Abstract
Increased and early lumbopelvic motion during trunk and limb movements is thought to contribute to low back pain (LBP). Therefore, reducing lumbopelvic motion could be an important component of physical therapy treatment. Our purpose was to examine the effects of classification-specific physical therapy treatment (Specific) based on the Movement System Impairment (MSI) model and non-specific treatment (Non-Specific) on lumbopelvic movement patterns during hip rotation in people with chronic LBP. We hypothesized that following treatment people in the Specific group would display decreased lumbopelvic rotation and achieve more hip rotation before lumbopelvic rotation began. We hypothesized that people in the Non-Specific group would display no change in these variables. Kinematic data collected before and after treatment for hip lateral and medial rotation in prone were analyzed. The Specific group (N=16) demonstrated significantly decreased lumbopelvic rotation and achieved greater hip rotation before the onset of lumbopelvic rotation after treatment with both hip lateral and medial rotation. The Non-Specific group (N=16) demonstrated significantly increased lumbopelvic rotation and no change in hip rotation achieved before the onset of lumbopelvic rotation. People who received treatment specific to their MSI LBP classification displayed decreased and later lumbopelvic motion with hip rotation, whereas people who received generalized non-specific treatment did not.
Keywords: low back pain, lumbopelvic motion, classification, treatment
Introduction
Several authors have proposed that repeated lumbopelvic motion is a factor in the development and course of low back pain (LBP) (Adams et al., 2002; McGill, 1997; Sahrmann, 2002). Increased lumbopelvic motion, particularly early in the range of trunk and limb movements, has been associated with low back pain (LBP) during clinical movement tests and activities of daily living (Burnett et al., 2004; Esola et al., 1996; Luomajoki et al., 2008; McClure et al., 1997; Roussel et al., 2009; Shum et al., 2005). A relationship between LBP symptoms and lumbopelvic movement patterns displayed during the test of hip lateral rotation performed in prone in people with LBP has previously been established. In particular, early lumbopelvic motion during hip lateral rotation is associated with increased symptoms in people with LBP (Gombatto et al., 2006; Scholtes and Van Dillen, 2007). Furthermore, people with LBP demonstrate earlier and greater lumbopelvic rotation during hip lateral rotation compared to people without LBP (Scholtes et al., 2009).
Minimizing lumbopelvic motion during limb movements, such as lumbopelvic rotation during hip rotation, may be an important component of physical therapy treatment for many people with LBP. When movements such as hip lateral or medial rotation cause increased LBP symptoms, manually restricting lumbopelvic motion improves symptoms in the majority of people (Van Dillen et al., 2003a; Van Dillen et al., 2009). Specifically training people with LBP to minimize lumbopelvic motion in directions (e.g., rotation) that are associated with symptoms is a concept central to treatment based on the Movement System Impairment (MSI) model for LBP (Sahrmann, 2002). It has been previously demonstrated that people with LBP can be trained to minimize lumbopelvic motion during hip lateral rotation within a treatment session (Scholtes et al., 2010). However, it also appears that people with LBP may not be able to minimize lumbopelvic motion as well as people without LBP (Scholtes et al., 2010). It is possible that proprioceptive deficits identified in people with LBP (Brumagne et al., 2000; O'Sullivan et al., 2003) make it more difficult for them to first recognize and then limit lumbopelvic motion. Given these findings, it is unclear if people with LBP are able to limit lumbopelvic motion during limb movements outside of a single treatment session and without immediate verbal or tactile instruction to do so. Furthermore, it is unclear if individualized movement-specific instruction is required to produce these longer-term improvements in a person's lumbopelvic movement pattern. The effects of non-specific treatment strategies for LBP, including trunk and limb strengthening and stretching, on lumbopelvic movement patterns during limb movements are unknown.
The purpose of this study was to compare the effect of two physical therapy treatments on lumbopelvic movement patterns with hip lateral and medial rotation performed in prone in people with LBP. We hypothesized that, following treatment, people with LBP who received MSI-based classification-specific (Specific) treatment would improve their lumbopelvic movement pattern to a greater extent than people with LBP who received non-specific (Non-Specific) treatment. Improvement was defined either as decreased lumbopelvic motion or as later onset of lumbopelvic motion during hip lateral and medial rotation.
Methods
Subjects
The 32 subjects analyzed for this study were a subset from a larger randomized controlled clinical trial (N = 101) comparing the effectiveness of two physical therapy treatments for chronic LBP, as defined by Von Korff (1994). Equal numbers of subjects in each treatment condition were selected to be analyzed. The selection of subjects was performed by a member of the research team who was not blinded to treatment condition assignment. This person was blinded to all other data including kinematics. For each treatment condition, the data was stratified by LBP subgroup. Cases were then randomly chosen from each stratum to parallel the proportions of LBP subgroups in the overall sample.
