Abstract
This report demonstrates the feasibility of an elective ovariosalpingohysterectomy by natural transluminal endoscopic surgery (NOTES) hybrid technique in a dog. A 5-mm abdominal cannula was used in combination with a 10-mm cannula (vaginal access). The patient’s quick recovery and the absence of complications are indicative of the effectiveness of this surgery.
Résumé
Ovariohystérectomie chez un chien à l’aide d’une technique NOTES hybride. Ce rapport démontre la faisabilité d’une ovariosalpingohystérectomie non urgente à l’aide d’une technique hybride de chirurgie endoscopique transluminale par voies naturelle (NOTES) chez un chien. Une canule abdominale de 5 mm a été utilisée en combinaison avec une canule de 10 mm (accès vaginal). Le rétablissement rapide du patient et l’absence de complications sont indicateurs de l’efficacité de cette chirurgie.
(Traduit par Isabelle Vallières)
Ovariosalpingohysterectomy (OVH) in dogs using minimally invasive surgery has been described since the 1990s (1). Several techniques have been developed using laparoscopic access or video-assisted surgery, allowing for elective surgeries and for the treatment of various reproductive disorders (2), including ovarian remnant syndrome (3), pyometra (4,5) and vaginal prolapse (6). Recently, laparoscopic access with 2 to 3 cannulas (7,8) or using a single cannula in video-assisted surgery (9) has been reported.
Natural transluminal endoscopic surgery (NOTES) encompasses an array of surgical procedures that utilize natural orifices for various surgical steps, with or without the use of laparoscopic access (10,11). This new type of surgery is a current trend in human medicine, and has been described for appendectomy (12), cholecystectomies (13), and nephrectomies (14). There are several studies on animals that confirm its feasibility and safety in surgeries such as nephrectomy, cholecystectomy, gastrojejunostomy, lymphadenectomy and pancreatectomy, using gastric, colonic, and/or vaginal access with a flexible endoscope (15–19).
Nevertheless, the use of NOTES in dogs is quite recent, and vaginal access for this type of surgery is uncommon. Less invasive procedures are preferred for video-endoscopic OVH in dogs, since the removal of the uterus and ovaries is the most widespread surgery performed in veterinary medicine (20).
The aim of the present case report is to describe a new technique that uses transvaginal access with a rigid endoscope, combined with laparoscopic surgery via a single 5-mm cannula for elective OVH in a dog.
Case description
The patient weighed 9 kg and was healthy on clinical and hematological examinations. When a decision was made to send the dog to an animal shelter and to put it up for adoption, minimally invasive OVH was then carried out. Premedication consisted of the combination of acepromazine maleate (Acepran 10%; Rhosifarma, Camboci-SP, Brazil) and morphine sulfate (Dimorf; Cristália, Itapira-SP, Brazil), 0.05 mg/kg body weight (BW), IV and 0.5 mg/kg BW, IV, respectively. Anesthesia was induced using diazepam (União Química Farmacêutica Nacional, Porto Alegre-RS, Brazil) plus ketamine (Ketamin-S; Cristália), 0.5 mg/kg BW, IV and 5 mg/kg BW, IV, respectively. Epidural anesthesia with lidocaine chlorhydrate was administered (Xylestesin; Cristália), in conjunction with morphine sulfate and bupivacaine (Neocaina; Cristália), 4 mg/kg BW, 0.01 mg/kg BW and 0.18 mg/kg BW, respectively. Anesthesia was maintained with isoflurane (Cristália) in 100% oxygen.
The animal was placed in dorsal recumbency, with its head turned towards the rack that contained the equipment for the video-assisted surgery. An intravesical urethral catheter #6 was kept in place throughout surgery, and the patient received ampicillin sodium (Amplocilin; Cellofarm, Serra-ES, Brazil) and enrofloxacin (Flotril 2.5%; Schering-Plough, Rio de Janeiro-RJ, Brazil) at the respective IV doses of 44.4 mg/kg BW and 5.5 mg/kg BW. The vaginal mucosa was rinsed with 1% polyvinyl pyrrolidone (Riodine; Indústria Farmacêutica Rioquímico, São José do Rio Preto-SP, Brazil).
