Abstract
Background
Patients have high reinjury rates after ACL reconstruction. Small knee flexion angles and large peak posterior ground reaction forces in landing tasks increase ACL loading.
Questions/purposes
We determined the effects of a knee extension constraint brace on knee flexion angle, peak posterior ground reaction force, and movement speed in functional activities of patients after ACL reconstruction.
Patients and Methods
Six male and six female patients 3.5 to 6.5 months after ACL reconstruction participated in the study. Three-dimensional videographic and force plate data were collected while patients performed level walking, jogging, and stair descent wearing a knee extension constraint brace, wearing a nonconstraint brace, and not wearing a knee brace. Knee flexion angle at initial foot contact with the ground, peak posterior ground reaction force, and movement speed were compared across brace conditions and between genders.
Results
Wearing the knee extension constraint brace increased the knee flexion angle at initial foot contact for each activity when compared with the other two brace conditions. Wearing the knee extension constraint brace also decreased peak posterior ground reaction force during walking but not during jogging and stair descent.
Conclusions
Although the knee extension constraint brace did not consistently reduce the peak posterior ground reaction force in all functional activities, it consistently increased knee flexion angle and should reduce ACL loading as suggested by previous studies. These results suggest the knee extension constraint brace has potential as a rehabilitation tool to alter lower extremity movement patterns of patients after ACL reconstruction to address high reinjury rates.
Level of Evidence
Level II, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
ACL rupture is a common injury in sports, leading to the highest direct medical cost of all sports injuries [9, 30]. As many as 100,000 to 250,000 people in the United States have an ACL injury each year [18, 20–22]. The US Armed Forces reports the military population has as much as 10 times the rate of ACL injuries as the general population [34]. The estimated cost for ACL reconstruction surgeries in 2000 was more than $2 billion [20]. The most recent study indicated the annual cost for ACL reconstruction surgery may be more than $4 billion [19].
ACL reconstruction surgery requires a long and costly rehabilitation. Some authors recommended patients need 4 to 6 months of rehabilitation before returning to sport activities after ACL reconstruction surgery and 6 to 9 months before returning to vigorous cutting and pivoting activities [5, 12, 15]. Although the majority of injured athletes are able to return to preinjury competition levels after rehabilitation, their performances may be adversely affected [7]. In addition, these athletes still have a higher risk of ACL reinjury [10, 13, 32, 33, 36, 37, 40] and of having secondary knee disorders develop, such as osteoarthritis, chronic knee instability, and damage to menisci and chondral surfaces [10, 16, 24, 42]. Enhanced rehabilitation techniques are needed to improve the outcome of the rehabilitation and quality of life of patients after ACL reconstruction.
A knee extension constraint brace has been designed and shown to be as effective in increasing knee flexion angle and decreasing peak posterior ground reaction force for subjects without lower extremity injuries during the landing of a stop-jump task [27, 42]. Increasing knee flexion angle and decreasing peak posterior ground reaction force during landing may reduce the risk for noncontact ACL injuries [1, 4, 14, 29, 31, 35, 42]. Therefore, this knee extension constraint brace may have potential as a rehabilitation tool to alter lower extremity movement patterns for patients after ACL reconstruction to address the high reinjury rate. Understanding the effects of wearing this knee extension constraint brace on lower extremity movement patterns in daily functional activities of the patients after ACL reconstruction is essential for future research of clinical applications of this brace.
We therefore determined the effects of the knee extension constraint brace on knee flexion angle and ground reaction forces for functional activities of patients after ACL reconstruction. We hypothesized patients wearing the knee extension constraint brace would increase their knee flexion angle at initial foot contact with the ground during level walking, jogging, and stair descent. We also hypothesized patients wearing the knee extension constraint brace would decrease peak ground reaction forces during the selected functional activities. We finally hypothesized wearing the brace would not affect the patients’ movement speeds for the selected functional activities.
