Abstract
Background
Squeaking is reportedly a complication in patients having ceramic-on-ceramic total hip implants. The etiology remains unknown and multifactorial with recent studies suggesting a relationship between the audible squeak and implant design. When we evaluated our ceramic-on-ceramic cohort, we noticed squeaking primarily in patients receiving an acetabular system designed with an elevated titanium rim.
Objectives/purposes
We therefore (1) determined the incidence of squeaking among four different ceramic-on-ceramic bearing surfaces used for THA at our institution; (2) evaluated the association between different acetabular designs and the incidence of squeaking; and (3) assessed other potential variables associated with squeaking.
Methods
We retrospectively reviewed 1507 patients having a ceramic-on-ceramic THA between 2002 and 2009; we separately analyzed those receiving an acetabular system with and without an elevated titanium rim. Data were collected through phone-administered questionnaires and retrospective reviews of patient charts for intraoperative findings, followup reports, demographic information, and radiographic findings.
Results
Squeaking occurred in 92 of the 1507 patients (6%). All 92 patients with squeaking received an elevated rim design (1291 patients) or an incidence of 7% with that design. We found no association between squeaking and any other examined factors.
Conclusion
Our findings complement the theory from in vitro studies suggesting that neck impingement on the elevated titanium rim is the probable cause of the increased frequency of squeaking with this design.
Level of Evidence
Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
By decreasing pain and increasing mobility in patients, THA has become one of the most successful orthopaedic procedures to date [18]. However, wear particles are the leading cause of osteolysis and reportedly subsequent implant loosening [3, 4, 12, 15, 32, 48] and a major cause of failure of THA [21]. Boutin introduced ceramic-on-ceramic (COC) bearings as an alternative to the metal-on-polyethylene bearings most commonly used in 1971 [7]. The success of ceramic implants [2, 4–6, 8, 41] is attributed to the excellent tribologic properties of alumina [20] associated with superior wear rates and a chemically inert nature which grants it biocompatibility [3, 11, 28] and greater longevity compared with the traditional metal-on-polyethylene bearing surface [4, 12, 14, 16, 25, 32]. The COC bearing surface is especially appealing to younger, more active patients who pose a greater risk for wear and need for arthroplasty [4, 12, 20, 28, 32, 34, 41, 43].
Despite over 32 years of success in Europe [20] and implant survival rates exceeding 85% at a minimum followup of 18.5 years [19], the use of COC in North America was not as enthusiastic as a result of concern with potential for fracture of this bearing surface [4, 34, 41]. Improvements in alumina manufacturing and prosthetic design reduced the incidence of fracture [3, 11, 12, 16, 26, 41, 45, 49]. However, there have been an increasing number of reports on audible noises that seemed linked to these hard bearing surfaces [28, 31, 35, 37, 39, 47], leading some to believe the implant material or design was still to blame [3, 40, 41, 43]. Various studies have documented an incidence of various noises including squeaking ranging from less than 1% to 20.9% of patients with COC bearing surfaces [9, 22, 24, 27, 31, 37, 47], for which the reported onset time averaged between 14 and 24 months postoperatively [22, 24, 27, 37, 47].
The exact etiology of squeaking the COC bearing surface remains unknown and is believed to be multifactorial. Numerous studies have attempted to elucidate the cause of squeaking. Some studies suggested squeaking may be related to patient factors such as younger age and increased height and weight [47]. Component malpositioning during surgery has been cited as a source of squeaking in several studies [39, 46, 47], whereas another study has refuted the role of component positioning as an etiologic factor for squeaking COC bearings [37]. The concept of edge loading [17, 44] and related stripe wear [42, 44], seen on ceramic explants, has also been linked to squeaking COC bearings [47]. Several recent studies have suggested the metallic debris potentially generated through neck impingement and transferred into the bearing surfaces may have led to disruption of the fluid-film lubrication and resulted in squeaking [10, 22, 40]. Another study suggested the design of the femoral stem may be implicated in squeaking after COC THA [38].
We therefore (1) determined the incidence of squeaking among four different ceramic-on-ceramic bearing surfaces used for THA at our institution; (2) evaluated the association between different acetabular designs and the incidence of squeaking; and (3) assessed other potential variables associated with squeaking.
Patients and Methods
We performed a retrospective review of 1507 patients (1756 hips) who underwent THA using COC bearings between January 2002 and December 2009. All COC bearings used were manufactured from alumina (Biolox Forte®; Ceramtec AG, Plochingen, Germany). We divided the patients into two cohorts based solely on whether the implant had or did not have an elevated rim from the titanium metal sleeve surrounding the ceramic liner. Group 1 consisted of 1291 patients and 1508 hips who received a COC THA using the Stryker Orthopaedics-manufactured Trident® Acetabular System. Of this group, 506 were female (average age, 50 years; range, 17–80 years) and 785 were male (average age, 50 years; range, 15–76 years). Group 2 consisted of 216 patients with 248 hips who received COC THA using acetabular cup designs lacking a titanium metal sleeve and manufactured by Biomet (Warsaw, IN), DePuy (New Brunswick, NJ), or Stelkast (McMurray, PA). Of this group, 91 were female (average age, 50 years; range, 21–79 years) and 125 were male (average age, 49 years; range, 18–69 years). Minimum followup was 1.1 years (mean, 4.2 years; range, 0.1–8.07 years). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. We had prior Institutional Review Board.
