Abstract
A 50-year-old male presented with haemoptysis. Patient had previous history of pulmonary tuberculosis. A tentative diagnosis of fungal ball was made on radiological examination. Surgical removal of lobe of lung was done and on histopathological examination a final diagnosis of aspergilloma was rendered.
Background
As this case had a previous history of pulmonary tuberculosis and remained asymptomatic for 2 years, and had episodes of haemoptysis later, the clinical diagnosis of reactivation of tuberculosis was made. But a tentative diagnosis of fungal ball was made, which was confirmed on histopathological diagnosis. So a differential diagnosis of fungal infection should be kept in mind in cases with previous history of tuberculosis.
Case presentation
A 50-year-old male presented with a history of two episodes of haemoptysis. There was no history of fever or breathlessness. Patient has taken antitubercular treatment for 9 months for pulmonary tuberculosis and remained disease-free for 2 years. Patient was mildly anaemic. On investigations, haemoglobin was 10 g/dl, total leucocyte count of 15 000 cells/mm3, differential leucocyte count was P70L20E10, erythrocyte sedimentation rate was 30 mm in the first hour, platelet count of 2.5 lac/mm3.
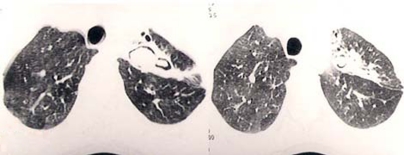
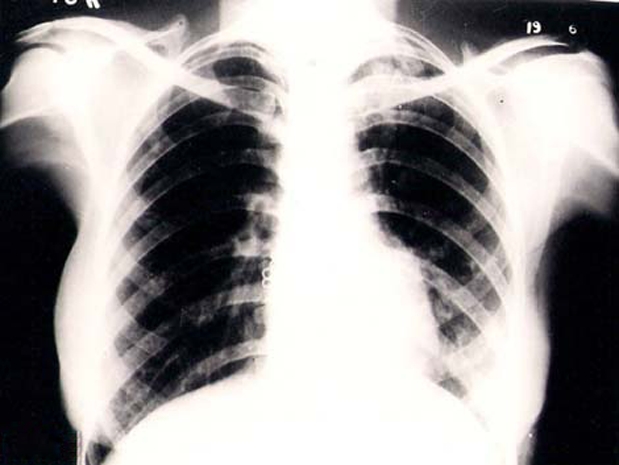
Prothrombin time and activated partial thromboplastin time was within normal limits. Sputum examination including culture for pyogenic and acid-fast bacilli were negative. X-ray chest showed a patch of haziness in left upper lung zone (figure 1). Axial high resolution CT scan at the level of upper thorax revealed cavity formation with round soft tissue lesion leading to formation of air crescent (figure 2). Surgical resection of left upper lobe was done and tissue was submitted for histopathological examination. Microscopic examination revealed, mononuclear cell infiltrate and congestion of lung parenchyma with adjacent fungal wall (figure 3). Fungal hyphae were hyaline, parallel-walled with acute angle branching (figure 4). On the basis of the above findings, a final diagnosis of aspergilloma was rendered.
Figure 1.
X-ray chest showing patch of haziness in left upper lung zone.
Figure 2.
Axial high-resolution CT showing cavity formation with round soft tissue lesion.
Figure 3.
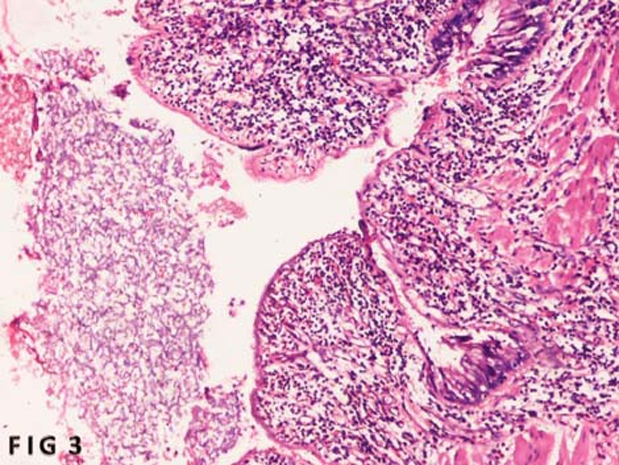
Section showing lung parenchyma and adjacent fungal ball (H&E×50).
Figure 4.
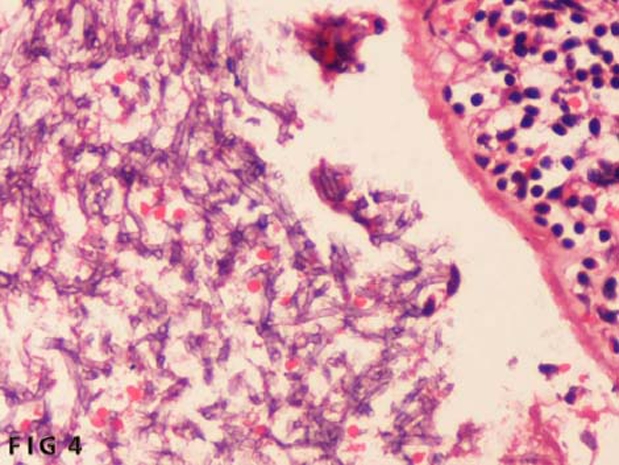
Section showing fungal hyphae branching at acute angle (H&E×500).
Treatment
Resection of upper lobe of lung was done.
Outcome and follow-up
Patient was discharged in good condition.
