Abstract
Background
Several studies have reported functional recovery of the shoulder after arthroscopic rotator cuff repair (ARCR). Preoperative estimation of the time required for functional recovery is important for determining surgical indications and for planning timing of the surgery and an appropriate postoperative physical therapy.
Questions/purposes
We therefore asked: (1) how long it takes to obtain functional recovery after ARCR, and (2) what preoperative factors influence functional recovery time.
Patients and Methods
We retrospectively evaluated 201 patients who had undergone ARCR. Using the Japanese Orthopaedic Association (JOA) shoulder scoring system, we defined the functional recovery period as the time required to achieve a score greater than 80% in each component. We evaluated the functional recovery periods and assessed preoperative influencing factors such as age, gender, shoulder stiffness, morphologic features of rotator cuff tears, and rotator cuff tear size.
Results
Sixty-three patients (31%) took less than 3 months, 81 patients (40%) took between 3 and 6 months, and 57 patients (28%) took greater than 6 months to achieve a score greater than 80% in each JOA shoulder assessment component. Younger patients without shoulder stiffness and with smaller rotator cuff tears had shorter functional recovery periods.
Conclusions
One hundred forty-four patients (72%) obtained functional recovery within 6 months after ARCR. Age, shoulder stiffness, and rotator cuff tear size influenced functional recovery time.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
A rotator cuff tear is a common and sometimes debilitating injury of the shoulder. Surgical repair of a chronic rotator cuff tear is indicated when nonoperative treatment fails, and the patient otherwise is a reasonable surgical candidate. Low morbidity such as a quick decrease in postoperative pain [5, 6, 29] and rapid functional recovery within 12 months [1, 7] after shoulder arthroscopy have accelerated the development of this technique in the past 20 years.
The techniques used for rotator cuff repair have evolved from the traditional open or mini-open repair to ARCR [34]. ARCR is now a well-established surgical technique, and some studies [17, 30] have reported functional recovery and tendon healing in patients undergoing ARCR for rotator cuff injuries. Although several studies have reported restoration of shoulder function using the Constant-Murley [9], UCLA [11], and American Shoulder and Elbow Surgeons (ASES) [18] at followup periods of 2 to 14 years [20, 35, 36], the time required for functional recovery after surgery was reported in only one study [7].
Postoperative clinical improvement is important for evaluating the general effects of each surgical treatment: preoperative estimation of the time required for functional recovery is helpful for determining surgical indications, the timing of surgery, and appropriate postoperative physical therapy. Faster functional recovery may be desirable in younger patients and slower recovery may be acceptable for older patients.
The time required for functional recovery reportedly is related to several factors including age [19], rotator cuff tear size [22, 30], preoperative muscle weakness [28], and joint mobility [8]. In the literature, the information varies widely regarding the prognostic factors of rotator cuff repair [2, 3, 11, 13]. In young patients, rotator cuff repair has been used successfully for treating small tears detected at an early stage [2, 3, 13]. However, the surgical effect has been insufficient in patients with abductor muscle weakness and joint movement restriction, which are detected at a later stage [11]. These findings may indicate younger patients should undergo surgical treatment earlier than older patients. Further, because of poor functional recovery, surgical indications should be chosen more carefully for older patients diagnosed with a rotator cuff injury at a later stage than for patients diagnosed at an earlier stage. The surgical indications and timing vary according to the age, physical status, and requirements of the patients. The time required for functional recovery is likely an important factor affecting patients’ decisions to undergo ARCR.
We therefore asked (1) how long it takes to obtain functional recovery after ARCR, and (2) what preoperative factors influence functional recovery time.
Patients and Methods
We retrospectively reviewed 254 patients who underwent arthroscopic repairs for full- or partial-thickness rotator cuff tears between July 2001 and July 2007. The indications for surgery were insufficient recovery after at least 6 months nonoperative treatment; we attempted to ensure all patients had a good understanding of the importance of postoperative rehabilitation and agreed to participate. The contraindications for surgery were (1) poor general condition, and (2) anticipated poor compliance with postoperative physical therapy. Of the 254 patients we excluded 53 for the following reasons: (1) accompanying diseases (20 patients): calcifying tendinitis (12 patients), hemodialysis-related shoulder disease (three patients), recurrent shoulder dislocation (three patients), rheumatoid arthritis (one patient), ganglion (one patient); (2) insufficient operative record (19 patients); (3) posttraumatic (10 patients); and (4) lost to followup (four patients). This left 201 patients (79%) for review. There were 126 men and 75 women. The average age of the patients at surgery was 61.4 years (range, 33–83 years). The minimum followup was 6 months (average, 27.6 months; range, 6–78 months). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. This study was approved by our IRB.