Patient medical records were accessed to extract all important information such as the demographic variables. The collected demographic and prosthetic data were then compared between the two groups (Table 1).
Table 1.
Demographic distribution among the cohort
| Cohort time | Trident® cups | Non-Trident® cups | p | Relative risk | ||
|---|---|---|---|---|---|---|
| January 2002 to March 2009 | April 2006 to December 2009 | |||||
| Total | ||||||
| Patients | 1291 | Squeaking | Nonsqueaking | 216 | 0.0001 | 0/0.07 |
| 92* | 1199 | |||||
| Bilateral | 206 | 7† | 199 | 32 | 0.3732 | 0/0.03 |
| Hips | 1497 | 99 | 1398 | 248 | 0.0001 | 0/0.07 |
| Male | 785 (60.8%) | 50 (52.2%) | 735 (61.1%) | 125 (57.9%) | 0.4524 | |
| Female | 506 (39.2%) | 42 (43.2%) | 464 (38.9%) | 91 (42.1%) | ||
| Age | 49.8 (15.3–79.7) | 46.1 (18.9–66.9) | 50.0 (15.3–79.7) | 49.5 (17.9–78.6) | 0.6192 | |
| Height | 1.73 (1.24–2.49) | 1.72 (1.52–1.98) | 1.73 (1.24–2.49) | 1.72 (1.42–2.03) | 0.1732 | |
| Weight | 85.8 (37.2–214.6) | 82.9 (43.1–139.7) | 86.0 (37.2–214.6) | 87.9 (38.6–159.7) | 0.1742 | |
| BMI | 28.4 (13.2–57.6) | 27.7 (16.3–49.7) | 28.5 (13.2–57.6) | 29.4 (16.6–50.4) | 0.0167 | |
* Twelve of 92 patients had bilateral total hips; †seven of 12 patients with bilateral total hips, both hips were squeaking; BMI = body mass index.
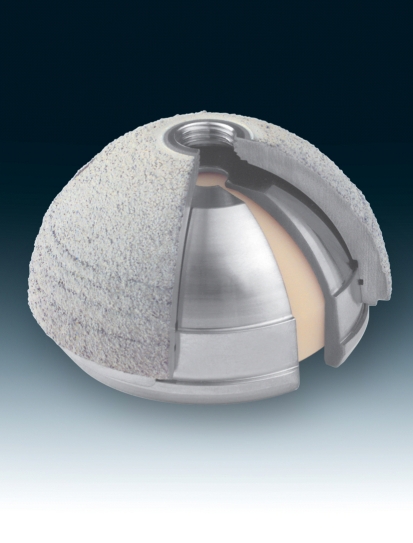
All THAs were performed by one of six surgeons using an anterolateral approach with patients in the supine position and under regional anesthesia. All components used were uncemented prostheses. Patients in Group 1 received either a Trident® PSL® (816 hips) or a Trident® Hemispherical® Cup (692 hips). The Trident® cup is a titanium-aluminum-vanadium (TAV) alloy and accepts a ceramic liner that has a commercially pure titanium sleeve surrounding it (Fig. 1). The rim of this titanium sleeve is actually elevated above the ceramic in this specific design. These cups were then paired with one of Stryker’s conventional TAV alloy stems (Omnifit®, Restoration HA®, Restoration Modular®, Secure-Fit®, Super Secure-Fit®) or with a Stryker stem made of a titanium-molybdenum-zirconium-ferrous (TMZF®) alloy (Accolade®). One hundred seventy-four patients received the Trident/TAV combination, whereas 1334 patients received the Trident®/TMZF® combination. Patients in Group 2 received acetabular cups referred to as C2a®-Taper (Biomet), Duraloc® (DePuy), or Surpass® (Stelkast). The C2a®-Taper cup was used in 39 patients (41 hips). The Duraloc® cup was used in 46 patients (50 hips). The Surpass® cup was used in 131 patients (157 hips). Furthermore, all acetabular systems in Group 2 were paired with stems made of conventional TAV alloy: Biomet Taperloc®, 39 patients (41 hips); DePuy S-Rom®, one patient (two hips); Tri-Lock®, 41 patients (48 hips); and Stelkast Provident®, 131 patients (157 hips) (Tables 2, 3).
Fig. 1.
