Abstract
Background
Posterior-stabilized TKAs, which use a polyethylene tibial post to articulate against a metal femoral cam, are used regularly. Reported complications are related to the patellofemoral articulation or the tibial post-cam mechanism. Fracture of the tibial post is an uncommon but disabling complication after posterior-stabilized TKA that requires operative treatment.
Questions/purposes
The literature was reviewed to determine the frequency of tibial post fracture and address three questions: (1) Is there a specific prosthetic design or patient demographics in knees with a fracture of the tibial post? (2) What are the common presenting complaints and methods of diagnosis? (3) What methods of treatment have been used?
Methods
A PubMed search of English language articles from February 1982 to April 2010 was performed and 20 articles, all Level IV studies, were identified.
Results
One specific design of posterior-stabilized tibial post with a central screw hole had a 12.4% incidence of fracture. Tibial post fracture has been reported with other designs, but with an incidence of 1% or less. The most common presenting symptoms include effusion, instability, or patella clunk syndrome. The most common method of diagnosis was clinical examination followed by arthroscopic examination. Treatment with revision to a new tibial polyethylene liner generally has been successful at short-term followup.
Conclusions
Tibial post fracture is a relatively uncommon complication after posterior-stabilized TKA that usually is treated successfully with liner exchange. The low quality of available literature makes it difficult to recommend a specific treatment protocol.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Posterior-cruciate ligament-substituting (PS) designs are commonly used for TKA. The first PS prosthesis, designed by Insall and Burstein, introduced a polyethylene tibial spine that engaged a metal cam on the femoral component during knee flexion [16]. This provided for better knee flexion and stairclimbing ability, compared with the original total condylar prosthesis, without an increase in component loosening [1, 10, 16]. The tibial post and femoral cam design has been used with success in subsequent TKA implant designs during the past 25 years [1, 10, 13, 20–22, 31]. Complications reported with the PS-design TKA implants may be related to the patellofemoral articulation, with patella clunk syndrome or crepitus, or to the post and cam mechanism, with tibial post wear, impingement, or breakage [27, 30].
The tibial spine-post femoral cam mechanism of a posterior-stabilized TKA implant was designed to engage only on the posterior side of the tibial post during flexion to improve femoral rollback and increase the amount of knee flexion. However, three retrieval studies of several designs of PS prostheses showed wear and deformation on the anterior side of the tibial post [7, 14, 30]. In one study of four different designs, 40% of the tibial post surface showed some form of deformation, and seven of 23 posts (30%) had severe damage, with gross loss of polyethylene [30]. A wide variability in wear patterns was related to differences in post location, geometry, and mechanics. In a study of seven revised knees with two different PS designs, there was osteolysis, presumably attributable to anterior tibial post wear and backside tibial component liner wear [7]. With one design, this post damage was attributable to anterior post impingement caused by flexion of the femoral component and excessive posterior slope of the tibial component. There was also a possibility of rotational force transmission to the tibial post-femoral cam mechanism with the other design. One study of 234 retrieved implants with two different post locations reported greater wear damage in implants with a more anterior post placement [14]. In a cadaveric study of seven knees with a single design second-generation PS prosthesis (NexGen LPS, Zimmer, Warsaw, IN, USA), anterior post impingement was found at low flexion angles of simulated heel strike and 0º to −9º hyperextension [24]. Using electron microscopy, a retrieval study of another PS design (Genesis II constrained, Smith and Nephew, Schenefeld, Germany) found anterior and posterior post fissures in all seven polyethylene liners at a mean of only 25 months in situ [33]. This design generates rotational constraint, with rotational load acting at the anterior and posterior corners of the post.
A systematic review of the literature of PS TKA implants was performed to determine the frequency of fracture of the tibial post and to address three questions: (1) is there a difference in prosthetic design or patient demographics in knees with a fracture of the tibial post; (2) what are the common presenting complaints and methods of diagnosis; and (3) what methods of treatment have been used?