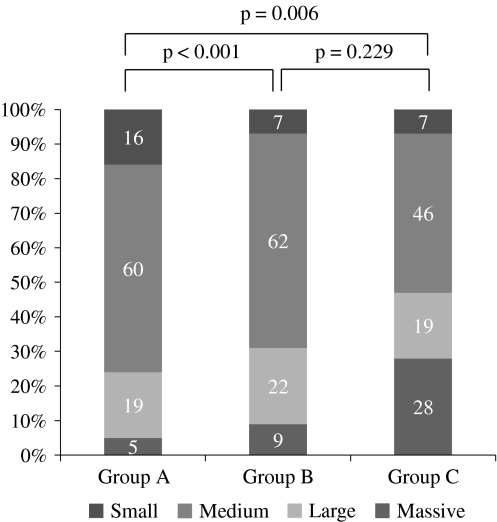
Two of the authors (TM, IM) measured the longitudinal and transverse dimensions of the tear on the preoperative MRI along the oblique coronal plane and oblique sagittal plane respectively by using a previously described method [31]. The tear sizes were classified as: small (< 1 cm), medium (1–3 cm), large (3–5 cm), and massive (> 5 cm) [10]. In this study, we observed 20 small tears, 115 medium tears, 40 large tears, and 26 massive tears.
All patients underwent preoperative physical therapy, with exercises for stretching and strengthening the cuffs, for more than 6 months and nonoperative treatment with NSAIDs. The patients were prohibited from performing pain-inducing physical activities. Patients not responding to nonoperative treatment underwent surgery if we believed they understood and could conform to the postoperative physiotherapy program. The primary purpose of the surgery was to relieve pain and the secondary purpose was functional recovery.
Shoulder arthroscopy was performed with the patient under general anesthesia and in the lateral decubitus position. All patients were operated on by the same surgeon (YI). All the patients underwent subacromial decompression for subacromial impingement. To determine whether the cuff tear could be repaired surgically, we performed debridement of the tear ends and investigated mobility of the tendon using arthroscopic holders. The tear was evaluated as reparable if the tendon could easily be brought to the original footprint without causing any stress. The patients who fulfilled the reparability criteria underwent ARCR by using suture anchors. Double-row repair was performed in 51 patients and single-row repair was performed in 150 patients. When the rotator cuff tear was the delamination type, we performed double-row repair. In patients with bursal-side partial thickness tears and in those with greater than 50% thickness of the articular side, the partial thickness tears were repaired. Arthroscopic capsulotomy was performed for patients with less than 120° in maximum rotational angles; total external and internal rotation angles at 90° abduction who, while under general anesthesia, were considered to have shoulder stiffness. Associated disorders and concomitant procedures were as follows: superior labrum anterior posterior (SLAP) lesions were observed in 54 patients and biceps disorders were observed in 24. SLAP debridement was performed in 48 patients and SLAP repairs were performed in six. A biceps tenotomy was performed in one patient and biceps tenodesis was performed in eight. Capsulotomies were performed in 126 patients with shoulder stiffness; osteoarthritis was found in 15 patients and intraarticular debridement was performed. Subscapularis tears were observed in 35 patients and repaired in all.
After surgery, the patients’ shoulders were immobilized using shoulder abduction braces. To minimize the risk of retears we uniformly used 30° abduction braces for small and medium-size tears and 60° abduction braces for large and massive-size tears. Pendulum, passive elevation, and external rotation exercises were started the second day after surgery. In the sixth week, the shoulder abduction braces were removed and stretching exercises were started to increase the movement span; strengthening exercises were started in the eighth week. These exercises were continued for 6 months.
