Abstract
Background
Recent advances in technology and the use of image archiving and communication systems (PACS) has led some institutions to abandon conventional plain film radiography and rely solely on digital computed radiography. The level of accuracy of digital radiography in measuring distances for orthopaedic applications is unclear.
Questions/purposes
Is it possible to accurately measure small distances using digital radiographs and PACS software?
Materials and Methods
A model for measuring articular step-off was created using a commercially produced radiographic phantom with predetermined markings at known distances. Radiographs were taken using both indirect and direct computed radiography systems, then uploaded to a PACS system. Eighteen observers measured the distance between standardized, preselected points on the radiographic phantom. The measured values were compared with the known values for each measurement.
Results
The mean measured values differed by 0 and 0.1 mm (SD, 0.5 mm) for indirect and direct radiographs, respectively, when measuring short distances and 1.4 mm and 2.6 mm (SD, 1.0 mm) for indirect and direct radiographs, respectively, when measuring longer distances. The intraclass correlation coefficient (ICC) for interobserver reliability was 0.82 for indirect and 0.75 for direct digital radiography. The ICC for intraobserver reliability was 0.94 for indirect and 0.90 for direct digital radiography.
Conclusion
Although the mean measured values were very accurate (within 0.1 mm for a known distance of 3.2 mm), the SD of measurements (0.5 mm) could affect the interpretation of data, especially in clinical situations such as evaluating the quality of fracture reduction.
Introduction
Recent advances in technology and the use of PACS has led some institutions to abandon conventional plain film radiography and rely solely on digital computed radiography. There is an inherent loss of resolution when using digital computed radiography rather than conventional plain film radiography [6]. Resolution can be expressed in terms of the number of line pairs per millimeter. Conventional films have five to 10 line pairs per mm, whereas many digital radiography systems have only two to four line pairs per mm [3, 6]. This means that although conventional radiographs can differentiate a difference of 0.1 to 0.2 mm between two points, digital radiographs can differentiate only a 0.25 mm to 0.5 mm difference between points.
The accuracy of the measurement of small distances also is compounded by the use of PACS software to measure distances. The combination of error from decreased resolution and software error may greatly affect our ability to measure small distances on digital radiographs, including fracture gaps [4]. We assume our measurements are accurate; however, there have been no published orthopaedic studies to confirm this assumption.
Long-term studies of functional outcomes in the distal radius [8, 9, 14], tibial plateau [2, 5, 13], and acetabulum [10, 11] fractures show improved outcomes with accurate reduction of the articular surface. For example, Matta [10] found that patients with an anatomic reduction after open reduction and internal fixation of acetabulum fractures achieved excellent outcomes, whereas patients with 2 mm of fracture step-off achieved poor outcomes.
The technique of acquiring digital images is different than for conventional radiography. In conventional radiography, the optical signal is derived from the light emitted in response to radiation. Digital radiography uses photostimulable phosphors, most commonly in the barium fluorohalide family, impregnated into an imaging plate or screen. The trapped charge of the latent image is released from metastable traps in a process called photostimulable luminescence (PSL). PSL causes the emission of a shorter wavelength of light (blue).
There are two types of digital radiographs, indirect and direct, which refer to the method of acquiring the image. In indirect computed radiography, an imaging plate containing the storage phosphor is placed in a light-tight cassette, exposed to the xray beam, and then placed in a reader that uses a laser to release the PSL. The PSL is detected with a photomultiplier tube (PMT) and the signal then is digitized to produce an image. In contrast, direct computed radiography directly converts the image without the intermediary step of processing a cassette [12].
The purpose of our study was to determine if it is possible to accurately measure small distances using digital radiographs and PACS software.
Patients and Methods
A model for measuring articular step-off was created using a commercially produced radiographic phantom with predetermined markings at known distances (Fig. 1). Radiographs were taken using standard techniques, with the accelerator 36 inches from the phantom and the beam centered on the phantom, and also were taken using an indirect computed radiography system (Axiom Aristos; Siemens USA, Malvern, PA, USA) and a mobile direct computed radiography system (Mobilett; Siemens USA). The images then were uploaded to a PACS system (iSite Radiology; Philips, Amsterdam, The Netherlands). Eighteen surgeons measured the distance between standardized, preselected points on the radiographic phantom. Two distances, one large and one small, were measured in millimeters for each of the two radiographs using PACS measurement tools (Fig. 2). Observers measured each value on two separate occasions, separated by 3 weeks. The measured values were compared with the known values for each measurement. Mean, median, SD, and 95% confidence intervals were calculated for each measurement. The ICC was calculated for interobserver and intraobserver reliability calculations owing to the continuous scale of the data and the number of observers.
