Abstract
Impetigo herpetiformis or gestational pustular psoriasis can account for 4.25% of all pregnancy dermatoses seen. Unlike other pregnancy dermatoses, it can be associated with constitutional symptoms including fever, rigors, arthralgia and complications of secondary infection and sepsis. There is an increased risk of fetal anomalies and stillbirths. A 25-year-old para 1 presented to primary care at 7 weeks gestation with a peri-umbilical rash non-responsive to topical steroids and underwent hospital admission at 31 weeks gestation with fever and a widespread painful erythematous rash. Her condition worsened despite high-dose oral steroids. With the use of cyclosporine and regular opioid analgesia over 2 weeks, her symptoms were adequately controlled. She went into spontaneous labour at 41+2 weeks and delivered a healthy male infant. Impetigo herpetiformis can be treated first line with topical and oral steroids and supportive measures, but immunomodulatory therapies such as cyclosporine have shown success in treating resistant cases.
Background
Impetigo herpetiformis or gestational pustular psoriasis or is a rare non-infectious dermatosis related to pregnancy which normally occurs during the third trimester of pregnancy, but well documented cases have occurred as early as the first trimester.1 Primiparous women are at the highest risk, though severity increases in subsequent pregnancies.2 It presents superficial pustules in an herpetiform distribution.3 The pustular eruption typically starts symmetrically in the axillae or groin flexures, below the breasts or around the umbilicus, sometimes in abdominal striae,4 but can extend to become generalised with desquamation, with mucous membranes being only infrequently affected.5 The condition differs from other pregnancy dermatoses in that it can be associated with constitutional symptoms including fever, rigors, gastrointestinal upset, malaise and arthralgia.6–8 There are less than 200 reported cases9 which means that pathogenesis is not fully understood, though the trigger may be maternal hypocalcaemia which can lead to serious maternal complications of confusion, tetany and death,6 high progesterone levels or an infectious cause.10 Other complications include fluid and electrolyte imbalance and maternal secondary infection and sepsis.5 Fetal concerns include placental insufficiency even when the disease is controlled in the mother and an increased stillbirth risk11 and fetal abnormalities.3 5 8 Lesions are expected to regress after delivery but may reoccur at times of stress and at an earlier gestational age in further pregnancies,2 as a characteristic eruption of erythematosquamous plaques covered with small or confluent
Case presentation
A 25-year-old woman was referred at 31 weeks gestation systemically unwell with a widespread erythematous rash. She initially presented to her general practitioner at 7 weeks gestation with a peri-umbilical rash, which was non-responsive to topical steroid preparations (trimovate, dermovate), causing pain not pruritis.
On admission, she was feverish at over 38°C and tachycardic, with an erythematous rash covering most of the body surface with confluent blisters and desquamation, having severe pain in all areas affected by the rash (figure 1).
Figure 1.
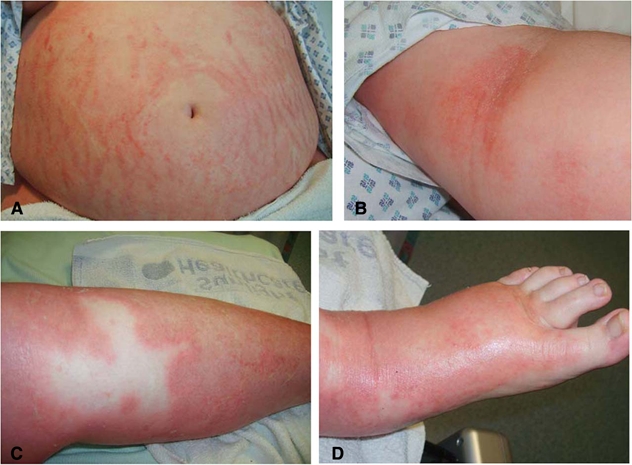
Impetigo herpetiformis occurring over (A) abdomen (B) flexure (C) lower limb and (D) foot.
Her obstetric history was gravida 2 para 1, with a previous uncomplicated pregnancy and normal vaginal delivery of a term 3520 g female infant 6 years previously. Her medical history included mild asthma requiring salbutamol, fluticasone and salmeterol inhalers for control.
