Introduction
The skeleton is a favorable site for the development of metastases from carcinomas and sarcomas can develop osseous metastatic disease. Bone metastasis distal to elbows and knees are quite rare; metastases to the hand are very rare as well, accounting for only 0.1% of all metastatic lesions [1]. Handley was the first to report this unusual manifestation in 1906 [2]. A recent review of the literature revealed 257 published cases involving bones of the hand [3]. Acral metastases to the phalanges of the hand usually involve a single bone, while those proximal to the phalanges often involve multiple bones [4]. Typically the patient presents with the insidious onset of pain and swelling in the affected anatomic region [5]. Commonly, hand metastases are misdiagnosed as infection or other inflammatory processes [6].
Herein, we report the case of a patient with digital metastasis, initially misdiagnosed and treated as infection. The purpose of this case report is to discuss the diagnostic and therapeutic options of this rare clinical manifestation of metastatic disease.
Case Report
A 75 years old woman referred to our clinic because of infectious-osteomyelitis of the distal phalanx of the middle right finger. The patient was under per-os antibiotic therapy for a week with no signs of clinical improvement. At the time of referral, the patient had a swollen, erythematous digit (Fig. 1). Mild tenderness was noticed upon palpation. The patient recalled a progressive fusiform expansion of the pulp of the third digit during the last 3 months, accompanied by intermittent pain. Pain became more constant the last month, and it was more intense during night hours. The patient did not have raised temperature during the past week. Axillary regional nodes were not palpable. Patient’s medical history was important for diabetes mellitus and non-small cell lung cancer. Diagnosis of non metastatic lung cancer was established 6 years ago. The patient had received chemotherapy with good clinical response at that time. X-ray of the hand demonstrated a destructive lesion of the last phalanx with diffuse edema of the surrounding soft tissues (Fig. 2). Bone scan was hot only at the involved phalanx and around the proximal inter-phalangeal (PIP) joint. CT examination of lung abdomen and pelvis revealed no obvious metastatic disease. White blood cell count was 9,500 K/μl and ESR was 45 mm/hour. Differential diagnosis essentially included bone metastasis and infection. A core needle biopsy was performed and the sample was sent for histologic examination and culture. The cultures of the material were negative. However, evaluation of the bioptic material revealed metastatic adenocarcinoma.
Fig. 1.
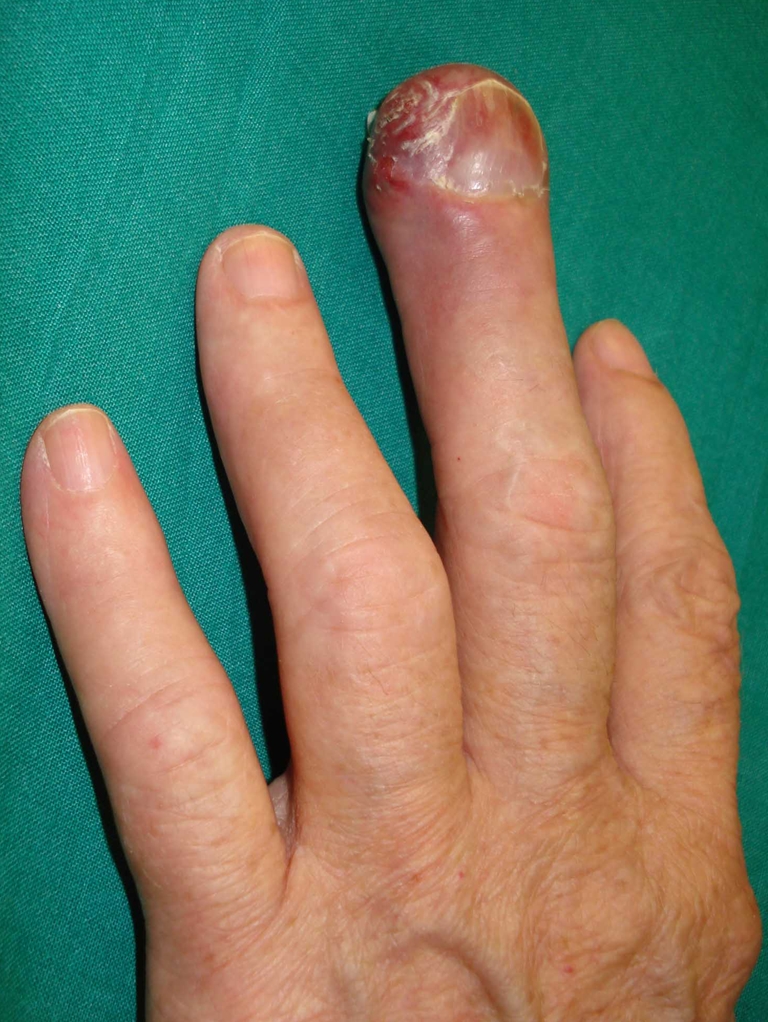
Swelling and erythematous appearance of the third digit extending to the level of the palmar surface of proximal inter-phalangeal joint
Fig. 2.