Fig. 1.
The radiographic phantom used in our study is shown. It is composed of a plastic background imprinted with radiopaque lines at fixed, known intervals.
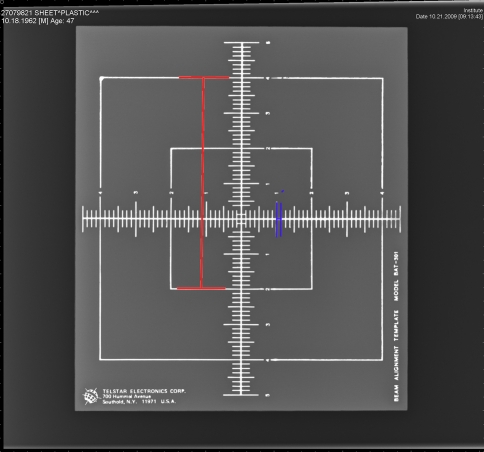
Fig. 2.
The distances measured for the indirect digital radiographs are shown.
Results
The known values for the indirect computed radiograph were 3.2 mm for the short distance and 152.4 mm for the long distance. The average measurement for the short distance was 3.1 mm (SD, 0.5 mm) with a range of 1.6 mm to 4.0 mm. The average measurement for the long distance was 153.8 mm (SD, 0.9 mm) with a range of 151.5 mm 155.2 mm. Therefore, the differences between the known value and the mean measured value for the indirect short and long measurements were 0.1 mm and 1.4 mm, respectively.
The known values for the direct computed radiograph were 203.2 mm and 6.3 mm. The average measurement was 6.3 mm (SD, 0.5 mm) with a range of 4.7 mm to 7.1 mm for the short distance and the average measurement was 205.8 mm (SD, 1.0 mm) with a range of 204.0 mm to 207.3 mm for the long distance. Therefore, the differences between the known value and the mean measured value for the indirect short and long measurements were 0 mm and 2.6 mm, respectively.
The ICCs for interobserver reliability were 0.82 for indirect and 0.75 for direct digital radiography. The ICCs for intraobserver reliability were 0.94 for indirect and 0.90 for direct digital radiography.
Discussion
The measurement of relatively small distances (1–2 mm) on radiographs has gained increasing importance regarding outcomes and indications in orthopaedic surgery. The recent transition of conventional radiographs to digital computed radiography and measurement using PACS software creates two potential sources of error in measurements. Although several studies have been published in the orthodontic literature confirming that digital radiographs are accurate for determining endodontic working length [1, 3, 7, 15], a review of the orthopaedic literature revealed no published studies confirming accuracy for orthopaedic applications. We therefore determined if it is possible to accurately measure small distances using digital radiographs and PACS software.
We acknowledge the following limitations to our study. First, caution must be taken when generalizing these results to fractures and real-life radiographs. In this study, the observers were asked to measure the distance between two discrete lines on a radiograph with no background noise or soft tissue shadows. The results of this study are applicable under ideal conditions and in vivo measurements most likely would be less accurate. Second, although the difference from the mean is small (0.1 mm in short distances and 1.4–2.6 mm in the long distances), the range (2.4 mm range for a known value of 3.1 mm) and standard deviation (0.5 mm) of measured values are large compared with the known value. This highlights the importance of comparing the measurements of multiple observers before making conclusions. Third, the selection of distances was limited by the availability of commercially produced radiographic phantoms with predetermined distances. However, having distances that were not standardized (ie, 1.0, 2.0, 3.0, etc) helped prevent bias by preventing observers from trending toward a round number for their measurement.
As expected, measurements were much closer to the known value for the small distances compared with the long distances. No observer was able to correctly measure the known value for either of the long distances. However, three subjects were able to precisely measure the short distance for the indirect radiograph, and one subject was able to measure the exact short distance for the direct radiograph.