Trident® Acetabular System from Stryker Orthopaedics (Mahwah, NJ) displaying the acetabular titanium-aluminum-vanadium (TAV) alloy shell, which accepts a ceramic liner that has a commercially pure titanium sleeve surrounding it.
Table 2.
Implant component distributions among Trident® (squeaking and nonsqueaking) and non-Trident® hips (cup-head)
| Stryker Trident® implant | Non-Stryker Trident® implant | |||||||
|---|---|---|---|---|---|---|---|---|
| Cup | Squeaking | Nonsqueaking | Biomet | DePuy | Stelkast | |||
| H | PSL | H | PSL | C2a® | Duraloc® | Surpass® | ||
| Size | 40 | NA | 0 | NA | 0 | NA | NA | NA |
| 42 | 0 | 0 | 0 | 0 | NA | NA | NA | |
| 44 | 0 | 0 | 0 | 0 | NA | NA | NA | |
| 46 | 0 | 8 | 0 | 45 | NA | NA | 0 | |
| 48 | 5 | 5 | 53 | 58 | 0 | 0 | 0 | |
| 50 | 0 | 13 | 28 | 144 | 3 | 1 | 16 | |
| 52 | 8 | 10 | 151 | 121 | 18 | 20 | 35 | |
| 54 | 6 | 11 | 111 | 125 | 5 | 8 | 36 | |
| 56 | 6 | 5 | 101 | 81 | 9 | 9 | 30 | |
| 58 | 2 | 13 | 37 | 133 | 0 | 6 | 18 | |
| 60 | 6 | 1 | 121 | 30 | 0 | 0 | 6 | |
| 62 | 1 | 0 | 23 | 8 | 0 | 0 | 2 | |
| 64 | 0 | 0 | 6 | 4 | 0 | 0 | 0 | |
| 66 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | |
| 68 | 0 | 0 | 1 | 1 | 0 | NA | 0 | |
| 70 | 0 | 0 | 0 | 0 | 0 | NA | 0 | |
| 72 | 0 | 0 | 0 | 0 | NA | NA | 0 | |
| 74 | 0 | 0 | NA | NA | NA | NA | ||
| Head | Squeaking | Nonsqueaking | Biomet | DePuy | Stelkast | |||
|---|---|---|---|---|---|---|---|---|
| Size | 28 | 16 | 215 | 9 | 7 | 30 | ||
| 32 | 61 | 872 | 32 | 43 | 127 | |||
| 36 | 22 | 322 | NA | NA | NA | |||
| Neck | Squeaking | Nonsqueaking | Biomet | DePuy | Stelkast | |||
|---|---|---|---|---|---|---|---|---|
| Length | −5 | 0 | 19 | NA | NA | NA | ||
| −4 | 13 | 238 | 19 | NA | NA | |||
| −3.5 | NA | NA | 6 | NA | 19 | |||
| −3 | 0 | 3 | NA | NA | NA | |||
| −2.7 | 3 | 52 | NA | NA | NA | |||
| −2.5 | 0 | 2 | NA | NA | NA | |||
| 0 | 59 | 739 | 13 | 2 | 86 | |||
| +1 | NA | NA | NA | 10 | NA | |||
| +1.5 | NA | NA | NA | 2 | NA | |||
| +2.5 | 0 | 1 | NA | NA | NA | |||
| +3.5 | NA | NA | NA | NA | 51 | |||
| +4 | 17 | 244 | 3 | NA | NA | |||
| +5 | 7 | 104 | NA | 19 | NA | |||
| +6 | NA | NA | NA | 0 | NA | |||
| +7.5 | 0 | 0 | NA | NA | NA | |||
| +8 | 0 | 0 | NA | NA | NA | |||
| +9 | NA | NA | NA | 17 | NA | |||
| +10 | NA | NA | NA | NA | 1 | |||
| 12 | 0 | 0 | NA | NA | NA | |||
H = Hemispherical® cup; PSL® = Peripheral Self-Locking cup; NA = not available.
Table 3.
