Abstract
This paper reports language ability and everyday functioning of 133 children with hearing impairment who were evaluated at 3 years of age, as part of the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study. The language abilities of children were evaluated using the Preschool Language Scale (PLS-4), Peabody Picture Vocabulary Test (PPVT), Diagnostic Evaluation of Articulation and Phonology (DEAP) and Child Development Inventory (CDI). Everyday functioning of children was evaluated by interviewing parents using the Parents’ Evaluation of Aural/oral performance of Children (PEACH) questionnaire. There were significant correlations among language measures, and also between the standardized language measures and the PEACH. On average, children who had language deficits exhibited difficulties in everyday functioning. The evidence lends support to a systematic use of parents’ observations to evaluate communicative functioning of children in real life. On average, children’s language attainment decreased as hearing loss increased, more so for children of less highly educated parents. Factors that were not significantly associated with speech and language outcomes at 3 years were age of amplification and socioeconomic status. As multiple factors affect children’s outcomes, it will be possible to examine their effects on outcomes of children when all data in the LOCHI study are available.
Keywords: Children, hearing impairment, language development
Introduction
About one to two children in every thousand born in Australia are fitted with hearing aids or receive cochlear implants for a permanent hearing loss before the age of 4 years (Ching, Oong, & van Wanrooy, 2007). Permanent childhood hearing loss has major developmental impacts on children’s literacy, psychosocial functioning and academic achievement (Davis et al., 1997; Helfand et al., 2001; Joint Committee on Infant Hearing, 2000). With the advent of portable, reliable hearing screening technologies, there is now good evidence that newborn hearing screening testing is highly accurate (Kennedy, McCann, Campbell, Kimm, & Thornton, 2005) and leads to early identification and treatment of infants with hearing loss (Wessex Universal Neonatal Hearing Screening Trial Group, 1998). Early intervention for childhood hearing loss is expected to improve language outcomes of children. This expectation, supported by several program-based studies in the late-1990s on retrospective associations between early diagnosis at age 6–9 months and better language at 2–5 years (Yoshinaga-Itano, Sedey, Coulter, & Mehl, 1998; Moeller, 2000), provided a driving force for systematic attempts to achieve universal newborn hearing screening (UNHS).
Despite the large-scale adoption of UNHS across the world, including Australia, serious evidence gaps remain. The US Preventive Services Task Force (USPSTF) conducted a systematic review of evidence in 2001 and reported (Helfand et al., 2001) that “evidence to determine whether earlier treatment resulting from screening leads to clinically important improvement in speech and language … is inconclusive because of the design limitations in existing studies”. In a subsequent updated review by the USPSTF (Nelson, Bougatsos, & Nygren, 2008), two additional studies were identified. One retrospective cohort study in the United Kingdom (UK) (Kennedy et al., 2006) evaluated the effect of UNHS on speech and language outcomes of 120 children born between 1992 and 1997 who underwent assessment at school age (mean 7.9 yrs, range: 5.4–11.7 years). The report indicated that children who were exposed to UNHS and who received intervention before 9 months of age had better scores than those who did not on receptive language, but not on expressive language or speech production. As the UNHS trial in the UK commenced before the vastly improved technology and services brought about by the Audiology Modernisation Project (Department of Health, 2004), the outcomes for those exposed or not exposed to UNHS may be differentially affected by the improvements though it is not clear in which direction. Another retrospective cohort study (Wake, Hughes, Poulakis, Collins, & Rickards, 2004), carried out in Australia, reported speech and language assessments of 89 children at 7–8 years of age residing in Victoria who were fitted with hearing aids by age 4.5 years. However, the study lacked statistical power to evaluate an effect of age of intervention because only 11 children in the cohort received intervention before 6 months of age. Two other systematic reviews were conducted. A Cochrane review (Puig, Municio, & Meda, 2005) comparing the long-term effectiveness of UNHS and early treatment failed to identify any randomized, controlled trial that fulfilled inclusion criteria. A subsequent systematic review in 2009 (Wolff, Hommerich, Riemsma, Antes, Lange, & Kleijnen, 2009) reported a lack of high-quality evidence regarding all elements of newborn hearing screening. Therefore, the fundamental question remains unanswered—whether, on a population basis, UNHS is effective in achieving its aims of better outcomes for children with permanent childhood hearing loss.
To address the long-term effectiveness of UNHS, it was necessary to conduct a prospective longitudinal study that directly compares outcomes of early and later-identified children. A combination of factors made the Australian environment uniquely well suited to this research. The presence of UNHS only in some regions enabled the effects of early detection and intervention to be examined in an ethical and controlled manner. The existence of a national service provider of audiological management of all children with hearing loss, Australian Hearing, enabled the study population to be truly representative of the general population of children with hearing impairment, ensured that uniform and consistent national protocols for intervention were implemented for all children, and contributed to minimizing loss to follow-up that would otherwise affect a longitudinal study. As the research arm of Australian Hearing, the National Acoustic Laboratories took advantage of this research environment and commenced the population study in 2005 to directly compare outcomes of early- and later-identified children over the first 5 years of life in a prospective manner (Ching, Dillon, Day, & Crowe, 2008a). The Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study is a population-based study that includes a cohort of children born in three Australian states, New South Wales (NSW), Victoria (VIC) and Queensland (QLD). Four hundred and seventy-five children are currently enrolled in the study. The children are evaluated at 6 and 12 months after initial intervention, and again at 3 and 5 years of age. The youngest child will complete evaluations at age 5 years in 2012. The present paper reports on the cross-sectional data of 133 children in the LOCHI study who were born between December 2002 and December 2006, and who had turned 3 years of age at the time of assessment.