AP x-ray demonstrating severe destruction of terminal phalanx of the middle digit
Taking into account the severity of bone destruction and the medical history of the patient, surgical resection of the lesion was considered as the appropriate type of treatment. The patient underwent third ray amputation. The third metacarpal bone and phalanges with their extensor and flexor tendons, digital nerve and vessels was excised en block. Only the base of the metacarpal bone was left in order to maintain the width of the palm. Distally the deep intervolar plate ligaments of the metacarpal heads were sutured together to close the space between the index and long fingers. The specimen was submitted for final pathologic evaluation. Following histological and immunohistochemical analyses of the resected specimen, a diagnosis of metastatic lung adenocarcinoma was made.
The patient followed an uneventful post operative period. Two months later the patient had painless unrestricted daily living use of her hand. Eight months later disseminated metastatic disease at the liver and brain developed and the patient deceased 15 months after hand surgery.
Discussion
Acral metastasis is a rare metastatic manifestation. Men are involved twice as often as women [3]. The distal phalanx of the third digit at the right hand is most frequently affected. The reason for this predilection is unclear. Ten percent of the patients develop metastasis in both hands [1]. Flyn et al have documented that lung cancer is the most common primary malignancy (44% of the cases), followed by kidney and breast carcinomas [3]. It is well known that bone is a fertile microenvironment that favors metastasis from several primary cancers. However, the molecular mechanisms involved in this phenomen have not been clarified yet. Several theories have been proposed in order to interpretate why specific tumors more often metastasize to the dominant hand, including repetitive microtrauma and increased blood flow; nevertheless, none of these definitely answer to this question [7]. Recent literature rather correlates metastatic disease and disease progression to the amount of circulating tumor cells [8].
In the clinical setting, digital metastases usually presents as erythematous, warm, and swollen digits. Although these lesions rarely can be painless [9], the patients frequently experience dull and aching pain that is often nocturnal [5]. Differential diagnosis primarily includes infectious or inflammatory processes, bone or soft tissue metastases as well as primary tumors [1, 5, 10–13]. It is not uncommon for the initial diagnosis to be a felon, osteomyelitis, gout, rheumatoid arthritis or squamous cell carcinoma. Especially when the diagnosis of the primary malignancy is not established, acral metastases are usually misdiagnosed as soft tissue or bone infections [5, 10]. As a rule, biopsy and culture of the lesion is required to establish the correct diagnosis [12].
On plain x-rays most metastases are lytic with permeative or destructive appearance. MRI studies are valuable in revealing soft tissue extension, tendon and neurovascular bundle involvement, facilitating surgical treatment plan. Once the diagnosis of acral metastasis is confirmed, a systematic survey for disseminated metastatic disease should be performed. A Technetium bone scan is useful for determining the presence of metastatic lesions in other skeletal locations [14]. Almost 50% of patients presenting with acral metastasis have pulmonary involvement at presentation [15]. This is the reason why acral metastases carries a dismal prognosis and most patients have a life expectancy of 6 months [1]. Although bone metastasis heralds a disseminated metastatic disease, some patients present with a low metastatic burden. These patients should not be considered as end stage patients, as better survival has been reported [3, 5, 16].
Local treatment options are radiation therapy (RT) and resection of metastasis [3, 10, 15]. For small lesions of the distal phalanx, amputation of the terminal part of the digit is adequate for pain and local disease control. The ability to perform a local excision is limited by the small amount of available tissue and the local extension of the tumor. Erosion of the cortex allows for invasion of the tumor into the surrounding soft tissues, into the pulp of the digit and through the deep flexor tendon attachment and its sheath, at more proximal palmar areas [17]. For these cases, in order to achieve good oncological margins, digital ray amputation is necessary. For more proximal lesions, although local resection can be performed, especially at central metacarpals, digital ray amputation provides better tumor control and functional result with acceptable aesthetic appearance of the hand [18, 19].
In our case, the distal phalanx was severely destructed and the tumor was spread proximally through the flexor tendon sheath, producing swelling and redness of the palmar soft tissues up to the level of the PIP joint. Surgical treatment and resection of the lesion was the only appropriate local treatment option. However, resection of the lesion to healthy soft tissue margin necessitated an amputation through the proximal inter-phalangeal joint and closure of the stump with a dorsal flap. However, such an amputation results in a non-functional digit and a digital ray amputation was preferred.
The intent of RT is mainly pain relief. After RT, progressive calcification of the lesion can be seen in radiosensitive tumors, increasing the mechanical strength of a bone lytic lesion. Although surgical treatment is preferred, relatively small metastasis located at the metacarpal bones can be treated with RT. Radiation therapy and splinting is preferable for patients who are not good candidates for surgery because of their medical status or with short life expectancy.
