Abstract
OBJECTIVE
Nonelderly patients presenting with knee pain often have patellofemoral maltracking or impingement abnormalities. There is a relative paucity of literature on the incidence and significance of impingement-related edema of the superolateral aspect of Hoffa’s (infrapatellar) fat pad in these cases. Our study was designed to systematically evaluate the correlation of superolateral Hoffa’s fat pad edema with various anatomic parameters of trochlear morphology and patellar alignment.
MATERIALS AND METHODS
We evaluated 50 knee MRI examinations in 47 patients for the presence of edema in superolateral Hoffa’s fat pad and associated anatomic abnormalities of the patellofemoral joint.
RESULTS
Of the 50 examinations, 25 (50%) showed superolateral Hoffa’s fat pad edema, and statistically significant differences were seen between those with and without edema with respect to sex (6/22 men vs 19/28 women) and patellar tendon patellar–length ratio (1.3 ± 0.16 and 1.1 ± 0.12 for those with and without edema, respectively).
CONCLUSION
The findings in our study suggest that edema in superolateral Hoffa’s fat pad may be an important indicator of underlying patellofemoral maltracking or impingement in younger, symptomatic patients.
Keywords: Hoffa’s fat pad edema, infrapatellar fat pad, malalignment, patellofemoral impingement
Anterior knee pain is a common complaint among patients referred for MRI. Typically, pain occurs during activities such as running, squatting, going up and down stairs, cycling, and jumping and can force patients to curtail or cease such exercise altogether [1]. Patellofemoral disorders are among the most frequently described sources of anterior knee pain [2], but the precise roles that various extrinsic and intrinsic predisposing factors play in the development of pain and how they interact are unclear.
Although patellofemoral maltracking or impingement has been implicated as an underlying cause of knee pain, the precise mechanisms eliciting symptoms are not fully understood due, at least in part, to the complexity of the joint [3]. In addition to shielding the tibiofemoral joint, the primary biomechanical function of the patella is to increase the mechanical advantage of the quadriceps muscle by extending its effective lever arm [3]. Moreover, the patella centers the divergent pull of the different quadriceps muscle components. Thus, normal patellar alignment in relation to the trochlear groove has important implications for proper load bearing [3, 4]. Clinically, patellofemoral disorders encompass aberrations in both static and dynamic forces acting on the joint [5]. Dynamic MRI studies have been used to diagnose these disorders [6], although such examinations have not yet reached widespread clinical use because of the lack of required technologist skill and interpretation standardization. Static parameters of trochlear geometry and patellofemoral alignment, such as the patellar tendon–patellar length ratio, femoral sulcus angle, sulcus depth, lateral patellofemoral angle, patellar translation, and tibial tubercle–trochlear groove distance have been used to infer dynamic maltracking abnormalities [6–11]. Such anatomic and biomechanical abnormalities are hypothesized to lead to chondrosis, early osteoarthritis, synovial proliferation, subchondral cystic or sclerotic changes, and fat pad impingement, all of which can cause pain [2, 12].
Chung et al. [13] described edema in the superolateral portion of the infrapatellar fat pad as a secondary sign of the patellar tendon–lateral femoral condyle friction syndrome. However, this finding has been acknowledged to be underreported in the radiology literature, and its precise relation to patellofemoral alignment remains less well defined [13, 14]. Because superolateral Hoffa’s fat pad edema is a frequent finding in patellar maltracking or impingement disorders, our study was designed to systematically evaluate its correlation with various anatomic parameters of trochlear morphology and patellar alignment.
Materials and Methods
Patient Selection
With approval of the institutional review board, we retrospectively reviewed the records of 212 patients who underwent MRI of the knee as outpatients over a 2-month period. Patients outside the ages of 14–50 years or those with a history of direct trauma to the knee, prior surgery or arthroscopy, or major internal derangement (such as anterior or posterior cruciate ligament tear) were excluded. This left 47 patients with 50 knee examinations available for analysis.
MRI
MR images were acquired on a 1.5-T scanner (Signa, GE Healthcare or Excelart, Toshiba) and an extremity coil with a 14- to 16-cm field of view and 256 × 256 matrix. The sequences obtained varied between outpatient imaging centers and included coronal and sagittal intermediate-weighted fast spin-echo (FSE) (TR range/TE range, 1,400–3,000/19–33), coronal and sagittal fat-suppressed T2-weighted FSE (1,720–4,200/60–84) or fat-suppressed intermediate-weighted FSE (1,520–3,000/20–26), axial intermediate-weighted FSE (1,500–2,500/20–27), and axial fat-suppressed T2-weighted (1,720–3,340/60–84) or fat-suppressed intermediate-weighted FSE (1,500–3,000/20–27) images. Images were independently reviewed by one third-year radiology resident and one board-certified radiologist with 8 years of experience in musculoskeletal imaging. All discrepant quantitative and qualitative measures were resolved by consensus.