Search Strategy and Criteria
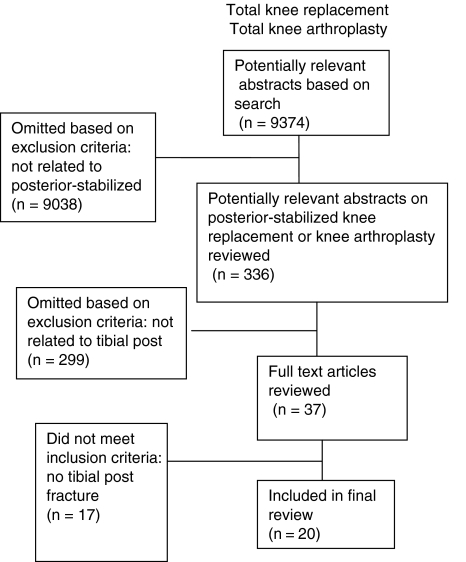
I first performed a comprehensive literature search to locate articles describing PS TKA. PubMed was searched for articles with the following MeSH entries: “total knee arthroplasty”, “posterior stabilized knee arthroplasty”, and “tibial post fracture”. The dates of the searches were from February 1, 1982 and April 23, 2010. These terms were taken in various combinations using the Boolean operators “AND” and “OR”. With the additional limitations of English language only and studies on humans only, the search yielded 9374 for “total knee replacement”, 5956 citations for “total knee arthroplasty”, 336 citations for “total knee arthroplasty and/or posterior stabilized”, and 37 citations for “posterior stabilized knee and tibial post and/or fracture”. The same key words used in the PubMed search were used in the EMBASE search, with limitations to English language only and studies on humans only. This search yielded 1764 citations for “total knee arthroplasty”, 468 citations for “posterior stabilized”, and 12 citations for “tibial post fracture”. Finally, appropriate articles were searched for in the Cochrane Database. Of 6153 abstracts dealing with “knee” or “tibia”, 17 abstracts and papers with tibial post fracture were reviewed for applicability. No limits were placed on the studies for number of patients, study design, absence of patient demographics, or length of followup. The bibliographies of identified studies were reviewed for other applicable articles. These searches resulted in 20 relevant articles for data extraction (Fig. 1).
Fig. 1.
A flowchart shows the literature searches for articles related to tibial post fractures
A standardized paper form was used to assist in data extraction from each study (Appendix 1). This form was used to extract patient-related factors, implant-related factors, diagnostic and treatment factors, and outcomes if available. Patient-related factors included number of patients, number of knees, mean age and weight or body mass index, patient gender, preoperative diagnosis, and history of trauma. Implant-related factors included implant type and manufacturer and months in situ. Diagnostic factors included the use of clinical examination, radiographs and other imaging modalities, and diagnostic arthroscopy. The treatment modality, followup time, and outcomes were recorded if available.
Results
It is difficult to determine the exact incidence of tibial post fracture. Hendel et al. reported an incidence of 1.2% (five of 332) with the Insall-Burstein II prosthesis (Zimmer) implanted during a 5-year period at one center [15]. In another study of this prosthesis, the incidence of tibial post fracture was 0.51% (one of 193 knees) with 5 to 14 years followup [20]. Bal et al. reported 70 of 564 (12.4%) consecutive PS prostheses (Foundation-100 Series Total Knee System®, Encore Orthopaedics, Austin, TX, USA) had revision surgery because of catastrophic failure of the tibial post [4]. However, this tibial post had a defective design, with a central hole in the post to allow screw fixation of the tibial liner to the metal tibial tray. These polyethylene components were machined from standard ram-extruded bar stock and sterilized with gamma irradiation in air or nitrogen, followed by vacuum packaging. The exact shelf life of these components was unknown, but estimated at less than 5 years from the date of manufacture. In addition to this large report of 70 tibial post fractures, and an earlier report of five fractures with the same prosthesis [27], there are only 27 total reported cases of tibial post fractures in 18 published articles (Table 1) in the English language during the past 10 years [3, 5, 8, 9, 11, 14, 15, 17–20, 23, 25, 26, 28–30, 32]. In these case series, the highest incidence was 1.2% [15], with most reporting less than 1%. As the prosthesis with a central hole in the post had an obvious design flaw, cases using it will be analyzed