This paper has three goals. The first was to report a comprehensive range of language outcomes for a contemporary cohort of 3-year-old children with congenital hearing loss across the spectrum of severity. The second goal was to examine the relationship between standardized measures in structured administrations and everyday functioning of children in different situations. There is some evidence to suggest that a child’s performance with amplification in different environments with different people provides a more realistic picture of the child’s ability than tests in a structured setting (Vidas, Hassan, & Parnes, 1992). It is not known to what extent the language ability assessed in a structured setting reflects the ability of children to function in everyday life. The third goal was to examine factors that affect language development of children with hearing loss at age 3 years, drawing from whole geographical populations rather than samples from specific early intervention programs to avoid potential biases.
As it has been reported in the literature on language development of children with normal hearing that better language was associated with higher maternal education (Dollaghan et al., 1999; Feldman et al., 2005) and socio-economic status (Horton-Ikard & Weismer, 2007; Walker, Greenwood, Hart, & Carta, 1994), we hypothesized that these same factors would influence children with hearing loss. In addition, previous reports on children with hearing loss indicated that severity of hearing loss affected language development of later-identified children at 8 years of age (Wake et al., 2004), but earlier age of intervention was associated with better language development at 3 years of age for children who attended specific intervention programs (e.g., Moeller, 2000; Yoshinaga-Itano et al., 1998). We hypothesized that severity of hearing loss would have similar developmental impacts on children at 3 years of age, irrespective of whether they received early or later intervention.
In brief, we report language ability of children with hearing impairment as measured by standardized tests, the relationship between standardized test scores and everyday life functioning based on parents’ observations, and factors that affect language development of children with hearing impairment when evaluated at 3 years of age.
Method
Participants
The participants were 133 children who were born between December 2002 and December 2006 in three states of Australia (NSW, VIC, and QLD), and who had turned 3 years of age at the time of testing. Characteristics of participants and their families are given in Table I. All children had bilateral hearing loss ranging from mild to profound degrees (averaged over 500 to 2000 Hz), and were fit with digital nonlinear hearing aids in both ears. Forty-five percent of children received their first hearing aids before 6 months of age; the remaining children received amplification between 6 and 34 months of age. The age of amplification was retrieved from the database of the national hearing service provider. All children used hearing aids for 4 or more hours a day, as reported by parents. The children received habilitation services from different programs, ranging from auditory-verbal, aural-oral, aural with sign support, and bilingual programs.
Table I.
Characteristics of participants and their families, separately for children who first received hearing aids before 6 months of age (< 6 m) and those at or after 6 months of age (≥ 6 m).
| Number (%) of participants |
||
|---|---|---|
| Characteristics | <6 m (n=60) |
≥ 6 m (n=73) |
| Gender (Female) | 25 (41.7) | 29 (39.7) |
| Degree of hearing loss (averaged hearing thresholds between 500 and 2000 Hz) | ||
| Mild | 9 (15.0) | 18 (24.7) |
| Moderate | 32 (53.3) | 38 (52.1) |
| Severe | 19 (16.7) | 13 (17.8) |
| Profound | 0 (0) | 4 (.1) |
| Maternal education – no. (%) | ||
| University qualification | 20 (33.3) | 27 (37.0) |
| Diploma or certificate | 24 (40.0) | 25 (34.2) |
| 7–12 years school attendance | 16 (26.7) | 19 (26.0) |
| ≤ 6 years school attendance | 0 (0) | 2 (2.7) |
| Socio-economic status – no. (%) | ||
| IRSAD <8 | 25 (41.7) | 27 (37.0) |
| IRSAD ≥8 | 35 (58.3) | 46 (63.0) |
Key: Index of Relative Socioeconomic Advantage and Disadvantage (IRSAD).
Assessment
Each child was assessed individually using the Preschool Language Scale version 4 (PLS-4, Zimmerman, Steiner, & Pond, 2002), the Peabody Picture Vocabulary Test version 4 (PPVT-4, Dunn & Dunn, 2007) and the Diagnostic Evaluation of Articulation and Phonology (DEAP, Dodd et al., 2002). All assessments were directly administered by qualified speech-language pathologists. Parents were requested to complete the Child Development Inventory (CDI, Ireton, 2005) and the Parents’ Evaluation of Aural/oral performance of Children (PEACH, Ching & Hill, 2007).