Clinical assessment of the shoulder was performed at 3 and 6 months postoperatively and consisted of a structured interview, detailed physical examination, and evaluation using the shoulder rating scale of the Japanese Orthopaedic Association (JOA) [15]. The shoulder assessment was used to determine level of pain (30 points), function including abduction strength and endurance (10 points), activities of daily living (10 points), ROM (30 points), radiographic evaluation (5 points), and joint stability (15 points); the maximum total score was 100 points.
On the basis of the JOA shoulder assessment, we considered functional recovery had occurred when the pain score was greater than 24 points, function score was greater than 8 points, activities of daily living score was greater than 8 points, and ROM score was greater than 24 points. The functional recovery period was defined as the time required to achieve a score greater than 80% in each JOA shoulder assessment component. The patients were divided into three groups on the basis of the recovery periods: Group A was comprised of patients with recovery periods less than 3 months, Group B had recovery periods between 3 and 6 months, and Group C had recovery periods greater than 6 months. The patients were divided into two age groups: patients 60 years or older and patients 59 years or younger.
We assessed preoperative factors including age, gender, shoulder stiffness, morphologic features of rotator cuff tears, and rotator cuff tear size, which may have influenced the functional recovery periods in each group. To determine the relationship between the functional recovery periods and the preoperative factors (age, gender, shoulder stiffness, morphologic features of rotator cuff tears, rotator cuff tear size), we used the Kruskal-Wallis and Bonferroni/Dunn tests. All analyses were conducted using StatView software (Abacus Concepts, Berkeley, CA, USA).
Results
To achieve a score greater than 80% in each JOA shoulder assessment component, it took 63 patients (31.3%) less than 3 months (Group A), 81 patients (40.3%) between 3 and 6 months (Group B), and 57 patients (28.4%) greater than 6 months (Group C). The mean active forward flexion improved from 125° preoperatively to 147° and 161° at 3- and 6-month followups, respectively (p < 0.001 and p < 0.001, respectively). The mean active abduction improved from 104° preoperatively to 134° and 153°at 3- and 6-month followups, respectively (p < 0.001 and p < 0.001, respectively). The mean total JOA score improved from 59 points preoperatively to 83 and 91 points at 3- and 6-month followups, respectively (p < 0.001 and p < 0.001, respectively).
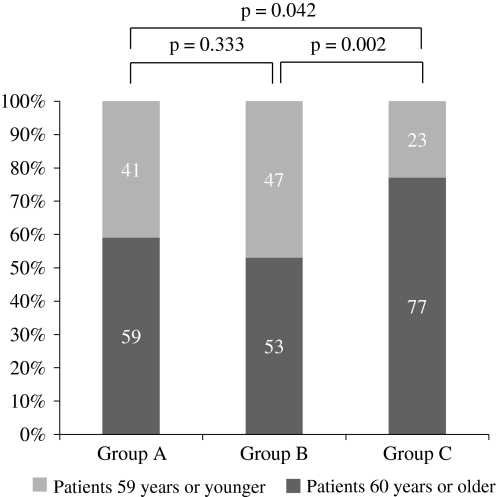
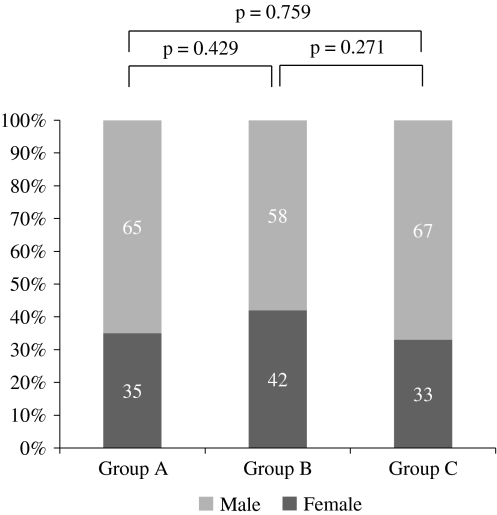
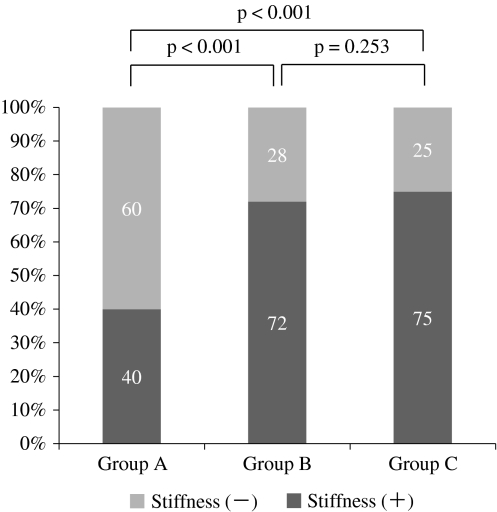
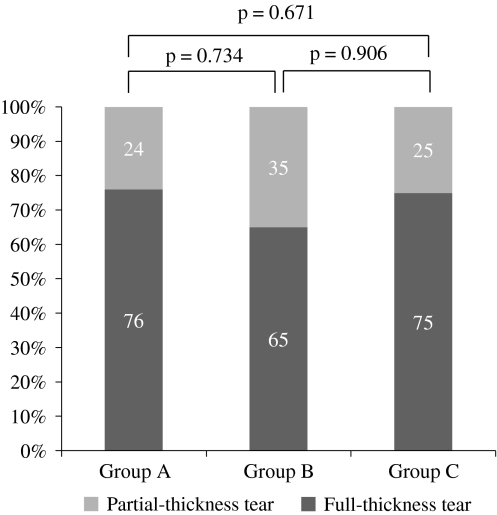