A single 5-mm abdominal cannula was inserted into the right lateral abdominal wall using the open approach, 2 cm laterally and 2 cm caudally to the third nipple. A skin incision of 1 cm was made. The abdominal cavity was insufflated with CO2 at the rate of 2 L/min until a pressure of 12 mmHg was achieved. A zero-degree 5-mm rigid endoscope (Astus Medical, Sao Paulo, SP, Brazil) was introduced through this cannula, allowing for the visualization of the left uterine horn. A 10-mm cannula was inserted through the vagina, and the obturator was guided towards the ventral surface of the vagina, caudally to the cervix. Given the long distance between the vulva and the site to be penetrated through the vaginal wall, it was not possible to penetrate it with the cannula. Therefore, a 4.5-mm Steinmann pin (Ortossíntese, São Paulo-SP, Brazil) was inserted through the cannula. After an incision was made in the vaginal wall, the endoscope was repositioned towards the vaginal access, which was fixed to the vulva using a size 0 nylon monofilament thread (Nylon; Shalon, São Luiz dos Montes Belos-GO, Brazil).
A transparietal suture (passed percutaneously through the abdominal wall) with the same type of thread was made using a 4-cm needle, which kept the uterine horn fixed to the wall by the external grasping of the thread tips with a Halsted clamp. The animal’s left forelimb was rotated to the right, and fastened together with the right limb on the operating table, in order to expose the left ovary and its ligaments and vessels. The endoscope was moved from the vaginal access to the abdominal cannula, and the suspensory ligament was ruptured with a Kelly clamp inserted through the vaginal cannula. After that, the mesovarium was dissected, in order to isolate the ovarian vessels for the placement of the titanium clip. Four titanium clips (SLS-clip; Vitalitec, Domalain, France) were placed, and the mesovarium was sectioned with Metzembaum scissors between the 2 proximal clips and the 2 distal ones. A gauze swab was used to wipe the blood shed from the section of the ovarian vessels.
After checking for hemostasis, the animal was rotated to the left side by traction of the right forelimb, as previously described. With the endoscope positioned at the right lateral access, the suspensory ligament was ruptured with a grasping forceps inserted through the vaginal access. Thereafter, the right ovary was fixed to the lateral abdominal wall with a transparietal suture as previously described. Likewise, its corresponding ovarian vessels were also ligated with 4 titanium clips and sectioned (Figure 1). The left suspensory ligament was held with a grasper and pulled out of the cavity through the vaginal wound, thus exposing the ovary and part of the right uterine horn. The uterine horns were then grasped with a conventional DeBakey forceps and totally exposed through the vaginal access, producing a vaginal hernia (Figure 2). Then the hemostasis of the uterine vessels and of the uterine body was achieved by the conventional access using 3 hemostatic forceps. Two modified Halsted transfixation ligatures were applied to the uterine body, the vaginal incision was closed with an interlocking Ford suture with 0 polyglactin 910 in both stages (Vicryl; Ethicon, São José dos Campos-SP, Brazil). The uterus was sectioned cranial to the ligations, and repositioned into the pelvic cavity.
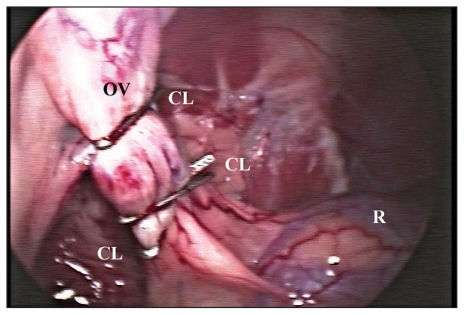
Figure 1.
Endoscopic visualization of the right mesovarium after the placement of titanium clips (CL) through the vaginal access for OVH, using NOTES-assisted laparoscopic surgery. R—right kidney; OV—right ovarian vessels.