The Preschool Language Scale (Zimmerman et al., 2002) is a norm-referenced test of receptive and expressive language ability for ages birth to 6 years 11 months. Australian language adaptations were used according to the instructions in the Examiner’s manual. The test consists of a picture book and manipulative toys designed to engage a child in order to elicit responses to tests items. The test gives two core subscales, Auditory Comprehension (AC) and Expressive Communication (EC), and a Total score. Standard scores have a mean of 100 and a standard deviation of 15.
The Peabody Picture Vocabulary Test-4 (Dunn & Dunn, 2007) is a widely used norm-referenced test of receptive vocabulary for ages 2.5 to 90+ years. The test consists of an easel with colourful pictures for eliciting responses from children. During a test, children were required to point to one of 4 pictures that represented the word produced by the tester. Standard scores have a mean of 100 and a standard deviation of 15.
The Diagnostic Evaluation of Articulation and Phonology (DEAP) (Dodd, Zhu, Crosbie, Holm, & Ozanne, 2002) is suitable for children between 3 years and 6 years 11 months. The Phonology Assessment subtest was used to assess production of vowels and consonants, and production errors were analysed in terms of phonological processes. The test consists of a book of 50 pictures to elicit single word items and 2 pictures for eliciting connected speech. The children’s productions were phonemically transcribed according to the International Phonetic Alphabet (International Phonetic Association, 1984). The transcriptions were entered into the Computed Assisted Speech and Language Assessment (CASALA v.4.0, University of Melbourne, 2007) software for deriving proportion of correct vowel and consonant productions. Australian norms on the DEAP test are available. Standard scores have a mean of 10 and a standard deviation of 3.
The Child Development Inventory (CDI) (Ireton, 2005) is a parent questionnaire designed to help assess and identify children with developmental problems for ages 15 months to 6 years. The 270 items in the test are grouped to form scales including Social, Self Help, Gross Motor, Fine Motor, Expressive Language, Language Comprehension, Letters, Numbers, and General Development. The Expressive Language and the Language Comprehension subscale scores are reported here. Language quotients were calculated by taking the ratio of the equivalent language age based on items reported by parents to the chronological age of the child. A language quotient of 100 denotes normal, age-appropriate development. A quotient of less than 80 denotes developmental problems.
The Parents’ Evaluation of Aural/oral performance of Children (PEACH) (Ching & Hill, 2007) is an interview-administered parent questionnaire for assessing children’s functional performance in different situations in everyday life, based on parents’ observations. Unlike other functional performance tools that were developed for assessing low levels of auditory function for children with profound hearing loss (e.g., Meaningful Auditory Integration Scale, Robbins, Renshaw, & Berry, 1991; Harrison, 2000), the PEACH scale is applicable for assessing children with hearing loss ranging from mild to profound degrees whose age ranges from 4 weeks to 18 years (for a review of functional performance tools for children, see Ching & Hill, 2007). Previous reports have indicated that the PEACH was a reliable measure for evaluating the effectiveness of amplification for children in real life (Ching, Hill, & Dillon, 2008b). Using the normative data and critical differences for the PEACH (Ching & Hill, 2007), performance of children with hearing loss can be related to their peers with normal hearing. In this paper, children’s performance is expressed in terms of deviation from age-appropriate means.
Demographic information was solicited from parents/primary carers and habilitationists by the use of a study-designed questionnaire. Socio-economic status was quantified in terms of the Index of Relative Socioeconomic Advantage and Disadvantage (IRSAD). This Index, developed by the Australian Bureau of Statistics (ABS), is one of four different indices that make up the Socio Economic Index for Area (SEIFA, ABS, 2008). Postcode data were used to give an indication of the economic and social resources of people and households within an area, based on 21 variables extracted from the Australian Bureau of Statistics (ABS) 2006 census data. A lower Index is associated with greater relative disadvantage. The Australian Bureau of Statistics recommended the use of the IRSAD to examine aspects of health where it is anticipated that disadvantaged people have worse outcomes compared to more advantaged people (ABS, 2008). Maternal education was specified in terms of a 4-point scale, in line with the ABS specifications. The categories ranged from less than or equal to 6 years of school attendance, 7 to 12 years of school attendance, diploma or certificate, and university qualification. Audiological information and age at hearing aid fitting were retrieved with parental consent from children’s files held at Australian Hearing.
Results
Language and phonological development
Table II gives the mean scores of children for different tests. The number of children who completed each test varied due to availability, attention span and other practical constraints. Statistical analyses were based on all eligible children. Analyses of variance (ANOVA) were conducted to investigate the effect of age of intervention on children’s language outcomes. Age of intervention refers to age of hearing aid fitting since age of hearing aid fitting and age of enrolment in a habilitation program were highly correlated (r = .83, p < .001), and age of hearing aid fitting was accurately retrieved from the database of Australian Hearing whereas age of enrolment in a program was based on parental report. Within-subject effects were adjusted by using the Greenhouse-Geisser epsilon correction (Greenhouse & Geisser, 1959; Statistica 7.1, StatSoft Inc. 2005). Where significant interaction effects were found, post-hoc analyses were carried out by using the Bonferroni procedure with adjusted significance level for multiple tests. Spearman rank order correlations were performed to examine the relationship among performance and preference measures, and multi-linear forward stepwise regression analyses were used to determine the factors affecting performance.