Implant component distributions among Trident® (squeaking and nonsqueaking) and non-Trident® hips (stem)
| Stryker Trident® implant | Non-Stryker Trident® implant | |||||
|---|---|---|---|---|---|---|
| Stem Model | Squeaking | Nonsqueaking | Biomet | DePuy | Stelkast | |
| Accolade® | 84 | 1239 | NA | NA | NA | |
| Omnifit® | 13 | 110 | NA | NA | NA | |
| Restoration HA® | 0 | 14 | NA | NA | NA | |
| Restoration M® | 0 | 8 | NA | NA | NA | |
| Secur-Fit HA® | 0 | 19 | NA | NA | NA | |
| Super Secur-Fit HA® | 2 | 8 | NA | NA | NA | |
| Provident® | NA | NA | NA | NA | 157 | |
| Taperloc® | NA | NA | 41 | NA | NA | |
| S-Rom® | NA | NA | NA | 2 | NA | |
| Tri-Lock | NA | NA | NA | 48 | NA | |
| Stem | Squeaking | Nonsqueaking | Biomet | DePuy | Stelkast | |
|---|---|---|---|---|---|---|
| Size | 0 | 3 | 39 | NA | 4 | NA |
| 1 | 5 | 94 | NA | 1 | NA | |
| 2 | 22 | 297 | NA | 11 | NA | |
| 2.5 | 0 | 13 | NA | 0 | NA | |
| 3 | 25 | 394 | NA | 5 | NA | |
| 3.5 | 0 | 5 | NA | 0 | NA | |
| 4 | 21 | 265 | NA | 8 | NA | |
| 4.5 | 1 | 9 | NA | 0 | NA | |
| 5 | 7 | 120 | 5 | 8 | NA | |
| 5.5 | 0 | 1 | NA | 0 | NA | |
| 6 | 5 | 37 | 1 | 6 | 7 | |
| 7 | 3 | 40 | NA | 3 | NA | |
| 7.5 | NA | NA | 15 | 0 | 11 | |
| 8 | 5 | 24 | NA | 1 | NA | |
| 8.75 | NA | NA | NA | NA | 18 | |
| 9 | 2 | 37 | 3 | 1 | NA | |
| 10 | 0 | 18 | 7 | 0 | 25 | |
| 11 | 0 | 6 | 6 | 0 | NA | |
| 11.25 | NA | NA | NA | 0 | 25 | |
| 12 | 0 | 1 | NA | 0 | NA | |
| 12.5 | NA | NA | 9 | 0 | 30 | |
| 13 | 0 | 4 | NA | 0 | NA | |
| 13.5 | NA | NA | 4 | 0 | NA | |
| 13.75 | NA | NA | NA | 0 | 22 | |
| 14 | 0 | 2 | NA | 1 | NA | |
| 15 | 0 | 0 | 1 | 0 | 12 | |
| 16 | 0 | 0 | NA | 1 | NA | |
| 17 | 0 | 1 | NA | 0 | NA | |
| 17.5 | NA | NA | 0 | 0 | 6 | |
| 18 | 0 | 3 | NA | 0 | NA | |
| 20 | 0 | 0 | 0 | 0 | 1 | |
| 22.5 | NA | NA | 0 | NA | 0 | |
| 23 | 0 | 1 | NA | 0 | NA | |
| 24 | 0 | 0 | NA | NA | NA | |
| 25 | 0 | 0 | 0 | NA | NA | |
| 26 | 0 | 0 | NA | NA | NA | |
| 27 | 0 | 0 | NA | NA | NA | |
| 28 | 0 | 0 | NA | NA | NA | |
| Stem | Squeaking | Nonsqueaking | Biomet | DePuy | Stelkast | |
|---|---|---|---|---|---|---|
| Offset | Standard | 72 | 898 | 27 | 27 | 101 |
| Lateral | 27 | 499 | 14 | 23 | 56 | |
NA = not available.
To obtain the incidence of squeaking in both groups, patients were surveyed by their respective surgeons during followup visits (postoperatively, 6 weeks postoperatively, 6 months postoperatively, 1 year postoperatively, and any other visits) or over the telephone (called by BA, JW) using a similar questionnaire as that used by Mai et al. [27]. Patients were then asked specifically regarding the existence of a squeaking noise from the operated hip with squeaking being described as a high-frequency pitch analogous to that heard from a nonlubricated hinge. If present, the squeaking was then further characterized by the following factors: audibility (if noise was noticed by only the patient or also by others nearby), onset time (period of time postsurgery in which the patient first became aware of the squeaking noise), intensity, frequency of squeaking occurrences, reproducibility on demand, and the various methods used by the patient in which squeaking could be generated (walking, bending forward, sitting, rising from a sitting position, going up or down stairs, and other) [27].
Two of us (CR, JP) independently reviewed all postoperative AP and lateral radiographic views to assess component positioning [1]. OrthoView® (Southampton Hampshire, UK) software was used by uploading the AP radiographs, then the image was calibrated, and the position of the acetabular component was assessed by using the inclination-anteversion tool from the system. Cup position was assessed for abduction, version, and height. Stems were evaluated for position and offset. All patients had postoperative radiographs available for measurement. Any radiologic measurement discrepancies were resolved with a third orthopaedic surgeon (RHR).
Statistical analysis was used to determine measures of central tendency (mean, median, and mode) and dispersion (SD, 95% confidence interval); descriptive statistics were applied to all data obtained.
We used a two-tailed unpaired t-test to assess differences in continuous variables (age, height, weight, body mass index, cup inclination, and cup version) between the two groups, and two-tailed Fisher’s exact test was used for nominal values (patients, hips, bilateral hips, gender, head size, and neck length). All patient parameters were analyzed using SPSS (Chicago, IL).