Image Analysis
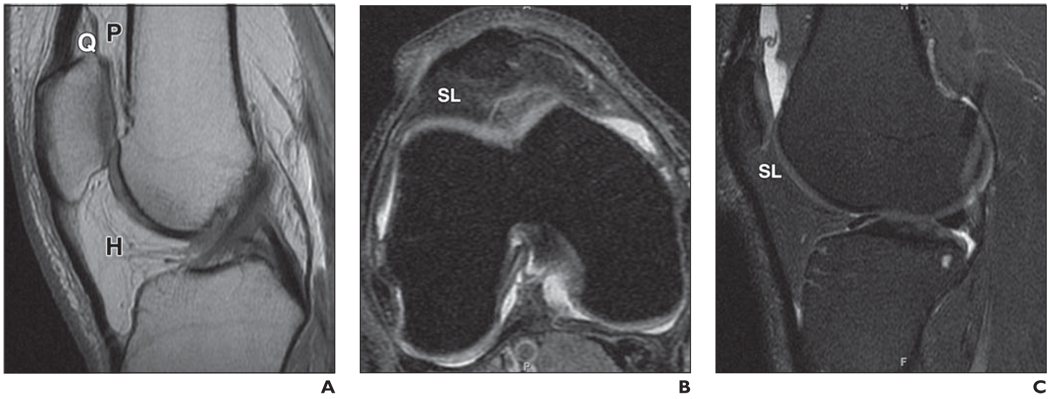
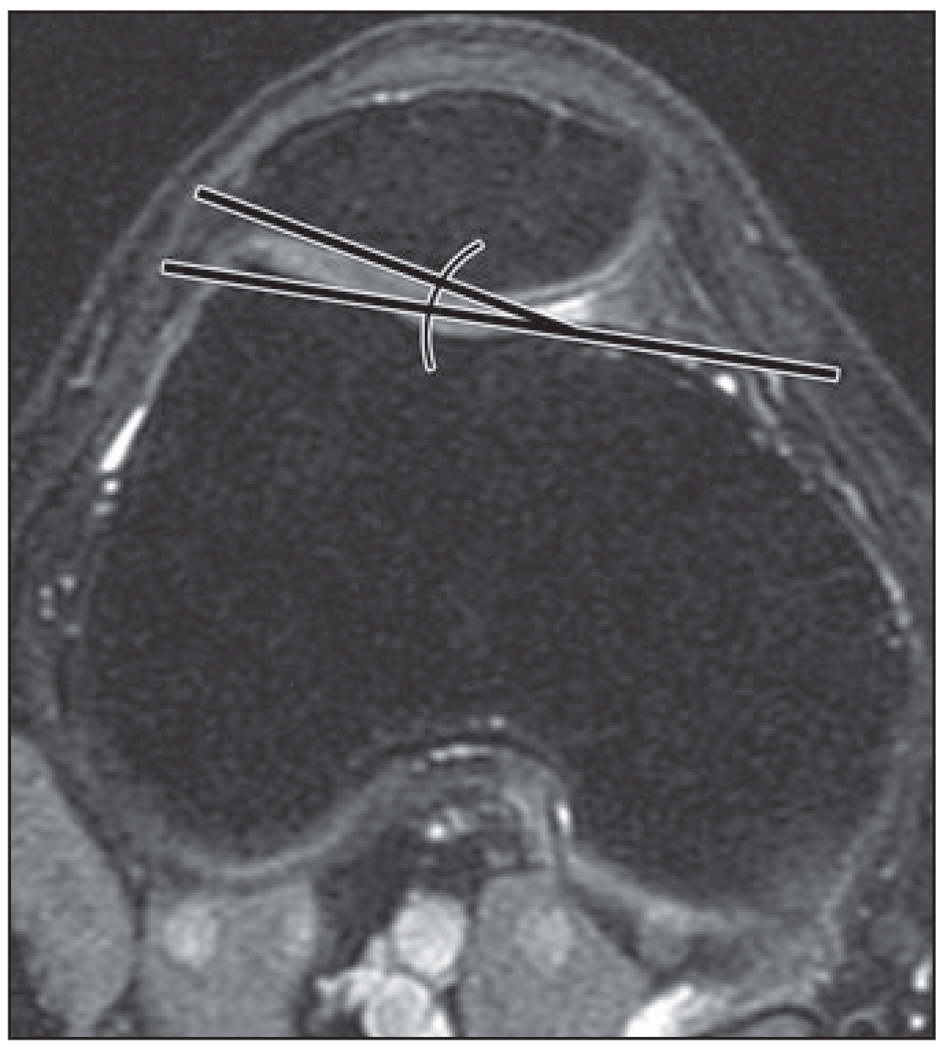
There are three fat pads in the anterior knee: the quadriceps fat pad, the prefemoral fat pad, and Hoffa’s fat pad (Fig. 1). We evaluated all three fat pads, specifically focusing on edema in the superolateral portion of Hoffa’s fat pad. For subtle cases of fat pad edema, a region of interest measurement of signal intensity in the superolateral portion had to be 20% higher than the surrounding normal fat pad signal to be recorded as positive. Patella alta was assessed using the Insall–Salvati ratio of patellar tendon: patella length for MRI, with patella alta suggested at ratio values of greater than 1.3 [15]. Other quantitative metrics included trochlear sulcus characteristics, patellar translation, and patellar tilt (Figs. 2–6). The sulcus depth and angle at both 3 cm above the joint line and at the level of the posterior physeal line were recorded in a method similar to other studies [11, 16]. Patellar translation was measured as the distance between perpendicular lines drawn on an axial image from the medial edge of the patella through the most anterior point of the medial condyle [17], with medial translation recorded as negative and lateral translation recorded as positive values. In evaluating patellar tilt, the lateral patellofemoral angle was measured between the bony lateral patellar facet and the tangent to the anterior condyles [17]. As a proxy for the clinically determined Q-angle, the degree of tibial tuberosity lateralization was quantified by measuring the transverse distance between the deepest portion of the trochlear groove and the midpoint of the patellar tendon insertion on the tibial tuberosity, similar to a method proposed by Wittstein et al. [7].