Age, shoulder stiffness, and rotator cuff tear size were the main preoperative factors influencing the functional recovery period. The percentage of patients 60 years or older was 59% in Group A, 53% in Group B, and 77% in Group C; the percentage of patients 60 years or older in Group C was higher (p = 0.002) than in Group B (Fig. 1). Gender did not influence the postoperative functional recovery periods (Fig. 2). Preoperative shoulder stiffness had an influence on postoperative functional recovery period. The percentages of patients with preoperative shoulder stiffness were 40%, 72%, and 75% in Groups A, B, and C, respectively. The incidence of preoperative shoulder stiffness was lower in Group A than Group B (p < 0.001) and Group C (p < 0.001) (Fig. 3). Morphologic features of rotator cuff tears (partial-thickness or full-thickness rotator cuff tears) did not influence the postoperative functional recovery periods (Fig. 4). The percentage of smaller tears was greater in Group A than in Groups B and C (p < 0.001 and p = 0.006 respectively); the rate of larger tears was greater in Group C than in Group A (p = 0.006). The rates of small tears were 16%, 7%, and 7% in Groups A, B, and C, respectively. The incidences of massive tears were 5%, 9%, and 28% in Groups A, B, and C, respectively (Fig. 5).
Fig. 1.
A graph shows variations in the functional recovery periods according to patient age. The percentage of patients 60 years or older in Group C was higher than in Group B.
Fig. 2.
The functional recovery periods according to gender were similar as shown in this graph.
Fig. 3.
The incidence of preoperative shoulder stiffness was observed frequently in Groups B and C.
Fig. 4.
Morphologic features of the rotator cuff tear did not influence the postoperative functional recovery period.
Fig. 5.
A graph shows the effect of rotator cuff tear size on the functional recovery period. The rate of smaller tears was higher in Group A than in Groups B and C, and the rate of larger tears was higher in Group C than in Group A.
There was one intraoperative implant-related complication. There were no postoperative infections. Six patients had postoperative shoulder stiffness and 13 had retears.
Discussion
ARCR has become an increasingly common treatment, and several studies have reported restoration of function [7, 17, 30]. Only Charousset et al. [7] reported it took 12 months after ARCR to achieve maximum recovery. To confirm that study, we therefore asked: (1) how long it takes to obtain functional recovery after ARCR, and (2) what preoperative factors influence functional recovery time.
Our study has some limitations. First, postoperative followup was 6 months; we specifically focused on early functional recovery and a 6-month followup was considered adequate. However, Charousset et al. [7] reported functional recovery is observed as early as 3 months after surgery and recovery progresses until 12 months postoperatively, when it reaches a plateau. We suggest future studies should have longer followups; such studies will be able to evaluate preoperative factors influencing late functional recovery after 6 months. Second, we did not have followup MRI for all patients to document tendon healing and therefore could not analyze the relationship between repair integrity and functional recovery. Third, we used two surgical methods, ie, single-row and double-row repairs. The study of one surgical method might allow less variable findings.