Table II.
Mean, standard deviation and range of performance.
| CDI-LCQ | CDI-ELQ | DEAP-PCS | DEAP-PVS | PEACH | PLS-AC | PLS-EC | PPVT | |
|---|---|---|---|---|---|---|---|---|
| Mean | 72.1 | 77.1 | 6.3 | 6.6 | −23.5 | 78.75 | 84.3 | 86.56 |
| n | 101 | 101 | 67 | 67 | 61 | 113 | 113 | 84 |
| Standard deviation |
29.1 | 33.5 | 2.6 | 2.1 | 22.5 | 24.6 | 19.8 | 19.3 |
| Range | .0 to 178.4 | .0 to 194.6 | 3.0 to 11.0 | 3.0 to 10.0 | −74.7 to 7.3 | 50.0 to 129.0 | 50.0 to 130.0 | 23.0 to 118.0 |
Key: Child Development Inventory – Language Comprehension Quotient (CDI-LCQ) and Expressive Language quotient (CDI-ELQ); Diagnostic Evaluation of Articulation and Phonology – consonant standard scores (DEAP-PCS) and vowel standard scores (DEAP-PVS); Parents’ Evaluation of Aural/oral performance of children (PEACH); Preschool Language Scale-Auditory Comprehension (PLS-AC) and Expressive Communication subscales (PLS-EC), Peabody Picture Vocabulary Test version 4 (PPVT).
On average, receptive vocabulary as measured by the PPVT indicated that children were just within 1 SD of the normative mean. On the other hand, the PLS-4 Auditory Comprehension (AC) and Expressive Communication (EC) standard scores were at or below 1 SD of the normative mean. Also, the language quotients of the CDI and the age-corrected PEACH scores suggest that children were below the normal range. In terms of speech production, children’s consonant and vowel scores were below 1 SD of the normative mean. Error patterns revealed in the transcriptions of children’s productions were analysed and phonological processes were identified. The error patterns were typical of children’s speech during normal development (McLeod, 2009; McIntosh & Dodd, 2008). The most dominant processes demonstrated by more than 70% of children included cluster reduction, stopping and gliding. Other processes that occurred for about 30% of children included fronting of velars, weak syllable deletion and final consonant deletion.
Relationship between standardized language measures and everyday life functioning
To examine the relationship among different measures, Spearman rank order correlation was performed (see Table III).
Table III.
Correlation coefficients among different outcomes measures, age at fitting in months (monfit) and three-frequency average hearing loss (3FAHL).
| Monfit | 3FA HL | PLS-AC | PLS-EC | PPVT | DEAP-PCS | DEAP-PVS | CDI-ELQ | CDI-LCQ | PEACH | |
|---|---|---|---|---|---|---|---|---|---|---|
| Monfit | – | .03 | .07 | −.04 | .04 | .15 | −.04 | −.01 | −.11 | .03 |
| 3FA HL | – | −.35** | −.42** | −.17 | −.20 | −.23 | −.32** | −.33** | −.18 | |
| PLS-AC | – | .89** | .81** | .48** | .47** | .71** | .75** | .57** | ||
| PLS-EC | – | .80** | .52** | .51** | .78** | .82** | .60** | |||
| PPVT | – | .45** | .46** | .49** | .57** | .41** | ||||
| DEAP-PCS | – | .73** | .60** | .38** | .18 | |||||
| DEAP-PVS | – | .56** | .43** | .21 | ||||||
| CDI-ELQ | – | .90** | .45** | |||||||
| CDI-LCQ | – | .62** | ||||||||
| PEACH | – |
Significant relations at p < .05 are shown by single asterisks,
and those at p < .01 are shown by double asterisks.
Key: Preschool Language Scale-Auditory Comprehension (PLS-AC) and Expressive Communication subscales (PLS-EC); Peabody Picture Vocabulary Test version 4 (PPVT); Diagnostic Evaluation of Articulation and Phonology – consonant standard scores (DEAP-PCS) and vowel standard scores (DEAP-PVS); Child Development Inventory – Expressive Language quotient (CDI-ELQ) and Language Comprehension Quotient (CDI-LCQ); Parents’ Evaluation of Aural/oral performance of children (PEACH).
The severity of hearing loss was significantly negatively related to language development (PLS-4 standard scores and CDI quotients) indicating that better hearing was associated with better speech and language development.
The expressive and receptive language abilities as measured by the PLS-4 were significantly positively correlated with other language measures, including receptive vocabulary (PPVT), vowel and consonant production (DEAP), and also parent report measures of language comprehension and expressive communication (CDI). These data provide new evidence on the concurrent validity of the assessments for children with hearing impairment measured at age 3 years.