separately from the other 27 reported cases. In the study of 70 fractured tibial posts with a central screw hole, there were substantial demographic differences between patients with and without tibial post fractures [4]. The patients with tibial post fractures were younger (64 versus 68 years), had a greater weight (204 versus 181 lbs), and were more likely to be males (71% versus 42%). The symptoms described by these patients were instability, pain, and patella clunking in 36 knees, and combinations of these symptoms in the remaining 34 knees. The mean time between index surgery and revision was 40 months (range, 24–83 months). The diagnosis usually was made if there was the presence of patella clunking and a positive posterior drawer test with the knee flexed greater than 90º. These patients were treated by revision using a deep-dish congruent tibial liner, with a mean followup of 28 months (range, 13–61 months). There were eight different posterior-stabilized prostheses in the 27 other cases of tibial post fractures: 11 Insall-Burstein II® [9, 14, 15, 20, 28], one Insall-Burstein I® [14], three NexGen® (all Zimmer) [8, 11, 23], four Scorpio® (Stryker, Mahwah NJ, USA) [17, 18, 25], four Genesis® (Smith & Nephew, Memphis, TN, USA) [19, 26, 30], two PFC-Sigma® [3, 32], one AMK (both DePuy, Warsaw IN, USA) [29], and one Dual-Articular® [5] (Biomet, Warsaw IN, USA). There were 18 women and five men (gender was not reported for four patients [four knees]). The mean patient age, reported for 23 patients (23 knees), was 63.4 years (range, 44–85 years). The preoperative diagnosis, reported for 17 knees, was osteoarthritis in 12, rheumatoid arthritis in three, posttraumatic arthritis in one, and revision in one. The patient weight, reported in only five cases, ranged from 66 to 123 kg (mean, 95.2 kg). The time in situ, stated in 22 cases, ranged from 2 to 100 months (mean, 37.9 months). For the 23 patients with a history, there was no trauma in 17 patients and a definite history of trauma in six patients.
Table 1.
Case reports of tibial post fractures
| Study | Patient age (years) | Gender | Patient weight (kg) | Diagnosis | Months in situ | Symptoms | Prosthesis | Trauma | Diagnostic tests | Treatment | Followup (months) | Comments |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bal et al. [3] | 68 | Female | 106 | Rheumatoid arthritis | 22 | Instability | PFC Sigma® (DePuy, Warsaw, IN, USA) | No | None | Liner exchange | 17 | Failed owing to tibial malrotation; revised to constrained condylar |
| Boesen et al. [5] | 65 | Female | 123 | Posttraumatic arthritis | 48 | Instability | Dual-Articular PS® (Biomet, Warsaw, IN, USA) | Yes | None | Liner exchange | 3 | |
| Chiu et al. [8] | 44 | Female | 66 | Rheumatoid arthritis | 63 | Effusion, recurvatum | NexGen® (Zimmer, Warsaw, IN, USA) | No | None | Liner exchange | 2 | |
| Clarke et al. [9] | 51 | Female | ns | Osteoarthritis | 63 | Effusion, popliteal cyst | Insall-Burstein II® (Zimmer, Warsaw IN, USA) | No | CT scan, arthroscopy | Liner exchange | 27 | |
| D’Angelo et al. [11] | 63 | Female | 100 | Osteoarthritis | 100 | Instability, effusion | NexGen® | No | Arthroscopy | Liner exchange | 6 | |
| Furman et al. [14] | ns | ns | ns | ns | ns | ns | Insall-Burstein II® 3 knees; Insall-Burstein I® 1 knee | ns | ns | ns | ns | |
| Hendel et al. [15] | 74 | Female | ns | ns | 38 | Pain, effusion, instability | Insall-Burstein II® | No | ns | Revision, rotating hinge | 5–8 years | |
| 69 | Female | ns | ns | 42 | Pain, effusion, instability | Insall-Burstein II® | No | ns | Revision, rotating hinge | 5–8 years | ||
| 68 | Female | ns | ns | 50 | Pain, effusion, instability | Insall-Burstein II® | No | ns | Liner exchange | 5–8 years | Medial collateral ligament reefing and knee brace in extension 6 weeks | |
| 56 | Female | ns | ns | 38 | Pain, effusion, instability | Insall-Burstein II® | No | ns | Liner exchange | 5–8 years | Medial collateral ligament reefing and knee brace in extension 6 weeks | |