Subjects enrolled in the clinical trial were between 18 and 60 years old, had a history of chronic LBP for at least 12 months, were experiencing their typical LBP symptoms but were not in an acute flare-up as defined by Von Korff (1994), and were able to stand and walk without assistance. People were excluded from the study if they had a history of spinal fracture or surgery, spinal deformity, disc herniation, pain or parasthesia below the knee, systemic inflammatory condition, or other serious medical condition. People were also excluded if they were pregnant, presented with a primary hip problem, displayed magnified symptom behavior (Waddell et al., 1980), were receiving worker's compensation or disability benefits, were involved in pending litigation for their LBP, or were referred from a specialized pain clinic. The testing protocol was approved by the University's Human Research Protection Office and all subjects provided written informed consent before participating in the study.
Laboratory and Clinical Procedures
At the pre-treatment laboratory visit, one of three physical therapists examined each subject in the clinical trial and classified him or her into a LBP subgroup according to a standardized examination based on the MSI model. The directions of early or increased lumbopelvic motion that were consistently displayed across examination tests and that were associated with symptoms were used to classify patients into LBP subgroups to direct treatment (Sahrmann, 2002; Van Dillen et al., 2003b). Each examining therapist had been trained to administer the standardized examination prior to participation in the study. Reliability of physical therapists performing examination items (Van Dillen et al., 1998) and of their ability to classify an individual's LBP problem based on the examination (Harris-Hayes and Van Dillen, 2009; Henry et al., 2009; Norton et al., 2004; Trudelle-Jackson et al., 2008) have been found to be acceptable. Ninety-eight percent of subjects in the overall sample were classified into either the Rotation or Rotation with Extension subgroups. Therefore, all subjects selected for the current study had been classified into one of these two subgroups. Both the Rotation and Rotation with Extension subgroups might be expected to demonstrate early and increased lumbopelvic motion and LBP symptoms with hip rotation. Subjects also completed a demographic and LBP history questionnaire (Deyo et al., 1994), a verbal numeric rating scale of symptoms (Downie et al., 1978; Jensen et al., 1994), the modified Oswestry Low Back Pain Disability Questionnaire (Fritz and Irrgang, 2001), and the Fear-Avoidance Beliefs Questionnaire (Waddell et al., 1993).
After the pre-treatment laboratory visit, all subjects in the clinical trial were randomly assigned to one of two physical therapy treatment conditions. A randomization scheme was prepared before the clinical trial began whereby the sample was stratified by LBP subgroup and subjects were assigned to a treatment condition based on a computer-generated list. Independent administrative personnel at the treatment sites were responsible for following the randomization scheme and assigning subjects to treatment conditions. Sixteen subjects in each treatment condition were included in the current study. The physical therapists performing the examination and laboratory measures were blinded to the subject's treatment condition. Treating therapists were different from those who performed the examination and laboratory data collection. Each subject participated in six treatment sessions administered weekly over a six week period. Subjects returned for the post-treatment laboratory visit approximately one week after completing their sixth treatment session. The standardized examination, self-report measures, and kinematic testing were repeated.
Treatment Conditions
Subjects in the Specific group received MSI-based classification-specific treatment that included 1) education regarding their specific LBP subgroup and specific directions of lumbopelvic motion and postures thought to be associated with their LBP symptoms, 2) training to minimize use of specific directions of lumbopelvic motion and postures associated with symptoms during activities of daily living, and 3) an individualized exercise program that included minimizing specific directions of lumbopelvic motion during trunk and limb movements that were symptom-provoking on examination. One of the exercises prescribed to subjects in the Specific group was hip lateral and medial rotation performed in prone, during which subjects were instructed to recruit their abdominal muscles and not let their pelvis move while rotating their leg. Subjects were allowed to place their hands on their pelvis to monitor pelvic motion. Subjects in the Non-Specific group received treatment components cited in the literature for people with chronic LBP, which included 1) general education regarding neutral spinal alignment, spinal anatomy, and the natural history of LBP, 2) training to maintain neutral spinal alignment during activities of daily living that are typically painful for people with LBP, and 3) an exercise program that emphasized increasing trunk and limb strength and flexibility (e.g., Friedrich et al., 1996; Friedrich et al., 1998; Mannion et al., 1999; Melnick et al., 1998; Moffett et al., 1999; Taimela et al., 2000; Torstensen et al., 1998). Both groups were encouraged to be active. Two physical therapists were trained to administer the Specific treatment. Four physical therapists, with no prior training in MSI-based treatment, were trained to administer the Non-Specific treatment. The Non-Specific therapists were blinded to the subject's LBP subgroup.
Kinematics
Kinematic data were collected for the tests of hip lateral and medial rotation at both the pre- and post-treatment laboratory visits. Each test was performed in prone with one knee flexed to 90°, beginning with the hip in neutral abduction/adduction and rotation. Subjects positioned their arms out to their sides in approximately 90° shoulder abduction. Subjects were instructed to either laterally or medially rotate the hip as far as possible and then return to the starting position. They were allowed to perform each movement at a self-selected speed and were given 10 seconds to complete the movement. One trial each was collected for both directions of hip rotation on both the left and right legs. Limb order was randomized. During the post-treatment laboratory collection, subjects were instructed to perform the movement according to their treating physical therapist's instructions or, if they had received no instructions, as they naturally would. They were not, however, allowed to alter the position of the test (i.e., they could not place their hands on their pelvis to monitor pelvic motion during the test).
