Abstract
Background
High survival has been reported for resurfacing arthroplasty in patients with femoral deformities. Also, hardware removal may not always be necessary with resurfacing arthroplasty and may eliminate some of the difficulties performing total hip arthroplasty (THA) in patients with posttraumatic osteoarthritis.
Questions/purposes
We therefore asked: (1) are survivorship higher in patients who underwent resurfacing arthroplasty compared with patients with nontraumatic osteoarthritis; and (2) are those higher compared with all patients who have resurfacing?
Methods
We identified 29 patients (29 hips) who had hip resurfacing for posttraumatic arthritis. These were compared with a matched cohort who had hip resurfacings for nontraumatic osteoarthritis and to all patients who underwent hip resurfacing for osteoarthritis during this time. The mean age was 47 years and mean body mass index was 27 kg/m2. Survivorship and Harris hip scores were compared. Radiographs were evaluated for signs of radiolucencies, penciling, or osteolysis. The mean followup was 39 months (range, 24–99 months).
Results
The 5-year survivorship was 90% in the posttraumatic group, 93% in the matched osteoarthritis group, and 97% in the entire osteoarthritis cohort. The mean Harris hip score for the posttraumatic group at last followup was 90 points. Other than the patients who underwent revision, we observed no radiographic radiolucencies or loosening in any of the groups.
Conclusions
The survival of resurfacing arthroplasty appears comparable to THA in posttraumatic osteoarthritis and for resurfacing in patients with osteoarthritis. Therefore, resurfacing may present an alternative treatment to THA in these patients.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Early reports of patients who have received metal-on-metal (MOM) hip resurfacing arthroplasty have demonstrated survival rates from 94% to 99% between 2 and 10 years of followup [1, 2, 5, 9, 11, 13, 14, 16]. Although these reports demonstrate an overall high survival rate, it is uncertain if hip resurfacing arthroplasty is a reasonable treatment alternative to total hip arthroplasty (THA) in patients with posttraumatic arthritis of the hip, specifically after femoral neck or acetabular fractures. Although recent reports have demonstrated similarly high survivorship in patients with expanded indications such as osteonecrosis [9], or developmental deformities of the hip such as Perthes disease and hip dysplasia [4], most resurfacings are performed on patients with primary osteoarthritis.
It is not uncommon for patients with posttraumatic osteoarthritis to ultimately undergo standard THA. This procedure may be difficult as a result of persistent deformity, bone loss, or hardware removal [3]. Survivorships of nearly 80% for standard THA after hip trauma have been reported at various followup intervals [14, 16]. Many of the resulting clinical failures occur because of difficulties that preexisting hardware and bone deficiencies add to the technical aspects of the procedure [14, 15]. For these patients, MOM hip resurfacing arthroplasty may offer an alternative to standard THA. In some cases, a hip resurfacing arthroplasty can be performed without removal of hardware, thereby avoiding some of the difficulties associated with standard THA. Despite the theoretical advantages of retained hardware, increased ease of dealing with deformities, and shortened operative time, these would only provide a benefit to the patient if implant survivorship is comparable or better than THA.
We therefore asked: (1) are survivorship and functional scores higher and radiographic failures lower in patients who underwent resurfacing arthroplasty compared patients with nontraumatic osteoarthritis; and (2) are those parameters higher compared with all patients who have resurfacing?