| 76 | Male | ns | ns | 61 | Posterior dislocation | Insall-Burstein II® | No | ns | Revision, rotating hinge | 5–8 years | ||
| Jung et al. [17] | 55 | Female | ns | Osteoarthritis | 2 | Pain, effusion, locking | Scorpio X3® (Stryker, Mahwah, NJ, USA) | No | None | Liner exchange | ns | |
| 60 | Female | ns | Osteoarthritis | 4 | Pain, effusion, instability | Scorpio X3® | No | None | Liner exchange | ns | ||
| Jung et al. [18] | 58 | Female | ns | Osteoarthritis | 3 | Mass, effusion, instability | Scorpio X3® | No | Arthroscopy | Liner exchange | ns | |
| Kruger et al. [19] | 55 | Male | ns | Osteoarthritis | ns | Pain, locking | Genesis® (Smith and Nephew, Memphis TN, USA) | Yes | Arthroscopy | Excision fragment only | ns | |
| 60 | Female | ns | Osteoarthritis | 39 | Instability, locking | Genesis® | Yes | Arthroscopy | Liner exchange | ns | ||
| Lachiewicz and Soileau [20] | 51 | Female | 80 | Rheumatoid arthritis | 65 | Pain, effusion, instability | Insall-Burstein II® | No | None | Liner exchange | 48 | |
| Lee et al. [23] | 63 | Male | BMI 27.8 | Osteoarthritis | 36 | Instability | NexGen Flex® | No | None | Liner exchange | 18 | |
| Lim et al. [25] | 72 | Female | ns | Osteoarthritis | 14 | Pain, effusion, recurvatum | Scorpio® | Yes | MRI, arthroscopy | Liner exchange | 24 | |
| Mariconda et al. [26] | 77 | Male | ns | Revision aseptic loosening | 36 | Pain, effusion, instability | Genesis® | No | Arthroscopy | Liner exchange | 12 | |
| Mestha et al. [28] | 85 | Female | ns | Osteoarthritis | 33 | Posterior subluxation | Insall-Burstein II® | No | None | Liner exchange | ns | |
| Ng and Chiu [29] | 55 | Female | ns | Osteoarthritis | 21 | Recurrent dislocations | AMK® (DePuy, Warsaw IN, USA) | Yes | Arthrogram | Revision | ns | |
| Puloski et al. [30] | 68 | Male | ns | Osteoarthritis | 35 | Instability | Genesis® | No | ns | ns | ns | |
| Sands and Silver [32] | 67 | Female | ns | ns | 48 | Instability | PFC Sigma® | No | None | Liner exchange | 60 |
ns = not stated in study; BMI = body mass index; CT = computerized axial tomography; MRI = magnetic resonance imaging
The presenting symptoms of tibial post fracture were pain, effusion, and instability in 10 patients, instability alone in nine, dislocation in two, a palpable mass in one, and effusion with symptomatic popliteal cyst in one. Symptoms were not reported for four patients. The diagnosis of tibial spine fracture was made using only clinical examination in 15 knees, arthroscopic examination in seven knees (two of which also had CT and MRI), and contrast arthrography in one knee. The method of diagnosis was not reported for four knees.
The treatment for the fracture of the tibial post was tibial polyethylene liner exchange with another posterior-stabilized component in 18 knees. The liner thickness was increased from 2 mm to 6 mm in most knees. Only one of these knees failed, owing to component malrotation, and rerevision of all components to a constrained, condylar prosthesis was performed [3]. However, length of followup was reported for only 12 patients (12 knees) at a mean of 28.6 months (range, 2–60 months). For four knees, the initial treatment was revision of the components, three of which had a rotating hinge prosthesis [15, 29]. Followup of 5 to 8 years was reported for these three knees. One knee was treated with arthroscopic excision of the fractured tibial post alone, but followup was not reported. The treatment for four knees was not reported.
Discussion
Although PS prostheses are commonly used for various arthritic knee problems, complications related to the tibial post and femoral cam mechanism are relatively uncommon. The goal of this systematic review was to address three questions: (1) is there a difference in prosthetic design or patient demographics in knees with a fracture of the tibial post; (2) what are the common presenting complaints and methods of diagnosis; and (3) what are the methods of treatment that have been used?