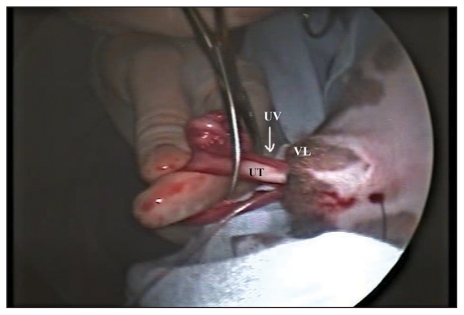
Figure 2.
Exteriorization of the uterus (UT) and ovaries for hemostasis of the uterine vessels (UV), with the patient in recumbent position. VL—vulva.
The peritoneal cavity was deflated and the abdominal incision was sutured at the subcutaneous level using the same absorbable stitch in a cross mattress pattern. The skin was sutured with a 5-0 nylon monofilament thread (Nylon; Shalon, São Luiz dos Montes Belos-GO, Brazil) using a simple interrupted pattern. Ketoprofen (Ketofen 10%; Mérial, Paulínia-SP, Brazil), 1.1 mg/kg BW, SC and tramadol (Tramal; Cristália), 1.8 mg/kg BW, SC were given at the end of the procedure. Tramadol was administered subcutaneously for 5 d during the postoperative period, ampicillin sodium was given subcutaneously, 3 times a day for 7 d, and the abdominal wound was cleansed every day with 0.9% sodium chloride.
The surgical procedure lasted 94 min; 1.6 L of CO2 was necessary to achieve the preset intra-abdominal pressure, and 51 L were required for the entire surgery. The only intraoperative complication consisted of subcutaneous emphysema due to gas leak through the abdominal access, caused by partial displacement of the 5-mm cannula during surgery. This problem was managed with gas drainage through the entry incision before its closure and by additional drainage of the subcutaneous tissue with a 40 × 12 mm needle. No gas was observed on the second postoperative day. No late or immediate postoperative complications developed. Three hours after surgery, the animal had a slight ataxic gait, still under the effect of anesthesia. By then, the animal had already urinated and defecated, showing no signs of discomfort during defecation, and had eaten kibble. Nine days afterwards, the suture was removed, and the animal showed primary healing.
The histological analysis of the uterus and ovary revealed slight to moderate multifocal hemorrhage, in addition to slight to moderate multifocal endometrial hyperplasia and occasional presence of hemorrhagic content in the uterine lumen. In the ovaries, moderate to severe multifocal hemorrhage was detected in the serous membrane.
After 110 postoperative days, the patient was submitted to laparoscopy in order to assess the peritoneal cavity and the healing of the vaginal wound. Three cannulas were used, 2 10-mm cannulas positioned in the preumbilical ventral midline and in the right abdominal wall, and 1 5-mm cannula, inserted into the left abdominal wall. The cannulas were placed in a triangular pattern; the 10-mm and zero-degree endoscope was inserted through the ventral midline, and graspers or Kelly clamps were inserted through the other cannulas. After examination, the larger surgical wounds were sutured with a cross mattress using polyglactin 910 size 2-0, and all accesses were closed at the subcutaneous level with the same suture material. A simple interrupted pattern with 5-0 monofilament nylon thread was used for all skin sutures.
Postoperative laparoscopy was performed in 27 min without any intraoperative or postoperative complications. We found an adhesion between the greater omentum and the left remaining mesovarium.
Discussion
Repositioning of the forelimbs during surgery, with rotation of the trunk, previously used by Silva (21) allowed for adequate exposure of the kidney and ovary on the rotated side, since the abdominal viscera were widely displaced medially. After that, the exposure of the suspensory ligament for rupture was facilitated. As indicated in conventional surgery (20), the authors perform the rupture of the suspensory ligament in order to expose the ovarian vessels, since this maneuver could facilitate the transparietal suture to be applied to the ovarian ligament and expose the ovarian vessels, which is essential for the accurate placement of the titanium clips. After the manipulation of both the uterine horn and the right ovary, it became evident that the first transparietal suture could have been avoided as the right suspensory ligament, more cranial than the contralateral one, was promptly accessed.
