Abstract
Tumors of salivary glands are uncommon and comprise of about 2%–4% of all head and neck tumors. About 75%–80% of these tumors are benign and include pleomorphic adenoma, monomorphic adenoma, oncocytoma, and papillary cystadenoma lymphomatosum. Mucoepidermoid carcinoma is the most common malignant tumor of salivary glands, representing 5–10% of all salivary gland tumors. Although known to be metastatic to local lymph nodes, distant metastases are rare (especially, with low and intermediate grade tumors). Histologic grade and the expression of various mucin glycoproteins are useful prognostic indicators. We present a case of mucoepidermoid carcinoma of parotid gland origin with distant metastases which is an uncommon occurrence with intermediate grade tumors. Also, this is the first reported case of humoral hypercalcemia of malignancy secondary to mucoepidermoid carcinoma.
Keywords: mucoepidermoid carcinoma, salivary gland tumors, humoral hypercalcemia of malignancy
Case
A 74 year old man presented with an enlarging painless left posterior parotid mass over a 4 month period. The patient had a history of coronary artery disease, acute pancreatitis, and benign prostate enlargement. He denied weight loss, fever, chills, dysphagia, dysphonia, facial numbness or paresis. The physical exam revealed a 3 × 4 cm left posterior rubbery fixed mass at the angle of the mandible without palpable lymphadenopathy. The neurological exam was negative for involvement of the cranial nerves.
Magnetic resonance imaging (MRI) of the neck was significant for a 3 × 2.3 × 2.7 cm left parotid mass involving the superficial and deep lobes of the gland with slight displacement of the submandibular vein, and without regional or distant lymphadenopathy. A fine needle aspiration (FNA) biopsy of the mass revealed epidermoid and mucous secreting cells. Subsequently, the patient had a deep lobe parotidectomy followed by immediate reconstruction with a sternocleidomastoid flap. The pathology report was diagnostic of an intermediate grade mucoepidermoid carcinoma of the salivary gland with clear margins; the clinical stage was pT2pN0pMx.
The patient received adjuvant radiotherapy delivered 5 days a week for 7 weeks at 180cGy per day. The patient was followed at the oncology clinic at 3 month intervals. Regular imaging with CT scan of the neck was done every 6 months without evidence of recurrence.
Thirty months postoperatively, the patient presented to the hospital with severe generalized weakness, decreased appetite, weight loss, and change in mental status. Laboratory evaluation revealed corrected calcium of 15.1 mg/dl, creatinine of 1.9 mg/dl, intact PTH of 3pg/ml, PTHrp of 11.1pg/ml, without monoclonal protein on immunofixation.
CT scan of the head, chest, abdomen and pelvis revealed a large heterogeneous mass in the left lobe of the liver measuring approximately 10.6 cm × 9.9 cm, with multiple smaller satellite lesions throughout the liver measuring up to 1.7 cm. A 1.9 × 1.6 cm right lower para esophageal lymph node adjacent to a hiatal hernia and a 1 cm right para tracheal lymph node were also found.
A CT guided needle biopsy of the liver mass was histologically similar to the parotid mass with the same immunohistochemical features including positive GCDFP-15. The transbronchial needle biopsy of the right para tracheal lymph node was negative for malignant cells. The patient was discharged after treatment with intra-venous pamidronate and fluids. The corrected calcium at discharge was 11.5 mg/dl.
The patient’s symptoms as well as the hypercalcemia resolved after 4 cycles of chemotherapy with carboplatin (AUC5) and paclitaxel (175 mg/m2) given every three weeks. A PET scan confirmed a partial response to the chemotherapy but revealed a level two 1 cm right cervical lymph node (SUV 4.3) that had not been seen on previous CT scans. The right para tracheal and para esophageal lymph nodes were unchanged and were not FDG avid. The liver mass decreased to 7 × 8.5 cm. Another CT scan of the abdomen and pelvis after the 6th cycle of chemotherapy revealed a decrease in the liver mass to 6.8 × 6.1 cm.
After the 6th cycle of chemotherapy, the patient developed grade IV peripheral neuropathy and as a result, paclitaxel was discontinued. After the 7th cycle of carboplatin, the patient developed thrombocytopenia necessitating withdrawal of the drug. Eight weeks later the patient was readmitted to the hospital for malignant hypercalcemia with corrected calcium of 16.4 mg/dl. A CT scan of the abdomen and pelvis revealed further progression of the liver mass to 14.2 × 13 cm. After discussion with the patient’s family, it was decided to discontinue any further disease-directed treatment and the patient was put under hospice care.
