Abstract
Cavernous lymphangiomas are usually identified in infants and children with the majority of lesions found around the head and neck, trunk or extremities. Tumours affecting the intra-abdominal organs are rare. The authors report a case of small bowel cavernous lymphangioma arising within the jejunum of a 34-year-old woman presenting with dyspnoea and anaemia, and review the existing literature relating to this uncommon tumour.
Background
Cavernous lymphangiomas of the small bowel are benign lesions that often present with anaemia. As it has traditionally been difficult to investigate the ileum and jejunum, these lesions have been regarded as being rare, and often not considered in the differential diagnosis of patients with iron deficiency anaemia related to the gastrointestinal tract. With the advent of capsule endoscopy and enteroscopy, the incidence of reporting of cavernous lymphangiomas appears to be increasing. The aim of this report and literature review is to highlight this tumour within the differential for anaemia, and to identify new means of investigation that may assist in achieving the diagnosis.
Case presentation
A 34-year-old woman was referred for investigation of dyspnoea and was found to have iron deficiency anaemia with a haemoglobin of 6 g/dl. There was no history of irregular or heavy menses and no gastrointestinal symptoms were noted. No significant medical history or family history was noted and physical examination was unremarkable.
Investigations
Upper and lower endoscopies did not reveal a bleeding source. A capsule endoscopy identified a lesion within the jejunum. A CT scan identified the mass but there was no evidence of metastatic spread and the nature of the mass was uncertain. A push enteroscopy demonstrated a lobular, circumferential mass in the proximal jejunum. It was submucosal in location, occupying the whole of the circumference and had a lymphangiectatic appearance (figure 1). The appearances were classically those of a cavernous lymphangioma. The site was marked with a tattoo of India ink.
Figure 1.

Enteroscopic appearance of the lymphangioma.
Treatment
An elective resection of the mass was performed. No ascites, lymphadenopathy, peritoneal disease or liver metastases were identified at laparotomy. The mass was identified by means of the tattoo placed at enteroscopy and the lesion was palpable at the marked point. A segmental resection was performed including adjacent mesentery and bowel, with an end-to-end anastomosis. An additional lesion, not identified on preoperative imaging, was found in the jejunal mesentery and was also excised.
Gross examination of the specimen revealed a polypoid, multinodular tumour measuring 5.3 × 4 × 1.5 cm with normal adjacent jejunum (figure 2). The tumour was spongy on cross-section and white fluid was expressed from cystic spaces. Histologically, the mucosa and submucosa were markedly expanded and replaced by dilated lymphatic spaces (figure 3) whereas the adjacent jejunum was normal (figure 4). The mesenteric lesion was an additional lymphangioma with fibromuscular lymphatic walls and luminal benign lymphoid aggregates (figure 5).
Figure 2.

This gross photograph of the segmental jejunal resection illustrates the striking multinodular and polypoid appearance of the jejunal lymphangioma, along with the entirely normal appearing adjacent jejunum.
Figure 3.
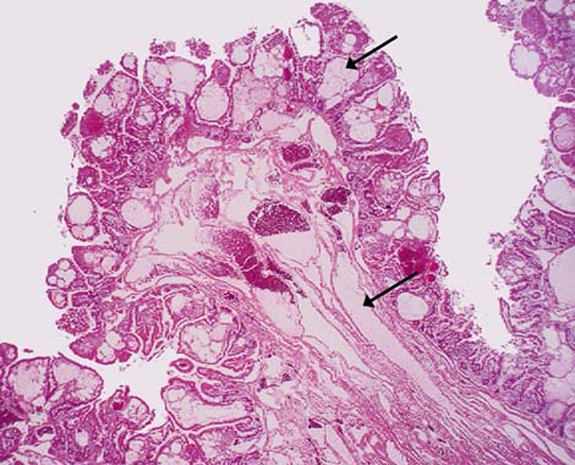
The mucosa and submucosa are expanded and replaced by innumerable dilated lymphatics (arrows).
Figure 4.