Patients and Methods
Six male and six female patients 3.5 to 6.5 months after ACL reconstruction surgery were recruited for this study. The age of these subjects ranged from 18 to 32 years with an average of 22.4 years. The use of human subjects was approved by the institution’s Biomedical Internal Review Board. Written consent was obtained from each subject before data collection. Each subject’s height, weight, ACL reconstruction date, and affected leg were recorded.
Each subject was tested for three functional activities under three brace conditions. The three functional activities were (1) level walking, (2) jogging, and (3) stair descent. For level walking and jogging, the subjects approached a force plate with four to five steps, landed with the testing leg on the force plate, and completed four to five more steps. For stair descent, subjects walked down a staircase consisting of four steps with the lowest two steps rigidly connected to force plates. The height of each step was 0.18 m. The order of testing activities was randomized for each subject.
The three brace conditions were (1) with the knee extension constraint brace, (2) with a brace without the constraint, and (3) without a brace. The knee extension constraint brace was made with upright upper thigh and lower calf cuffs (Djo LLC, Vista, CA, USA). Hook-and-loop straps attached the brace to the leg. The knee extension constraint consists of a spring mechanism that applies gradual increasing resistance to knee extension from 40° flexion until 10° flexion, at which point there is a rigid stop to prevent additional extension. The resistive torque is adjustable and was set to increase gradually to a maximum of 3.5 N·m just before 10° knee flexion. The knee brace without the constraint was made identical to the constraint brace except for the constraint feature. Braces were available in extra small, small, medium, and large sizes. The order of brace condition was randomized for each patient.
Passive reflective markers were placed on the patient bilaterally at the anterior superior iliac spine, acromion process of the shoulder, lateral thigh, tibial tuberosity, distal shank, and lateral malleolus. A passive reflective marker also was placed on the L4–L5 joint. Patients were allowed to practice each task until they felt comfortable, and performed five successful trials for each combination of functional activity and brace condition at a self-selected speed. A successful trial was defined as a trial in which videographic and force plate data were successfully collected.
Eight infrared video cameras were used to record the real-time three-dimensional (3-D) trajectories of reflective markers on the subject at a frame rate of 120 frames per second. The video cameras were calibrated for a calibration volume of 2.5 m long × 1.5 m wide × 2.5 m high containing the force plates and the space in which all functional activities were performed. Ground reaction force signals from two Type 4060A Bertec force plates (Bertec Corp, Worthington, OH, USA) were collected at a sampling rate of 1000 samples per second per channel. The videographic and analog data were time-synchronized and recorded using the Peak Performance Motus videographic and analog data acquisition system (Peak Performance Technology Inc, Englewood, CO, USA). After testing all functional activities for all brace conditions, additional passive reflective markers were placed bilaterally on the lateral and medial tibial condyles and medial malleoli. A static standing trial was performed in which 3-D videographic data of all reflective markers were collected while the patient stood at the center of the area covered by the force plates.
The real-time 3-D coordinates of the reflective markers collected during each trial of functional activities were filtered through a Butterworth low-pass digital filter at an estimated optimum cutoff frequency of 10 Hz [41]. The locations of the lateral and medial tibial condyles and medial malleoli in each frame of each trial of the functional activities were estimated from the position and orientation of the tibia and the locations of the markers on the lateral and medial tibial condyles and medial malleoli relative to the tibia. The position and orientation of the tibia in a given frame were determined from the locations of the markers on the tibial tuberosity, distal tibia, and lateral malleoli in the frame. The locations of the markers on the lateral and medial tibial condyles and medial malleoli relative to the tibia were obtained from the locations of all the reflection markers in the static standing trial. The locations of hip centers were estimated as described by Bell et al. [3]. The knee center was defined as the middle point between the medial and lateral tibial condyles. The ankle center was defined as the middle point between medial and lateral malleoli. Knee angles were calculated as Euler angles of the tibia reference frame relative to the femur reference frame with flexion-extension, valgus-varus, and internal-external rotation as the first, second, and third rotations, respectively. The horizontal speeds of the hip centers at initial foot contact with the ground were averaged as the corresponding horizontal speed of the pelvis and used as an estimate of whole-body horizontal speed at the initial foot contact with the ground. Electric signals from the force plates were converted into three components of the ground reaction force vector, location of the center of pressure, and free moments. Ground reaction forces were normalized to body weight. All signal processing and data reduction were performed using MotionSoft 3-D motion data reduction program package Version 6.5 (MotionSoft Inc, Chapel Hill, NC, USA).