Results
The incidence of squeaking at 7%% was higher (p = 0.001) in patients receiving the Trident® COC system compared with 0% among patients who received a recessed ceramic liner. The incidence of squeaking tended to be higher (p = 0.50) among patients who received the Trident® system and TMZF® stems (6%) compared with the incidence with the Trident® system and other femoral stems (5.8%). The mean time to squeaking was 20 months (range, 2–48 months) among the Trident® group. Squeaking had diminished in 12 patients (13 hips) over time and remained similar in 80 patients (86 hips). Ten patients (11 hips) have undergone revision arthroplasty because of squeaking. Impingement, defined as contact between the femoral neck and the rim of the ceramic liner, was confirmed in seven (64%) of the explants.
The inclination angle of the acetabular component at 38° (range, 24°–55°) and version of 43° (range, 0°–67°) among the Trident® group was similar to the inclination at 38° (range, 23°–55°) or the version at 42° (range, 5°–66°) for patients receiving non-Trident® systems (p = 0.71) for inclination and (p = 0.41) for version.
No difference in squeaking incidence was observed among surgeons.
There were no cases of fractured ceramic.
Discussion
We believe the COC bearing surface is a reasonable option for a population of active patients demanding more from their prosthesis [28]. However, an incidence of squeaking found among patients with these COC implants has been recorded [39, 48]. This problem was first noted among centers in North America that used the Trident® system (Stryker). We initially reported an incidence of squeaking of 6.4% for patients receiving the Trident® system [36]. Squeaking linked to other designs of COC have since been reported but more commonly found with the Trident® system. We therefore (1) determined the incidence of squeaking among four different ceramic-on-ceramic bearing surfaces used for THA at our institution; (2) evaluated the association between different acetabular designs and the incidence of squeaking; and (3) assessed other potential variables associated with squeaking.
A few limitations of this study are worth mentioning. First, the followup for hips receiving the non-Trident® design was shorter than that for the Trident® COC hips. The latter can bias the results against the Trident® system by raising the cumulative incidence of squeaking. However, squeaking with the Trident® system appeared to occur mostly within the first 2 years. Second, we did not address the potential role of the femoral stem in squeaking. Several studies [32, 38] have reported a higher incidence of squeaking with the TMZF® stems when compared with other stem designs. Although we do not dispute the role of the femoral stem in causing squeaking, we have noted the Trident® COC system, regardless of the type of femoral stem used, has a much higher incidence of squeaking. The combination of the Trident® COC bearing system with a TMZF® femoral stem appears to increase its incidence further. Third relates to the definition of squeaking. To determine the incidence of squeaking for patients with a COC bearing surface, we developed a questionnaire, comparable to that used in related studies [22, 27], that was administered in person or over the phone. Questionnaires provide a dependable way of collecting information that is easily duplicated [13, 23, 24, 30]. However, the limitation of their administration may relate to the exact “definition” of squeaking. It is plausible some patients may have erroneously referred to other noises such as clicking as squeaking, whereas some patients may have ignored a true squeaking noise as unimportant and not reported it. So, despite our attempt to have a “standard definition” for squeaking, its true incidence may have been influenced by patient perception of the questions posed.
Regardless of design variations, the etiology of squeaking COC remains elusive with no one factor being declared as the ultimate culprit. Based on our initial clinical observation and the retrieval analysis of a small cohort of patients with squeaking COC undergoing revision arthroplasty, we presumed impingement of the femoral stem and the acetabular rim of the ceramic socket to be the culprit. In our retrieval study of the COC explants, gross impingement between the acetabular rim of the ceramic liner and the femoral neck occurred in 63.6% of the retrieved implants [29]. Although presence of impingement was not essential for generation of squeaking in these revised cases, it was common. We cannot say how many patients experience impingement without squeaking COC, but impingement may be an important contributor to the issue. This is supported by Chevillotte et al. [10] who found metal particle transfer into the articulating surface led to generation of squeaking in the COC bearing surface. The Trident® COC design, with an elevated titanium rim around the ceramic acetabular liner, would appear to potentiate both impingement and metal debris production. The rim is intended to protect the acetabular component from chipping and increase its burst strength as confirmed by D’Antonio et al. [12]. All the non-Trident® COC bearing surfaces used at our institution involve recessed seating of the ceramic liner into an acetabular shell. With these designs, the impingement may still occur between the femoral neck and the acetabular component leading to generation of metal debris and potential squeaking [33]. The latter may in fact explain why squeaking is not purely limited to the Trident® system and can happen with other COC designs.