Investigations
Initial investigations showed a negative septic screen; blood cultures and swabs from the rash and pustules showed no growth. Her total calcium and albumin were low albumin, with a raised erythrocyte sedimentation rate (ESR) and C reactive protein and neutrophilia, other results were within normal limits. Serum autoantibody screens including antipemphigoid autoantibodies were negative and the skin biopsy was negative for IgM, IgG, IgA, C3 and fibrinogen, supporting a diagnosis of impetigo herpetiformis.10
Treatment
Five days of increasing oral steroid therapy to a maximum of 80 mg prednisolone daily12 failed to control symptoms, so cyclosporine was commenced and the steroid dosage was tapered over the following 14 days. A dose of 200 mg cyclosporine twice daily achieved symptom control after 9 days. During this period the patient had been requiring regular opioid-based analgesia for symptomatic relief.
Outcome and follow-up
She was monitored intensely throughout the remainder of her pregnancy and went into spontaneous labour at 41+2 weeks, rupturing membranes during labour, with a normal vaginal delivery of a 3200 g male infant. He required no resuscitation at birth or special care in the neonatal period and had a normal baby check.
Discussion
Impetigo herpetiformis is a rare condition of unknown aetiology which primarily affects pregnant women, though it can occur in the puerperium or in non-pregnancy women.13 In a 3-year longitudinal study it accounted for 4.25% of all pregnancy dermatoses seen.14 It typically occurs in women with no pre-existing skin conditions or family history of skin disease, but case reports of twin sisters both developing impetigo herpetiformis during pregnancy suggest that it may have a genetic predisposition.15 Triggering factors have been suggested to be hypocalcaemia, hypoparathyroidism,16 hypoalbuminaemia, stress and exposure to bacterial or other infection,17 but with such a low number of cases none have been proven. The formation of blisters may be associated with a relative imbalance of skin elastase and its inhibitors as a result of low levels of skin derived antileucoproteinase.18
The diagnosis remains a primarily clinical diagnosis with support from typical findings of leukocytosis, raised ESR, low calcium and albumin or low parathyroid hormone levels. Typical histology shows parakeratosis, acanthosis, intraepidermal spongiform pustules containing neutrophils and papillary dermal infiltration of lymphocytes and neutrophils.5 16 Immunohistochemistry is negative for C3 and IgG which differentiates it from gestational pemphigus and there is typically no specific serology or autoantibodies noted.19 Swabs from pustules are generally sterile, though they can be complicated by secondary infections, requiring antibiotic therapy.
Impetigo herpetiformis is usually treated successfully with topical or oral steroid preparations, and unresponsive cases may receive cyclosporine,20 though this can be associated with early rupture of membranes with no significant teratogenic effect.10 Supportive management includes correction of fluid and electrolyte imbalances, antibiotic therapy for secondary infections, analgesia for pain and patients require more intensive fetal monitoring and may require earlier delivery.21 These patients may present an anaesthetic challenge if operative delivery is required, particularly if mucosal involvement has occurred.11 There are case reports of other methods which been used in pregnancy in cases resistant to steroids, including narrow band ultraviolet B therapy,22 psoralen ultraviolet A,23 clofazimine24 and the antitumour necrosis factor drug infliximab in a steroid resistant case with good maternal and fetal outcome.25 Methotrexate and oral retinoids remain treatment options only in the postnatal or non-pregnant patient.
Learning points.
-
▶
Impetigo herpetiformis is a rare but important dermatosis of pregnancy, which needs early recognition and prompt treatment to prevent potentially fatal maternal and fetal complications.
-
▶
It presents in a typical fashion in the third trimester with erythematous plaques and sterile blisters and remains a primarily clinical diagnosis/diagnosis of exclusion.