Discussion
Mucoepidermoid carcinoma is one of the most common malignant tumors of salivary glands, representing 5%–10% of all salivary gland tumors. However, these tumors are also known to occur in lips, tongue, and buccal mucosa.1 Although known to be metastatic to local lymph nodes, distant metastases are rare (especially, with low and intermediate grade tumors).
Histologic grading has been shown to be of prognostic significance in these tumors, but there has been a lack of consensus about a standard grading system. Nevertheless, grading is based on various factors including proportion of different cell types, nuclear to cytoplasmic ratio, presence of multiple nuclei, hyperchromatism, mitotic rate, anaplasia characterized by cellular and nuclear pleomorphism, proportion of cystic spaces compared to solid areas, necrosis, neural invasion, vascular infiltration, and tumor size.2,3 Among these, the features that correlate with poor outcomes are 4 or more mitotic figures per ten high power fields, necrosis, anaplasia, neural involvement, and a cystic component of less than twenty percent.
The histologic grade usually correlates well with prognosis, as non-high grade tumors rarely metastasize. In the rare instances when low and intermediate grade tumors metastasize, they are more likely to be of minor salivary gland origin.4,5 Our case is an atypical one since intermediate grade MEC’s originating from parotid glands uncommonly metastasize distantly.
The diagnosis of metastatic disease from salivary glands was based on expression of GCDFP-15 in both the primary tumor and the metastatic lesions. GCDPF-15 is a marker of glandular differentiation and is associated with apocrine secretion. Immunohistchemically this glycoprotein has been identified in apocrine cells of breast and skin, parotid glands, and sub-mucosal bronchial glands.6 Among the tumors of salivary gland origin, 76% of the benign lesions vs. 28% of the malignant ones stained positively for the protein. In another study, GCDFP-15 was found to be positive in 40% cases of mucoepidermoid carcinoma.7
Evaluating the origin of meastatic disease could be difficult and confusing in many cases because of the presence of concomitant cancers. In our case, although the origin of metastatic disease was considered to be of the salivary gland origin, the chance of having a second malignancy could not be completely ruled out. Mucke et al. have suggested the role of endoscopy and bronchoscopy at the time of initial staging of salivary gland tumors.8 The role of bronchoscopy was significant in the detection of concomitant malignancies. 6 out of 95 patients were identified to have malignancies in the lung with 4 being carcinomas of lung and 2 represented metastases from the salivary gland tumors.
The expression of mucin glycoproteins on mucoepidermoid carcinoma has been evaluated in various studies. MUC5 AC in high grade MEC’s is helpful in differentiating them from squamous cell carcinomas, MUC4 is associated with better tumor differentiation and better prognosis, and the expression of MUC1 is related to tumor progression and worse prognosis.
Hypercalcemia has been reported to occur in 20–30 percent of cases of cancer at some point in the disease. In 80% of these, it is mediated by the secretion of PTHrP by the tumor cells and is termed as Humoral Hypercalcemia of Malignancy (HHM).9 It is associated with various squamous cell, endometrial, breast and renal cancers among others. To our knowledge, this is the first reported case of humoral hyeprcalcemia associated with mucoepidermoid carcinoma. The development of hypercalcemia in cancer patients signifies a pre-terminal event in the disease course, as it was in our patient. According to one study, 50% of cancer patients with hypercalcemia died within 30 days of developing high calcium levels.10
This case emphasizes the importance of the development of a standard grading system to better characterize mucoepidermoid carcinomas. The importance of various immunohistochemical markers needs to be better defined, and further studies are needed to evaluate their diagnostic and prognostic significance.
Figure 1.
MRI of the neck done on the initial presentation showing a 3 cm by 2.3 cm by 2.7 cm left parotid mass, involving the superficial and deep lobes of the left parotid gland.
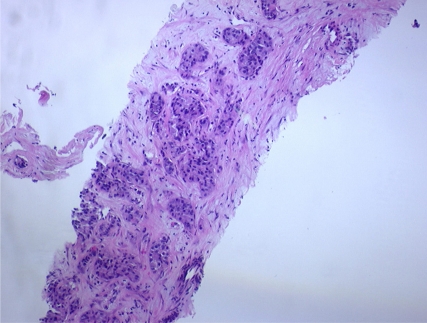
Figure 2.