Discussion
Aspergillus received its name because of resemblance to aspergillum which is used to sprinkle holy water. Aspergillosis is the term used to describe the spectrum of diseases caused by different species of Aspergillus which includes non-invasive disease, aspergilloma, allergic bronchopulmonary aspergillosis, chronic necrotising pneumonia and invasive pulmonary aspergillosis. Aspergillus fumigatus is the most common causative agent.1 It can be found in air, soil, water, food and decomposing vegetations. Route of transmission is through inhalation of conidia, however, infections can be transmitted through water aerosol. After inhalation, the conidia rests in the lung alveoli, where they may germinate especially when associated with immunosuppressed status, and converts into hyphae. The incidence is rising because of increasing number of immunosuppressed patients.
Aspergilloma, also known as Aspergillus fungus ball grows in pre-existing pulmonary cavity which may formed due to previous tuberculosis condition, carcinoma, emphysematous bulla or sarcoidosis.2–5 They are usually present in upper lobe of lung.6 Other sites of involvement are the brain and the kidneys. Patients may remain asymptomatic7 or may present with episodes of haemoptysis which may be massive and life-threatening.8 Cough with fever are other clinical manifestations. Radiological examination may reveal intracavitary density that is positionally mobile.9 Many other conditions like abscesses, neoplasm, haematoma, hydatid cyst and Wegener’s granulomatosis also have similar radiological findings.10–12 Histologically, it is comprised of fungal hyphae, tissue debris, inflammatory cells, fibrin and mucus. The hyphae range in diameter from 2.5 to 4.5 µm and branch at an acute angle. Few serum tests may be helpful in making the diagnosis. Detection of antibodies to Aspergillus by serum precipitin, which is positive in 95% of cases may be helpful in making the diagnosis.13
Treatment should start when the patient becomes symptomatic. Surgical resection of affected lobe of lung is curative but may not possible in all the patients. Oral itroconazole may provide partial or complete resolution. Intracavitary administration of amphotericin-B alone or in combination with other drugs is reported to be effective.14 Bronchial artery embolisation may be used for life-threatening haemoptysis.15
Learning points.
-
▶
Aspergillus fungus ball grows in pre-existing pulmonary cavity which may formed due to previous tuberculosis condition, carcinoma, emphysematous bulla or sarcoidosis
-
▶
Patient may remain asymptomatic for a long duration
-
▶
Bronchial artery embolisation may be used as a treatment modality in patients with life-threatening hemoptysis.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Soubani AO, Chandrashekar PH. The clinical spectrum of pulmonary aspergillous. Chest 2002;121:1988–99 [DOI] [PubMed] [Google Scholar]
- 2.Zizzo G, Castriota-Scanderbeg A, Zarrelli N, et al. Pulmonary aspergillosis complicating ankylosing spondylitis. Radiol Med 1996;91:817–18 [PubMed] [Google Scholar]
- 3.Kawamura S, Maesaki S, Tomono K, et al. Clinical evaluation of 61 patients with pulmonary aspergilloma. Intern Med 2000;39:209–12 [DOI] [PubMed] [Google Scholar]
- 4.Rippon JW. Chapter 23: aspergillosis. Medical Mycology. Third edition Philadelphia, PA: W. B. Saunders, 1988:618–50 [Google Scholar]
- 5.Tomlinson JR, Sahn SA. Aspergilloma in sarcoid and tuberculosis. Chest 1987;92:505–8 [DOI] [PubMed] [Google Scholar]
- 6.Tuncel E. Pulmonary air meniscus sign. Respiration 1984;46:139–44 [DOI] [PubMed] [Google Scholar]
- 7.Glimp RA, Bayer AS. Pulmonary aspergilloma. Diagnostic and therapeutic considerations. Arch Intern Med 1983;143:303–8 [DOI] [PubMed] [Google Scholar]
- 8.British Tuberculosis and thoracic Association Aspergilloma and residual tuberculous cavities: the results of resurvey. Tubercle 1970;51:227–45 [PubMed] [Google Scholar]
- 9.Roberts CM, Citron KM, Strickland B. Intrathoracic aspergilloma: role of CT in diagnosis and treatment. Radiology 1987;165:123–8 [DOI] [PubMed] [Google Scholar]
- 10.Bandoh S, Fujita J, Fukunaga Y, et al. Cavitary lung cancer with an aspergilloma-like shadow. Lung Cancer 1999;26:195–8 [DOI] [PubMed] [Google Scholar]
- 11.Le Thi Huong D, Wechsler B, Chamuzeau JP, et al. Pulmonary aspergilloma complicating Wegener’s granulomatosis. Scand J Rheumatol 1995;24:260. [DOI] [PubMed] [Google Scholar]
- 12.Knower MT, Kavanagh P, Chin R., Jr Intracavitory haematoma simulating mycetoma formation. J Thorac Imag 2002;17:84–8 [DOI] [PubMed] [Google Scholar]
- 13.Yong RC, Benett JE. Invasive aspergillosis: absence of detectable antibody response. Am Rev Respir Dis 1971;104:710–16 [DOI] [PubMed] [Google Scholar]
- 14.Giron JM, Poey CG, Fajadet PP, et al. Inoperable pulmonary aspergilloma: percutaneous CT-guided injection with glycerin and amphotericin B paste in 15 cases. Radiology 1993;188:825–7 [DOI] [PubMed] [Google Scholar]
- 15.Mal H, Rullon I, Mellot F, et al. Immediate and long-term results of bronchial artery embolization for life-threatening hemoptysis. Chest 1999;115:996–1001 [DOI] [PubMed] [Google Scholar]