Two-way analyses of covariance (ANCOVAs) with mixed design were performed to compare knee flexion angle at initial foot contact and peak posterior ground reaction force for each activity. Brace condition was treated as a repeated measure, with gender as an independent measure and the horizontal speed of the pelvis as the covariate. Previous research has shown gender may affect knee flexion angle and ground reaction forces [6, 11, 23, 25, 28], therefore, gender was included to determine whether there was an interaction effect between brace condition and gender. The goal of this study was to determine the brace effect, and not the gender effect.
Two-way ANOVA with mixed design also was performed to compare the horizontal speed of the pelvis for each activity. Brace condition was treated as a repeated measure, with gender as an independent measure.
One-way ANOVA with repeated measures was performed to compare the dependent variables among brace conditions for each gender if an interaction of brace condition and gender was detected. Paired t tests were performed to locate differences if a main effect of brace condition was detected.
A Type I error rate of 0.05 was chosen to indicate statistical significance. Bonferroni adjustment was made for post hoc paired t tests to guarantee the overall Type I error rate for each ANOVA analysis. All statistical analyses were performed using SPSS Version 11 (SPSS Inc, Chicago, IL, USA).
Results
No interaction effects between brace condition and gender were present for any dependent variables in any functional activity (p ≥ 0.341).
Brace condition affected (p = 0.001) the knee flexion angle at initial foot contact for all three functional activities (Table 1). Subjects had greater (p = 0.001) knee flexion angles at initial foot contact when wearing the knee extension constraint brace compared with when wearing the nonconstraint brace and no brace (Table 1). Walking speed affected (p = 0.034) the knee flexion angle. The knee flexion angle decreased as the walking speed increased. Jogging and stair descent speeds did not affect (p ≥ 0.401) the knee flexion angle.
Table 1.
Effect of brace condition on knee flexion angle at initial foot contact with the ground
| Functional activity | Gender | Knee flexion angle (°) | ||
|---|---|---|---|---|
| Constraint brace | Nonconstraint brace | No brace | ||
| Level walking* | Female | 3.0 ± 3.1 | 0.0 ± 3.8 | −1.3 ± 3.1 |
| Male | 5.3 ± 2.9 | 1.6 ± 2.5 | 1.5 ± 3.2 | |
| Jogging* | Female | 11.2 ± 4.5 | 6.9 ± 5.2 | 6.5 ± 4.0 |
| Male | 11.6 ± 2.2 | 8.3 ± 2.6 | 7.6 ± 2.6 | |
| Stair descending* | Female | 13.6 ± 2.3 | 9.6 ± 1.9 | 6.7 ± 2.5 |
| Male | 18.2 ± 6.7 | 14.4 ± 6.9 | 13.7 ± 6.1 | |
Values are expressed as mean ± SD; *knee flexion angle was greater when wearing the constraint brace than when wearing the nonconstraint brace (p = 0.001) and no brace (p = 0.001).
Brace condition affected (p = 0.021) peak posterior ground reaction force for level walking (Table 2). Subjects had lower peak posterior ground reaction forces when wearing the knee extension constraint brace than when wearing the nonconstraint brace (p = 0.025) and no brace (p = 0.007) (Table 2). Brace condition did not affect the peak posterior ground reaction force for jogging (p = 0.538) and stair descent (p = 0.390) (Table 2). Walking speed affected (p = 0.009) the peak posterior ground reaction force. The peak posterior ground reaction force decreased as the walking speed increased. Jogging and stair descent speeds did not affect the peak posterior ground reaction force (p ≥ 0.368).
Table 2.