A six-camera, three-dimensional motion capture system (EVaRT, Motion Analysis Corporation, Santa Rosa, CA, USA) was used to measure kinematics. Retro-reflective markers used in this analysis were on the following landmarks: 7 cm bilateral to the first sacral vertebra (S1), the lateral knee joint line, and the distal aspect of the lateral malleolus. The pelvic segment was defined by a vector between the S1 markers. The lower leg segment was defined by a vector between the markers on the lateral knee joint line and the distal aspect of the lateral malleolus (Figure 1). Data were collected at a sampling rate of 60 Hz. Data were initially filtered using a fourth-order, dual-pass, Butterworth filter with a cut-off frequency of 2.0 Hz. Initiation and termination of the pelvic and lower limb segment rotations in the transverse plane were determined from angular displacement and velocity data. Based on individual pelvic segment movement times, subject-specific filtering frequencies were then applied to the raw data (Winter, 2005).
Figure 1.
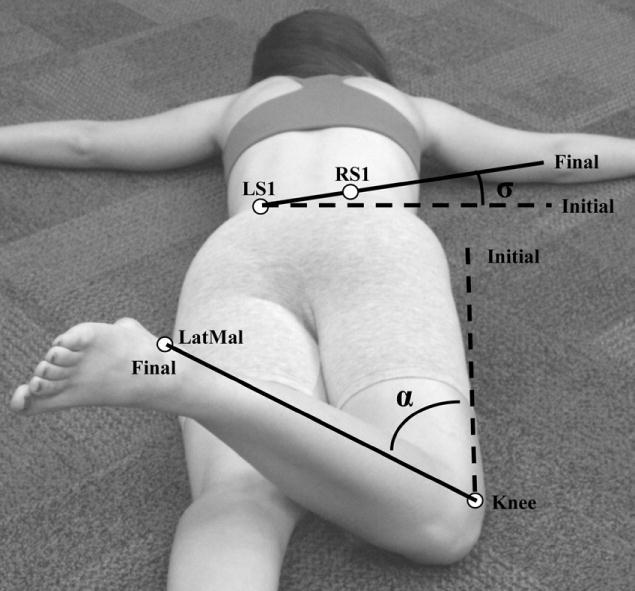
Kinematic model for calculating lower limb segment (α) and pelvic segment (σ) rotation. LS1: marker left of first sacral vertebra, RS1: marker right of first sacral vertebra, LatMal: lateral malleolus.
For each test of hip lateral and medial rotation, the angular displacement of the pelvic (σ) and lower leg (α) segments in the transverse plane were calculated between their initial and final positions (Figure 1). Lumbopelvic rotation range of motion (ROM) was represented by the rotation of the pelvic segment (σ) in the transverse plane. Hip rotation was calculated by subtracting pelvic rotation (σ) from rotation of the lower leg (α). To provide an indication of lumbopelvic timing, the amount of hip rotation completed at the onset of pelvic segment rotation was calculated. Data for the left and right sides were averaged for each subject. For data analysis, hip and lumbopelvic rotation values were converted so that positive values consistently reflected rotation in the direction of the limb, independent of the hip test or leg involved. Good reliability has been documented for these measures using a similar marker set (Gombatto et al., 2006). For lumbopelvic rotation, Gombatto et al (2006) reported intraclass correlation coefficients (3,1) of 0.80 (right) and 0.82 (left), and standard error of the measurement values of 0.8° (both right and left sides). For hip lateral rotation, they reported intraclass correlation coefficients (3,1) of 0.97 (right) and 0.99 (left), and standard error of the measurement values of 1.4° (right) and 1.5° (left).
Data Analysis
Independent-samples t-tests and chi-square tests for independence were used to compare demographic and baseline characteristics between treatment groups. A 2 × 2 mixed model analysis of variance (ANOVA) was conducted to explore the effect of time (between pre- and post-treatment laboratory visits) and treatment group on lumbopelvic rotation ROM, the amount of hip rotation completed before the onset of lumbopelvic rotation, and hip rotation ROM. The amount of hip rotation completed before the onset of lumbopelvic rotation was calculated to determine whether lumbopelvic motion occurred relatively early or late with respect to hip movement (i.e., smaller amounts of hip rotation completed before the onset of lumbopelvic rotation indicate earlier motion of the lumbopelvic region). Lumbopelvic rotation ROM and the amount of hip rotation completed before the onset of lumbopelvic rotation were the primary dependent variables of interest and were analyzed to determine if the change in lumbopelvic movement pattern was different between treatment conditions. Hip rotation ROM was also measured and analyzed to determine whether changes in the lumbopelvic movement pattern could be attributed to changes in total hip rotation ROM. Partial eta squared (η2) values were calculated to estimate effect size and were interpreted as follows: small η2=0.01, medium η2=0.06, and large η2=0.14 (Cohen, 1988). Partial eta squared represents the variance in the dependent variable explained by the effect of interest divided by variance explained by the effect of interest plus error variance (Tabachnick and Fidell, 2007). In this case, the effect of interest was the interaction of time and treatment group. When interactions between time and treatment group were found, paired-samples t-tests were then used to examine change in the dependent variables between pre- and post-treatment collection within each treatment group. All tests were two-tailed with alpha set at 0.05.