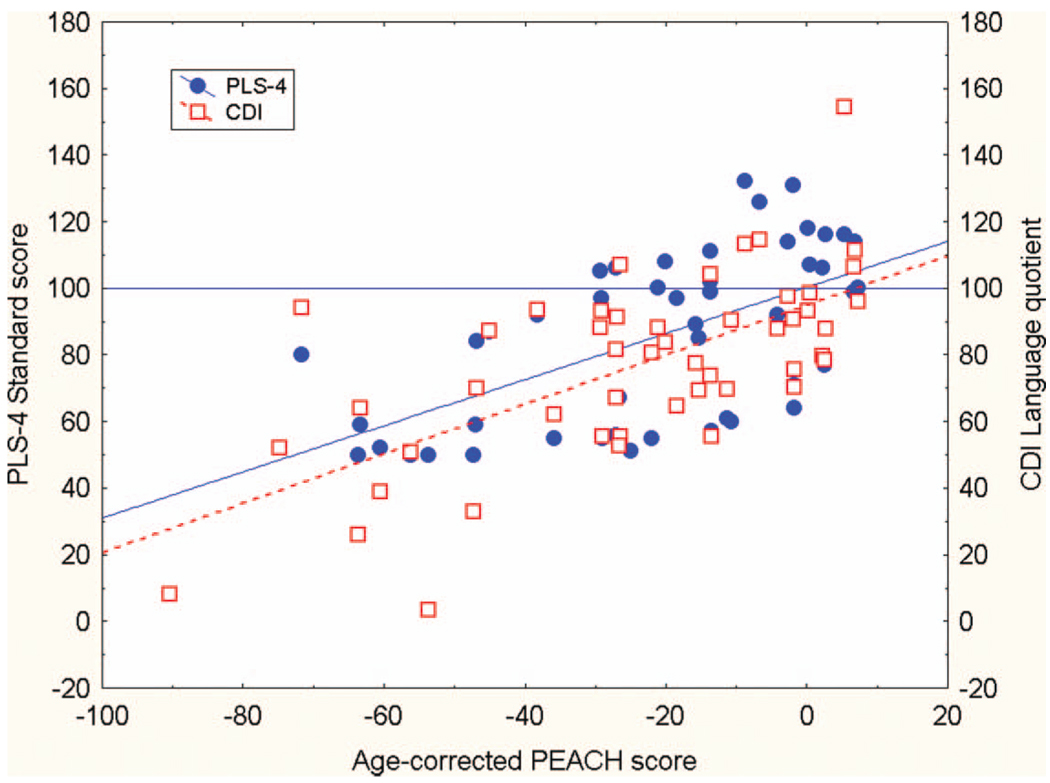
There were significant correlations between children’s everyday life functioning as observed by parents (PEACH scores) and language ability measured either by direct child assessment using the PLS-4 or by parental report based on the CDI. Figure 1 shows the relationship between PEACH scores (corrected for age) and PLS-4 standard scores (Total score) as well as CDI language quotients. The linear regression lines indicate that PEACH scores increased with increase in PLS-4 scores (solid line); and increase in CDI language quotients (broken line). The data suggest that children whose everyday functioning scores (PEACH) were within 1 SD of the normative mean also achieved language performance within 1 SD of the normative mean.
Figure 1.
Relation of age-corrected Parents’ Evaluation of Aural/oral performance of children (PEACH) score and Preschool Language Scale (PLS-4) Total Language standard score (left y-axis, solid regression line) and Child Development Inventory (CDI) Mean Language quotient (right y-axis, broken regression line). Filled circles depict PLS-4 scores and open squares depict CDI language quotients.
The present data demonstrate that children who had deficits in language ability experienced difficulties in everyday functioning in different situations (denoted by negative age-corrected PEACH scores). As the PLS-4 was designed to assess a child’s receptive and expressive language through tasks that focus on applied language skills related to comprehending language and communicating ideas (Preschool Language Scale, Examiners manual, 2002), the significant correlation with the PEACH provides evidence on convergent validity (Murphy & Davidshofer, 1988) of related constructs (language skills) being measured in structured (test environment) and unstructured settings (everyday use). These results lend support to the use of the PEACH to evaluate young children’s aural/oral communicative functioning in everyday life. The PEACH measure is useful not only because it reflects a child’s real-life functioning compared to his normal-hearing peers, but also because it can be used for evaluating children of non-English speaking background or children whose primary mode of communication is not spoken English.
Factors affecting language development at 3 years of age
To investigate the effect of age of amplification on language performance after allowing for the effect of severity of hearing loss, analyses of variance were conducted with the PLS-4 AC and EC subscale scores as repeated measures, age of intervention (< 6 months vs. ≥ 6 months) as a categorical factor, and three-frequency average hearing loss as a continuous covariate. The analyses revealed that the main effect of age of intervention was not significant (F[1,111] = .02, p = .8). Analyses of variance were carried out with PPVT scores, DEAP scores, and CDI language quotients separately, all showing that age of intervention was not significant (p = .8; p = .7; and p = .5 respectively).