Patients and Materials
From two institutions we identified all 29 patients (29 hips) who underwent hip resurfacing arthroplasty for posttraumatic osteoarthritis between 2001 and 2007. Of the 29 patients, there were 10 with a history of acetabular trauma and reconstruction (as illustrated in Fig. 1), 16 with a history of femoral trauma (as illustrated in Fig. 2), and three with a history of a traumatic dislocation. Patients were considered to have posttraumatic osteoarthritis if they underwent treatment for prior femoral neck, intertrochanteric, or acetabular fractures. All patients were treated operatively for their trauma with open reduction and internal fixation, percutaneous pinning, or dynamic hip screw implantation. All patients underwent nonoperative treatment for their posttraumatic osteoarthritis and had either Grade 3 or 4 symptomatic osteoarthritis. Contraindications for hip resurfacing arthroplasty included pregnancy, active infection with HIV or hepatitis, documented allergy to cobalt, chromium, or molybdenum, end-stage renal disease, or any neurologic deficit that might adversely affect gait or weightbearing ability. No patients were excluded for any of these criteria. Patients were indicated for THA if they stated a preference for THA over resurfacing or did not have adequate bone stock remaining for implantation of a resurfacing as assessed (by either MAM or TPG) pre- or intraoperatively. We compared these patients with two additional cohorts: (1) a matched cohort of patients who underwent hip resurfacing arthroplasty for nontraumatic osteoarthritis; and (2) all patients who underwent hip resurfacing arthroplasty for nontraumatic osteoarthritis during this time period. Of the 29 patients operated on for posttraumatic osteoarthritis, there were 22 men and seven women with a mean age of 47 years (range, 20–60 years) and a mean body mass index of 27 kg/m2 (range, 19–37 kg/m2). The minimum followup in this group was 24 months (average, 39 months; range, 24–99 months). The second cohort, matched for age (within 5 years) and gender, underwent resurfacing arthroplasty for nontraumatic osteoarthritis (Table 1). This group consisted of 29 hips in 27 patients. There were 20 men and seven women in the matched cohort with a mean age of 42 years (range, 22–52 years) and an average body mass index of 29 kg/m2 (range, 24–37 kg/m2). The minimum followup in this group was 24 months (average, 43 months; range, 24–110 months). In the third cohort, there were 530 patients (622 hips) who underwent resurfacing arthroplasty for all causes. There were 382 men and 148 women with a mean age of 53 years (range, 23–81 years) and a mean body mass index of 28 kg/m2 (range, 16–48 kg/m2). Their minimum followup was 26 months (average, 41 months; range, 26–112 months). Some of these patients were reported on in the past as part of an IDE study at earlier followup [10]. Other patients have been subsets of other reports (eg, patients with developmental dysplasia, osteonecrosis, or Legg-Calvé-Perthes disease). However, all of the patients were uniquely evaluated at latest followup for the present study. No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Institutional Review Board approvals were obtained for this study.
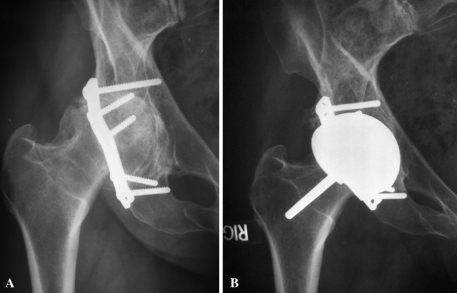
Fig. 1A–B.
AP radiographs are shown of a 49-year-old woman with a history of open reduction and internal fixation of a prior acetabular fracture who underwent hip resurfacing arthroplasty. (A) Preoperative radiograph; (B) radiograph taken 2 years postoperatively (Used with permission from Sinai Hospital of Baltimore, Inc.).
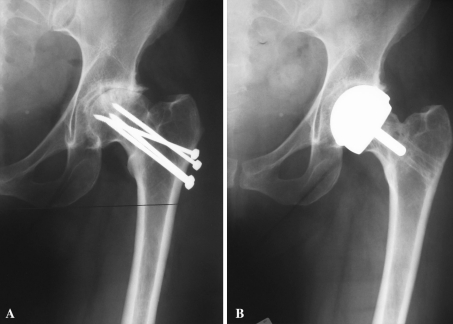
Fig. 2A–B.
AP radiographs are shown of a 45-year-old woman with a history of prior percutaneous pinning of a nondisplaced femoral neck fracture who underwent hip resurfacing arthroplasty. (A) Preoperative radiograph; (B) radiograph taken 2 years postoperatively (Used with permission from Sinai Hospital of Baltimore, Inc.).
Table 1.