Results
Subject Characteristics
There were no significant differences in baseline demographic variables, LBP history, symptom behavior, and LBP subgroup distribution between treatment groups (P > 0.05) (Table 1).
Table 1.
Subject characteristics.
| Classification-specific (N=16) | Non-specific (N=16) | |||
|---|---|---|---|---|
| Mean | (SEM) | Mean | (SEM) | |
| % Female | 56.3 | (NA) | 50.0 | (NA) |
| Age (years) | 44.38 | (2.59) | 40.25 | (3.17) |
| Height (cm) | 172.50 | (3.01) | 170.46 | (2.24) |
| Weight (kg) | 76.75 | (3.48) | 76.59 | (2.71) |
| BMI (kg/m2) | 25.65 | (0.64) | 26.24 | (0.57) |
| Modified Oswestrya | 21.00 | (1.87) | 21.88 | (2.17) |
| LBPb Onset (years) | 12.70c | (2.46) | 9.91 | (1.96) |
| Current paind | 3.09 | (0.44) | 3.09 | (0.52) |
| Average paind | 3.91 | (0.40) | 3.50 | (0.43) |
| % Rotation | 62.5 | (NA) | 62.5 | (NA) |
0-100%,
LBP = low back pain,
N=15, one missing value
0-10 verbal numeric rating scale
Lumbopelvic Rotation ROM
There was a significant interaction between time and treatment group for lumbopelvic rotation ROM with both hip lateral and medial rotation (lateral: F (1,30) = 18.33, P < 0.001; η2 = 0.38; medial: F (1,30) = 19.67, P < 0.001; η2 = 0.40). For both directions of hip rotation, the Specific group significantly decreased lumbopelvic rotation ROM after treatment (pre-treatment minus post-treatment values, lateral: mean difference = 2.84 ± 0.80° (standard error of the mean), t (15) = 3.57, P = 0.003; medial: mean difference = 4.52 ± 1.23°, t (15) = 3.67, P = 0.002). The Non-Specific group significantly increased lumbopelvic rotation ROM after treatment for both directions of hip rotation (lateral: mean difference = -1.10 ± 0.46°, t (15) = -2.38, P = 0.03; medial: mean difference = -1.80 ± 0.72°, t (15) = -2.52, P = 0.02) (Figure 2).
Figure 2.
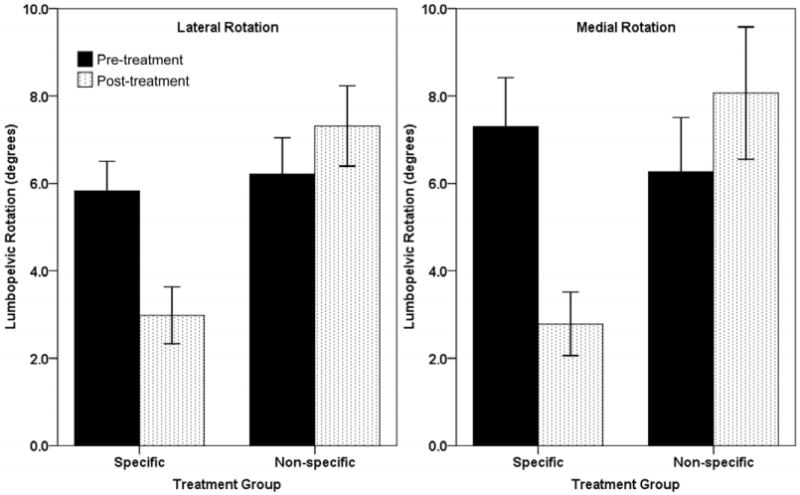
Lumbopelvic rotation range of motion in degrees (means ± standard errors) for each treatment group pre- and post-treatment.
Hip Rotation Completed Before the Onset of Lumbopelvic Rotation
There was a significant interaction between time and treatment group for the amount of hip rotation completed before the onset of lumbopelvic rotation with both hip lateral and medial rotation (lateral: F (1,30) = 5.73, P = 0.02; η2 = 0.16; medial: F (1,30) = 11.46, P = 0.002; η2 = 0.28). The Specific treatment group significantly increased the amount of hip rotation completed before the onset of lumbopelvic rotation for both hip lateral and medial rotation (lateral: mean difference = -8.78 ± 2.44°, t (15) = -3.60, P = 0.003; medial: mean difference = -8.26 ± 2.77°, t (15) = -2.98, P = 0.009). The Non-Specific treatment group did not change the amount of hip rotation completed before the onset of lumbopelvic rotation between pre and post-treatment laboratory visits for either direction of hip rotation (lateral: mean difference = -0.41 ± 2.50°, t (15) = -0.16, P = 0.87; medial: mean difference = 1.88 ± 1.13°, t (15) = 1.66, P = 0.12) (Figure 3).
Figure 3.