The jejunum adjacent to the lymphangioma was normal histologically, as illustrated here with intact villous architecture, mucosa and submucosa, lacking dilated lymphatic spaces. This feature excludes diffused lymphangiomatosis from the differential.
Figure 5.
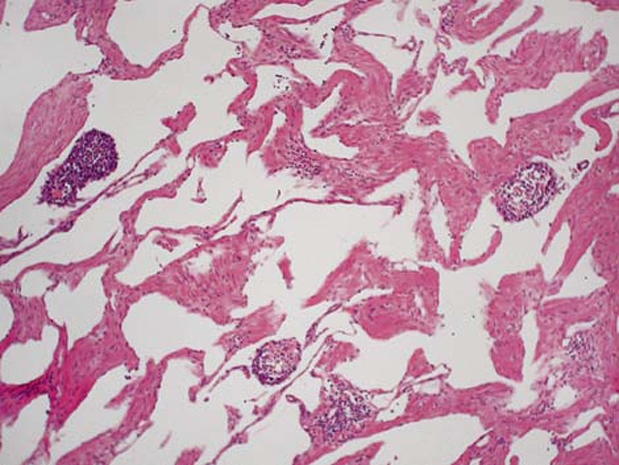
In addition to the mass forming lymphangioma occupying the wall of the jejunum, an additional focal mesenteric lymphangioma was identified in the resection specimen. The fibromuscular walls making up the lymphatic vessels and luminal benign lymphoid aggregates are illustrated.
Outcome and follow-up
The patient’s postoperative recovery was unremarkable and at follow-up she was asymptomatic.
Discussion
Cavernous lymphangiomas are a rare tumour of the lymphatic system, mainly affecting the head and neck, trunk and extremities with the vast majority of tumours presenting in infancy and childhood.1 Lymphangiomas account for 6%2 of small bowel tumours seen in children but are a smaller percentage, approximately 1.4–2.4% in adults.3 Within the peritoneal cavity, the majority of lymphangiomas are identified within the mesentery and retroperitoneum.4 Lesions affecting the jejunum or ileum are rare and account for less than 1% of all lymphangiomas.5
The histological features of cavernous lymphangioma were first described by Gaudier and Gorse in 1913.6 The tumour is a benign lesion consisting of single-layer endothelial-lined lymphatic spaces containing chylous or serous material.7
Review of the English language literature for the 50-year period from 1960 to 2009 reveals only 19 reports of small bowel lymphangiomas (table 1).3 8–24 A total of 40 patients are reported, with a wide age range at presentation from 5 to 75 years and an equal gender distribution have been observed. Of those in which a specific anatomical small bowel location was noted, 24 of the lesions were within the jejunum and 5 in the ileum.
Table 1.
English literature summary of jejunal and ileal lymphangioma case reports
| Author | Year | No | Gender | Age | Presentation | Location | Other lesions | Treatment |
|---|---|---|---|---|---|---|---|---|
| Shyung | 2009 | 2 | M | 32 | Anaemia | NS | No | DBE |
| M | 43 | Incidental | NS | No | NS | |||
| Feng | 2009 | 1 | M | 69 | Melaena | Jejunum | No | DBE |
| Yeh | 2009 | 1 | NS | NS | GI bleeding | Ileum | No | Resection |
| Crook | 2008 | 1 | M | 33 | GI bleeding | Jejunun | No | Resection |
| Huang | 2008 | 1 | M | 51 | Melaena | Jejunum | No | Resection |
| Norris | 2008 | 1 | F | 23 | Ovarian mass | Jejunum | Yes | Resection |
| Hsu | 2007 | 1 | F | 75 | Anaemia | Jejunum | No | Resection |
| Pickhardt | 2007 | 1 | F | 55 | Asymptomatic | Ileum | No | Resection |
| Oshita | 2005 | 1 | M | 5 | Intussusception | Jejunum | NS | Resection |
| Honda | 2003 | 1 | F | 31 | Anaemia | Jejunum | No | Resection |
| Seki | 1998 | 1 | F | 54 | Abdominal mass | Jejunum | Omentum (main) | Resection |
| Uncu | 1997 | 2 | M | 43 | Abdominal mass | Ileum | No | Resection |
| M | 19 | Incidental | Ileum | No | Resection | |||
| Hanagiri | 1992 | 1 | M | 53 | Obstruction | NS | No | Resection |
| Shigematsu | 1988 | 3 | M | 55 | Anaemia/melaena | Jejunum (2) + ileum (1) | No | Resection |