A comparison of the demographic and clinical data of the traumatic and nontraumatic osteoarthritis groups
| Data | Posttraumatic OA | Matched nontraumatic OA | All nontraumatic OA |
|---|---|---|---|
| [95% CI] | [95% CI] | ||
| Men (hips) | 22 (22) | 20 (22) | 382 (454) |
| Women (hips) | 7 (7) | 7 (7) | 148 (166) |
| Age in years (range) | 48 (20–63) | 42 (22–52) | 53 (24–81) |
| [44–52] | [40–45] | ||
| Body mass index (range) | 27 (19–37) | 29 (24–37) | 28 (16–48) |
| [25–29] | [28–31] | ||
| Followup period in months (range) | 39 (24–99) | 90 (24–110) | 58 (26–112) |
| [34 to 44] | [83–97] | ||
| Bilateral hip resurfacing (%) | 0 | 2 (7%) | 90 (15%) |
| HHS preoperatively (range) | 54 (30–71) | 57 (31–73) | 54 (31–73) |
| [50–58] | [52–62] | ||
| HHS postoperatively (range) | 90 (58–100) | 90 (49–96) | 91 (49–100) |
| [84–95] | [86–93] | ||
| Survival (%) | 26 (90%) | 27 (93%) | 600 (97%) |
| [73%–98%] | [77%–99%] | [95%–98%] |
OA = osteoarthritis; CI = confidence interval; HHS = Harris hip score.
All surgeries were performed using either an anterolateral approach (MAM) or a posterior approach (TPG) as per the surgeon’s preference. Resurfacing systems included Cormet 2000 (Corin, Ltd, Stryker, Mahwah, NJ), Conserve Plus (Wright Medical, Arlington, TN), and ReCap (Biomet, Warsaw, IN) devices. First, the acetabulum was prepared, reaming to the templated component size, and the cup implanted in a press-fit manner under fluoroscopic guidance. Only necessary hardware for press-fitting an acetabular cup was removed with implantation done in a manner similar to standard THA. The pin-shaft angle was measured with a target angle of 140º (± 5º). Femoral hardware was removed if it was believed to interfere with the femoral component stem (Fig. 2); therefore, 13 of 16 patients retained their femoral hardware. Often, screws could be left in place in the femoral neck if they did not interfere with the femoral component. The femur was then prepared according to manufacturer-specific guidelines and all femoral components were cemented in place. No other special techniques were necessary.
Physical therapy, including strengthening regimens, was initiated on the first postoperative day, and all patients were encouraged to ambulate as tolerated. Weightbearing was restricted to 50% with the aid of a crutch or cane until the 6 weeks postoperatively, at which time the patients were instructed to advance to full weightbearing as tolerated. Physical therapy was performed twice a day during the patient’s hospital stay for mobility training and strengthening, and patients were instructed to perform at-home exercises for strength at least twice a day for the first 3 weeks postoperatively.
Patients were evaluated in the clinic at 3 weeks, 2 months, 6 months, 1 year, and then yearly after surgery. At each visit we performed a clinical examination that included: assessment of any pain (location, quality, intensity), determining whether the patient was able to perform standard activities of daily living, inspection of the operative site (for any signs of irritation, infection, or dehiscence), and measuring ROM, strength, and gait. Standard AP and lateral radiographs were taken at followup visits to evaluate the patient for any signs of radiographic complications, including progressive radiolucencies, femoral neck penciling, or heterotopic ossification. Patient charts were reviewed for any clinical complications, including intraoperative fractures, occurrence of deep-vein thrombosis or pulmonary embolism during the acute postoperative period, and any signs of wound irritation or dehiscence.
All patients were evaluated radiographically at followup visits with sequential assessment allowing for comparison of alignment. Three authors (AJJ, UIM, MAM) independently evaluated all radiographs for radiolucencies using criteria described by DeLee and Charnley [6] for the acetabular component and by various authors for the femoral resurfacing component [1, 4]. Any interobserver variability was discussed among the three evaluators until a consensus was reached regarding interpretation. One or more progressive radiolucencies of at least 2 mm on sequential radiographs were considered positive criteria for component loosening.
Kaplan-Meier survivorship curves were calculated for the matched cohorts of patients with traumatic and nontraumatic osteoarthritis. A log-rank test was used to compare the two curves. Additionally, 95% confidence intervals were calculated to statistically compare the reported mean survivorship and Harris hip scores for all cohorts. We used SigmaStat (SYSTAT, San Jose, CA) for all analyses.