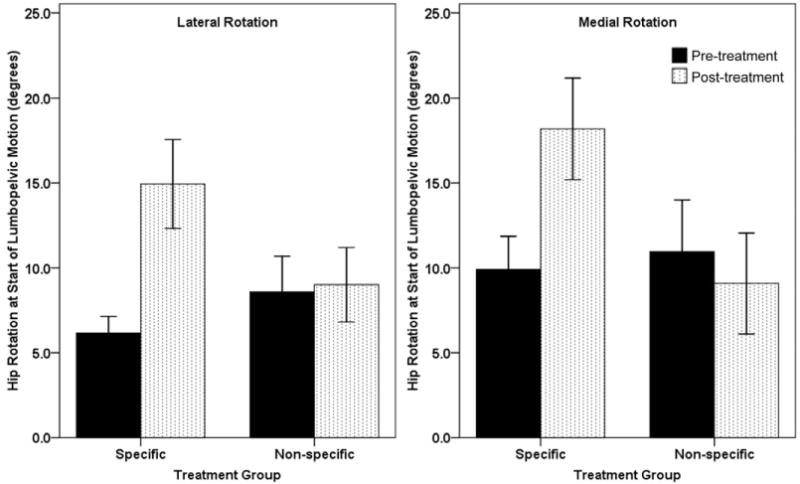
Hip rotation completed at the onset of lumbopelvic rotation (means ± standard errors) for each treatment group pre- and post-treatment.
Hip Rotation ROM
During hip lateral rotation, there was a significant interaction between time and treatment group for hip rotation ROM (F (1,30) = 5.96, P = 0.02; η2 = 0.17). However, there were no significant changes in hip lateral rotation ROM between laboratory visits for either treatment group (Specific: mean difference = 3.30 ± 1.71°, t (15) = 1.94, P = 0.07; Non-Specific: mean difference = -1.90 ± 1.27°, t (15) = -1.49, P = 0.16). During hip medial rotation, there was no interaction between time and treatment group, and no main effect of time or treatment group, for hip rotation ROM (P > 0.05) (Figure 4).
Figure 4.
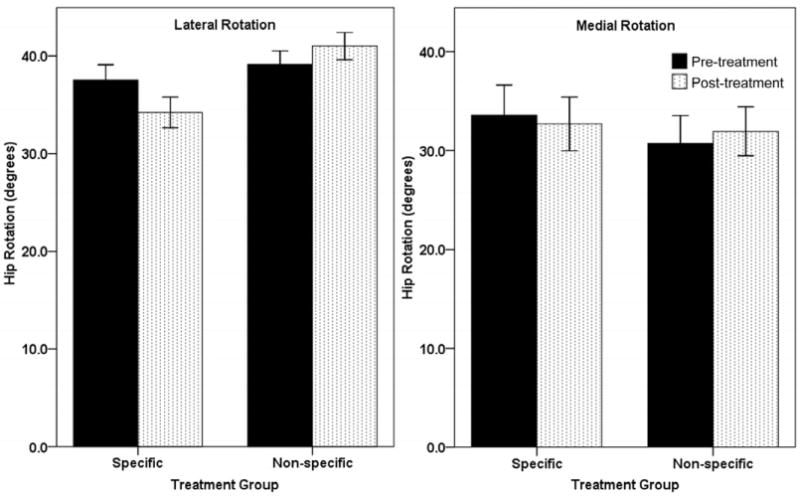
Hip rotation range of motion in degrees (means ± standard errors) for each treatment group pre- and post-treatment.
Discussion
The purpose of the current study was to compare the effect of two physical therapy treatments for LBP on lumbopelvic movement patterns with hip lateral and medial rotation. Subjects in the Specific group demonstrated significant improvements in lumbopelvic movement patterns during hip rotation, including both decreased lumbopelvic rotation ROM and the completion of more hip rotation before the onset of lumbopelvic rotation. In contrast, subjects in the Non-Specific group demonstrated increased lumbopelvic rotation ROM and no change in the amount of hip rotation completed before the onset of lumbopelvic rotation. Because there were no significant changes in hip lateral or medial rotation ROM, subjects were not likely limiting hip rotation as a strategy to limit lumbopelvic motion. The results of this study are important because they (1) demonstrate the ability of people with LBP to improve lumbopelvic movement patterns after the completion of treatment and without immediate guidance, and (2) demonstrate that LBP classification-specific exercise and instruction reduces lumbopelvic motion, whereas generalized strength and flexibility exercise does not reduce lumbopelvic motion. Additionally, these results provide data for lumbopelvic movement patterns with hip medial rotation in people with LBP, which has not previously been reported.
Previous studies have documented lumbopelvic motion with hip lateral rotation and have associated this motion with LBP (Gombatto et al., 2006; Scholtes et al., 2009; Scholtes and Van Dillen, 2007). In the current study, we also documented lumbopelvic motion during hip medial rotation in people with LBP. Although data for lumbopelvic motion with hip medial rotation in people without LBP are not available, the similar amounts of lumbopelvic rotation ROM and points in the range of hip rotation when lumbopelvic motion began, as well as the patterns of change following treatment, with both hip lateral and medial rotation suggest a generalized decrease in lumbopelvic control in people with LBP. Several investigators have demonstrated increased or early lumbopelvic motion with other clinical tests of trunk and limb movements in people with LBP compared to people without LBP (Esola et al., 1996; Luomajoki et al., 2008; McClure et al., 1997). In fact, one study documented that decreased control of lumbopelvic motion with clinical tests of limb movement was predictive of LBP development (Roussel et al., 2009). The results of this study contribute to the growing body of evidence suggesting that lumbopelvic motion may play a significant role in the development or course of a LBP problem.