Our data suggest approximately 30% of patients achieve functional recovery within 3 months after ARCR, 40% between 3 and 6 months, and 30% greater than 6 months. A number of studies have reported preoperative factors influencing functional outcomes after rotator cuff repair (Table 1). Feng et al. [12] reported aging was the main factor in progressive degeneration of the rotator cuff and aging should be considered the most important factor contributing to the pathogenesis of rotator cuff tears. Age-dependent decline of healing potential in degenerated rotator cuffs and age-dependent progression of shoulder dysfunction caused by rotator cuff tears have been observed [4, 26]. Oh et al. [22] reported postoperative clinical outcomes were lower in older patients. Our results are consistent with these findings. Gender did not influence the functional recovery period. Charousset et al. [7] reported female gender was a negative predictive factor for improvement of clinical results. However, Feng et al. [12] reported gender was not correlated with postoperative outcome. There is no consensus regarding this issue. Several studies suggest preoperative stiffness does not affect the final outcome [23, 32]. Oh et al. [23] reported moderate preoperative shoulder stiffness does not affect the clinical outcomes of rotator cuff repairs if arthroscopic capsular release with manipulation is added to the index procedure. Cho et al. [8] reported the final outcomes were equally good in patients with or without stiffness, but restoration of ROM is slower in patients with full-thickness rotator cuff tears and stiffness of the shoulder. However, these studies reported the clinical outcomes more than 6 months after surgery. We assessed early functional recovery and found shoulder stiffness may be a preoperative factor influencing the functional recovery period. Hsu et al. [14] reported patients with partial tears of the rotator cuff had better clinical scores than those with complete tears. However, morphologic features of the rotator cuff tear did not influence functional recovery time in our study. Rotator cuff tear size is another factor affecting the functional recovery after ARCR. Although one previous study indicated tear size does not affect the clinical results [25], another showed a close relationship between tear size and the postoperative function [21]. Oh et al. [22] also reported the tear size correlated with clinical outcomes. Ozbaydar et al. [24] suggested the size of rotator cuff tears affects the results of surgical repair because the patients diagnosed with large tears generally have poor tendon quality and severe tendon retraction. Our observations are consistent with these findings. We found postoperative rehabilitation periods were longer for patients with larger tears than for those with smaller tears because of severe functional deficits.
Table 1.
Preoperative influencing factors after rotator cuff repair reported in the literature
| Study | Preoperative influencing factors for functional outcomes | Outcome times (months) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age | Tear size | Stiffness | Fatty degeneration | Retraction | Muscle strength | Gender | Tear morphology | ||
| Charousset et al. [7] | × | ND | ND | ND | ND | ND | ○ | ND | 3–31 |
| Cho & Rhee [8] | ND | ND | ○ | ND | ND | ND | ND | ND | 0.75–74 |
| Feng et al. [12] | × | ○ | × | ○ | ○ | ○ | × | ○ | 12–336 |
| Hsu et al. [14] | ND | ND | ND | ND | ND | ND | ND | ○ | 24–85 |
| Nho et al. [21] | × | ○ | ND | ND | ND | ND | ○ | ND | 12–24 |
| Oh et al. [22] | ○ | ○ | ND | × | ND | ND | ○ | ND | 12–39 |
| Oh et al. [23] | ND | ND | × | ND | ND | ND | ND | ND | 3–32 |
| Ozbaydar et al. [24] | ○ | ○ | × | ○ | ○ | × | ND | ND | 12–61 |
| Shen et al. [28] | ND | ND | ND | ND | ND | ○ | ND | ND | 57–77 |
| Current study | ○ | ○ | ○ | ND | ND | ND | × | × | 3–6 |
○ = significantly different; × = not significantly different; ND = not described.
Several methods are available for clinical assessment of the shoulder. The UCLA [11], Constant-Murley [9], and ASES [18] scores are commonly used in Europe and the United States. The JOA shoulder assessment score is frequently used in Japan, and its usefulness has been described [15, 16, 27, 33]. This shoulder assessment includes measurement of the level of shoulder pain, function including abduction strength endurance, activities of daily living, ROM, radiographic evaluation, and joint stability, thereby allowing objective estimation of several clinical parameters. Previous studies [15, 25, 35, 36] have reported a shoulder assessment score greater than 80% after ARCR was a “good” or “excellent” clinical outcome; therefore, we regarded 80% in each component as a standard value for functional recovery.