CT abdomen showing a 10.6 cm by 9.8 cm heterogenous mass in the liver.
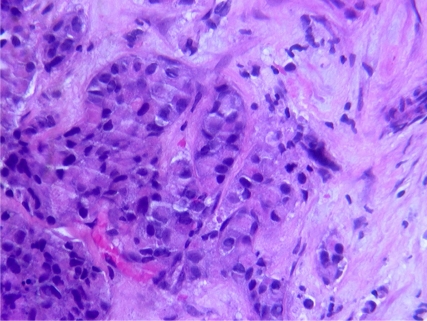
Figure 3.
CT guided FNA biopsy specimen showing poorly differentiated squamous carcinoma with rare neuroendocrine differentiation.
Figure 4.
CT guided FNA cytology smears positive for poorly differentiated squamous carcinoma with rare neuroendocrine differentiation.
Footnotes
Disclosure
This manuscript has been read and approved by all authors. This paper is unique and is not under consideration by any other publication and has not been published elsewhere. The authors and peer reviewers of this paper report no conflicts of interest. The authors confirm that they have permission to reproduce any copyrighted material. Written informed consent was obtained from the patient for the publication of this case report.
Authors’ Contributions
MP was the major contributor to the discussion section of this manuscript, conducted literature review and participated in the manuscript revisions. NA was the major contributor to the Case Presentation section of the manuscript and was involved in direct patient care. FF and PF were the attending physicians on the case and participated in the manuscript revisions.
References
- 1.Pulmonary Mucoepidermoid Carcinoma With Prominent Tumor-Associated Lymphoid Proliferation. Shilo K, Foss RD, Franks TJ, Deperalta-Venturina M, Travis WD. Am J Surg Pathol. 2005 Mar;29(3):407–11. doi: 10.1097/01.pas.0000151616.14598.e7. [DOI] [PubMed] [Google Scholar]
- 2.Auclair PL, Goode RK, Ellis GL. Mucoepidermoid carcinoma of intraoral salivary glands: evaluation and application of grading criteria in 143 cases. Cancer. 1992;69:2021–30. doi: 10.1002/1097-0142(19920415)69:8<2021::aid-cncr2820690803>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 3.Batsakis JG, Luna MA. Histopathologic grading of salivary gland neoplasms: I. mucoepidermoid carcinomas. Ann Otol Rhinol Laryngol. 1990;99(10 Pt 1):835–8. doi: 10.1177/000348949009901015. [DOI] [PubMed] [Google Scholar]
- 4.Clode AL, et al. Mucoepidermoid carcinoma of the salivary glands: a reappraisal of the influence of tumor differentiation on prognosis. J Surg Oncol. 1991;46:100–6. doi: 10.1002/jso.2930460207. [DOI] [PubMed] [Google Scholar]
- 5.Evans HL. Mucoepidermoid carcinoma of salivary glands: a study of 69 cases with special attention to histologic grading. Am J Clin Pathol. 1984;81:696–701. doi: 10.1093/ajcp/81.6.696. [DOI] [PubMed] [Google Scholar]
- 6.Gross cystic disease fluid protein-15 in salivary gland tumors. Arch Pathol Lab Med. 1991 Feb;115(2):158–63. [PubMed] [Google Scholar]
- 7.MUC1, MUC2, MUC4, and MUC5AC expression in salivary gland mucoepidermoid carcinoma: diagnostic and prognostic implications. Handra-Luca A, Lamas G, Bertrand JC, Fouret P. Am J Surg Pathol. 2005 Jul;29(7):881–9. doi: 10.1097/01.pas.0000159103.95360.e8. [DOI] [PubMed] [Google Scholar]
- 8.Mücke T, Kesting MR, Hohlweg-Majert B, Hölzle F, Wolff KD. The role of bronchoscopy and gastroscopy in intra-oral minor salivary gland carcinomas at initial staging. British Journal of Oral and Maxillofacial Surgery. 2009;47:608–11. doi: 10.1016/j.bjoms.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Stewart AF. Hypercalcemia associated with cancer. N Engl J Med. 2005;352:373–9. doi: 10.1056/NEJMcp042806. [DOI] [PubMed] [Google Scholar]
- 10.Horwitz MJ, Stewart AF. Humoral hypercalcemia of malignancy. In: Favus MF, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. 5th ed. Washington D.C.: American Society for Bone and Mineral Research; 2003. pp. 246–50. [Google Scholar]