Speculations discussed thus far raise an important issue that component positioning is even more critical with the hard-on-hard bearing surface if impingement and the undesired consequences arising as a result of it are to be avoided. The latter may explain why some studies have implicated component positioning as an important factor in the generation of squeaking in COC bearing surfaces [47]. One may hence speculate that component malpositioning in the absence of impingement and generation of metal particles is unlikely to lead to generation of squeaking [37]. Previous studies have also implicated component positioning in the generation of squeaking. One study found a higher variance in acetabular anteversion and inclination in hips that squeaked [47].
The other important factor relates to the type of femoral component used. Murphy et al. also showed the incidence was 0.6% when the ceramic liner sat evenly with the metal shell, 3.2% with an elevated metal rim, and finally at 7.6% when the cup with an elevated encasement was paired with a TMZF® alloy stem [32]. Mai et al. claimed squeaking could only be attributed to the geometry and small size of the femoral necks [27]. However, because we do not have patients who received the TMZF® alloy stem paired with a cup-liner assembly without a protruding rim, we cannot conclusively associate this particular stem design to squeaking.
Although we cannot be certain the design of the acetabular component is the only factor leading to squeaking, the potential for impingement between the elevated acetabular rim and the femoral neck is, in our opinion, a critical factor leading to this problem [12, 22, 24, 27]. Unlike previous studies, we did not find any demographic factor to be a major contributor to squeaking. Our findings support those of D’Antonio et al. in their investigation of the elevated metal sleeve-liner system [12]. No link was made to any patient demographics despite a report claiming that an increased demand and load put on the prosthetic device by younger, taller, and heavier patients is attributed to squeaking [47].
We substantially decreased the use of the Trident COC system at our institution by the end of 2007 and now pay special attention to component positioning in patients receiving all designs of COC bearing surface to avoid impingement. We continue to advocate the use of the COC bearing surface for young, active patients despite the squeaking dilemma.
Footnotes
One of the authors (JP) is a consultant for Stryker Orthopaedics (Mahwah, NJ) and has intellectual properties on SmarTech (Philadelphia, PA); and one of the authors (RHR) is a consultant for and receives royalties from Stryker Orthopaedics.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK. Anteversion of the acetabular cup. Measurement of angle after total hip replacement. J Bone Joint Surg Br. 1986;68:409–413. doi: 10.1302/0301-620X.68B3.3733807. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Burak C, Skinner HB. Concerns about ceramics in THA. Clin Orthop Relat Res. 2004;429:73–79. doi: 10.1097/01.blo.0000150132.11142.d2. [DOI] [PubMed] [Google Scholar]
- 3.Bierbaum BE, Nairus J, Kuesis D, Morrison JC, Ward D. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res. 2002;405:158–163. doi: 10.1097/00003086-200212000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Bizot P, Larrouy M, Witvoet J, Sedel L, Nizard R. Press-fit metal-backed alumina sockets: a minimum 5-year followup study. Clin Orthop Relat Res. 2000;379:134–142. doi: 10.1097/00003086-200010000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Boehler M, Knahr K, Plenk H, Jr, Walter A, Salzer M, Schreiber V. Long-term results of uncemented alumina acetabular implants. J Bone Joint Surg Br. 1994;76:53–59. [PubMed] [Google Scholar]
- 6.Boutin P. Total arthroplasty of the hip by fritted aluminum prosthesis. Experimental study and 1st clinical applications [in French] Rev Chir Orthop Reparatrice Appar Mot. 1972;58:229–246. [PubMed] [Google Scholar]
- 7.Boutin P. Total hip arthroplasty using a ceramic prosthesis. Pierre Boutin (1924–1989) Clin Orthop Relat Res. 2000;379:3–11. doi: 10.1097/00003086-200010000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Boutin P, Christel P, Dorlot JM, Meunier A, de RA, Blanquaert D, Herman S, Sedel L, Witvoet J. The use of dense alumina-alumina ceramic combination in total hip replacement. J Biomed Mater Res. 1988;22:1203–1232. [DOI] [PubMed]