Improving lumbopelvic movement patterns by reducing lumbopelvic motion with trunk and limb movements could be an important component of rehabilitative and preventative treatment of LBP. Studies have shown that within a session, when pain-producing lumbopelvic motion is manually restricted during limb movements, low back pain symptoms are decreased or eliminated in most people (Van Dillen et al., 2003a; Van Dillen et al., 2009). Healthy people familiar with stabilization training are able to limit lumbopelvic motion during supine hip flexion within a session following both verbal instruction and tactile feedback (Elia et al., 1996). Scholtes et al (2010) showed that people with LBP can also limit lumbopelvic motion with hip lateral rotation within a treatment session following verbal and tactile instruction. However, the Scholtes et al (2010) study additionally demonstrated that people with LBP do not appear to limit lumbopelvic motion as well as people without LBP within a session. Potentially, proprioceptive deficits that have been identified in people with LBP (Brumagne et al., 2000; O'Sullivan et al., 2003) could make it more difficult for them to refine their movement patterns, particularly over time. The current study, however, demonstrates that people with LBP can reduce lumbopelvic motion that may be contributing to their LBP 1) after the conclusion of treatment and 2) outside of the direct supervision of their treating therapist.
These data also provide evidence that people with LBP require specific instruction in order to improve particular movement patterns. In this study, classification-specific instruction resulted in a reduction of lumbopelvic motion with hip rotation in both lateral and medial directions, whereas non-specific instruction that included flexibility and strength training did not. The inability to improve lumbopelvic movement patterns with flexibility training is supported by research on healthy subjects who demonstrated no change in hip or lumbar motion during early forward bending following a 3-week hamstring stretching program (Li et al., 1996). While muscle length or strength could contribute to the presence of certain movement patterns (Sahrmann, 2002), the results of the current study suggest that simply addressing flexibility and strength limitations may not be enough to achieve improvement in the movement pattern. In fact, in this study, non-specific treatment that involved flexibility and strength training significantly increased lumbopelvic motion and did not have an effect on where in the range of hip rotation lumbopelvic motion began. If repeated early or excessive lumbopelvic motion is a factor in the development or course of low back pain, as previous authors have proposed (Adams et al., 2002; McGill, 1997; Sahrmann, 2002), and if minimizing lumbopelvic motion is important for reducing LBP symptoms in the long-term as it is in the short-term (Van Dillen et al., 2003a; Van Dillen et al., 2009), then this study suggests that specific training is a necessary component of treatment. Improvements in lumbopelvic motion are not achieved with non-specific treatment.
The degrees of change in lumbopelvic rotation ROM and hip rotation completed before the onset of lumbopelvic rotation for the Specific group may appear small. However, changes in lumbopelvic rotation ROM and hip rotation at the onset of lumbopelvic rotation during both hip lateral and medial rotation for the Specific group clearly exceed the standard errors of the measurement based on the Gombatto et al (2006) study. Additionally, these changes exceed the minimal detectable changes calculated at the 95% confidence interval (lumbopelvic rotation ROM: ± 2.22°; hip rotation at the onset of lumbopelvic rotation: ± 4.16°) using the standard errors of the measurement from the Gombatto et al (2006) study and methods outlined by Stratford et al (1996).
The fact that data for pain and functional disability post-treatment are not included in this study may be viewed as a limitation. We feel that inclusion of such data would not be appropriate because the subjects in this study were participants in a larger randomized clinical trial with multiple treatment components. Many factors, not only the modification of lumbopelvic motion with hip rotation specifically, could have influenced pain and functional disability outcomes for either subgroup.
We recognize that testing a movement prescribed to the Specific group as an exercise could also be considered a limitation of this study. It is logical for the Specific group, who was trained in the movement, to demonstrate improvement in lumbopelvic movement patterns after treatment. However, to our knowledge, no prior studies have tested the effect of specific movement training on lumbopelvic movement patterns in people with low back pain outside of a single treatment session. People with low back pain have demonstrated proprioceptive deficits (Brumagne et al., 2000; O'Sullivan et al., 2003) and a decreased ability to improve lumbopelvic movement patterns within a physical therapy session compared to people without low back pain (Scholtes 2010). Due to the habitual or automatic nature of movement and the proprioceptive awareness required to limit lumbopelvic motion during movement, it should not be assumed that people with low back pain have the ability to change movement patterns that may be contributing to their pain outside of a single treatment session or without the immediate guidance of their physical therapist, even if they are trained in that specific movement. Furthermore, the effects of commonly cited and practiced physical therapy treatment components, such as those prescribed in the Non-Specific condition, on lumbopelvic movement patterns were previously unknown. Finally, it is possible that the results of this study may be an effect of the Specific treatment as a whole. All subjects in the Specific group were given other exercises, functional training, and education with the aim of minimizing lumbopelvic motion. It is not known from the current study whether changes in lumbopelvic movement patterns during a specifically trained movement transfer to changes in lumbopelvic movement patterns during novel movements, and activities of daily living, in particular. Investigations of such questions are currently being conducted.