After performing this evidence-based review, it is clear that the literature is limited. First, there are no Level I or Level II studies. Most of the studies are case reports and biomechanical retrieval studies of tibial post fracture and its treatment. It is difficult to make informed treatment recommendations as we rely on Level IV studies typically with limited numbers of selected patients for our decision-making. Second, current studies are characterized by poor reporting of demographic data and radiographic alignment and lack of medium-term followup after treatment. Success of treatment was poorly defined in most studies. Other than the three reports of fractured tibial posts fabricated from highly cross-linked polyethylene [17, 18, 25], the quality of the polyethylene used in the knees was not reported. Third, there may be some selection bias from restricting my searches to the English language. Fourth, the studies span more than 10 years and surgical techniques evolve and improve with time, which can affect results.
One specific prosthetic design that was associated with the highest incidence of tibial post fracture was identified. This prosthesis had a hole in the post for screw fixation of the polyethylene liner to the tibial tray [4, 27]. Revision for catastrophic failure of the tibial post was necessary in 12.4% of knees at a mean of 40 months postoperatively [4]. These patients were different from patients in the other group with fractures of the tibial post, in that they were predominantly male, and they were younger and heavier than the patients without fractures of the post. The presenting complaint with this prosthesis after the post fracture included patella clunking in most knees, which was not seen in the other group with tibial post fractures. These findings likely indicate some unique design flaw with this PS prosthesis and its tibial post. The treatment of these failed knees was also different than that of the other group, with the use of a deep dish congruent liner in all patients, with successful results at short-term followup.
In the other group of 27 tibial post fractures, there were eight different prosthetic designs from five different implant manufacturers, indicating that the complication of tibial post fracture can occur with various designs. One particular design, the Insall-Burstein II® prosthesis, had 11 fractures. In a retrieval study, Furman et al. reported that the post damage and fracture probably were related to this design having a more anterior post location than the Insall-Burstein I® prosthesis [14]. However, there were possible confounding variables in that study, such as excessive flexion or valgus alignment of the femoral component and posterior slope of the tibial component, that led to impingement, post wear, and eventual fracture [14]. Malalignment of PS components in either the sagittal or coronal planes likely is related to tibial post fracture, but a review of the literature could not prove this.
The presenting symptoms of tibial post fracture most commonly include pain, effusion, and instability, but instability alone was frequently reported. These complaints and the lack of a traumatic event in most cases indicate that the history and physical examination findings are not specific for tibial post fracture, and a high degree of clinical suspicion is necessary. There were no characteristic radiographic findings and other methods of imaging were used so infrequently that no strong recommendation can be made. Arthroscopic examination was diagnostic in the seven cases in which it was used, so perhaps this is warranted when the diagnosis or need for revision surgery is uncertain. However, almost all patients with severe symptoms will require some type of revision surgery, therefore the necessity of routine arthroscopy of unstable PS knees probably is not warranted.
The most frequent treatment for tibial post fracture was reoperation with PS liner exchange, usually increasing the thickness of the liner by 2 mm to 6 mm. However, a strong recommendation in support of this treatment is not possible, owing to the lack of followup in many cases, and the short-term followup (mean, 28.6 months) in the other cases. The use of tibial liner exchange for various knee problems, including instability and wear, was questioned in three Level IV studies [2, 6, 12]. Brooks et al. reported failure in 29% (four of 14) of revisions with polyethylene exchange only for prosthetic knee instability [6]. Revision of the components to constrained condylar or rotating-hinge components was performed infrequently in these cases. The best available data provided by this review suggest that PS tibial liner exchange may be successful, at least for 2 to 5 years followup, in many patients with fracture of the tibial post if alignment of the components is satisfactory. High-quality, multicenter, randomized trials comparing liner exchange with full revision of components are needed to confirm the results of this systemic review.
Acknowledgment
I thank Stephen Pearlman for help with the literature search.
Appendix 1. Tibial post fracture data extraction form
Study author
Number of knees (patients)
Patient age at time of index arthroplasty
Patient gender
Primary preoperative diagnosis
Patient weight or body mass index
Months in situ before fracture occurred
Brand of total knee arthroplasty prosthesis
Presenting symptoms
Trauma involved: Yes, No
Preoperative diagnostic procedures
Treatment
Followup time
Reoperations
Footnotes
One of the institutions of the author (Chapel Hill Orthopedics Surgery and Sports Medicine) has received funding from Zimmer, for support of other studies.