Effect of brace condition on peak posterior ground reaction force
| Functional activity | Gender | Peak posterior ground reaction force (body weight) | ||
|---|---|---|---|---|
| Constraint brace | Nonconstraint brace | No brace | ||
| Level walking* | Female | 0.155 ± 0.041 | 0.179 ± 0.055 | 0.193 ± 0.053 |
| Male | 0.167 ± 0.034 | 0.197 ± 0.072 | 0.192 ± 0.065 | |
| Jogging | Female | 0.138 ± 0.075 | 0.119 ± 0.064 | 0.158 ± 0.090 |
| Male | 0.181 ± 0.114 | 0.223 ± 0.124 | 0.205 ± 0.095 | |
| Stair descending | Female | 0.017 ± 0.096 | 0.027 ± 0.073 | 0.022 ± 0.086 |
| Male | 0.034 ± 0.048 | 0.043 ± 0.063 | 0.050 ± 0.038 | |
Values are expressed as mean ± SD; *peak posterior ground reaction force was lower when wearing the constraint brace than when wearing the nonconstraint brace (p = 0.025) and no brace (p = 0.007).
Brace condition affected (p = 0.035) walking speed (Table 3). Patients had lower walking speeds when wearing the constraint brace and nonconstraint brace than when wearing no brace (p = 0.001 and p = 0.012, respectively). Brace condition also affected (p = 0.043) the stair descent speed (Table 3). Subjects had greater stair descent speeds when wearing the knee extension constraint brace and when wearing no brace than when wearing the nonconstraint knee brace (p = 0.002 and p = 0.019, respectively). Brace condition did not affect (p = 0.876) horizontal jogging speed (Table 3).
Table 3.
Effect of brace condition on horizontal movement speed
| Functional activity | Gender | Horizontal movement speed (m/s) | ||
|---|---|---|---|---|
| Constraint brace | Nonconstraint brace | No brace | ||
| Level walking*,† | Female | 1.54 ± 0.15 | 1.54 ± 0.08 | 1.63 ± 0.09 |
| Male | 1.56 ± 0.13 | 1.64 ± 0.30 | 1.69 ± 0.20 | |
| Jogging | Female | 2.63 ± 0.37 | 2.54 ± 0.31 | 2.55 ± 0.29 |
| Male | 2.74 ± 0.28 | 2.76 ± 0.25 | 2.77 ± 0.29 | |
| Stair descending‡ | Female | 0.76 ± 0.09 | 0.72 ± 0.11 | 0.75 ± 0.09 |
| Male | 0.87 ± 0.14 | 0.78 ± 0.09 | 0.83 ± 0.09 | |
Values are expressed as mean ± SD; *movement speed was lower (p = 0.001) when wearing the constraint brace than when wearing no brace; †movement speed was lower (p = 0.012) when wearing the nonconstraint brace than when wearing no brace; ‡movement speed was lower when wearing the nonconstraint brace than when wearing the constraint brace (p = 0.002) and no brace (p = 0.019).
Discussion
Patients have high reinjury rates after ACL reconstruction. Small knee flexion angles and large peak posterior ground reaction forces in landing tasks increase ACL loading. We determined the effects of a knee extension constraint brace on knee flexion angle, peak posterior ground reaction force, and movement speed in functional activities of patients after ACL reconstruction.
Our study has several limitations that should be considered in future studies. The knee extension constraint brace was designed to modify lower extremity sagittal plane biomechanics for dynamic activities. Evaluation of the effects of the knee extension constraint brace on lower extremity kinematics and kinetics was focused on sagittal plane mechanisms in this study. Although one study on ACL loading showed sagittal plane biomechanics are the major contributors to ACL loading, knee valgus-varus and internal rotation moments also affect ACL loading [29]. Future studies should determine the effects of the knee extension constraint brace on nonsagittal plane biomechanics. Also, although we showed the knee extension constraint brace altered the knee flexion angle at initial contact and peak posterior ground reaction force for our patients, we did not measure ACL loading or the probability for ACL injuries with altered lower extremity motion patterns. Future studies are needed to develop methods to measure ACL loading in vivo to confirm the effects of the knee extension constraint brace. Additionally, the nonsignificant effects of the constraint brace on the ground reaction forces might be consequences of Type II errors owing to small sample size. Future studies with large sample sizes may be needed to reevaluate the effect of the constraint brace on the ground reaction force.