| F | 65 | Incidental | Jejunum (7) | Duodenum | Resection | |||
| M | 46 | Abdominal pain | Jejunum (2) | No | Resection | |||
| Colizza | 1981 | 1 | F | 58 | Melaena | Jejunum | Stomach | Resection |
| Cohen | 1971 | 1 | NS | NS | NS | Jejunum | NS | NS |
| Schmutzer | 1964 | 3 | NS | NS | Incidental | Jejunum | No | Resection |
| NS | NS | Incidental | Ileum | No | Resection | |||
| NS | NS | Incidental | NS | No | Resection | |||
| Good | 1962 | 16 | NS | NS | NS | NS | NS | NS |
| Ralston | 1961 | 1 | M | 58 | Anaemia | Jejunum | No | Resection |
DBE, double-balloon enteroscopy; GI, gastrointestinal; NS, not stated.
Hanagiri and colleagues also document an additional 33 patients from the Japanese literature between 1967 and 1990. In addition to the 19 English literature reports, 8 were from the Far East, including 5 Japanese and 3 Taiwanese manuscripts, suggesting that there may be a Japanese/Taiwanese predisposition to small bowel lymphangiomas. In the Japanese language literature, although the age distribution was comparable, there were twice as many males as females with an equal distribution between ileum and jejunum.
The number of lymphangiomas reported has increased in recent literature, with 10 of the 19 papers published in the past decade. This is likely due to improvements in diagnostic imaging with the advent of capsule endoscopy and double-balloon enteroscopy rather than a true increase in the prevalence of the tumour.
The standard management of lymphangiomas until recently has been through surgical resection. However, with the advent of double-balloon enteroscopy, this modality may be able to treat small tumours and this indeed has been accomplished in two cases.23 24
Learning points.
-
▶
Cavernous lymphangiomas are rare tumours of the lymphatic system, mainly affecting the head and neck, trunk and extremities usually presenting in infancy and childhood.
-
▶
Lesions affecting the small bowel are uncommon but appear to be on the increase probably due to improvements in diagnostic modalities available.
-
▶
The standard management of lymphangiomas until recently has been through surgical resection, however, the development of double-balloon enteroscopy has been successfully used to treat small tumours and may become the standard of care in the future.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Alqahtani A, Nguyen LT, Flageole H, et al. 25 years’ experience with lymphangiomas in children. J Pediatr Surg 1999;34:1164–8 [DOI] [PubMed] [Google Scholar]
- 2.Fonkalsrud EW. Congenital malformations of the lymphatic system. Semin Pediatr Surg 1994;3:62–9 [PubMed] [Google Scholar]
- 3.Hanagiri T, Baba M, Shimabukuro T, et al. Lymphangioma in the small intestine: report of a case and review of the Japanese literature. Surg Today 1992;22:363–7 [DOI] [PubMed] [Google Scholar]
- 4.Rieker RJ, Quentmeier A, Weiss C, et al. Cystic lymphangioma of the small-bowel mesentery: case report and a review of the literature. Pathol Oncol Res 2000;6:146–8 [DOI] [PubMed] [Google Scholar]
- 5.Uncu H, Erdem E, Kuterdem E. Lymphangiomas of the ileum: a report of two cases and a review of the literature. Surg Today 1997;27:542–5 [DOI] [PubMed] [Google Scholar]