References
- 1.Abdeen AR, Collen SB, Vince KG. Fifteen-year to 19-year follow-up of the Insall-Burstein-I total knee arthroplasty. J Arthroplasty. 2010;25:173–178. doi: 10.1016/j.arth.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Babis GC, Trousdale RT, Morrey BF. The effectiveness of isolated tibial insert exchange in revision total knee arthroplasty. J Bone Joint Surg Am. 2002;84:64–68. doi: 10.2106/00004623-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Bal BS, Greenberg D. Failure of a metal-reinforced tibial post in total knee arthroplasty. J Arthroplasty. 2007;22:464–467. [DOI] [PubMed]
- 4.Bal BS, Greenberg D, Li S, Mauerhan D, Schultz L, Cherry K. Tibial post failures in a condylar posterior cruciate substituting total knee arthroplasty. J Arthroplasty. 2008;23:650–655. doi: 10.1016/j.arth.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Boesen MP, Jensen TT, Husted H. Secondary knee instability caused by fracture of the stabilizing insert in a dual-articular total knee. J Arthroplasty. 2004;19:941–943. doi: 10.1016/j.arth.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 6.Brooks DH, Fehring TK, Griffin WL, Mason JB, McCoy TH. Polyethylene exchange only for prosthetic knee instability. Clin Orthop Relat Res. 2002;405:182–188. doi: 10.1097/00003086-200212000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan JJ, O’Rourke MR, Goetz DD, Schmalzried TP, Campbell PA, Johnston RC. Tibial post impingement in posterior-stabilized total knee arthroplasty. Clin Orthop Relat Res. 2002;404:83–88. doi: 10.1097/00003086-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Chiu YS, Chen WM, Huang CK, Chiang CC, Chen TH. Fracture of the polyethylene tibial post in a NexGen posterior-stabilized knee prosthesis. J Arthroplasty. 2004;19:1045–1049. doi: 10.1016/j.arth.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Clarke HD, Math KR, Scuderi GR. Polyethylene post failure in posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19:652–657. doi: 10.1016/j.arth.2004.02.026. [DOI] [PubMed] [Google Scholar]
- 10.Colizza WA, Insall JN. Scuderi GR: The posterior stabilized total knee prosthesis: assessment of polyethylene damage and osteolysis after a ten-year minimum follow-up. J Bone Joint Surg Am. 1995;77:1713–1720. doi: 10.2106/00004623-199511000-00011. [DOI] [PubMed] [Google Scholar]
- 11.D’Angelo F, Marcolli D, Bulgheroni P, Murena L, Congiu T, Cherubino P. Two stage fracture of a polyethylene post in a 9-year-old posterior-stabilized knee prosthesis: a case report. J Med Case Reports. 2010;4:65. doi: 10.1186/1752-1947-4-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Engh GA, Koralewicz LM, Pereles TR. Clinical results of modular polyethylene insert exchange with retention of total knee arthroplasty components. J Bone Joint Surg Am. 2000;82:516–523. doi: 10.2106/00004623-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Font-Rodriguez DE, Scuderi GR. Insall JN: Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79–86. doi: 10.1097/00003086-199712000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Furman BD, Lipman J, Klingman M, Wright TM, Haas SB. Tibial post wear in posterior-stabilized knee replacements is design-dependent. Clin Orthop Relat Res. 2008;466:2650–2655. doi: 10.1007/s11999-008-0422-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hendel D, Garti A, Weisbort M. Fracture of the central polyethylene tibial spine in posterior stabilized total knee arthroplasty. J Arthroplasty. 2003;18:672–674. doi: 10.1016/S0883-5403(03)00192-X. [DOI] [PubMed] [Google Scholar]
- 16.Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: a modification of the total condylar design. Two to four-year clinical experience. J Bone Joint Surg Am. 1982;64:1317–1323. [PubMed] [Google Scholar]
- 17.Jung KA, Lee SC, Hwang SH, Kim SM. Fracture of a second-generation highly cross-linked UHMWPE tibial post in a posterior-stabilized Scorpio knee system. Orthopedics. 2008;31:1137–1139. doi: 10.3928/01477447-20081101-10. [DOI] [PubMed] [Google Scholar]