Our results support our first hypothesis that after ACL reconstruction, patients would increase their knee flexion angle at initial foot contact for selected functional activities while wearing the knee extension constraint brace. These results are consistent with those of previous studies for recreational athletes without ACL injuries [27, 42].
Our results partially support our second hypothesis that after ACL reconstruction, patients would decrease their peak posterior ground reaction forces during selected functional activities while wearing the knee extension constraint brace. Our results showed that after ACL reconstruction, patients decreased their peak posterior ground reaction force during level walking while wearing the knee extension constraint brace. These results are also consistent with those of previous studies for recreational athletes without ACL injuries [27, 42]. However, our patients did not show a decrease in the peak posterior ground reaction force during jogging and stair descent while wearing the knee extension constraint brace. These results suggest the effect of wearing the constraint brace on peak posterior ground reaction force during jogging and stair descent is inconsistent across functional activities.
Our results also partially support our third hypothesis that after reconstruction, patients would not change their movement speeds while wearing the knee extension constraint brace. Although wearing the constraint brace had no major effect on horizontal jogging speed, it resulted in a decrease in the horizontal walking speed and an increased stair descent speed. Considering the jogging speed was greater than the level walking and stair descending speeds, we hypothesize the brace affects the performance of lower-speed tasks but not high-speed tasks. Future studies are needed to test this hypothesis.
The observed differences in knee flexion angle at the initial foot contact and peak posterior ground reaction force across brace conditions should be considered as the effect of brace condition, instead of effects of movement speed. The ANCOVAs showed walking speed and brace condition contributed to the variations of knee flexion angle and peak posterior ground reaction force. The ANCOVAs also showed jogging and stair descent speeds did not contribute to the variations in knee flexion angle and peak posterior ground reaction force for jogging and stair descent. These results indicate the differences in knee flexion angle and peak posterior ground reaction force across brace conditions are not attributable to variation in movement speed.
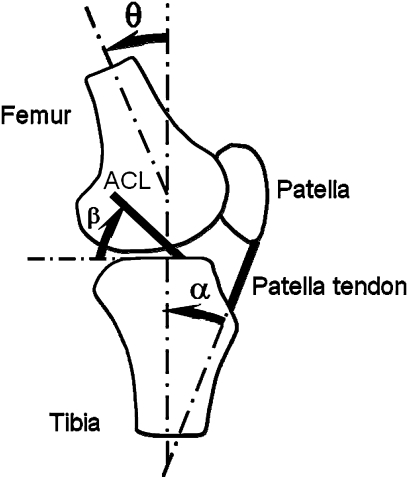
Increasing the knee flexion angle in functional activities after ACL reconstruction surgery should protect ACL grafts from excessive loading independent of posterior ground reaction force. ACL loading decreases as knee flexion angle increases, especially when the knee flexion angle is less than 30° [29]. At a given knee flexion angle, ACL loading decreases as the anterior shear force applied on the proximal end of the tibia decreases [17, 38]. The relationship between ACL loading and knee flexion angle is attributable to the relationships between the patellar tendon-tibial shaft angle and knee flexion angle and between the ACL elevation angle and knee flexion angle (Fig. 1). The patellar tendon-tibial shaft angle decreases as the knee flexion angle increases [31]. With constant quadriceps muscle force, therefore, the anterior shear force applied on the knee decreases as knee flexion angle increases [31]. The ACL elevation angle also decreases as the knee flexion angle increases [26], therefore, ACL loading decreases as knee flexion angle increases for a given anterior shear force at the knee.
Fig. 1.
The patellar tendon-tibial shaft angle (α), ACL elevation angle (β), and knee flexion angle (θ) are shown.
