Abstract
Wearing complete dentures can be an extremely uncomfortable experience for the people with Xerostomia. Various treatment modalities have been suggested in the literature to overcome the problem of xerostomia in complete denture patients. Incorporating reservoirs containing salivary substitutes, into dentures, is one of these treatment modalities. This paper presents case report of a patient suffering from xerostomia who was successfully treated with a new form of reservoir dentures. This new split denture technique resulted in a reservoir denture that provided good lubrication of the oral tissues, was easily cleaned by the wearer and was produced from routine denture materials. Details of its design, construction and other potential applications are also presented.
Keywords: Xerostomia, Reservoir, Split denture
Introduction
Xerostomia is a common clinical condition characterized not only by the dry mouth, but also by difficulty in normal oral and oropharyngeal functions. Extreme discomfort in wearing dentures is a common complaint associated with it. Xerostomia has many possible causes associated with it such as old age, anxiety, depression, salivary gland diseases, sjogren’s syndrome, medication––related side effects, head and neck radiation and medically compromised conditions like diabetes mellitus [1, 2]. Medications are the most common cause associated with xerostomia [3, 4].
A variety of approaches have been used to supply xerostomic patients with a moist oral environment. These include, increasing the frequency of water intake, changing dietary habits by including more citrus fruits in the diet, salivary stimulants which include sugar free chewing gums or lozenges [5]. In severe xerostomic patients, salivary substitutes may be utilized. One method of using salivary substitutes is incorporating salivary reservoir in the dentures like palatal reservoir and reservoir in mandibular complete denture [6, 7]. In case of medication induced xerostomia, after discussion with patient’s physician the timing, dosage or a change in medication may reduce the severity of the problem.
This paper presents the case report of a xerostomic patient who was successfully treated with a new form of reservoir denture where all other treatment modalities had failed. A method for fabricating mandibular reservoir denture is presented.
Clinical Report
A 63 years old female patient reported to the department of prosthodontics, D.A.V. (C) Dental College, Yamuna Nagar, Haryana with chief complaint of difficulty in wearing old dentures associated with dryness of mouth and throat. She had to drink water number of times in the night leading to a restless sleep.
Patient reported with a medical history of asthma and hypertension from last 5–6 years and diabetes from last 10–12 yrs. The patient was on medications for the same. Patient was a denture wearer from last one year and had chronic irritation from them associated with soreness and burning sensation especially with the lower denture.
On clinical examination, completely edentulous upper and lower ridges with dry, thin and friable mucosa were observed. Old dentures appeared to be satisfactory when examined. After a number of unsuccessful adjustments of the existing dentures, it was decided to fabricate a new set of maxillary and mandibular dentures with salivary reservoir incorporated in mandibular denture.
This clinical report describes a technique for the fabrication of split mandibular denture that was selected as a treatment modality for the patient.
Technique
The split denture was fabricated in four steps: preparatory stage; construction of clear acrylic mandibular base section; construction of pink acrylic teeth section; and denture delivery with reservoir placement.
Preparatory Stage
Primary and secondary impressions of maxillary and mandibular residual ridges were made using conventional techniques.
The master casts obtained were marked as No. 1 models. The master casts were duplicated using reversible hydrocolloid impression material (Neoloid, Neoloy products Co., Illinosis) and poured in dental stone (Gypstone type III, Dentpro Pvt. Ltd., Jammu). The duplicated models were then marked No. 2 models. The maxillo-mandibular relationship was recorded with mandible in a retruded position and acceptable freeway space. No. 1 models were then articulated and teeth arrangement was done. No. 2 models were articulated using same jaw relation record. Shorter teeth were selected for mandibular denture to have a deeper area for future placement of reservoir. The trial was done to patient’s satisfaction.
Construction of the Clear Acrylic Mandibular Base Section
Mandibular trial denture was kept aside and wax up for base section was done on the mandibular cast on No. 2 model. The distance between the upper margin of the waxed up base segment and upper teeth should be length of mandibular teeth + 3 mm for adequate thickness of acrylic. The wax up was kept smooth, with the occlusal surface as flat as possible with clearly defined occlusal edges. Attachment screws were kept in place, two in molar region on both sides and one in anterior region. They were placed exactly in the center of the waxed up base section and kept parallel to each other (Fig. 1). These were incorporated to help in fitting two segments of the denture that is clear acrylic base section and pink acrylic teeth section together. Putty index was made with impression of maxillary teeth on one side and impression of attachment screws on the other side for reorientation.
Fig. 1.
Wax up for clear acrylic base section with attachment screws in place
This wax up for base section along with attachment screws was flasked and packed in the normal manner. Once the de-waxing was done, the attachment screws were removed to duplicate them in clear acrylic resin. After applying separating medium, the flask was packed with clear heat cure acrylic resin. Care was taken in polishing to ensure that the square occlusal edges were maintained to get good fit of the two segments (Fig. 2).
Fig. 2.
Waxed up base segment duplicated in clear heat cure acrylic resin
Construction of Pink Acrylic Teeth Segment
A duplicate of clear acrylic base section was made using reversible hydrocolloid impression material and poured in dental stone.