To examine the effects of socio-economic status, maternal education and severity of hearing loss on language performance, stepwise forward regression analyses were carried out with PLS-4 total language scores as dependent variables, maternal education (≤12 years vs. > 12 years), socio-economic status (IRSAD < 6 vs. ≥6), severity of hearing loss (continuous factor: 3FA HL), and age of intervention (< 6 months vs. ≥ 6 months) as independent variables. After accounting for the effect of severity of hearing loss (Beta = −.43, p < .0001), maternal education was significant (Beta = −.22, p = .005). No other factors contributed significantly to language scores. On average, children in families with maternal education exceeding 12 years attained language skills within the lower edge of normal limits, whereas those in families with maternal education less than 12 years had language skills below 2SD of the normative mean. The same finding applies to all children, on average, irrespective of whether children first received hearing aids before or after 6 months of age.
Caveat
The present report shows performance of children evaluated at age 3 years. A limitation is that not all children completed tests. Nevertheless, the ANOVA on PLS-4 outcomes for children who received early versus later amplification had at least 53 children in each group, which permitted detection of an effect size of .3 within-group standard deviation with a power of 80%, for an alpha level of .05. In the multilinear regression of PLS-4 scores with 4 predictor variables, a very high ratio of data points to coefficients (28:1) was maintained.
The present analyses suggest that age of intervention was not a significant factor affecting language outcomes as measured by the PLS-4, after allowing for the effect of severity of hearing loss and maternal education. Multiple factors are potentially important in affecting performance, including the likelihood that more of the children who received intervention after 6 months of age had acquired or progressive hearing loss, and thus had access to speech during their first 6 months of life. Moreover socio-economic status assessed at an individual level rather than based on postal codes may have a significant effect on outcomes. When all information solicited via the custom-designed demographic questionnaire and all outcomes data from the LOCHI study become available, it will be possible to account for the effects of these factors to further investigate the effect of age of intervention on long-term speech, language and educational attainment as well as the rate of development of children with hearing loss. Furthermore, preliminary data at age 5 years for a small subgroup of children are already indicating that age of intervention has an effect on language acquisition. Also, data on children with cochlear implants reported separately (Ching et al., 2009) support the importance of early implantation on language development. When all data on the LOCHI study are available, it will be possible to investigate whether different risk and protective factors apply at different ages (cf. Harrison & McLeod, 2009; Reilly et al., 2009) for children with hearing impairment who use different hearing technology.
Summary and discussion
This report shows the impact of hearing loss on language development and everyday functioning of children at 3 years of age. On average, children who received intervention before 6 months of age attained language levels below 1 SD of the normative mean on several standardized measures. Despite access to early detection and early intervention, the preliminary findings suggest that children experienced disadvantages in language development and everyday functioning at a young age.
The significant relationship between everyday functioning of children based on a systematic use of parental observations (PEACH) and the standardized language measures lends support to the validity of the PEACH in assessing children’s development of aural-oral communicative functioning in real life.
For children at 3 years of age, the degree of hearing loss and the level of maternal education appeared to be important factors affecting children’s development. Maternal education may be a nonspecific factor that encompasses multiple facets. For example, more highly educated parents might engage in reading activities with their children more often than less highly educated parents, and children in families of more highly educated parents might demonstrate greater interest in reading processes than their peers (Bracken & Fischel, 2008; Bornstein & Bradley, 2003). However, this study did not assess the reading activities of parents or whether parents of higher SES engaged more in reading activities with their children, independent of the severity of hearing loss of the children. Our future attempts to identify significant factors will investigate the effects of the history of language impairment in a family, reading activities in a family, parental involvement in intervention as rated by early intervention teachers, amount and type of intervention, in addition to other predictor variables, on development of language of children with hearing impairment. We have not included type of communication mode in intervention (e.g., auditory-verbal, oral, oral with sign support or bilingual) in the current analysis because it cannot be inferred whether the mode determines the effectiveness of amplification or whether the efficacy of the device has determined the mode of communication that is possible. For this reason, we will defer investigation of the influence of intervention type on outcomes of children until we obtain data not only on the communication mode in current intervention but also the changes, if any, of intervention types over the first 5 years of life.
Whereas previous program-based studies conducted in the USA suggest apparent benefits at age 3 years for children who received intervention before 6 months of age (Moeller, 2000; Yoshinaga-Itano et al., 1998), the present population-based study does not reveal a significant effect of age of intervention on language development of children with hearing aids. On average, all children exhibited deficits in language acquisition at 3 years of age. When all data become available, it will be possible to investigate multiple factors, including age of intervention, on development of children not only at an early age but also when they enter and progress through the school system. Currently, we know very little about why, for a certain severity of hearing loss, some children do well and some poorly; and some develop at a normal rate whereas others do not. These questions will be addressed in future investigations.
Acknowledgments
We gratefully thank all the children and their families for participating in this study. The data were reported at the Speech Pathology Australia Conference of the Speech Pathology Association in Adelaide, May, 2009. We sincerely thank the reviewers for their comments and suggestions on an earlier version of the manuscript. The HEARing CRC collaborating agencies include Catholic Centre for Hearing Impaired Children, Cochlear Implant Clinic of the Royal Victorian Eye and Ear Hospital, Hear and Say Centre, Matilda Rose Early Intervention Centre, Royal Institute for Deaf and Blind Children, St Gabriel’s School for Hearing Impaired Children, The Shepherd Centre and Sydney Cochlear Implant Centre. This study is supported by the National Institutes of Health Grant no. R01DC008080, Office of Hearing Services, Department of Health in Australia, Australian Hearing, New South Wales Department of Health and Oticon Foundation.