- 18.Jung KA, Lee SC, Hwang SH, Kim SM. Fractured polyethylene tibial post in a posterior-stabilized knee prosthesis presenting as a floating palpable mass. J Knee Surg. 2009;22:374–376. doi: 10.1055/s-0030-1247780. [DOI] [PubMed] [Google Scholar]
- 19.Kruger T, Reichel H, Decker T, Hein W. Arthroscopy after dysfunctional total knee arthroplasty: two cases with peg fracture of the polyethylene insert. Arthroscopy. 2000;16:E21. doi: 10.1053/jars.2000.16286. [DOI] [PubMed] [Google Scholar]
- 20.Lachiewicz PF, Soileau ES. The rates of osteolysis and loosening associated with a modular posterior stabilized knee replacement: results at five to fourteen years. J Bone Joint Surg Am. 2004;86:525–530. doi: 10.1302/0301-620X.86B8.15438. [DOI] [PubMed] [Google Scholar]
- 21.Lachiewicz PF, Soileau ES. Fifteen-year survival and osteolysis associated with a modular posterior stabilized knee replacement: a concise follow-up of a previous report. J Bone Joint Surg Am. 2009;91:1419–1423. doi: 10.2106/JBJS.H.01351. [DOI] [PubMed] [Google Scholar]
- 22.Laskin RS. The Genesis total knee prosthesis: a 10-year followup study. Clin Orthop Relat Res. 2001;388:95–102. doi: 10.1097/00003086-200107000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Lee CS, Chen WM, Kou HC, Lo WH, Chen CL. Early nontraumatic fracture of the polyethylene tibial post in a NexGen LPS-flex posterior stabilized knee prosthesis. J Arthroplasty. 2009;24:1292.e5–1292.e9. [DOI] [PubMed]
- 24.Li G, Papannagari R, Most E, Park SE, Johnson T, Tanamal L, Rubash HE. Anterior tibial post impingement in a posterior stabilized total knee arthroplasty. J Orthop Res. 2005;23:536–541. doi: 10.1016/j.orthres.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Lim HC, Bae JH, Hwang JH, Kim SJ, Yoon JY. Fracture of a polyethylene tibial post in a Scorpio posterior-stabilized knee prosthesis. Clin Orthop Surg. 2009;1:118–121. doi: 10.4055/cios.2009.1.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mariconda M, Lotti G, Milano C. Fracture of posterior-stabilized tibial insert in a Genesis knee prosthesis. J Arthroplasty. 2000;15:529–530. doi: 10.1054/arth.2000.4810. [DOI] [PubMed] [Google Scholar]
- 27.Mauerhan DR. Fracture of the polyethylene tibial post in a posterior cruciate-substituting total knee arthroplasty mimicking patellar clunk syndrome: a report of 5 cases. J Arthroplasty. 2003;18:942–945. doi: 10.1016/S0883-5403(03)00333-4. [DOI] [PubMed] [Google Scholar]
- 28.Mestha P, Shenava Y, D’Arcy JC. Fracture of the polyethylene tibial post in posterior stabilized (Insall-Burstein II) total knee arthroplasty. J Arthroplasty. 2000;15:814–815. doi: 10.1054/arth.2000.6615. [DOI] [PubMed] [Google Scholar]
- 29.Ng TP, Chiu KY. Recurrent dislocation of total knee arthroplasty: an unusual cause. J Arthroplasty. 2003;18:1067–1070. doi: 10.1016/j.arth.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 30.Puloski SK, McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB. Tibial post wear in posterior stabilized total knee arthroplasty: an unrecognized source of polyethylene debris. J Bone Joint Surg Am. 2001;83:390–397. doi: 10.2106/00004623-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Ranawat CS, Luessenhop CP, Rodriguez JA. The press-fit condylar modular total knee system: four-to-six year results with a posterior-cruciate substituting design. J Bone Joint Surg Am. 1997;79:342–348. doi: 10.2106/00004623-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Sands KC, Silver JW. Fracture of the polyethylene tibial post in a posterior stabilized PFC total knee arthroplasty. Orthopedics. 2005;28:1203–1204. doi: 10.3928/0147-7447-20051001-20. [DOI] [PubMed] [Google Scholar]
- 33.Skwara A, Tibesku CO, Reichelt R, Fuchs-Winkelmann S. Damages of the tibial post in constrained total knee prostheses in the early postoperative course: a scanning electron microscopic study of polyethylene inlays. BMC Musculoskelet Disord. 2008;9:83. doi: 10.1186/1471-2474-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]