Fig. 1.
37-year-old man with knee pain and small joint effusion but normal fat pads.
A, Midsagittal intermediate-weighted MR image shows normal quadriceps (Q), prefemoral fat pad (P), and Hoffa’s fat pad (H).
B, Axial intermediate-weighted MR image with fat suppression shows normal appearance of superolateral portion (SL) of Hoffa’s fat pad.
C, Sagittal intermediate-weighted MR image with fat saturation shows normal appearance of superolateral Hoffa’s fat pad (SL).
Fig. 2.
Method for determining patellar tendon–patellar length ratio. Greatest diagonal length of patella (solid line) and distance of patellar tendon from inferior patellar pole to tibial tubercle (dashed line) were measured on midsagittal image. Normal patellar tendon–patellar length ratio is between 0.9 and 1.3 [15].
Fig. 6.
Method for determining tibial tuberosity to trochlear groove distance. While scrolling axially (but depicted coronally for better visualization), lateral distance (double-headed arrow) from trochlear groove (arrowhead) to tibial tuberosity (asterisk) is measured. Normal tibial tubercle–trochlear groove distance is ≤ 10 mm [7].
Other recorded findings included qualitative assessment of the quadriceps and patellar tendon, patellar morphology, retinacular integrity, muscle injury or atrophy, and presence of joint effusion. The soft tissues were analyzed for any areas of abnormal signal intensity or masses. Abnormal morphology of the patellar and quadriceps tendons, with or without abnormal signal intensity, was classified as tendinopathy. Patellar morphology was classified by Wiberg type [18] and, to simplify statistical analysis, converted to binary data as either type 1 (medial and lateral facets equal in length, thought to be most stable) or type 2/3 (lateral facet longer than the medial facet). Areas of abnormal signal intensity or fatty infiltration of the muscles around the joint were classified as abnormal. Any amount of supraphysiologic joint fluid (defined for study purposes as > 5-mm thickness of fluid signal on the midline sagittal fat-suppressed sequence in the suprapatellar recess) was classified as an effusion.
Statistical Analysis
Subjects were categorized according to the presence or absence of superolateral Hoffa’s fat pad edema. Differences in sex proportion, prefemoral, and quadriceps fat pad edema were analyzed using Fisher’s exact test; univariate analysis of differences in age, patellar tendon–patellar length ratio, patellofemoral angle, sulcus angle, sulcus depth, tibial tubercle–trochlear groove distance, and patellar lateralization was carried out using a two-tailed Student’s t test. Subjects were also grouped by sex for analysis of patellar tendon–patellar length ratio using the Student’s t test. Additionally, two-way analysis of variance was performed with sex and patellar tendon–patellar length ratio as factors for the presence of superolateral Hoffa’s fat pad edema and with sex and patellofemoral angle as factors for superolateral Hoffa’s fat pad edema. Patients were dichotomized with respect to patella alta using a threshold ratio of 1.3 for patellar tendon–patellar length ratio; Fisher’s exact test was performed in analyzing the association of patella alta with superolateral Hoffa’s fat pad edema. Statistical analysis was carried out using statistical software (SPSS Statistics 17.0), with significance defined at p = 0.05.
Results
Twenty-five of 50 patients (50%) exhibited edemalike T2 hyperintense signal in the superolateral portion of Hoffa’s fat pad (representative examples in Figs. 7–9). Tables 1 and 2 summarize patient demographics and the results of the morphologic assessment with respect to the presence or absence of edema in the superolateral portion of Hoffa’s fat pad. There was no significant difference in age between those patients with and without superolateral Hoffa’s fat pad edema (Student’s t test, p = 0.39). However, there were more women with superolateral Hoffa’s fat pad edema than men (Fisher’s exact test, p = 0.01). In addition, there was a statistically significant association between the presence of superolateral Hoffa’s fat pad edema and prefemoral fat pad edema (Fisher’s exact test, p = 0.004); no association was found between superolateral Hoffa’s fat pad edema and quadriceps fat pad edema (Fisher’s exact test, p = 0.23).