References
- Australian Bureau of Statistics. 2030.0 – Information Paper: An Introduction to Socio-economic Indexes for Areas (SEIFA) 2008 Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2039.02006?Open Document.
- Bornstein MH, Bradley RH. Socioeconomic status, parenting, and child development. Monographs in Parenting. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Bracken SS, Fischel JE. Family reading behaviour and early literacy skills in preschool children from low-income backgrounds. Early Education and Development. 2008;19:45–67. [Google Scholar]
- Ching TYC, Hill M. The Parents’ Evaluation of Aural/oral performance of Children (PEACH) scale: Normative data. Journal of American Academy of Audiology. 2007;18:221–237. doi: 10.3766/jaaa.18.3.4. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Oong R, van Wanrooy E. The ages of intervention in regions with and without UNHS and the prevalence of childhood hearing impairment in Australia. Australian and New Zealand Journal of Audiology. 2007;28:137–150. [Google Scholar]
- Ching TYC, Dillon H, Day J, Crowe K. The NAL study on longitudinal outcomes of hearing-impaired children: Interim findings on language of early and later-identified children at 6 months after hearing aid fitting. In: Seewald R, Bamford J, editors. A sound foundation through early amplification 2007, Proceedings of the Fourth International Conference; Switzerland: Phonak AG; 2008a. pp. 185–199. [Google Scholar]
- Ching TYC, Hill M, Dillon H. Effect of variations in hearing-aid frequency response on real-life functional performance of children with severe or profound hearing loss. International Journal of Audiology. 2008b;47:461–475. doi: 10.1080/14992020802116128. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Dillon H, Day J, Crowe K, Close L, Chisholm K, Hopkins T. Early language outcomes of children with cochlear implants: Interim findings of the NAL study on longitudinal outcomes of children with hearing impairment. Cochlear Implant International. 2009;10 Suppl.1:28–32. doi: 10.1002/cii.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S. A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment. Health Technology Assessment. 1997;1(10):i–iv. [PubMed] [Google Scholar]
- Department of Health. Department Report 2004. London: Department of Health; 2004. [Google Scholar]
- Dodd B, Zhu H, Crosbie S, Holm A, Ozanne A. Diagnostic Evaluation of Articulation and Phonology. London: Harcourt; 2002. [Google Scholar]
- Dollaghan CA, Campbell TF, Paradise JL, Feldman HM, Janosky JE, Pitcairn DN, Kurs-Lasky M. Maternal education and measures of early speech and language. Journal of Speech, Language, and Hearing Research. 1999;43:1432–1443. doi: 10.1044/jslhr.4206.1432. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn DM. Peabody Picture Vocabulary Test. 4th ed. Circle Pines, MN: American Guidance Service; 2007. [Google Scholar]
- Feldman HM, Campbell TF, Kurs-Lasky M, Rockette HE, Dale PS, Colborn DK, Paradise JL. Concurrent and predictive validity of parent reports of child language at ages 2 and 3 years. Child Development. 2005;76:856–868. doi: 10.1111/j.1467-8624.2005.00882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhouse SW, Geisser S. On methods in the analysis of profile data. Psychometrika. 1959;24:95–112. [Google Scholar]
- Harrison M. How do we know we’ve got it right? Observing performance with amplification. In: Seewald R, editor. A sound foundation through early amplification: Proceedings of an international conference; Switzerland: Phonak AG; 2000. [Google Scholar]
- Harrison LJ, McLeod S. Risk and protective factors associated with speech and language impairment in a nationally representative sample of 4- to 5-year-old children. Journal of Speech, Language, and Hearing Research. 2009 doi: 10.1044/1092-4388(2009/08-0086). published online 28 Sept 2009, doi: 10.1044/1092-4388(2009/08-0086). [DOI] [PubMed] [Google Scholar]
- Helfand M, Thompson DC, Davis RL, McPhillips H, Homer CJ, Lieu TL. Newborn hearing screening: Systematic evidence review. Rockville, MD: Agency for Healthcare Research and Quality; 2001. AHRQ publication 02-S001. Retrieved July 2007, from www.ahrq.gov/clinic/serfiles.htm. [PubMed] [Google Scholar]
- Horton-Ikard R, Weismar SE. A preliminary examination of vocabulary and word learning in African American toddlers from middle and low socioeconomic status homes. American Journal of Speech-Language Pathology. 2007;16:381–392. doi: 10.1044/1058-0360(2007/041). [DOI] [PubMed] [Google Scholar]
- International Phonetic Association. The principles of the International Phonetic Association. London: International Phonetic Association; 1984. [Google Scholar]