Results
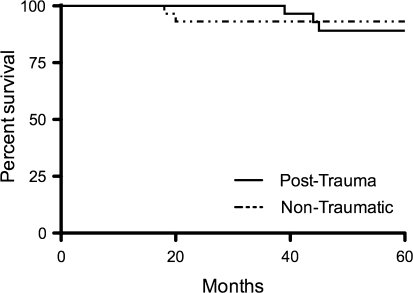
At last followup, three of the 29 hips had undergone revision, resulting in a 90% 5-year survival rate (95% confidence interval [CI], 73%–98%) (Fig. 3), which was similar to the matched cohort (two revisions of 29 hips, 93% 5-year survival rate; 95% CI, 77%–99%) (Fig. 3). Two of the posttraumatic failures were in patients with prior acetabular trauma and the third was in a patient with a history of a proximal femur fracture. There were three failures in the study cohort. Two acetabular components were revised for painful, loose acetabular components (one at 12 months, the other at 24 months). The third was a patient who had a history of open reduction internal fixation for femoral neck fracture and underwent a THA for a femoral neck fracture 36 months after the resurfacing procedure. All patients were doing well at most recent followup. The surviving hips in the posttraumatic resurfacing group had mean Harris hip scores of 90 points at final followup (range, 58–100 points), showing improvement from the mean preoperative score of 54 points (range, 30–71 points). Twenty-three of the surviving hips had Harris hip scores greater than 80 points at most recent followup. In the matched cohort, the mean Harris hip score improved from a preoperative score of 57 points (range, 31–73 points) to 90 points (range, 49–96 points). We found no radiographic evidence of malalignment, progressive lucencies, or femoral neck penciling in either the posttraumatic hip resurfacing group or the matched group that underwent resurfacing for osteoarthritis.
Fig. 3.
A Kaplan-Meier survivorship plot of the matched traumatic and nontraumatic resurfacing cohorts is shown. The estimated 5-year survivorship of the traumatic osteoarthritis cohort was 90% (95% confidence interval [CI], 73%–98%), and the estimated 5-year survivorship of the nontraumatic osteoarthritis cohort was 93% (95% CI, 77%–99%). The log rank characteristic comparing the two survivorship curves was 0.671.
The overall cohort of patients who underwent resurfacing for nontraumatic osteoarthritis had a survivorship of 97% (600 of 620) at a mean followup of 5 years (95% CI, 95%–98%), which was similar to the survivorship of the resurfacings in patients who underwent the procedure for posttraumatic osteoarthritis (90% survival; 95% CI, 73%–98%). The mean Harris hip score in the nontraumatic osteoarthritis cohort improved from a mean preoperative score of 58 points (range, 24–96 points) to a mean postoperative score of 92 points (range, 32–100 points).
Two patients with surviving hip resurfacing arthroplasties had unfavorable Harris hip scores of 58 and 66 points, respectively. Both patients had improvements in their flexion and function scores. One patient showed an increase from 90º to 122° of flexion and from 21 to 26 points; the other increased from 90º to 100° of flexion and from 31 to 47 points for functional scores. One of these patients developed an L4 radiculopathy from L4/L5 spondylolisthesis, resulting in pain and numbness and a subsequent antalgic gait. Both patients were men, older than 50 years of age, and had body mass indices greater than 30 kg/m2.
Discussion
Posttraumatic osteoarthritis can be a challenge to treat as a result of the potential young age of patients, presence of hardware, and possibility for posttraumatic deformity. Conventional THA has been used to treat these patients when there is disabling pain not responsive to nonoperative treatment. However, resurfacing may have the potential to offer an alternative treatment that can preserve bone and allow surgeons more options when dealing with implanted hardware and deformities. According to the literature, the ideal candidates for resurfacing arthroplasty are male patients, younger than 55 years old, and having a primary diagnosis of osteoarthritis [1, 2, 14]. Several reports suggest patients with osteonecrosis or developmental deformities of the hip have comparable survivorship to patients with primary arthritis [8, 9]. In patients with posttraumatic arthritis, several problems present challenges for surgeons, including trauma-related deformity, bone loss, and retained hardware. Survivorship for THA ranges from 78% to 97% [3, 7, 12, 15] (Table 2). One of the major advantages to using a resurfacing arthroplasty is the ability to implant the prosthesis without removal of plates, screws, or other hardware that are required in a standard THA. Therefore, we asked: (1) are survivorship and functional scores higher and radiographic failures lower in patients who underwent resurfacing arthroplasty compared with patients with nontraumatic osteoarthritis; and (2) are those parameters higher compared with all patients who have resurfacing?