Conclusion
People with chronic LBP who received individualized classification-specific treatment emphasizing minimizing lumbopelvic motion demonstrated improved control of lumbopelvic motion with hip lateral and medial rotation after treatment. They demonstrated a decreased amount of lumbopelvic motion and later onset of lumbopelvic motion during both directions of hip rotation. In contrast, people who received generalized non-specific treatment emphasizing strength and flexibility demonstrated increased lumbopelvic motion and no change in the amount of hip rotation completed before the onset of lumbopelvic motion following treatment. These results demonstrate that people with chronic LBP are able to improve lumbopelvic movement patterns that may be contributing to their pain following treatment and without guidance.
Furthermore, the results suggest that classification-specific exercise and instruction, rather than non-specific exercise and instruction, for LBP results in improved lumbopelvic movement patterns.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams MA, Bogduk N, Burton K, Dolan P. The Biomechanics of Back Pain. 1st. Edinburgh: Churchill Livingstone; 2002. [Google Scholar]
- Brumagne S, Cordo P, Lysens R, Verschueren S, Swinnen S. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine. 2000;25(8):989–94. doi: 10.1097/00007632-200004150-00015. [DOI] [PubMed] [Google Scholar]
- Burnett AF, Cornelius MW, Dankaerts W, O'Sullivan PB. Spinal kinematics and trunk muscle activity in cyclists: a comparison between healthy controls and non-specific chronic low back pain subjects-a pilot investigation. Manual Therapy. 2004;9(4):211–9. doi: 10.1016/j.math.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale: Lawrence Erlbaum Associates, Inc.; 1988. The analysis of variance; pp. 273–406. [Google Scholar]
- Deyo RA, Andersson G, Bombardier C, et al. Outcome measures for studying patients with low back pain. Spine. 1994;19(18 Suppl):2032S–6S. doi: 10.1097/00007632-199409151-00003. [DOI] [PubMed] [Google Scholar]
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Annals of the Rheumatic Diseases. 1978;37(4):378–81. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elia DS, Bohannon RW, Cameron D, Albro RC. Dynamic pelvic stabilization during hip flexion: A comparison study. Journal of Orthopaedic and Sports Physical Therapy. 1996;24(1):30–6. doi: 10.2519/jospt.1996.24.1.30. [DOI] [PubMed] [Google Scholar]
- Esola MA, McClure PW, Fitzgerald GK, Siegler S. Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine. 1996;21(1):71–8. doi: 10.1097/00007632-199601010-00017. [DOI] [PubMed] [Google Scholar]
- Friedrich M, Cermak T, Maderbacher P. The effect of brochure use versus therapist teaching on patients performing therapeutic exercise and on changes in impairment status. Physical Therapy. 1996;76(10):1082–8. doi: 10.1093/ptj/76.10.1082. [DOI] [PubMed] [Google Scholar]
- Friedrich M, Gittler G, Halberstadt Y, Cermak T, Heiller I. Combined exercise and motivation program: effect on the compliance and level of disability of patients with chronic low back pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 1998;79(5):475–87. doi: 10.1016/s0003-9993(98)90059-4. [DOI] [PubMed] [Google Scholar]
- Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Physical Therapy. 2001;81(2):776–8. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- Gombatto SP, Collins DR, Sahrmann SA, Engsberg JR, Van Dillen LR. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clinical Biomechanics. 2006;21(3):263–71. doi: 10.1016/j.clinbiomech.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Harris-Hayes M, Van Dillen LR. Inter-tester reliability of physical therapists classifying low back pain problems based on the movement system impairment classification system. Physical Medicine and Rehabilitation. 2009;1(2):117–26. doi: 10.1016/j.pmrj.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry SM, Van Dillen LR, Trombley AL, Dee JM, Bunn JY. Reliability of the movement system impairment classification schema for subgrouping people with low back pain. Journal of Orthopedic and Sports Physical Therapy. 2009;39:A97. [Google Scholar]
- Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58(3):387–92. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- Li Y, McClure PW, Pratt N. The effect of hamstring muscle stretching on standing posture and on lumbar and hip motions during forward bending. Physical Therapy. 1996;76(8):836–45. doi: 10.1093/ptj/76.8.836. [DOI] [PubMed] [Google Scholar]
- Luomajoki H, Kool J, de Bruin ED, Airaksinen O. Movement control tests of the low back; evaluation of the difference between patients with low back pain and healthy controls. BMC Musculoskeletal Disorders. 2008;9:170–81. doi: 10.1186/1471-2474-9-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannion AF, Muntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24(23):2435–8. doi: 10.1097/00007632-199912010-00004. [DOI] [PubMed] [Google Scholar]
- McClure PW, Esola M, Schreier R, Siegler S. Kinematic analysis of lumbar and hip motion while rising from a forward, flexed position in patients with and without a history of low back pain. Spine. 1997;22(5):552–8. doi: 10.1097/00007632-199703010-00019. [DOI] [PubMed] [Google Scholar]
