]
- Fulwiler C, Forbes C, Santangelo SL, Folstein M. Self-mutilation and suicide attempt: Distinguishing features in prisoners. Journal of the American Academy of Psychiatry and the Law. 1997;25(1):69–77. [PubMed] [Google Scholar]
- Ge XJ, Conger RD. Adjustment problems and emerging personality characteristics from early to late adolescence. American Journal of Community Psychology. 1999;27:429–459. doi: 10.1023/A:1022238227937. [DOI] [PubMed] [Google Scholar]
- Gibson HB. Self-reported delinquency among schoolboys, and their attitudes to police. British Journal of Social and Clinical Psychology. 1967;6:168–173. doi: 10.1111/j.2044-8260.1967.tb00517.x. [DOI] [PubMed] [Google Scholar]
- Golomb M, Fava M, Abraham M, Rosenbaum JF. Gender differences in personality disorders. American Journal of Psychiatry. 1995;152(4):579–582. doi: 10.1176/ajp.152.4.579. [DOI] [PubMed] [Google Scholar]
- Gough HG. California Psychological Inventory manual. Palo Alto, CA: Consulting Psychologists Press; 1957. [Google Scholar]
- Gough HG. Theory and measurement of socialization. Journal of Consulting Psychology. 1960;24:23–30. [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Smith SM, Dawson DA, Pulay AJ, Pickering RP, Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69(4):533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Baruch DE, Bornovalova MA, Lejuez CW. Factors associated with co-occurring borderline personality disorder among inner-city substance users: the roles of childhood maltreatment, negative affect intensity/reactivity, and emotion dysregulation. Comprehensive Psychiatry. 2008;49:603–615. doi: 10.1016/j.comppsych.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Grilo CM. Are there gender differences in DSM-IV personality disorders? Comprehensive Psychiatry. 2002;43(6):427–430. doi: 10.1053/comp.2002.35907. [DOI] [PubMed] [Google Scholar]
- Gunderson JG. Borderline personality disorder: A clinical guide. Washington, D.C: American Psychiatric Press; 2001. [Google Scholar]
- Hochhausen NM, Lorenz AR, Newman JP. Specifying the impulsivity of female inmates with borderline personality disorder. Journal of Abnormal Psychology. 2002;111:495–501. [PubMed] [Google Scholar]
- Hopko DR, Stanley MA, Reas DL, Wetherell JL, Beck JG, Novy DM, et al. Assessing worry in older adults: Confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychological Assessment. 2003;15(2):173–183. doi: 10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Morey LC, Edelen MO, Shea MT, Grilo CM, Sanislow CA, et al. A comparison of interview and self-report methods for the assessment of borderline personality disorder criteria. Psychological Assessment. 2008;20:81–85. doi: 10.1037/1040-3590.20.1.81. [DOI] [PubMed] [Google Scholar]
- Hyler SE. Personality Questionnaire, PDQ-41. NewYork, NY: New York State Psychiatric Institute; 1994. [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-case disorders: Findings from the Minnesota Twin Family Study. Development and Psychopathology. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Jacobo MC, Blais MA, Baity MR, Harley R. Concurrent validity of the Personality Assessment Inventory borderline scales in patients seeking dialectical behavior therapy. Journal of Personality Assessment. 2007;88(1):74–80. doi: 10.1080/00223890709336837. [DOI] [PubMed] [Google Scholar]
- Jasinski JL, Williams LM, Siegel JA. Childhood abuse and lack of parental care as risk factors for heavy drinking among African-American women: A prospective study. Child Abuse and Neglect. 2000;24:1061–1071. doi: 10.1016/s0145-2134(00)00158-7. [DOI] [PubMed] [Google Scholar]
- Johnson DM, Shea MT, Yen S, Battle CL, Zlotnick C, Sanislow CA, et al. Gender differences in borderline personality disorder: Findings from the collaborative longitudinal personality disorders study. Comprehensive Psychiatry. 2003;44(4):284–292. doi: 10.1016/S0010-440X(03)00090-7. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women. 2. Convicted felons entering prison. Archives of General Psychiatry. 1996;53:513–519. doi: 10.1001/archpsyc.1996.01830060057008. [DOI] [PubMed] [Google Scholar]
- Kim KJ, Conger RD, Lorenz FO, et al. Parent-adolescent reciprocity in negative affect and its relation to early adult social development. Developmental Psychology. 2001;37:775–790. [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Daughters SB, Nowak JA, Lynch T, Rosenthal MZ, Kosson D. Examining the inventory of interpersonal problems as a tool for conducting analogue studies of mechanisms underlying Borderline Personality Disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34:313–324. doi: 10.1016/j.jbtep.2003.11.002. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Links PS, Heslegrave RJ, Mitton JE, van Reekum R, Patrick J. Borderline personality disorder and substance abuse: Consequences of comorbidity. Canadian Journal of Psychiatry. 1995;40:9–14. doi: 10.1177/070674379504000105. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Archives of General Psychiatry. 1998;55:941–948. doi: 10.1001/archpsyc.55.10.941. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Schroeder ML, Jackson DN. Factorial structure of traits delineating personality-disorders in clinical and general population samples. Journal of Abnormal Psychology. 1992;101:432–440. doi: 10.1037//0021-843x.101.3.432. [DOI] [PubMed] [Google Scholar]
- Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology. 2005;88:139, 157–721. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Miller JD, Lynam DR, Widiger TA, Leukefeld C. Personality disorders as extreme variants of common personality dimensions: Can the Five-Factor Model adequately represent psychopathy? Journal of Personality. 2001;69(2):253–276. doi: 10.1111/1467-6494.00144. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Dougherty DM, Barratt ES, Oderinde V, Mathias CW, Harper RA, et al. Increased impulsivity in cocaine dependent subjects independent of antisocial personality disorder and aggression. Drug & Alcohol Dependence. 2002;68:105–111. doi: 10.1016/s0376-8716(02)00106-0. [DOI] [PubMed] [Google Scholar]
- Morey LC. Personality Assessment Inventory: Professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Paris J. Antisocial and borderline personality disorders: Two separate diagnoses or two aspects of the same psychopathology? Comprehensive Psychiatry. 1997;38:237–242. doi: 10.1016/s0010-440x(97)90032-8. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the multidimensional personality questionnaire. Psychological Assessment. 2002;14(2):150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology. 1995;51(6):768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Kim YY, Proietti JM, Barkham M. Scales for personality disorders developed from the inventory of interpersonal problems. Journal of Personality Disorders. 1996;10:355–369. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reynolds SK, Clark LA. Predicting dimensions of personality disorder from domains and facets of the Five-Factor Model. Journal of Personality. 2001;69(2):199–222. doi: 10.1111/1467-6494.00142. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Caspi A, Moffitt TE. J Personal Soc Psychol. Vol. 81. 2001. The kids are alright: growth and stability in personality development from adolescence to adulthood; pp. 582–93. [PubMed] [Google Scholar]
- Roberts BW, Caspi A, Moffitt TE. The kids are alright: Growth and stability in personality development from adolescence to adulthood. Journal of Personality and Social Psychology. 2001;81(4):670–683. [PubMed] [Google Scholar]
- Robins LN, Baber T, Cottler LB. International Diagnostic Interview: Expanded Substance Abuse module. St. Louis, MO: Author; 1987. [Google Scholar]
- Romero-Daza N, Weeks M, Singer M. “Nobody gives a damn if I live or die”: Violence, drugs, and street-level prostitution in inner-city Hartford, Connecticut. Medical Anthropology. 2003;22:233–259. doi: 10.1080/01459740306770. [DOI] [PubMed] [Google Scholar]
- Saulsman LM, Page AC. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review. 2004;23(8):1055–1085. doi: 10.1016/j.cpr.2002.09.001. [DOI] [PubMed] [Google Scholar]
- Schwartz AC, Bradley RL, Sexton M, Sherry A, Ressler KJ. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatric Services. 2005;56:212–215. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- Segal DL, Hook JN, Coolidge FL. Personality dysfunction, coping styles, and clinical symptoms in younger and older adults. Journal of Clinical Geropsychology. 2001;7:201–212. [Google Scholar]
- Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. American Journal of Psychiatry. 1991;148:1647–1658. doi: 10.1176/ajp.148.12.1647. [DOI] [PubMed] [Google Scholar]
- Siever LJ, Torgersen S, Gunderson JG, Livesley WJ, Kendler KS. The borderline diagnosis III: Identifying endophenotypes for genetic studies. Biological Psychiatry. 2002;51:964–968. doi: 10.1016/s0006-3223(02)01326-4. [DOI] [PubMed] [Google Scholar]
- Silk KR, Lee S, Hill EM, Lohr NE. Borderline symptoms and severity of sexual abuse. American Journal of Psychiatry. 1995;152:1059–1064. doi: 10.1176/ajp.152.7.1059. [DOI] [PubMed] [Google Scholar]
- Silva PA. The Dunedin Multidisciplinary Health and Development Study: a 15 year longitudinal study. Paediatric and Perinatal Epidemiology. 1990;4:76–107. doi: 10.1111/j.1365-3016.1990.tb00621.x. [DOI] [PubMed] [Google Scholar]
- Skinner A. The Drug Abuse Screening Test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: Measurement and validation. Journal of Abnormal Psychology. 1982;91:199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: Psychopathology, comorbidity, and personality structure. Biological Psychiatry. 2002;51:936–950. doi: 10.1016/s0006-3223(02)01324-0. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Oldham JM, Bender DS, Dyck IR, Stout RL, Morey LC, et al. Dimensional Representations of DSM-IV Personality Disorders: Relationships to Functional Impairment. American Journal of Psychiatry. 2005;162:1919–1925. doi: 10.1176/appi.ajp.162.10.1919. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Krasner SS, Solomon EP. The experience, expression, and control of anger. In: Janisse MP, editor. Health psychology: Individual differences and stress. New York: Springer-Verlag; 1988. pp. 89–108. [Google Scholar]