Table 2.
Reported arthroplasty results for patients with posttraumatic osteoarthritis
There are several limitations to this study. First, our patients had a minimum of 2 years followup. Although no patients were lost to followup, our observations are preliminary and the cohort needs to continue to be monitored. Nonetheless, the data suggest resurfacing may be an alternative treatment for this disease and offer the surgeon options when deciding how to treat a patient with posttraumatic osteoarthritis. Second, the study cohort was only matched to patients who underwent resurfacing for nontraumatic osteoarthritis. Another comparison group would be to match patients who underwent resurfacing arthroplasty directly to those who underwent THA for traumatic osteoarthritis. There were insufficient patients at the senior authors’ institutions to effectively perform this comparison. In lieu of this, the authors provided a literature review of the survivorship of THA in the treatment of posttraumatic osteoarthritis for comparison of the study cohort to patients who underwent standard THA.
One of the major challenges associated with treating posttraumatic osteoarthritis is dealing with posttraumatic deformity. Some authors have reported outcomes of resurfacing arthroplasty in patients with preoperative hip deformities [8, 9]. Although patients with posttraumatic osteoarthritis do not have a history of developmental dysplasia, they often have a history of femoral deformities subsequent to the original trauma. Boyd et al. reported a series of 19 hips with developmental dysplasia of the hip and a mean followup of 51 months (range, 26–72 months) [4]. Eighteen of the 19 hips had excellent Harris hip scores (greater than 80 points). These results are similar to this study, showing an improvement from a mean of 54 points preoperatively to 90 points postoperatively. Similarly, Li et al. reported on a series of 26 hips in 21 patients who underwent resurfacing arthroplasty for developmental dysplasia of the hip and compared their results with patients who underwent THA for the same diagnosis [8]. Similar to our study, they found no difference between the reported postoperative Harris hip scores of the two groups, but there was an increased ROM in the group that underwent resurfacing as opposed to standard THA. Additionally, our reported survivorship of resurfacings is comparable to, and better than, some of the reported survivorship rates of conventional THA in this population, which range from 78% to 97% (Table 2) [3, 7, 12, 15].
As a result of the technical difficulty associated with THA in patients with posttraumatic osteoarthritis, intraoperative and postoperative complications are concerns for this patient population. Hammad et al. reported 32 patients who underwent THA 15 months after fixation of an intertrochanteric fracture with dynamic hip screws [7]. In their study, only 78% of patients had good or excellent clinical results as determined by the investigators using Harris hip scores at final followup (greater than 80 points) with an overall improvement from a mean score of 26 points preoperative (range not reported) to a mean score of 84 points (range not reported) postoperatively. Additionally, they reported several complications, including one intraoperative femur fracture, three postoperative deep venous thromboses, and a postoperative heterotopic ossification in eight hips. We observed none of these complications in our patients. Bellabarba et al. reported 30 patients treated for posttraumatic arthritis after acetabular fractures with a THA [3]. They found increased operative times and blood loss when compared with performing THA on patients without posttraumatic arthritis. The mean Harris hip score increased from 44 points preoperatively to 88 points postoperatively. Although this is only slightly lower than the increase noted in our study, the important difference between our study and those regarding standard THA is the incidence of complications. We found none of the complications reported by authors who performed THAs on patients with posttraumatic arthritis in our resurfacing patients.
Hip resurfacing arthroplasty has achieved survivorship of 94% [1, 2, 14] when the appropriate patient selection criteria are used. Our observations suggest the survivorship in an expanded patient population such as those with posttraumatic osteoarthritis may be similar to these reported survivorships and could be better than those reported for standard THA in these sometimes challenging patient populations. Although deformities and implanted hardware can present challenges leading to increased difficulty, morbidity, blood loss, and complications when performing a standard THA, these issues are less of a concern when performing a hip resurfacing arthroplasty.