The present report describes an uncommon case of bone metastasis to the digit. It also highlights the need to maintain an index of suspicion that inflammatory lesions of the hand can represent metastatic disease. Local treatment aims to pain relief, local disease control and restoration of a functional hand. Local excision or digital ray amputation, as needed, is the preferred surgical option.
References
- 1.Kerin R. Metastatic tumours of the hand. A review of the literature. J Bone Joint Surg Am. 1983;65:1331–1335. [PubMed] [Google Scholar]
- 2.Handley WS. Cancer of the breast and its operative treatment. London: Murray; 1906. [Google Scholar]
- 3.Flynn CJ, Danjoux C, Wong J, Christakis M, Rubenstein J, Yee A, et al. Two cases of acrometastasis to the hands and review of the literature. Curr Oncol. 2008;15:51–58. doi: 10.3747/co.v15i5.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bahk WJ, Rhee SK, Kang YK, Lee AH, Park JM, Chung YG. Gastric cancer acrometastases to all digits of one hand following closed intramedullary nailing. Skeletal Radiol. 2006;35:529–532. doi: 10.1007/s00256-005-0047-3. [DOI] [PubMed] [Google Scholar]
- 5.Hsu CS, Hentz VR, Yao J. Tumours of the hand. Lancet Oncol. 2007;8:157–166. doi: 10.1016/S1470-2045(07)70035-9. [DOI] [PubMed] [Google Scholar]
- 6.Hayden RJ, Sullivan LG, Jebson PJ. The hand in metastatic disease and acral manifestations of paraneoplastic syndromes. Hand Clin. 2004;20:335–343. doi: 10.1016/j.hcl.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Papachristou DJ, Basdra EK, Papavassiliou AG (2010) Bone metastases: Molecular mechanisms and novel therapeutic interventions. Med Res Rev. Sept 3 [DOI] [PubMed]
- 8.Cohen DE, SJ AKR, Meropol NJ. Circulating tumor cells: evolving evidence and future challenges. Oncologist. 2009;14(11):1070–1082. doi: 10.1634/theoncologist.2009-0121. [DOI] [PubMed] [Google Scholar]
- 9.Sneddon J. Painless metastatic deposit in a finger presenting as a pulp infection with osteitis. Br J Clin Pract. 1969;23:511–513. [PubMed] [Google Scholar]
- 10.Amadio PC, Lombardi RM. Metastatic tumors of the hand. J Hand Surg Am. 1987;12(2):311–316. doi: 10.1016/s0363-5023(87)80299-x. [DOI] [PubMed] [Google Scholar]
- 11.Spiteri V, Bibra A, Ashwood N, Cobb J. Managing acrometastases treatment strategy with a case illustration. Ann R Coll Surg Engl. 2008;90:W8–W11. doi: 10.1308/147870808X303137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993;29:228–236. doi: 10.1016/0190-9622(93)70173-Q. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi E, Kawai A, Endo M, Suehara Y, Takeda K, Nakatani F, et al. Myxoinflammatory fibroblastic sarcoma. J Orthop Sci. 2008;13:566–571. doi: 10.1007/s00776-008-1274-y. [DOI] [PubMed] [Google Scholar]
- 14.Vande Streek P, Carretta RF, Weiland FL, Shelton DK. Upper extremity radionuclide bone imaging: the wrist and hand. Semin Nucl Med. 1998;28:14–24. doi: 10.1016/S0001-2998(98)80016-0. [DOI] [PubMed] [Google Scholar]
- 15.Healey JH, Turnbull AD, Miedema B, Lane JM. Acrometastases. A study of twenty-nine patients with osseous involvement of the hands and feet. J Bone Joint Surg Am. 1986;68:743–746. [PubMed] [Google Scholar]
- 16.Jung ST, Ghert MA, Harrelson JM, Scully SP. Treatment of osseous metastases in patients with renal cell carcinoma. Clin Orthop. 2003;409:223–431. doi: 10.1097/01.blo.0000059580.08469.3e. [DOI] [PubMed] [Google Scholar]
- 17.Enneking WF. Musculoskeletal tumour surgery. Edinburgh: Churchill Livingstone; 1983. [Google Scholar]
- 18.Nuzumlali E, Orhun E, Oztürk K, Cepel S, Polatkan S. Results of ray resection and amputation for ring avulsion injuries at the proximal interphalangeal joint. J Hand Surg Br. 2003;28:578–581. doi: 10.1016/S0266-7681(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 19.Peimer CA, Wheeler DR, Barrett A, Goldschmidt PG. Hand function following a single ray amputation. J Hand Surg Am. 1999;24:1245–1248. doi: 10.1053/jhsu.1999.1245. [DOI] [PubMed] [Google Scholar]