The surgery was too time-consuming, but this was the first procedure in which this access was used. Notwithstanding, it was possible to observe that the proposed technique was not complex and proved to be safe and minimally invasive, which was confirmed by the patient’s quick recovery and by the results obtained in the postoperative period.
The repositioning of the rigid endoscope during exposure and hemostasis of the ovarian vessels was regarded as unnecessary after this new OVH approach was later tested in other animals (22). In those animals in which the laparoscope was kept at the ventral midline throughout surgery, it was possible to rupture the suspensory ligament and ligate the ovary for the placement of the transparietal suture by inserting a Kelly clamp directly through the vaginal access. This technical change rendered the procedure easier to perform and less time-consuming, since the vaginal access was used only for the positioning of the surgical instruments used for dieresis and hemostasis, and not to provide visualization of the cavity via the endoscope. Another important aspect described by those authors is that the use of the abdominal port directly in the ventral midline, and not in the muscle wall as in the present case, minimizes muscle injury and is associated with better esthetic outcomes, as the entry wound for the placement of the 5-mm cannula can be opened directly upon the umbilical scar, thus concealing the scar.
In conclusion, OVH by NOTES, combined with laparoscopy, with the placement of a 5-mm cannula into the muscle wall and a 10-mm cannula through the vaginal access, is feasible and appropriate for neutering dogs. CVJ
Footnotes
Reprints will not be available from the authors.
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Siegl VH, Böhn R, Ferguson J. Laparoskopische Ovariohysterektomie bei einem Hund. Wien Tierarztl Monatsschr. 1994;81:149–152. [Google Scholar]
- 2.Freeman LJ. Minimally invasive surgery of the reproductive system. In: Freeman LJ, editor. Veterinary Endosurgery. St Louis: Missouri Mosby; 1998. pp. 105–117. [Google Scholar]
- 3.Beck CA, Pippi NL, Raiser AG, et al. Ovariectomia laparoscópica em uma cadela com ovários remanescentes: Relato de caso. Medvep. 2004;2:15–19. [Google Scholar]
- 4.Minami S, Okamoto Y, Eguchi H, Kato K. Successful laparoscopy assisted ovariohysterectomy in two dogs with pyometra. J Vet Med Sci. 1997;59:845–879. doi: 10.1292/jvms.59.845. [DOI] [PubMed] [Google Scholar]
- 5.Brun MV, Oliveira RP, Barcellos HHA, et al. Tratamento de diferentes apresentações de piometra em cães por cirurgia laparoscópica ou video-assistida. Medvep. 2006;4:26–33. [Google Scholar]
- 6.Brun MV, Valle SF, Guimarães LD, Trindade AB, Bairros MC. Ovário-histerectomia laparoscópica no tratamento de prolapso vaginal em uma cadela. Proc Arq Bras Med Vet Zoo. 2006;35:60–61. [Google Scholar]
- 7.Austin B, Lanz OI, Hamilton SM, Broadstone RV, Martin RA. Laparoscopic ovariohysterectomy in nine dogs. J Am Anim Hosp Assoc. 2003;39:391–396. doi: 10.5326/0390391. [DOI] [PubMed] [Google Scholar]
- 8.Santos FR, Brun MV, Ataíde MW, et al. Ovariosalpingohisterectomia laparoscópica com dois portais em cães filhotes [CD ROM]. Proc 17a Mostra de Iniciação Científica da UPF; Passo Fundo, RS, Brazil. 2007. [Google Scholar]