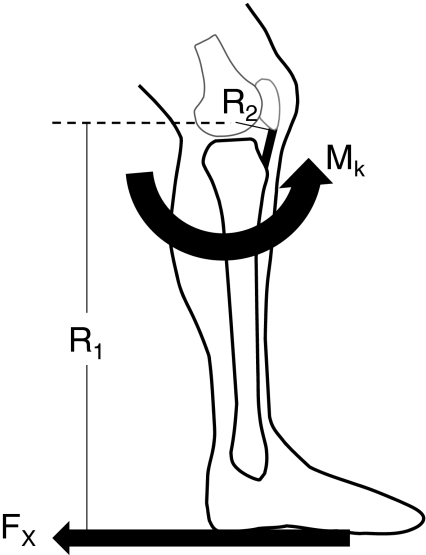
Decreasing peak posterior ground reaction force for functional activities after ACL reconstruction surgery also should protect the ACL from excessive loading [39]. The posterior ground reaction force generates a knee flexion moment that must be resisted by a knee extension moment generated by the quadriceps muscles through the patellar tendon. Decreasing the posterior ground reaction force decreases the required internal knee extension moment, thus decreasing the quadriceps and patellar tendon forces (Fig. 2). Decreasing patellar tendon force decreases the anterior shear force imposed on the ACL when the knee flexion angle is less than 60° [2, 31]. An in vivo study showed the peak ACL loading occurs at the time of impact peak vertical ground reaction force during a hop landing task [8], and the impact peak posterior and vertical ground reaction forces occur essentially at the same time during a stop-jump task [43]. These studies show the important effect of the peak posterior ground reaction force on ACL loading and the risk of noncontact ACL injury.
Fig. 2.
The diagram illustrates posterior ground reaction force (Fx), moment arm of posterior ground reaction force (R1), knee extension moment (Mk), and moment arm of the patella tendon (R2).
Our results combined with those of previous studies suggest the constraint brace has potential as a rehabilitation tool to improve outcomes of the rehabilitation after ACL reconstruction. Our patients increased knee flexion angles for all three functional activities and decreased peak posterior ground reaction force for level walking while wearing the constraint brace. Previous studies have shown increasing knee flexion angle and decreasing peak posterior ground reaction force decrease ACL loading, indicating the knee extension constraint brace may protect patients after ACL reconstruction from excessive ACL loading. Use of the knee extension construction brace may enable earlier return to sports and exercise after ACL reconstruction. Additionally, the altered lower extremity movement patterns may decrease the risk of reinjury after ACL reconstruction if the altered lower extremity movement patterns persist after removal of the brace. Future studies are needed to explore these possibilities.
Footnotes
Christopher Stanley contributed to this article in his personal capacity. The views expressed are his own and do not necessarily represent the views of the National Institutes of Health or the United States Government.
One of the authors (BY) has received funding from DJO LLC (Vista, CA). All other authors certify that they have no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at University of North Carolina at Chapel Hill.
References
- 1.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. Am J Sports Med. 1995;23:694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 2.Arms SW, Pope MH, Johnson RJ, Fischer RA, Arvidsson I, Eriksson E. The biomechanics of anterior cruciate ligament rehabilitation and reconstruction. Am J Sports Med. 1984;12:8–18. doi: 10.1177/036354658401200102. [DOI] [PubMed] [Google Scholar]
- 3.Bell AL, Pedersen DR, Brand RA. A comparison of the accuracy of several hip center location prediction methods. J Biomech. 1990;23:617–621. doi: 10.1016/0021-9290(90)90054-7. [DOI] [PubMed] [Google Scholar]
- 4.Berns GS, Hull ML, Patterson HA. Strain in the anteromedial bundle of the anterior cruciate ligament under combination loading. J Orthop Res. 1992;10:167–176. doi: 10.1002/jor.1100100203. [DOI] [PubMed] [Google Scholar]
- 5.Beynnon BD, Uh BS, Johnson RJ, Abate JA, Nichols CE, Fleming BC, Poole AR, Roos H. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med. 2005;33:347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- 6.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 7.Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34:1911–1917. doi: 10.1177/0363546506290186. [DOI] [PubMed] [Google Scholar]