-
▶
It can be treated first line with topical and oral steroids and supportive measures, but immunomodulatory therapies available in dermatology also show success in treating resistant cases.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Gligora M, Kolacio Z. Hormonal treatment of impetigo herpetiformis. Br J Dermatol 1982;107:253. [DOI] [PubMed] [Google Scholar]
- 2.Beveridge GW, Harkness RA, Livingstone JR. Impetigo herpetiformis in two successive pregnancies. Br J Dermatol 1966;78:106–12 [DOI] [PubMed] [Google Scholar]
- 3.Sauer GC, GEHA BJ. Impetigo herpetiformis. Report of a case treated with corticosteroid-review of the literature. Arch Dermatol 1961;83:119–26 [DOI] [PubMed] [Google Scholar]
- 4.Creasy RK, Resnik R, eds. Maternal-fetal Medicine: Principles and Practice. Fifth edition Philadelphia, PA: Elsevier Health Sciences; 2004:1207–8 [Google Scholar]
- 5.Oumeish OY, Parish JL. Impetigo herpetiformis. Clin Dermatol 2006;24:101–4 [DOI] [PubMed] [Google Scholar]
- 6.Freedberg IM, Eisen AZ, Wolff K, et al., eds. Dermatology in General Medicine. Fifth edition New York, NY: McGraw Hill; 1999:1967–8 [Google Scholar]
- 7.Sasseville D, Wilkinson RD, Schnader JY. Dermatoses of pregnancy. Int J Dermatol 1981;20:223–41 [DOI] [PubMed] [Google Scholar]
- 8.Champion RH, Burton JL, Burns DA, eds. Rook’s Textbook of Dermatology. Sixth edition Oxford: Blackwell Scientific Publications; 1998:1639–40 [Google Scholar]
- 9.Nasser N, Sasseville D. Dermatologic diseases of pregnancy. Dermatologie - Conferences Scientifiques 2006;5:1–6 [Google Scholar]
- 10.Roth MM. Pregnancy dermatoses: diagnosis, management, and controversies. Am J Clin Dermatol 2011;12:25–41 [DOI] [PubMed] [Google Scholar]
- 11.Gambling D, Douglas MJ, McKay RSF, eds. Obstetric Anesthesia and Uncommon Disorders. Second edition Cambridge: Cambridge University Press; 2008:349 [Google Scholar]
- 12.Wolf Y, Groutz A, Walman I, et al. Impetigo herpetiformis during pregnancy: case report and review of the literature. Acta Obstet Gynecol Scand 1995;74:229–32 [DOI] [PubMed] [Google Scholar]
- 13.Erdem T, Kerakuzu A, Parlak M, et al. Non gestational impetigo herpetiformis. Tr J of Med Sciences 1999;29:597–9 [Google Scholar]
- 14.Samdani AJ. Pregnancy dermatoses: a three-year study. Pak L Med Sci 2004;20:292–5 [Google Scholar]
- 15.Vicdan K, Gokay Z, Var T, et al. Twin sisters with impetigo herpetiformis. Eur J Obstet Gynecol Reprod Biol 1995;63:195–6 [DOI] [PubMed] [Google Scholar]
- 16.Moynihan GD, Ruppe JP., Jr Impetigo herpetiformis and hypoparathyroidism. Arch Dermatol 1985;121:1330–1 [PubMed] [Google Scholar]
- 17.Sahin HG, Sahin HA, Metin A, et al. Recurrent impetigo herpetiformis in a pregnant adolescent: case report. Eur J Obstet Gynecol Reprod Biol 2002;101:201–3 [DOI] [PubMed] [Google Scholar]
- 18.Kuijpers AL, Schalkwijk J, Rulo HF, et al. Extremely low levels of epidermal skin-derived antileucoproteinase/elafin in a patient with impetigo herpetiformis. Br J Dermatol 1997;137:123–9 [PubMed] [Google Scholar]
- 19.Vaughan Jones SA, Hern S, Nelson-Piercy C, et al. A prospective study of 200 women with dermatoses of pregnancy correlating clinical findings with hormonal and immunopathological profiles. Br J Dermatol 1999;141:71–81 [DOI] [PubMed] [Google Scholar]
- 20.Imai N, Watanabe R, Fujiwara H, et al. Successful treatment of impetigo herpetiformis with oral cyclosporine during pregnancy. Arch Dermatol 2002;138:128–9 [DOI] [PubMed] [Google Scholar]
- 21.Arslanpence I, Dede FS, Gokcu M, et al. Impetigo herpetiformis unresponsive to therapy in a pregnant adolescent. J Pediatr Adolesc Gynecol 2003;16:129–32 [DOI] [PubMed] [Google Scholar]
- 22.Vun YY, Jones B, Al-Mudhaffer M, et al. Generalized pustular psoriasis of pregnancy treated with narrowband UVB and topical steroids. J Am Acad Dermatol 2006;54(2 Suppl):S28–30 [DOI] [PubMed] [Google Scholar]
- 23.El-Din Selim MM, Rehak A, Abdel-Hafez K, et al. Impetigo herpetiformis. Report of a case treated with photochemotherapy (PUVA). Dermatol Monatsschr 1982;168:44–8 [PubMed] [Google Scholar]
- 24.Zabel J, Erenski P. [Clofazimine in the treatment of impetigo herpetiformis]. Przegl Dermatol 1984;71:161–3 [PubMed] [Google Scholar]
- 25.Puig L, Barco D, Alomar A. Treatment of psoriasis with anti-TNF drugs during pregnancy: case report and review of the literature. Dermatology (Basel) 2010;220:71–6 [DOI] [PubMed] [Google Scholar]