- 9.Capello WN, D’Antonio JA, Feinberg JR, Manley MT, Naughton M. Ceramic-on-ceramic total hip arthroplasty: update. J Arthroplasty. 2008;23(Suppl):39–43. doi: 10.1016/j.arth.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Chevillotte C, Trousdale RT, Chen Q, Guyen O, An KN. The 2009 Frank Stinchfield Award: ‘Hip squeaking’: a biomechanical study of ceramic-on-ceramic bearing surfaces. Clin Orthop Relat Res. 2010;468:345–350. doi: 10.1007/s11999-009-0911-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clarke IC. Role of ceramic implants Design and clinical success with total hip prosthetic ceramic-to-ceramic bearings. Clin Orthop Relat Res. 1992;282:19–30. [PubMed] [Google Scholar]
- 12.D’Antonio J, Capello W, Manley M, Naughton M, Sutton K. Alumina ceramic bearings for total hip arthroplasty: five-year results of a prospective randomized study. Clin Orthop Relat Res. 2005;436:164–171. doi: 10.1097/01.blo.0000162995.50971.39. [DOI] [PubMed] [Google Scholar]
- 13.Dawson J, Carr A. Outcomes evaluation in orthopaedics. J Bone Joint Surg Br. 2001;83:313–315. doi: 10.1302/0301-620X.83B3.12148. [DOI] [PubMed] [Google Scholar]
- 14.Dorlot JM, Christel P, Meunier A. Wear analysis of retrieved alumina heads and sockets of hip prostheses. J Biomed Mater Res. 1989;23(Suppl):299–310. doi: 10.1002/jbm.820231405. [DOI] [PubMed] [Google Scholar]
- 15.Dorr LD, Wan Z, Shahrdar C, Sirianni L, Boutary M, Yun A. Clinical performance of a Durasul highly cross-linked polyethylene acetabular liner for total hip arthroplasty at five years. J Bone Joint Surg Am. 2005;87:1816–1821. doi: 10.2106/JBJS.D.01915. [DOI] [PubMed] [Google Scholar]
- 16.Garino JP. Modern ceramic-on-ceramic total hip systems in the United States: early results. Clin Orthop Relat Res. 2000;379:41–47. doi: 10.1097/00003086-200010000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Glaser D, Komistek RD, Cates HE, Mahfouz MR. Clicking and squeaking: in vivo correlation of sound and separation for different bearing surfaces. J Bone Joint Surg Am. 2008;90(Suppl 4):112–120. doi: 10.2106/JBJS.H.00627. [DOI] [PubMed] [Google Scholar]
- 18.Greene JW, Malkani AL, Kolisek FR, Jessup NM, Baker DL. Ceramic-on-ceramic total hip arthroplasty. J Arthroplasty. 2009;24(Suppl):15–18. doi: 10.1016/j.arth.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 19.Hamadouche M, Boutin P, Daussange J, Bolander ME, Sedel L. Alumina-on-alumina total hip arthroplasty: a minimum 18.5-year follow-up study. J Bone Joint Surg Am. 2002;84:69–77. [PubMed] [Google Scholar]
- 20.Hannouche D, Hamadouche M, Nizard R, Bizot P, Meunier A, Sedel L. Ceramics in total hip replacement. Clin Orthop Relat Res. 2005;430:62–71. doi: 10.1097/01.blo.0000149996.91974.83. [DOI] [PubMed] [Google Scholar]
- 21.Harris WH. Wear and periprosthetic osteolysis: the problem. Clin Orthop Relat Res. 2001;393:66–70. doi: 10.1097/00003086-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Jarrett CA, Ranawat AS, Bruzzone M, Blum YC, Rodriguez JA, Ranawat CS. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009;91:1344–1349. doi: 10.2106/JBJS.F.00970. [DOI] [PubMed] [Google Scholar]
- 23.Johanson NA, Charlson ME, Szatrowski TP, Ranawat CS. A self-administered hip-rating questionnaire for the assessment of outcome after total hip replacement. J Bone Joint Surg Am. 1992;74:587–597. [PubMed] [Google Scholar]
- 24.Keurentjes JC, Kupers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008;466:1438–1443. doi: 10.1007/s11999-008-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lusty PJ, Watson A, Tuke MA, Walter WL, Walter WK, Zicat B. Wear and acetabular component orientation in third generation alumina-on-alumina ceramic bearings: an analysis of 33 retrievals [corrected] J Bone Joint Surg Br. 2007;89:1158–1164. doi: 10.2106/JBJS.F.01466. [DOI] [PubMed] [Google Scholar]
- 26.Mahoney OM, Dimon JH., III Unsatisfactory results with a ceramic total hip prosthesis. J Bone Joint Surg Am. 1990;72:663–671. [PubMed] [Google Scholar]
- 27.Mai K, Verioti C, Ezzet KA, Copp SN, Walker RH, Colwell CW., Jr Incidence of ‘squeaking’ after ceramic-on-ceramic total hip arthroplasty. Clin Orthop Relat Res. 2010;468:413–417. doi: 10.1007/s11999-009-1083-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manley MT, Sutton K. Bearings of the future for total hip arthroplasty. J Arthroplasty. 2008;23(Suppl):47–50. doi: 10.1016/j.arth.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 29.Matar WY, Restrepo C, Parvizi J, Kurtz SM, Hozack WJ. Revision hip arthroplasty for ceramic-on-ceramic squeaking hips does not compromise the results. J Arthroplasty. 2010;25(6 Suppl):81–86. [DOI] [PubMed]