Although the mean measured values were accurate (within 0.1 mm for a known distance of 3.2 mm), the standard deviation of measurements (0.5 mm) could affect the interpretation of data, especially in clinical situations such as when evaluating the quality of fracture reduction. For example, when considering the quality of acetabular reduction, two standard deviations (1.0 mm) make the difference between an anatomic reduction (0 mm step-off) and an imperfect reduction (1 mm step-off) indistinguishable. Although the SD for the longer distances was 1.0 mm for the indirect radiography, a 1-mm difference in applications such as leg-length discrepancy is unlikely to be clinically important.
Acknowledgments
We thank John P. Gaughan PhD and the Temple University School of Medicine Biostatistics and Consulting Center for assistance with the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Almenar Garcia A, Forner Navarro L, Ubet Castello V, Minana Laliga R. Evaluation of a digital radiography to estimate working length. J Endod. 1997;23:363–365. doi: 10.1016/S0099-2399(97)80183-5. [DOI] [PubMed] [Google Scholar]
- 2.Blokker CP, Rorabeck CH, Bourne RB. Tibial plateau fractures: an analysis of the results of treatment in 60 patients. Clin Orthop Relat Res. 1984;182:193–199. [PubMed] [Google Scholar]
- 3.Burger CL, Mork TO, Hutter JW, Nicoll B. Direct digital radiography versus conventional radiography for estimation of canal length in curved canals. J Endod. 1999;25:260–263. doi: 10.1016/S0099-2399(99)80155-1. [DOI] [PubMed] [Google Scholar]
- 4.Cole RJ, Bindra RR, Evanoff BA, Gilula LA, Yamaguchi K, Gelberman RH. Radiographic evaluation of osseous displacement following intra-articular fractures of the distal radius: reliability of plain radiography versus computed tomography. J Hand Surg Am. 1997;22:792–800. doi: 10.1016/S0363-5023(97)80016-0. [DOI] [PubMed] [Google Scholar]
- 5.Decoster TA, Nepola JV, el-Khoury GY. Cast brace treatment of proximal tibia fractures: a ten-year follow-up study. Clin Orthop Relat Res. 1988;231:196–204. [PubMed] [Google Scholar]
- 6.Garmer M, Hennigs SP, Jager HJ, Schrick F, Loo T, Jacobs A, Hanusch A, Christmann A, Mathias K. Digital radiography versus conventional radiography in chest imaging: diagnostic performance of a large-area silicon flat-panel detector in a clinical CT-controlled study. AJR Am J Roentgenol. 2000;174:75–80. doi: 10.2214/ajr.174.1.1740075. [DOI] [PubMed] [Google Scholar]
- 7.Hedrick RT, Dove SB, Peters DD, McDavid WD. Radiographic determination of canal length direct digital radiography versus conventional radiography. J Endod. 1994;20:320–326. doi: 10.1016/S0099-2399(06)80093-2. [DOI] [PubMed] [Google Scholar]
- 8.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647–659. [PubMed] [Google Scholar]
- 9.Marsh JL, Buckwalter J, Gelberman R, Dirschl D, Olson S, Brown T, Llinias A. Articular fractures: does an anatomic reduction really change the result? J Bone Joint Surg Am. 2002;84:1259–1271. [PubMed] [Google Scholar]
- 10.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 11.Matta JM, Anderson LM, Epstein HC, Hendricks P. Fractures of the acetabulum: a retrospective analysis. Clin Orthop Relat Res. 1986;205:230–240. [PubMed] [Google Scholar]
- 12.Rowlands JA. The physics of computed radiography. Phys Med Biol. 2002;47:R123–166. doi: 10.1088/0031-9155/47/23/201. [DOI] [PubMed] [Google Scholar]
- 13.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: the Toronto experience 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 14.Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994;19:325–340. doi: 10.1016/0363-5023(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 15.Woolhiser GA, Brand JW, Hoen MM, Geist JR, Pikula AA, Pink FE. Accuracy of film-based, digital, and enhanced digital images for endodontic length determination. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:499–504. doi: 10.1016/j.tripleo.2004.07.024. [DOI] [PubMed] [Google Scholar]