Footnotes
One of the authors (MAM) has received royalties from Stryker Orthopaedics, is a paid consultant for Stryker Orthopaedics and Wright Medical Technologies, and has received institutional support from the National Institutes of Health (NIAMS and NICHD), Stryker Orthopaedics, Tissue Gene, and Wright Medical Technologies. One of the authors (TPG) has received royalties from Biomet Orthopaedics.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Sinai Hospital of Baltimore and Midlands Orthopaedics.
Contributor Information
Fei Liu, Email: feilresearch@gmail.com.
Thomas P. Gross, Email: grossortho@yahoo.com.
References
- 1.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed] [Google Scholar]
- 2.Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings. An independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329. doi: 10.1302/0301-620X.87B3.15556. [DOI] [PubMed] [Google Scholar]
- 3.Bellabarba C, Berger RA, Bentley CD, Quigley LR, Jacobs JJ, Rosenberg AG, Sheinkop MB, Galante JO. Cementless acetabular reconstruction after acetabular fracture. J Bone Joint Surg Am. 2001;83:868–876. doi: 10.1302/0301-620X.83B6.11649. [DOI] [PubMed] [Google Scholar]
- 4.Boyd HS, Ulrich SD, Seyler TM, Marulanda GA, Mont MA. Resurfacing for Perthes disease: an alternative to standard hip arthroplasty. Clin Orthop Relat Res. 2007;465:80–85. doi: 10.1097/BLO.0b013e318156bf76. [DOI] [PubMed] [Google Scholar]
- 5.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 6.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 7.Hammad A, Abdel-Aal A, Said HG, Bakr H. Total hip arthroplasty following failure of dynamic hip screw fixation of fractures of the proximal femur. Acta Orthop Belg. 2008;74:788–792. [PubMed] [Google Scholar]
- 8.Li J, Xu W, Xu L, Liang Z. Hip resurfacing for the treatment of developmental dysplasia of the hip. Orthopedics. 2008;31:1199. doi: 10.3928/01477447-20081201-11. [DOI] [PubMed] [Google Scholar]
- 9.Mont MA, Seyler TM, Marker DR, Marulanda GA, Delanois RE. Use of metal-on-metal total hip resurfacing for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):90–97. doi: 10.2106/JBJS.F.00543. [DOI] [PubMed] [Google Scholar]
- 10.Mont MA, Seyler TM, Ulrich SD, Beaule PE, Boyd HS, Grecula MJ, Goldberg VM, Kennedy WR, Marker DR, Schmalzried TP, Sparling EA, Vail TP, Amstutz HC. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70. doi: 10.1097/BLO.0b013e318159dd60. [DOI] [PubMed] [Google Scholar]
- 11.Nishii T, Sugano N, Miki H, Takao M, Koyama T, Yoshikawa H. Five-year results of metal-on-metal resurfacing arthroplasty in Asian patients. J Arthroplasty. 2007;22:176–183. doi: 10.1016/j.arth.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Ranawat A, Zelken J, Helfet D, Buly R. Total hip arthroplasty for posttraumatic arthritis after acetabular fracture. J Arthroplasty. 2009;24:759–767. doi: 10.1016/j.arth.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 14.Vail TP, Mina CA, Yergler JD, Pietrobon R. Metal-on-metal hip resurfacing compares favorably with THA at 2 years followup. Clin Orthop Relat Res. 2006;453:123–131. doi: 10.1097/01.blo.0000238852.08497.92. [DOI] [PubMed] [Google Scholar]
- 15.Weber M, Berry DJ, Harmsen WS. Total hip arthroplasty after operative treatment of an acetabular fracture. J Bone Joint Surg Am. 1998;80:1295–1305. doi: 10.2106/00004623-199809000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Witzleb WC, Arnold M, Krummenauer F, Knecht A, Ranisch H, Gunther KP. Birmingham Hip Resurfacing arthroplasty: short-term clinical and radiographic outcome. Eur J Med Res. 2008;13:39–46. [PubMed] [Google Scholar]