Fig. 7.
47-year-old woman with knee pain.
A and B, Sagittal (A) and axial (B) T2-weighted MR images with fat suppression show hyperintense edemalike signal (arrow) within superolateral aspect of infrapatellar (Hoffa’s) fat pad.
Fig. 9.
34-year-old man with bilateral knee pain.
A and B, Sagittal intermediate-weighted images with fat suppression in both right (A) and left (B) knees show superolateral Hoffa’s fat pad edema (arrow).
TABLE 1.
Superolateral Hoffa’s Fat Pad Edema Demographics and Other Knee Fat Pads
| Parameter | Age (y) | Men/Women | Quadriceps Fat Pad Edema |
Prefemoral Fat Pad Edema |
|---|---|---|---|---|
| Without edema | 33.8 (12.3) | 16/9 | 0 | 6 |
| With edema | 31.5 (11.6) | 6/19 | 3 | 17 |
| Students’ t or Fisher’s exact testa (p) | 0.39 | 0.01 | 0.23 | 0.004 |
Note—Data in parentheses are SD.
Student’s t test was used to test for statistically significant difference in age between the two groups; Fisher’s exact test was used for sex and associations with quadriceps and prefemoral fat pads.
TABLE 2.
Morphologic Measurements of Superolateral Hoffa’s Fat Pad Edema
| Parameter | PTPL | PFA (°) | Sulcus Angle (°) | Sulcus Deptha (mm) | TTTG (mm) | Patellar Lateralization (mm) |
|---|---|---|---|---|---|---|
| Mean without edema | 1.1 (0.12) | 7.0 (2.2) | 155 (10.9) | 3.5 (1.7) | 10.9 (2.4) | 1.2 mm (1.9) |
| Mean with edema | 1.3 (0.16) | 4.8 (4.9) | 150 (8.4) | 4.4 (1.4) | 11.4 (3.4) | 0.8 mm (2.8) |
| Student’s t test (p) | < 0.001 | 0.047b | 0.07 | 0.06 | 0.57 | 0.60 |
Note—Data in parentheses are SD. PTPL = patellar tendon–patellar length ratio, PFA = lateral patellofemoral angle, TTTG = tibial tuberosity to trochlear groove distance.
Measured at 3 cm above joint line.
When sex was added as a covariate, p = 0.15.
Univariate analysis showed significant differences between patients with and without superolateral Hoffa’s fat pad edema with respect to patellar tendon–patellar length ratio and patellofemoral angle at the p = 0.05 significance level (Table 2). Although there was a trend toward a shallower sulcus, as evidenced by greater femoral sulcus angle and decreased sulcus depth (as measured at 3 cm above the joint line) in patients with superolateral Hoffa’s fat pad edema, these associations did not reach statistical significance (Student’s t test, p = 0.07 and 0.06, respectively). Using measurements of the femoral sulcus angle and sulcus depth at the physeal line also failed to show significant associations (data not shown). There was no statistically significant difference in tibial tubercle–trochlear groove distance or patellar translation. Wiberg patellar type did not differ between those with and without superolateral Hoffa’s fat pad edema (Fisher’s exact test, p = 0.99).
There was no statistically significant association between patellar tendon–patellar length ratio and sex (Student’s t test, p = 0.25), and the association between superolateral Hoffa’s fat pad edema and patellar tendon–patellar length ratio remained significant when sex was added as a covariate (two-way analysis of variance, p = 0.001). The association between patellofemoral angle and superolateral Hoffa’s fat pad edema did not remain significant when sex was added as a covariate (two-way analysis of variance, p = 0.15). Using a ratio of 1.3 as a cutoff [15], patella alta was seen in 11 subjects with and only one without superolateral Hoffa’s fat pad edema (Fisher exact text, p = 0.002). No significant association was found between superolateral Hoffa’s fat pad edema and the presence of quadriceps or patellar tendinopathy, retinacular integrity, or muscle injury or atrophy (data not shown).
Discussion
Hoffa’s infrapatellar fat pad is one of three anterior fat pads of the knee, the other two being the anterior suprapatellar (quadriceps) and posterior suprapatellar (prefemoral) fat pads. The infrapatellar fat pad is an intracapsular structure and plays a role in stabilizing the patella in extremes of flexion and extension [19]. Superior to inferior, it extends from the patella to the anterior menisci and tibial periosteum and anterior to posterior, from the patella tendon to the synovial lining of the knee. Superoposteriorly, it extends to the cartilage overlying the anterior aspect of the distal femur [14, 20]. Both intrinsic and extrinsic disease processes can affect it. Intrinsic abnormalities include intracapsular chondroma, localized nodular synovitis, postprocedural fibrosis, shear injury, and nonspecific inflammation; extrinsic causes include processes related to articular disease (e.g., intraarticular bodies, meniscal cyst), synovial abnormalities (e.g., pigmented villonodular synovitis, rheumatoid arthritis, synovial or ganglion cysts), and anterior extracapsular abnormalities such as patellofemoral disorders [14, 20, 21].