- 30.McGee MA, Howie DW, Ryan P, Moss JR, Holubowycz OT. Comparison of patient and doctor responses to a total hip arthroplasty clinical evaluation questionnaire. J Bone Joint Surg Am. 2002;84:1745–1752. doi: 10.2106/00004623-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Morlock M, Nassutt R, Janssen R, Willmann G, Honl M. Mismatched wear couple zirconium oxide and aluminum oxide in total hip arthroplasty. J Arthroplasty. 2001;16:1071–1074. doi: 10.1054/arth.2001.27233. [DOI] [PubMed] [Google Scholar]
- 32.Murphy SB, Ecker TM, Tannast M. Two- to 9-year clinical results of alumina ceramic-on-ceramic THA. Clin Orthop Relat Res. 2006;453:97–102. doi: 10.1097/01.blo.0000246532.59876.73. [DOI] [PubMed] [Google Scholar]
- 33.Murphy SB, Ecker TM, Tannast M. Incidence of squeaking after alumina ceramic-ceramic total hip arthroplasty. J Arthroplasty. 2008;23:327. doi: 10.1016/j.arth.2008.01.284. [DOI] [Google Scholar]
- 34.Nizard R, Sedel L, Hannouche D, Hamadouche M, Bizot P. Alumina pairing in total hip replacement. J Bone Joint Surg Br. 2005;87:755–758. doi: 10.1302/0301-620X.87B6.16150. [DOI] [PubMed] [Google Scholar]
- 35.Ranawat AS, Ranawat CS. The squeaking hip: a cause for concern-agrees. Orthopedics. 2007;30:738–743. doi: 10.3928/01477447-20070901-32. [DOI] [PubMed] [Google Scholar]
- 36.Restrepo C, Matar WY, Parvizi J, Rothman RH, Hozack WJ. Natural history of squeaking after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2340–2345. doi: 10.1007/s11999-009-1223-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Restrepo C, Parvizi J, Kurtz SM, Sharkey PF, Hozack WJ, Rothman RH. The noisy ceramic hip: is component malpositioning the cause? J Arthroplasty. 2008;23:643–649. doi: 10.1016/j.arth.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 38.Restrepo C, Post ZD, Kai B, Hozack WJ. The effect of stem design on the prevalence of squeaking following ceramic-on-ceramic bearing total hip arthroplasty. J Bone Joint Surg Am. 2010;92(3):550–557. [DOI] [PubMed]
- 39.Rodriguez JA, Gonzalez DA, McCook N. Squeaking in total hip replacement: a cause for concern. Orthopedics. 2008;31:874, 877–874, 878. [DOI] [PubMed]
- 40.Sariali E, Stewart T, Jin Z, Fisher J. Three-dimensional modeling of in vitro hip kinematics under micro-separation regime for ceramic on ceramic total hip prosthesis: an analysis of vibration and noise. J Biomech. 2010;43:326–333. doi: 10.1016/j.jbiomech.2009.08.031. [DOI] [PubMed] [Google Scholar]
- 41.Sedel L. Evolution of alumina-on-alumina implants: a review. Clin Orthop Relat Res. 2000;379:48–54. doi: 10.1097/00003086-200010000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Shishido T, Yamamoto K, Tanaka S, Masaoka T, Clarke IC, Williams P. A Study for a retrieved implant of ceramic-on-ceramic total hip arthroplasty. J Arthroplasty. 2006;21:294–298. doi: 10.1016/j.arth.2005.05.025. [DOI] [PubMed] [Google Scholar]
- 43.Sieber HP, Rieker CB, Kottig P. Analysis of 118 second-generation metal-on-metal retrieved hip implants. J Bone Joint Surg Br. 1999;81:46–50. doi: 10.1302/0301-620X.81B1.9047. [DOI] [PubMed] [Google Scholar]
- 44.Taylor S, Manley MT, Sutton K. The role of stripe wear in causing acoustic emissions from alumina ceramic-on-ceramic bearings. J Arthroplasty. 2007;22(Suppl 3):47–51. doi: 10.1016/j.arth.2007.05.038. [DOI] [PubMed] [Google Scholar]
- 45.Walter A. On the material and the tribology of alumina-alumina couplings for hip joint prostheses. Clin Orthop Relat Res. 1992;282:31–46. [PubMed] [Google Scholar]
- 46.Walter WL, Insley GM, Walter WK, Tuke MA. Edge loading in third generation alumina ceramic-on-ceramic bearings: stripe wear. J Arthroplasty. 2004;19:402–413. doi: 10.1016/j.arth.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 47.Walter WL, O’toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007;22:496–503. doi: 10.1016/j.arth.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 48.Walter WL, Waters TS, Gillies M, Donohoo S, Kurtz SM, Ranawat AS, Hozack WJ, Tuke MA. Squeaking hips. J Bone Joint Surg Am. 2008;90(Suppl 4):102–111. doi: 10.2106/JBJS.H.00867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Willmann G. Ceramic femoral head retrieval data. Clin Orthop Relat Res. 2000;379:22–28. doi: 10.1097/00003086-200010000-00004. [DOI] [PubMed] [Google Scholar]