- 9.Devitt CM, Cox RE, Hailey JJ. Duration, complications, stress, and pain of open ovariohysterectomy versus a simple method of laparoscopic-assisted ovariohysterectomy in dogs. J Am Vet Med Assoc. 2005;227:921–927. doi: 10.2460/javma.2005.227.921. [DOI] [PubMed] [Google Scholar]
- 10.Kavic MS. Natural orifice translumenal endoscopic surgery: “NOTES. JSLS. 2006;10:133–134. [PMC free article] [PubMed] [Google Scholar]
- 11.McGee MF, Rosen MJ, Marks J, et al. A primer on natural orifice transluminal endoscopic surgery: Building a new paradigm. Surg Innov. 2006;13:86–93. doi: 10.1177/1553350606290529. [DOI] [PubMed] [Google Scholar]
- 12.Hochberger J, Lamade W. Transgastric surgery in the abdomen: The dawn of a new era? Gastrointest Endosc. 2005;62:293–296. doi: 10.1016/j.gie.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Forgione A, Maggioni D, Sansonna F, et al. Transvaginal endoscopic cholecystectomy in human beings: Preliminary results. J Laparoendosc Adv Surg Tech Part A. 2008;18:345–351. doi: 10.1089/lap.2007.0203. [DOI] [PubMed] [Google Scholar]
- 14.Branco AW, Branco Filho AJ, Kondo W, et al. Hybrid transvaginal nephrectomy. Eur Urol. 2008;53:1290–1294. doi: 10.1016/j.eururo.2007.10.053. [DOI] [PubMed] [Google Scholar]
- 15.Simopoulos C, Kouklakis G, Zezos P, et al. Peroral transgastric endoscopic procedures in pigs: Feasibility, survival, questionings, and pitfalls. Surg Endosc. 2009;23:394–402. doi: 10.1007/s00464-008-9930-z. [DOI] [PubMed] [Google Scholar]
- 16.Cahill RA, Perretta S, Leroy J, Dallemagne B, Marescaux J. Lymphatic mapping and sentinel node biopsy in the colonic mesentery by natural orifice transluminal endoscopic surgery (NOTES) Ann Surg Oncol. 2008;15:2677–2683. doi: 10.1245/s10434-008-9952-8. [DOI] [PubMed] [Google Scholar]
- 17.Clayman RV, Box GN, Abraham JBA, et al. Transvaginal single-port NOTES nephrectomy: Initial laboratory experience. J Endourol. 2007;21:640–644. doi: 10.1089/end.2007.0145. [DOI] [PubMed] [Google Scholar]
- 18.Ryou M, Fong DG, Pai RD, Tavakkolizadeh A, Rattner DW, Thompson CC. Dual-port distal pancreatectomy using a prototype endoscope and endoscopic stapler: A natural orifice transluminal endoscopic surgery (NOTES) survival study in a porcine model. Endoscopy. 2007;39:881–887. doi: 10.1055/s-2007-966908. [DOI] [PubMed] [Google Scholar]
- 19.Pai RD, Fong DG, Bundga ME, Odze RD, Rattner DW, Thompson CC. Transcolonic endoscopic cholecystectomy: A NOTES survival study in a porcine model (with video) Gastrointest Endosc. 2006;64:428–434. doi: 10.1016/j.gie.2006.06.079. [DOI] [PubMed] [Google Scholar]
- 20.Wilson GP, Hayes HM. Ovário-histerectomia em candelas e gatas. In: Bojrab MJ, editor. Cirurgia dos pequenos animais. 2a ed. SãoPaulo: Rocca C0; 1986. pp. 365–369. [Google Scholar]
- 21.Silva MAM. MS Thesis. Goiânia: Universidade Federal de Goiás; 2007. Avaliação laparoscópica das aderências intraperitoneais pós-cirúrgicas de cadelas: Emprego de duas doses de solução de azul de metileno a 1% na profilaxia. [Google Scholar]
- 22.Brun MV, Silva MAM, Feranti JPS, et al. NOTES híbrida na realiza-ção de ovariosalpingohisterectomia em 12 cadelas. Proc 8º Congresso Brasileiro de Cirurgia e Anestesiologia Veterinária; 2008. [Google Scholar]