Hoffa [22] first recognized chronic impingement of the fat pad between the femur and tibia in 1904. The impingement manifests as fat pad enlargement and increased T2 signal [14, 20]. A second form of impingement, which is clinically more common but radiologically more subtle, occurs at the superolateral portion of the fat pad between the patellar tendon and lateral femoral condyle and results in high T2 signal intensity related to edema [14]. It is this signal abnormality in superolateral Hoffa’s fat pad that has recently been suggested as a secondary sign of patellofemoral maltracking in the patellar tendon–lateral femoral condyle friction syndrome [13, 14], but its relation to the underlying joint geometry has never been systematically evaluated.
In this study, we found that female sex and several markers of patellar instability appear to be associated with superolateral Hoffa’s fat pad edema in patients with knee pain referred for MRI. These markers included a higher position of the patella and at least a trend toward increased lateral patellar tilt compared with patients without superolateral Hoffa’s fat pad edema. These findings suggest that the edema signal observed in the superolateral portion of Hoffa’s fat pad is the result of abnormal friction and mechanical impingement of the fat pad between the lateral femoral condyle and the patellar tendon, as previously postulated by Chung et al. [13]. A similar phenomenon occurring at the level of the superior pole of the patella may be responsible for the association of superolateral Hoffa’s fat pad edema and prefemoral fat pad edema, which has received little attention in the radiologic literature. In our study, the prefemoral fat pad edema was also localized to the central or lateral portion of the fat pad.
Because we interpret superolateral Hoffa’s fat pad edema as a marker of underlying patellofemoral disorder, including maltracking and impingement, we sought to systematically evaluate parameters of the joint geometry and morphology. How malalignment is defined remains a subject of debate. More recently, patellofemoral malalignment has been understood to describe a clinical abnormality resulting from a complex constellation of static and dynamic forces acting on the patellofemoral joint. Post et al. [5] defined patellofemoral malalignment as “bony alignment, joint geometry, soft-tissue restraints, neuromuscular control, and functional demands [combining] to produce symptoms as a result of abnormally directed loads, which exceed the physiologic threshold of the tissues.” Sex differences in the biomechanics of the patellofemoral joint that may predispose to patellofemoral maltracking abnormalities [23] likely contribute to the fact that more females were observed to have superolateral Hoffa’s fat pad edema in our study.
Patella alta traditionally has been measured by the radiographic method proposed by Insall and Salvati, which has been adapted for use in MRI [15]. Patella alta is the most consistent anatomic feature of patellar instability [24], which allows excessive lateral motion by reducing the articular contact between the patella and trochlea at a given angle of flexion [4, 25]. Mechanical modeling experiments have shown that because patella alta causes a delay in patellofemoral articular contact, maximal contact force and contact pressure between the patella and trochlea are abnormally increased [26]. These factors likely account for the association between patella alta and articular cartilage abnormalities as well as patellar malalignment and instability [25, 27]. The statistically significant association in our study between superolateral Hoffa’s fat pad edema and patella alta is in accordance with these theories and previous studies [13]. However, it should be noted that the correlation between patella alta, patellar cartilage defects, and patellofemoral congruence has recently been challenged [28, 29].
In our results, the association between increased patellar tilt (indicated by lower patellofemoral angle) and superolateral Hoffa’s fat pad edema was shown to be attributable, at least in part, to sex differences. Although it may not be independently significant, the association between patellar tilt and superolateral Hoffa’s fat pad edema is in keeping with the idea that the angle of engagement between the lateral patellar facet and lateral facet of the trochlea is a critical determinant of dynamic patellofemoral stability [4, 8]. This implies that instability of the patella during engagement with the sulcus could be responsible for edema in Hoffa’s fat pad as the result of a friction syndrome. Although patellar lateralization has also been suggested as an underlying cause of patellofemoral instability [30], we found no significant difference in this measurement between patients with superolateral Hoffa’s fat pad edema and those without. In addition, despite the fact that patients with increased tibial tubercle–trochlear groove distance and Q angle (the clinical surrogate of the tibial tubercle–trochlear groove distance) are more likely to have patellofemoral malalignment and are at increased risk for patellar subluxation [31], in our study patients with superolateral Hoffa’s fat pad edema showed only marginally higher mean tibial tubercle–trochlear groove distance, which did not reach statistical significance.