Our data suggest one can expect that patients who are 59 years or younger before surgery can achieve good functional recovery within 6 months of undergoing ARCR, and patients with smaller tears and without stiffness may recover within 3 months. The functional recovery period after ARCR may depend on the patient’s age, absence or presence of stiffness, and size of tears. Patients who are younger, have no stiffness, and have smaller tears may have shorter functional recovery periods after ARCR.
Acknowledgments
We thank Doctors Yoshihiro Nakao, Yoshifumi Naka, and Hiroyasu Tomo for assistance during surgery and for postoperative patient care.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Baker CL, Liu SH. Comparison of open and arthroscopically assisted rotator cuff repairs. Am J Sports Med. 1995;23:99–104. doi: 10.1177/036354659502300117. [DOI] [PubMed] [Google Scholar]
- 2.Bassett RW, Cofield RH. Acute tears of the rotator cuff: the timing of surgical repair. Clin Orthop Relat Res. 1983;175:18–24. [PubMed] [Google Scholar]
- 3.Björkenheim JM, Paavolainen P, Ahovuo J, Slätis P. Surgical repair of the rotator cuff and surrounding tissues: factors influencing the results. Clin Orthop Relat Res. 1988;236:148–153. [PubMed] [Google Scholar]
- 4.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 5.Boszotta H, Prünner K. Arthroscopically assisted rotator cuff repair. Arthroscopy. 2004;20:620–626. doi: 10.1016/j.arthro.2004.04.058. [DOI] [PubMed] [Google Scholar]
- 6.Buess E, Steuber KU, Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy. 2005;21:597–604. doi: 10.1016/j.arthro.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Charousset C, Grimberg J, Duranthon LD, Bellaïche L, Petrover D, Kalra K. The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008;24:25–33. doi: 10.1016/j.arthro.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 8.Cho NS, Rhee YG. Functional outcome of arthroscopic repair with concomitant manipulation in rotator cuff tears with stiff shoulder. Am J Sports Med. 2008;36:1323–1329. doi: 10.1177/0363546508314402. [DOI] [PubMed] [Google Scholar]
- 9.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 10.DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563–567. [PubMed] [Google Scholar]
- 11.Ellman H, Hanker G, Bayer M. Repair of the rotator cuff: end-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 12.Feng S, Guo S, Nobuhara K, Hashimoto J, Mimori K. Prognostic indicators for outcome following rotator cuff tear repair. J Orthop Surg (Hong Kong) 2003;11:110–116. doi: 10.1177/230949900301100202. [DOI] [PubMed] [Google Scholar]
- 13.Hawkins RJ, Misamore GW, Hobeika PE. Surgery for full-thickness rotator-cuff tears. J Bone Joint Surg Am. 1985;67:1349–1355. [PubMed] [Google Scholar]
- 14.Hsu SL, Ko JY, Chen SH, Wu RW, Chou WY, Wang CJ. Surgical results in rotator cuff tears with shoulder stiffness. J Formos Med Assoc. 2007;106:452–461. doi: 10.1016/S0929-6646(09)60294-1. [DOI] [PubMed] [Google Scholar]
- 15.Ide J, Maeda S, Takagi K. A comparison of arthroscopic and open rotator cuff repair. Arthroscopy. 2005;21:1090–1098. doi: 10.1016/j.arthro.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Ide J, Tokiyoshi A, Hirose J, Mizuta H. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg Am. 2007;89:2378–2388. doi: 10.2106/JBJS.G.00082. [DOI] [PubMed] [Google Scholar]
- 17.Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J Bone Joint Surg Am. 2009;91:1055–1062. doi: 10.2106/JBJS.G.00118. [DOI] [PubMed] [Google Scholar]
- 18.King GJ, Richards RR, Zuckerman JD, Blasier R, Dillman C, Friedman RJ, Gartsman GM, Iannotti JP, Murnahan JP, Mow VC, Woo SL. A standardized method for assessment of elbow function. Research Committee, American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 1999;8:351–354. doi: 10.1016/S1058-2746(99)90159-3. [DOI] [PubMed] [Google Scholar]