- 8.Cerulli G, Benoit DL, Lamontagne M, Caraffa A, Liti A. In vivo anterior cruciate ligament strain behaviour during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003;11:307–311. doi: 10.1007/s00167-003-0403-6. [DOI] [PubMed] [Google Scholar]
- 9.Cumps E, Verhagen E, Annemans L, Meeusen R. Injury risk and socioeconomic costs resulting from sports injuries in Flanders: data derived from sports insurance statistics 2003. Br J Sports Med. 2008;42:767–772. doi: 10.1136/bjsm.2007.037937. [DOI] [PubMed] [Google Scholar]
- 10.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 11.Decker MJ, Torry MR, Wyland DJ, Sterett WI, Steadman JR. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon) 2003;18:662–669. doi: 10.1016/S0268-0033(03)00090-1. [DOI] [PubMed] [Google Scholar]
- 12.Delay BS, Smolinski RJ, Wind WM, Bowman DS. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Knee Surg. 2001;14:85–91. [PubMed] [Google Scholar]
- 13.DeVita P, Lassiter T, Jr, Hortobagyi T, Torry M. Functional knee brace effects during walking in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 1998;26:778–784. doi: 10.1177/03635465980260060701. [DOI] [PubMed] [Google Scholar]
- 14.DeVita P, Torry M, Glover KL, Speroni DL. A functional knee brace alters joint torque and power patterns during walking and running. J Biomech. 1996;29:583–588. doi: 10.1016/0021-9290(95)00115-8. [DOI] [PubMed] [Google Scholar]
- 15.Feller JA, Cooper R, Webster KE. Current Australian trends in rehabilitation following anterior cruciate ligament reconstruction. Knee. 2002;9:121–126. doi: 10.1016/S0968-0160(02)00009-1. [DOI] [PubMed] [Google Scholar]
- 16.Finsterbush A, Frankl U, Matan Y, Mann G. Secondary damage to the knee after isolated injury of the anterior cruciate ligament. Am J Sports Med. 1990;18:475–479. doi: 10.1177/036354659001800505. [DOI] [PubMed] [Google Scholar]
- 17.Fleming BC, Renstrom PA, Beynnon BD, Engstrom B, Peura GD, Badger GJ, Johnson RJ. The effect of weightbearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34:163–170. doi: 10.1016/S0021-9290(00)00154-8. [DOI] [PubMed] [Google Scholar]
- 18.Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1997;79:1556–1576. doi: 10.2106/00004623-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Garrett WE, Jr, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ, Harrast J, Derosa GP. American Board of Orthopaedic Surgery Practice of the Orthopaedic Surgeon: Part-II, certification examination case mix. J Bone Joint Surg Am. 2006;88:660–667. doi: 10.2106/JBJS.E.01208. [DOI] [PubMed] [Google Scholar]
- 20.Gottlob CA, Baker CL, Jr, Pellissier JM, Colvin L. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272–282. doi: 10.1097/00003086-199910000-00034. [DOI] [PubMed] [Google Scholar]
- 21.Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE, Garrick JG, Hewett TE, Huston L, Ireland ML, Johnson RJ, Kibler WB, Lephart S, Lewis JL, Lindenfeld TN, Mandelbaum BR, Marchak P, Teitz CC, Wojtys EM. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE, Jr, Hannafin JA, Hewett TE, Huston LJ, Ireland ML, Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, Myklebust G, Noyes FR, Powers C, Shields C, Jr, Shultz SJ, Silvers H, Slauterbeck J, Taylor DC, Teitz CC, Wojtys EM, Yu B. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II Meeting, January 2005. Am J Sports Med. 2006;34:1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 23.Heijne A, Fleming BC, Renstrom PA, Peura GD, Beynnon BD, Werner S. Strain on the anterior cruciate ligament during closed kinetic chain exercises. Med Sci Sports Exerc. 2004;36:935–941. doi: 10.1249/01.MSS.0000128185.55587.A3. [DOI] [PubMed] [Google Scholar]
- 24.Irvine GB, Glasgow MM. The natural history of the meniscus in anterior cruciate insufficiency: arthroscopic analysis. J Bone Joint Surg Br. 1992;74:403–405. doi: 10.1302/0301-620X.74B3.1587888. [DOI] [PubMed] [Google Scholar]