Trochlear dysplasia has typically been identified on the basis of trochlear sulcus depth, femoral sulcus angle, and lateral trochlear inclination [9, 16, 32]. A shallow trochlear sulcus predisposes to lateral patellar subluxation [4, 32] and therefore might be expected to predispose to increased patellar friction over the lateral femoral condyle. Our data, although not reaching statistical significance, did suggest a trend toward the presence of superolateral fat pad edema and trochlear morphology, specifically a shallower sulcus depth and increased femoral sulcus angle. The lack of statistical significance may reflect insufficient study power because the absolute values of measurements for sulcus depth were small, and differences would therefore be difficult to discern. Furthermore, it has been shown that patients with anterior knee pain of undetermined cause show higher rates of trochlear dysplasia [9]. Because our study population was composed of symptomatic patients, this bias could obscure an increase in femoral sulcus angle and decrease in sulcus depth among patients with superolateral Hoffa’s fat pad edema compared with asymptomatic individuals.
Although trochlear dysplasia is thought to be genetically determined, patellar morphology may be shaped more by the complex interplay between the patella and trochlea during early learning of ambulation. In fact, a shortened medial patellar facet (Wiberg types II and III) has been shown to be associated with dysplastic trochlea, patellofemoral disorders, and isolated patellofemoral arthritis [4, 18]. However, no significant association between superolateral Hoffa’s fat pad edema and a shortened medial patellar facet was observed in this study.
Several theories have been proposed to explain the cause of anterior knee pain and its association with patellofemoral maltracking and impingement disorders. One possible mechanism involves repeated impaction of the medial patellar facet on the femur due to increased medial laxity. The resulting subchondral bone damage and associated synovial irritation or retinacular injury may contribute to pain [2]. Immunohistochemical findings of significantly higher substance-P nerve fibers in the fat pads of patients with anterior knee pain compared with control subjects suggests that pain may actually originate in the fat pad itself [33]. In this vein, it has also been postulated that impingement of the suprapatellar pouch, manifesting as quadriceps fat pad edema or enlargement, contributes to pain in some patients [34]. However, the lack of any significant associations between quadriceps fat pad abnormalities and various morphologic indicators of potential patellar maltracking or impingement in these studies provides important context in which to interpret our findings with respect to superolateral Hoffa’s fat pad edema.
Several study limitations should be considered. First, this was a relatively small retrospective study, and readers could not practicably be blinded to the presence of Hoffa’s edema while assessing patellofemoral morphology. Second, no true control group of asymptomatic patients was included. Thus, true differences in patients with superolateral Hoffa’s fat pad edema and normal control subjects may be even larger than those observed here because morphologic measurements in patients without edema may nonetheless be skewed. Third, we only assessed bony morphology without respect to the cartilaginous contour, which has been shown to differ from that of the underlying bone [35]. This choice was guided by precedents set in previous studies for anatomic measurements of the patellofemoral joint [11, 16, 17]. Fourth, the level of clinical detail supplied in the MRI requisition of this group of patients was not sufficient to allow subcategorization of patients with anterior versus more generalized knee pain. Nonetheless, we believe our results remain clinically important because subclinical patellofemoral tracking disorders may yet prove to be important risk factors for development of osteoarthritis in longer-term studies. Finally, as described by Chung et al. [13], as a result of the presence of patella alta in several cases, the precise relationship of the patella and trochlea was difficult to evaluate on axial images at specified levels (e.g., physeal line or 3 cm above the joint line). In these instances, the next highest slice depicting the patella was used. Future work could more quantitatively assess fat pad hypertrophy or T2 signal hyperintensity and include evaluation of the patellar and femoral cartilage. In addition, because the relationships between the patella and femur change with increasing degrees of knee flexion [10, 36], dynamic–kinematic MRI studies on patients with Hoffa’s edema may further elucidate its pathophysiology.
In conclusion, our results indicate that edema in the superolateral aspect of Hoffa’s fat pad may be an important indicator of patellofemoral malalignment, as evidenced by a small but statistically significant increase in the patellar tendon–patellar length ratio and trends toward increased lateral patellar tilt and a shallower trochlear sulcus compared with those without edema. We postulate that these factors positively influence excessive friction or pressure of the lateral patellar facet over the lateral femoral condyle, resulting in edema in the intervening superolateral portion of Hoffa’s fat pad. Such a mechanism may be an underappreciated cause of anterior knee pain in younger patients referred for MRI.
Fig. 3.
Method for determining patellar translation. Distance between parallel lines is drawn on axial image (3 cm above joint line) from medial edge of patella (dashed line) through most anterior point of medial condyle (solid line). Lines are perpendicular to tangent line through posterior femoral condyles. Normal distance is < 2 mm [11].
Fig. 4.
Methods for determining sulcus angle and sulcus depth.
A, On axial image 3 cm above joint line, sulcus angle is measured between lines paralleling bony cortex of femoral trochlea; normal femoral sulcus angle < 144° [11].