- McGill SM. The biomechanics of low back injury: implications on current practice in industry and the clinic. Journal of Biomechanics. 1997;30(5):465–75. doi: 10.1016/s0021-9290(96)00172-8. [DOI] [PubMed] [Google Scholar]
- Melnick M, Saunders HD, Saunders R. Managing Back Pain. Chaska, MN: The Saunders Group Incorporated; 1998. [Google Scholar]
- Moffett JK, Torgerson D, Bell-Syer S, et al. Randomized controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. British Medical Journal. 1999;319(7205):279–83. doi: 10.1136/bmj.319.7205.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton BJ, Sahrmann SA, Van Dillen LR. Differences in measurements of lumbar curvature related to gender and low back pain. Journal of Orthopaedic and Sports Physical Therapy. 2004;34(9):524–34. doi: 10.2519/jospt.2004.34.9.524. [DOI] [PubMed] [Google Scholar]
- O'Sullivan PB, Burnett A, Floyd AN, et al. Lumbar repositioning deficit in a specific low back pain population. Spine. 2003;28(10):1074–9. doi: 10.1097/01.BRS.0000061990.56113.6F. [DOI] [PubMed] [Google Scholar]
- Roussel N, Nijs J, Truijen S, Mottram S, Van Moorsel A, Stassijns G. Altered lumbopelvic movement control but not generalized joint hypermobility is associated with increased injury in dancers: A prospective study. Manual Therapy. 2009;14(6):630–5. doi: 10.1016/j.math.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. 1st. St. Louis, MO: Mosby, Inc.; 2002. [Google Scholar]
- Scholtes SA, Norton BJ, Lang CE, Van Dillen LR. The effect of within-session instruction on lumbopelvic motion during a lower limb movement in people with and people without low back pain. Manual Therapy. 2010 doi: 10.1016/j.math.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholtes SA, Gombatto SP, Van Dillen LR. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clinical Biomechanics. 2009;24(1):7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholtes SA, Van Dillen LR. Gender-related differences in prevalence of lumbopelvic region movement impairments in people with low back pain. Journal of Orthopaedic and Sports Physical Therapy. 2007;37(12):744–53. doi: 10.2519/jospt.2007.2610. [DOI] [PubMed] [Google Scholar]
- Shum GLK, Crosbie J, Lee RYW. Symptomatic and asymptomatic movement coordination of the lumbar spine and hip during an everyday activity. Spine. 2005;30(23):E697–E702. doi: 10.1097/01.brs.0000188255.10759.7a. [DOI] [PubMed] [Google Scholar]
- Stratford PW, Binkley J, Gill C, Moreland J. Using the Roland-Morris questionnaire to make decisions about individual patients. Physiotherapy Canada. 1996;48(2):107–10. [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th. Boston, MA: Pearson Education Inc; 2007. Review of univariate and bivariate statistics; pp. 33–59. [Google Scholar]
- Taimela S, Diederich C, Hubsch M, Heinricy M. The role of physical exercise and inactivity in pain recurrence and absenteeism from work after active outpatient rehabilitation for recurrent or chronic low back pain: a follow-up study. Spine. 2000;25(14):1809–16. doi: 10.1097/00007632-200007150-00012. [DOI] [PubMed] [Google Scholar]
- Torstensen TA, Ljunggren AE, Meen HD, Odland E, Mowinckel P, Geijerstam S. Efficiency and costs of medical exercise therapy, conventional physiotherapy, and self-exercise in patients with chronic low back pain. A pragmatic, randomized, single-blinded, controlled trial with 1-year follow-up. Spine. 1998;23(23):2616–24. doi: 10.1097/00007632-199812010-00017. [DOI] [PubMed] [Google Scholar]
- Trudelle-Jackson E, Sarvaiya-Shah SA, Wang SS. Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with chronic low back pain. Journal of Orthopaedic and Sports Physical Therapy. 2008;38(6):371–6. doi: 10.2519/jospt.2008.2760. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. Physical Therapy. 1998;78(9):979–88. doi: 10.1093/ptj/78.9.979. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Archives of Physical Medicine and Rehabilitation. 2003a;84(3):313–22. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. Movement system impairment-based categories for low back pain: stage 1 validation. Journal of Orthopaedic and Sports Physical Therapy. 2003b;33(3):126–42. doi: 10.2519/jospt.2003.33.3.126. [DOI] [PubMed] [Google Scholar]
- Van Dillen LR, Maluf KS, Sahrmann SA. Further examination of modifying patient-preferred movement and alignment strategies in patients with low back pain during symptomatic tests. Manual Therapy. 2009;14(1):52–60. doi: 10.1016/j.math.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Korff M. Studying the natural history of back pain. Spine. 1994;19(Suppl 18):2041S–6S. doi: 10.1097/00007632-199409151-00005. [DOI] [PubMed] [Google Scholar]
- Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine. 1980;5(2):117–25. doi: 10.1097/00007632-198003000-00005. [DOI] [PubMed] [Google Scholar]
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- Winter DA. Biomechanics and motor control of human movement. 3rd. Hoboken, NJ: John Wiley & Sons; 2005. [Google Scholar]