- 6.Gaudier H, Gorse P. Lymphangiome kystique abdoménoscrotal retropéritonéal. Presse Méd 1913;21:458–89 [Google Scholar]
- 7.Takiff H, Calabria R, Yin L, et al. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg 1985;120:1266–9 [DOI] [PubMed] [Google Scholar]
- 8.Ralston M. Lymphangioma-haemangioma of the jejunum: a rare cause of alimentary tract bleeding. Aust N Z J Surg 1961;30:209–11 [DOI] [PubMed] [Google Scholar]
- 9.Good A. Tumors of the small intestine. Am J Roentgenol 1962;89:685–705 [PubMed] [Google Scholar]
- 10.Schmutzer KJ, Holleran WM, Regan JF. Tumors of the small bowel. Am J Surg 1964;108:270–6 [DOI] [PubMed] [Google Scholar]
- 11.Cohen A, McNeill D, Terz JJ, et al. Neoplasms of the small intestine. Am J Dig Dis 1971;16:815–24 [DOI] [PubMed] [Google Scholar]
- 12.Colizza S, Tiso B, Bracci F, et al. Cystic lymphangioma of stomach and jejunum: report of one case. J Surg Oncol 1981;17:169–76 [DOI] [PubMed] [Google Scholar]
- 13.Shigematsu A, Iida M, Hatanaka M, et al. Endoscopic diagnosis of lymphangioma of the small intestine. Am J Gastroenterol 1988;83:1289–93 [PubMed] [Google Scholar]
- 14.Seki H, Ueda T, Kasuya T, et al. Lymphangioma of the jejunum and mesentery presenting with acute abdomen in an adult. J Gastroenterol 1998;33:107–11 [DOI] [PubMed] [Google Scholar]
- 15.Honda K, Ihara E, Ochiai T, et al. Lymphangioma of small intestine. Gastrointest Endosc 2003;58:574–5 [DOI] [PubMed] [Google Scholar]
- 16.Oshita M, Okazaki T, Yamataka A, et al. Jejuno-jejunal intussusception secondary to submucosal lymphangioma in a child. Pediatr Surg Int 2005;21:1001–3 [DOI] [PubMed] [Google Scholar]
- 17.Pickhardt PJ, Kim DH, Taylor AJ, et al. Extracolonic tumors of the gastrointestinal tract detected incidentally at screening CT colonography. Dis Colon Rectum 2007;50:56–63 [DOI] [PubMed] [Google Scholar]
- 18.Hsu SJ, Chang YT, Chang MC, et al. Bleeding jejunal lymphangioma diagnosed by double-balloon enteroscopy. Endoscopy 2007;39(Suppl 1):E5–6 [DOI] [PubMed] [Google Scholar]
- 19.Norris JR, Stacey M, Rampaul RS, et al. Jejunal lymphangioma presenting as an ovarian mass. J R Army Med Corps 2008;154:243–4 [DOI] [PubMed] [Google Scholar]
- 20.Huang Q, Minor MA, Weber HC. Clinical challenges and images in GI. Diagnosis: Cavernous lymphangioma of the jejunum. Gastroenterology 2009;136:1170, 1465. [DOI] [PubMed] [Google Scholar]
- 21.Crook DW, Knuesel PR, Froehlich JM, et al. Comparison of magnetic resonance enterography and video capsule endoscopy in evaluating small bowel disease. Eur J Gastroenterol Hepatol 2009;21:54–65 [DOI] [PubMed] [Google Scholar]
- 22.Yeh TS, Liu KH, Su MY, et al. Laparoscopically assisted bowel surgery in an era of double-balloon enteroscopy: from inside to outside. Surg Endosc 2009;23:739–44 [DOI] [PubMed] [Google Scholar]
- 23.Li F, Osuoha C, Leighton JA, et al. Double-balloon enteroscopy in the diagnosis and treatment of hemorrhage from small-bowel lymphangioma: a case report. Gastrointest Endosc 2009;70:189–90 [DOI] [PubMed] [Google Scholar]
- 24.Shyung LR, Lin SC, Shih SC, et al. Proposed scoring system to determine small bowel mass lesions using capsule endoscopy. J Formos Med Assoc 2009;108:533–8 [DOI] [PubMed] [Google Scholar]