B, On same image, sulcus depth is determined by vertical distance (solid line) between deepest point of sulcus and line tangent to anterior-most point of femoral condyles (dashed line). Normal sulcus depth is ≥ 3 mm [16].
Fig. 5.
Method for determining lateral patellofemoral angle. On axial image 3 cm above joint line, angle is measured between line parallel to bony lateral patellar facet and line tangent to the anterior condyles. Normal patellofemoral angle ≥ 8° [11].
Fig. 8.
49-year-old woman with knee pain.
A and B, Sagittal (A) and axial intermediate-weighted (B) MR images with fat saturation show slightly more subtle edema (arrow) in superolateral Hoffa’s fat pad.
Acknowledgment
The authors thank Jiangxia Wang for her assistance with statistical analysis.
Supported by grant number 1T32EB006351 from the National Institutes of Health (NIH). The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- 1.Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population: a two-year prospective study. Am J Sports Med. 2000;28:480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 2.Biedert RM, Sanchis-Alfonso V. Sources of anterior knee pain. Clin Sports Med. 2002;21:335–347. doi: 10.1016/s0278-5919(02)00026-1. vii. [DOI] [PubMed] [Google Scholar]
- 3.Hungerford DS, Barry M. Biomechanics of the patellofemoral joint. Clin Orthop Relat Res. 1979:9–15. [PubMed] [Google Scholar]
- 4.Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM. Surgical biomechanics of the patellofemoral joint. Arthroscopy. 2007;23:542–553. doi: 10.1016/j.arthro.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Post WR, Teitge R, Amis A. Patellofemoral malalignment: looking beyond the viewbox. Clin Sports Med. 2002;21:521–546. doi: 10.1016/s0278-5919(02)00011-x. x. [DOI] [PubMed] [Google Scholar]
- 6.Brossmann J, Muhle C, Schröder C, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187:205–212. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- 7.Wittstein JR, Bartlett EC, Easterbrook J, Byrd JC. Magnetic resonance imaging evaluation of patellofemoral malalignment. Arthroscopy. 2006;22:643–649. doi: 10.1016/j.arthro.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Laurin CA, Lévesque HP, Dussault R, Labelle H, Peides JP. The abnormal lateral patellofemoral angle: a diagnostic roentgenographic sign of recurrent patellar subluxation. J Bone Joint Surg Am. 1978;60:55–60. [PubMed] [Google Scholar]
- 9.Keser S, Savranlar A, Bayar A, Ege A, Turhan E. Is there a relationship between anterior knee pain and femoral trochlear dysplasia? Assessment of lateral trochlear inclination by magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2008;16:911–915. doi: 10.1007/s00167-008-0571-5. [DOI] [PubMed] [Google Scholar]
- 10.McNally EG, Ostlere SJ, Pal C, Phillips A, Reid H, Dodd C. Assessment of patellar maltracking using combined static and dynamic MRI. Eur Radiol. 2000;10:1051–1055. doi: 10.1007/s003300000358. [DOI] [PubMed] [Google Scholar]
- Chhabra A, Subhawong TK, Carrino JA. A systematised MRI approach to evaluating the patellofemoral joint. [Accessed July 9, 2010];Skeletal Radiol. doi: 10.1007/s00256-010-0909-1. [Epub 2010 Mar 10] www.ncbi.nlm.nih.gov/pubmed/20217407. [DOI] [PMC free article] [PubMed]
- 12.Kalichman L, Zhang Y, Niu J, et al. The association between patellar alignment and patellofemoral joint osteoarthritis features: an MRI study. Rheumatology (Oxford) 2007;46:1303–1308. doi: 10.1093/rheumatology/kem095. [DOI] [PubMed] [Google Scholar]
- 13.Chung CB, Skaf A, Roger B, Campos J, Stump X, Resnick D. Patellar tendon-lateral femoral condyle friction syndrome: MR imaging in 42 patients. Skeletal Radiol. 2001;30:694–697. doi: 10.1007/s002560100409. [DOI] [PubMed] [Google Scholar]
- 14.Saddik D, McNally EG, Richardson M. MRI of Hoffa’s fat pad. Skeletal Radiol. 2004;33:433–444. doi: 10.1007/s00256-003-0724-z. [DOI] [PubMed] [Google Scholar]
- 15.Miller TT, Staron RB, Feldman F. Patellar height on sagittal MR imaging of the knee. AJR. 1996;167:339–341. doi: 10.2214/ajr.167.2.8686598. [DOI] [PubMed] [Google Scholar]
- 16.Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216:858–864. doi: 10.1148/radiology.216.3.r00se38858. [DOI] [PubMed] [Google Scholar]
- 17.Katchburian MV, Bull AM, Shih YF, Heatley FW, Amis AA. Measurement of patellar tracking: assessment and analysis of the literature. Clin Orthop Relat Res. 2003:241–259. doi: 10.1097/01.blo.0000068767.86536.9a. [DOI] [PubMed] [Google Scholar]