- Ireton H. Child Development Inventory. Minnesota: Child Development Review; 2005. [Google Scholar]
- Joint Committee on Infant Hearing (American Academy of Audiology, American Academy of Pediatrics, American Speech-Language-Hearing Association, Directors of Speech and Hearing Programs in State Health and Welfare Agencies) Year 2000 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2000;106:798–817. doi: 10.1542/peds.106.4.798. [DOI] [PubMed] [Google Scholar]
- Kennedy CR, McCann D, Campbell MJ, Kimm L, Thornton R. Universal newborn hearing screening for permanent childhood hearing impairment: An 8-year follow-up of a controlled trial. Lancet. 2005;366(9486):660–662. doi: 10.1016/S0140-6736(05)67138-3. [DOI] [PubMed] [Google Scholar]
- Kennedy CR, McCann DC, Campbell MJ, Law CM, Mullee M, Petrou S, et al. Language ability after early detection of permanent childhood hearing impairment. New England Journal of Medicine. 2006;354:2131–2141. doi: 10.1056/NEJMoa054915. [DOI] [PubMed] [Google Scholar]
- McIntosh B, Dodd B. Two-year-olds’ phonological acquisition: Normative data. International Journal of Speech-Language Pathology. 2008;10:460–469. doi: 10.1080/17549500802149683. [DOI] [PubMed] [Google Scholar]
- McLeod S. Speech sound acquisition. In: Bernthal JE, Bankson NW, Flipsen P Jnr, editors. Articulation and phonological disorders: Speech sound disorders in children. 6th ed. Boston, MA: Pearson Education; 2009. pp. 63–120.pp. 385–405. [Google Scholar]
- Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3) doi: 10.1542/peds.106.3.e43. Available at: www.pediatrics.org/cgi/content/full/106/3/e43.sos. [DOI] [PubMed] [Google Scholar]
- Murphy KR, Davidshofer CO. Psychological testing: Principles and applications. Englewood Cliffs, NJ: Prentice-Hall International Editions; 1988. [Google Scholar]
- Nelson HD, Bougatsos C, Nygren P. Universal newborn hearing screening: Systematic review to update the 2001 U.S. Preventive Services Task Force Recommendation. Pediatrics. 2008;122:e266–e276. doi: 10.1542/peds.2007-1422. [DOI] [PubMed] [Google Scholar]
- Puig T, Municio A, Meda C. Universal neonatal hearing screening versus selective screening as part of the management of childhood deafness. Cochrane Database Systematic Review. 2005:CD003731. doi: 10.1002/14651858.CD003731.pub2. [DOI] [PubMed] [Google Scholar]
- Reilly S, Bavin EL, Bretherton L, Conway L, Eadie P, Cini E, Prior M, Ukoumunne OC, Wake M. The Early Language in Victoria Study (ELVS): A prospective, longitudinal study of communication skills and expressive vocabulary development at 8, 12 and 24 months. International Journal of Speech-Language Pathology. 2009;11:344–357. [Google Scholar]
- Robbins AM, Renshaw J, Berry S. Evaluating meaningful auditory integration in profoundly hearing-impaired children. American Journal of Otolology. 1991;12 Supp. l:144–150. [PubMed] [Google Scholar]
- Statistica Rel. 7.1. STATISTICA software. USA: StatSoft Inc.; 2005. [Google Scholar]
- Vidas S, Hassan R, Parnes LS. Real-life performance considerations of four pediatric multi-channel cochlear implant recipients. Journal of Otolaryngology. 1992;21:387–393. [PubMed] [Google Scholar]
- Wake M, Hughes EK, Poulakis Z, Collins C, Rickards F. Outcomes of children with mid-profound congenital hearing loss at 7 to 8 years: A population study. Ear and Hearing. 2004;25:1–8. doi: 10.1097/01.AUD.0000111262.12219.2F. [DOI] [PubMed] [Google Scholar]
- Walker D, Greenwood C, Hart B, Carta J. Prediction of school outcomes based on early language production and socioeconomic factors. Child Development. 1994;65:606–621. [PubMed] [Google Scholar]
- Wessex Universal Neonatal Hearing Screening Trial Group. Controlled trial of universal neonatal screening for early identification of permanent childhood hearing impairment. Lancet. 1998;352(9145):1957–1964. [PubMed] [Google Scholar]
- Wolff R, Hommerich J, Riemsma R, Antes G, Lange S, Kleijnen J. Hearing screening in newborns. Systematic review of accuracy, effectiveness, and effects of intervention after screening. Archives of Disorders of Children. 2009 doi: 10.1136/adc.2008.151092. published online 26 Mar 2009, doi:10.136/adc.2008.151092. [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano C, Sedey AL, Coulter D, Mehl. AL. Language of early- and later-identified children with hearing loss. Pediatrics. 1998;102:1161–1171. doi: 10.1542/peds.102.5.1161. [DOI] [PubMed] [Google Scholar]
- Zimmerman I, Steiner V, Pond R. Preschool Language Scale. 4th ed. San Antonio, TX: The Psychological Corporation; 2002. [Google Scholar]