- Stein MB, Pinsker-Aspen JH, Hilsenroth MJ. Borderline pathology and the Personality Assessment Inventory (PAI): An evaluation of criterion and concurrent validity. Journal of Personality Assessment. 2007;88:81–89. doi: 10.1080/00223890709336838. [DOI] [PubMed] [Google Scholar]
- Taylor J, McGue M, Iacono WG, Lykken DT. A behavioral genetic analysis of the relationship between the Socialization scale and self-reported delinquency. Journal of Personality. 2000;68:29–50. doi: 10.1111/j.1467-6494.2000.t01-1-.x. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Unpubhshed manuscript. University of Minnesota; Minneapolis: 1982. Brief manual for the Multidimensional Personality Questionnaire. [Google Scholar]
- Trull TJ. Borderline personality-disorder features in nonclinical young-adults.1. Identification and validation. Psychological Assessment. 1995;7:33–41. [Google Scholar]
- Trull TJ, Sher KJ, Minks-Brown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders: a review and integration. Clinical Psychology Review. 2000;20:235–253. doi: 10.1016/s0272-7358(99)00028-8. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Widiger TA, Lynam DR, Costa PT. Borderline personality disorder from the perspective of general personality functioning. Journal of Abnormal Psychology. 2003;112(2):193–202. doi: 10.1037/0021-843x.112.2.193. [DOI] [PubMed] [Google Scholar]
- Verona E, Hicks BM, Patrick CJ. Psychopathy and suicidality in female offenders: Mediating influences of personality and abuse. Journal of Consulting and Clinical Psychology. 2005;73:1065–1073. doi: 10.1037/0022-006X.73.6.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verona E, Patrick CJ, Joiner TE. Psychopathy, antisocial personality, and suicide risk. Journal of Abnormal Psychology. 2001;110:462–470. doi: 10.1037//0021-843x.110.3.462. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist: Reliability, validity, & diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. Oct, [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Widiger TA, Weissman MM. Epidemiology of borderline personality disorder. Hospital and Community Psychiatry. 1991;42:1015–21. doi: 10.1176/ps.42.10.1015. [DOI] [PubMed] [Google Scholar]
- Winograd G, Cohen P, Chen HN. Adolescent borderline symptoms in the community: prognosis for functioning over 20 years. Journal of Child Psychology and Psychiatry. 2008;49:933–941. doi: 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Vujanovic AA. Inter-rater and test-retest reliability of the revised diagnostic interview for borderlines. Journal of Personality Disorders. 2002;16:270–276. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry. 1998a;155:1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis II comorbidity of borderline personality disorder. Comprehensive Psychiatry. 1998b;39:296–302. doi: 10.1016/s0010-440x(98)90038-4. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Khera GS, Bleichmar J. Treatment histories of borderline inpatients. Comprehensive Psychiatry. 2001;42:144–150. doi: 10.1053/comp.2001.19749. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. Zanarini rating scale for borderline personality disorder (ZAN-BPD): A continuous measure of DSM-IV borderline psychopathology (vol 17, pg 233, 2003) Journal of Personality Disorders. 2003;17:370–370. doi: 10.1521/pedi.17.3.233.22147. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Williams AA, Lewis RE, Reich RB, Vera SC, Marino MF, et al. Reported pathological childhood experiences associated with the development of borderline personality disorder. American Journal of Psychiatry. 1997;154:1101–1106. doi: 10.1176/ajp.154.8.1101. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Yong L, Frankenburg FR, Hennen J, Reich DB, Marino MF, et al. Severity of reported childhood sexual abuse and its relationship to severity of borderline psychopathology and psychosocial impairment among borderline inpatients. Journal of Nervous and Mental Disorders. 2002;190:381–387. doi: 10.1097/00005053-200206000-00006. [DOI] [PubMed] [Google Scholar]
- Zlotnick C. Posttraumatic stress disorder (PTSD), PTSD comorbidity, and childhood abuse among incarcerated women. Journal of Nervous and Mental Disease. 1997;182:761–763. doi: 10.1097/00005053-199712000-00007. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Rothschild L, Zimmerman M. The role of gender in the clinical presentation of patients with borderline personality disorder. Journal of Personality Disorders. 2002;16(3):277–282. doi: 10.1521/pedi.16.3.277.22540. [DOI] [PubMed] [Google Scholar]
- Zuckerman M. Sensation Seeking: Beyond the Optimal Level of Arousal. Lawrence Erlbaum Associates; Hillsdale, NJ: 1979. [Google Scholar]