- 18.Fucentese SF, von Roll A, Koch PP, Epari DR, Fuchs B, Schottle PB. The patella morphology in trochlear dysplasia: a comparative MRI study. Knee. 2006;13:145–150. doi: 10.1016/j.knee.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Bohnsack M, Hurschler C, Demirtas T, Rühmann O, Stukenborg-Colsman C, Wirth CJ. Infrapatellar fat pad pressure and volume changes of the anterior compartment during knee motion: possible clinical consequences to the anterior knee pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2005;13:135–141. doi: 10.1007/s00167-004-0561-1. [DOI] [PubMed] [Google Scholar]
- 20.Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. RadioGraphics. 1997;17:675–691. doi: 10.1148/radiographics.17.3.9153705. [DOI] [PubMed] [Google Scholar]
- 21.Schweitzer ME, Falk A, Pathria M, Brahme S, Hodler J, Resnick D. MR imaging of the knee: can changes in the intracapsular fat pads be used as a sign of synovial proliferation in the presence of an effusion? AJR. 1993;160:823–826. doi: 10.2214/ajr.160.4.8456672. [DOI] [PubMed] [Google Scholar]
- 22.Hoffa A. The influence of adipose tissue with regard to pathology of the knee joint. JAMA. 1904;43:795–796. [Google Scholar]
- 23.Csintalan RP, Schulz MM, Woo J, McMahon PJ, Lee TQ. Gender differences in patellofemoral joint biomechanics. Clin Orthop Relat Res. 2002;402:260–269. doi: 10.1097/00003086-200209000-00026. [DOI] [PubMed] [Google Scholar]
- 24.Simmons E, Cameron JC. Patella alta and recurrent dislocation of the patella. Clin Orthop Relat Res. 1992:265–269. [PubMed] [Google Scholar]
- 25.Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89:1749–1755. doi: 10.2106/JBJS.F.00508. [DOI] [PubMed] [Google Scholar]
- 26.Luyckx T, Didden K, Vandenneucker H, Labey L, Innocenti B, Bellemans J. Is there a biomechanical explanation for anterior knee pain in patients with patella alta? Influence of patellar height on patellofemoral contact force, contact area and contact pressure. J Bone Joint Surg Br. 2009;91:344–350. doi: 10.1302/0301-620X.91B3.21592. [DOI] [PubMed] [Google Scholar]
- 27.Arendt E. Anatomy and malalignment of the patellofemoral joint: its relation to patellofemoral arthrosis. Clin Orthop Relat Res. 2005:71–75. doi: 10.1097/01.blo.0000171543.60966.a6. [DOI] [PubMed] [Google Scholar]
- 28.Ali SA, Helmer R, Terk MR. Patella alta: lack of correlation between patellotrochlear cartilage congruence and commonly used patellar height ratios. AJR. 2009;193:1361–1366. doi: 10.2214/AJR.09.2729. [DOI] [PubMed] [Google Scholar]
- 29.Endo Y, Schweitzer ME, Bordalo-Rodrigues M, Rokito AS, Babb JS. MRI quantitative morphologic analysis of patellofemoral region: lack of correlation with chondromalacia patellae at surgery. AJR. 2007;189:1165–1168. doi: 10.2214/AJR.07.2236. [DOI] [PubMed] [Google Scholar]
- 30.Arendt EA, Fithian D, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21:499–519. doi: 10.1016/s0278-5919(02)00031-5. [DOI] [PubMed] [Google Scholar]
- 31.Caylor D, Fites R, Worrell TW. The relationship between quadriceps angle and anterior knee pain syndrome. J Orthop Sports Phys Ther. 1993;17:11–16. doi: 10.2519/jospt.1993.17.1.11. [DOI] [PubMed] [Google Scholar]
- 32.Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination—initial experience. Radiology. 2000;216:582–585. doi: 10.1148/radiology.216.2.r00au07582. [DOI] [PubMed] [Google Scholar]
- 33.Witoński D, Wagrowska-Danielewicz M. Distribution of substance-P nerve fibers in the knee joint in patients with anterior knee pain syndrome: a preliminary report. Knee Surg Sports Traumatol Arthrosc. 1999;7:177–183. doi: 10.1007/s001670050144. [DOI] [PubMed] [Google Scholar]
- 34.Roth C, Jacobson J, Jamadar D, Caoili E, Morag Y, Housner J. Quadriceps fat pad signal intensity and enlargement on MRI: prevalence and associated findings. AJR. 2004;182:1383–1387. doi: 10.2214/ajr.182.6.1821383. [DOI] [PubMed] [Google Scholar]
- 35.Stäubli HU, Dürrenmatt U, Porcellini B, Rauschning W. Anatomy and surface geometry of the patellofemoral joint in the axial plane. J Bone Joint Surg Br. 1999;81:452–458. doi: 10.1302/0301-620x.81b3.8758. [DOI] [PubMed] [Google Scholar]
- 36.MacIntyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88:2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]