- 25.James CR, Sizer PS, Starch DW, Lockhart TE, Slauterbeck J. Gender differences among sagittal plane knee kinematic and ground reaction force characteristics during a rapid sprint and cut maneuver. Res Q Exerc Sport. 2004;75:31–38. doi: 10.1080/02701367.2004.10609131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li G, DeFrate LE, Rubash HE, Gill TJ. In vivo kinematics of the ACL during weight-bearing knee flexion. J Orthop Res. 2005;23:340–344. doi: 10.1016/j.orthres.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Lin CF, Liu H, Garrett WE, Yu B. Effects of a knee extension constraint brace on selected lower extremity motion patterns during a stop-jump task. J Appl Biomech. 2008;24:158–165. doi: 10.1123/jab.24.2.158. [DOI] [PubMed] [Google Scholar]
- 28.Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon) 2001;16:438–445. doi: 10.1016/S0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- 29.Markolf KL, Burchfield DI, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 30.Miyasaka KC, Daniel DM, Stone ML, Hirshman P. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;4:3–8. [Google Scholar]
- 31.Nunley RM, Wright D, Renner JB, Yu B, Garrett WE., Jr Gender comparison of patellar tendon tibial shaft angle with weight bearing. Res Sports Med. 2003;11:173–185. [Google Scholar]
- 32.Oates KM, Eenenaam DP, Briggs K, Homa K, Sterett WI. Comparative injury rates of uninjured, anterior cruciate ligament-deficient, and reconstructed knees in a skiing population. Am J Sports Med. 1999;27:606–610. doi: 10.1177/03635465990270051001. [DOI] [PubMed] [Google Scholar]
- 33.Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29:196–200. doi: 10.1177/03635465010290021301. [DOI] [PubMed] [Google Scholar]
- 34.Owens BD, Mountcastle SB, Dunn WR, DeBerardino TM, Taylor DC. Incidence of anterior cruciate ligament injury among active duty US military servicemen and servicewomen. Mil Med. 2007;172:90–91. doi: 10.7205/milmed.172.1.90. [DOI] [PubMed] [Google Scholar]
- 35.Pandy MG, Shelburne KB. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech. 1997;30:1015–1024. doi: 10.1016/S0021-9290(97)00070-5. [DOI] [PubMed] [Google Scholar]
- 36.Ramsey DK, Wretenberg PF, Lamontagne M, Nemeth G. Electromyographic and biomechanic analysis of anterior cruciate ligament deficiency and functional knee bracing. Clin Biomech (Bristol, Avon) 2003;18:28–34. doi: 10.1016/S0268-0033(02)00138-9. [DOI] [PubMed] [Google Scholar]
- 37.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 38.van den Bogert AJ, McLean SG. Comment: effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2006;34:312–315; Author reply: 313–315. [DOI] [PubMed]
- 39.Dijck RA, Saris DB, Willems JW, Fievez AW. Additional surgery after anterior cruciate ligament reconstruction: can we improve technical aspects of the initial procedure. Arthroscopy. 2008;24:88–95. doi: 10.1016/j.arthro.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 40.Walden M, Hagglund M, Ekstrand J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med. 2006;40:158–162. doi: 10.1136/bjsm.2005.021055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yu B, Gabriel D, Noble L, An KN. Estimate of the optimum cutoff frequency for the Butterworth low-pass digital filter. J Appl Biomech. 1999;15:318–329. [Google Scholar]
- 42.Yu B, Herman D, Preston J, Lu W, Kirkendall DT, Garrett WE. Immediate effects of a knee brace with a constraint to knee extension on knee kinematics and ground reaction forces in a stop-jump task. Am J Sports Med. 2004;32:1136–1143. doi: 10.1177/0363546503262204. [DOI] [PubMed] [Google Scholar]
- 43.Yu B, Lin CF, Garrett WE. Lower extremity biomechanics during the landing of a stop- jump task. Clin Biomech (Bristol, Avon). 2006;21:297–305. doi: 10.1016/j.clinbiomech.2005.11.003. [DOI] [PubMed] [Google Scholar]