- 19.Lam F, Mok D. Open repair of massive rotator cuff tears in patients aged sixty-five years or over: is it worthwhile? J Shoulder Elbow Surg. 2004;13:517–521. doi: 10.1016/j.jse.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 20.Murray TF, Jr, Lajtai G, Mileski RM, Snyder SJ. Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to 6-year follow-up. J Shoulder Elbow Surg. 2002;11:19–24. doi: 10.1067/mse.2002.120142. [DOI] [PubMed] [Google Scholar]
- 21.Nho SJ, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg. 2009;18:697–704. doi: 10.1016/j.jse.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25:30–39. doi: 10.1016/j.arthro.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Oh JH, Kim SH, Lee HK, Jo KH, Bin SW, Gong HS. Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008;24:983–991. doi: 10.1016/j.arthro.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Ozbaydar MU, Tonbul M, Tekin AC, Yalaman O. Arthroscopic rotator cuff repair: evaluation of outcomes and analysis of prognostic factors][in Turkish. Acta Orthop Traumatol Turc. 2007;41:169–174. [PubMed] [Google Scholar]
- 25.Ozbaydar MU, Tonbul M, Yalaman O. [The results of arthroscopic repair of full-thickness tears of the rotator cuff] [in Turkish] Acta Orthop Traumatol Turc. 2005;39:114–120. [PubMed] [Google Scholar]
- 26.Riley GP, Harrall RL, Constant CR, Chard MD, Cawston TE, Hazleman BL. Tendon degeneration and chronic shoulder pain: changes in the collagen composition of the human rotator cuff tendons in rotator cuff tendinitis. Ann Rheum Dis. 1994;53:359–366. doi: 10.1136/ard.53.6.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sano H, Mineta M, Kita A, Itoi E. Tendon patch grafting using the long head of the biceps for irreparable massive rotator cuff tears. J Orthop Sci. 2010;15:310–316. doi: 10.1007/s00776-010-1453-5. [DOI] [PubMed] [Google Scholar]
- 28.Shen PH, Lien SB, Shen HC, Lee CH, Wu SS, Lin LC. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg. 2008;17(1 suppl):1S–7S. doi: 10.1016/j.jse.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 29.Shinoda T, Shibata Y, Izaki T, Shitama T, Naito M. A comparative study of surgical invasion in arthroscopic and open rotator cuff repair. J Shoulder Elbow Surg. 2009;18:596–599. doi: 10.1016/j.jse.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007;89:953–960. doi: 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 31.Toyoda H, Ito Y, Tomo H, Nakao Y, Koike T, Takaoka K. Evaluation of rotator cuff tears with magnetic resonance arthrography. Clin Orthop Relat Res. 2005;439:109–115. doi: 10.1097/01.blo.0000176142.01262.35. [DOI] [PubMed] [Google Scholar]
- 32.Trenerry K, Walton JR, Murrell GA. Prevention of shoulder stiffness after rotator cuff repair. Clin Orthop Relat Res. 2005;430:94–99. doi: 10.1097/01.blo.0000137564.27841.27. [DOI] [PubMed] [Google Scholar]
- 33.Uchiyama Y, Hamada K, Khruekarnchana P, Handa A, Nakajima T, Shimpuku E, Fukuda H. Surgical treatment of confirmed intratendinous rotator cuff tears: retrospective analysis after an average of eight years of follow-up. J Shoulder Elbow Surg. 2010;19:837–846. doi: 10.1016/j.jse.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 34.Verma NN, Dunn W, Adler RS, Cordasco FA, Allen A, MacGillivray J, Craig E, Warren RF, Altchek DW. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy. 2006;22:587–594. doi: 10.1016/j.arthro.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 35.Wilson F, Hinov V, Adams G. Arthroscopic repair of full-thickness tears of the rotator cuff: 2- to 14-year follow-up. Arthroscopy. 2002;18:136–144. doi: 10.1053/jars.2002.30443. [DOI] [PubMed] [Google Scholar]
- 36.Wolf EM, Pennington WT, Agrawal V. Arthroscopic rotator cuff repair: 4- to 10-year results. Arthroscopy. 2004;20:5–12. doi: 10.1016/j.arthro.2003.11.001. [DOI] [PubMed] [Google Scholar]