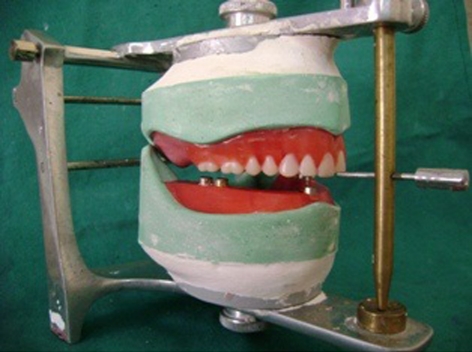
The maxillary trial denture was kept in place on No. 1 model and articulated with the duplicated stone model of the mandibular clear acrylic base section with the help of putty index made earlier for reorientation (Fig. 3). Mandibular denture teeth were waxed up on the duplicate of clear acrylic base section and occlusion was checked (Fig. 4). The waxed up teeth section was then flasked and processed in pink heat cure acrylic resin. After careful deflasking, the pink acrylic teeth segment of the mandibular denture was attached to clear acrylic base segment for polishing. The two sections should ‘click’ into place at this point. All polishing was done with the both segments together to ensure a flush, smooth finish and no damage to edges. The result was a full lower denture with a clear acrylic base and a removable pink acrylic teeth segment.
Fig. 3.
Base section articulated in place and replaced with its stone model
Fig. 4.
Mandibular teeth in occlusion with maxillary trial denture
Denture Delivery and Reservoir Placement
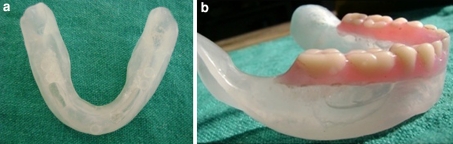
The dentures, still with no reservoirs, were now issued to the patient and worn for a time to allow the patient to adjust and complete any minor adjustments. After one week, reservoirs were cut into the clear acrylic base segment of the mandibular denture in premolar region on both sides using acrylic trimmer. Since the internal surfaces of the reservoirs cannot be polished, they were cut as clearly and smoothly as possible to facilitate easy cleaning (Fig. 5a).
Fig. 5.
a Reservoir made in clear acrylic base section. b Artificial saliva placed in reservoir and two segments fitted together
Reservoirs were placed in each posterior segment in the premolar region. The reservoirs were made as large as possible while maintaining sufficient thickness of denture walls for strength. A minimum thickness of 2 mm was maintained for reservoir walls.
As the base section was made up of clear acrylic, extent of the reservoir can be easily visualized (Fig. 5b). A 0.5 mm diameter round bur was used to drill a drainage hole from the inferior aspect of lingual flange of the denture into the reservoirs on both sides. The patient was told to separate the two segments and fill the reservoir with artificial saliva. The artificial saliva used in this case was “wet mouth” (carboxymethylcellulose). The split denture was now reissued to the patient and post-operative instructions were given to the patient (Fig. 6). Patient was kept on recall appointments of 1 week, 3 weeks, 3 months and after 6 months. During the follow up appointments size of the drainage hole was adjusted to ensure the flow of saliva up to minimum of 3–4 h. Patient had to refill the reservoir after 3–4 h. Patient found a great relief in her symptoms of dry mouth and was satisfied with the denture.
Fig. 6.
Post-operative intraoral view
Discussion
A variety of approaches has been described in the literature for incorporating salivary reservoir in complete dentures. All of them have varying degree of success. The split denture has added advantage over other techniques of incorporating reservoir like ready access to the reservoir, easy cleaning and adjustment of the reservoir as needed. Use of clear acrylic for the base segment helps the clinician to determine the size and position for placement of the reservoir. Also it enables the patient to clearly visualize the level of salivary substitute within the chamber.
However this method also has some disadvantages associated with it like laboratory stages are time consuming and precision is essential to ensure accurate and smoothly fitting segments. Additionally, repairs and relines of the split denture become complex.
The case selection is also an important criterion for construction of split denture. There should be sufficient vertical dimension for placement of reservoir. Patients must have manual dexterity to separate and rejoin the two segments of the split denture. Minimal undercuts should be present in the mandibular denture base area for reseating of the clear acrylic base section.
Summary and Conclusion
The split denture technique has helped the patient a lot in overcoming her problems associated with dry mouth. She had been wearing it from last one year and finds it easy to use, clean and had great relief in her symptoms of xerostomia. The split denture technique can be modified to use in maxillary dentures. Further improvement in the technique could be the use of precision attachments in place of attachment screws.
Footnotes
The article was presented at P G Conference held at Bangalore in 2008.
References
- 1.Greenspan D. Oral complications of cancer therapies, management of salivary dysfunction. NCI Monogr. 1990;9:159–161. [PubMed] [Google Scholar]
- 2.Moore PA, Orchard T. Type 1 diabetes mellitus, xerostomia and salivary flow rates. Oral Surg Oral Med Oral Path. 2001;92:281–291. doi: 10.1067/moe.2001.117815. [DOI] [PubMed] [Google Scholar]
- 3.Guggenheimer J, Moore PA. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003;134(1):61–69. doi: 10.14219/jada.archive.2003.0018. [DOI] [PubMed] [Google Scholar]
- 4.Davis AN. A comparison of artificial saliva and chewing gum in the management of xerostomia in patients with advanced cancer. Palliat Med. 2000;14:197–203. doi: 10.1191/026921600672294077. [DOI] [PubMed] [Google Scholar]
- 5.Sinclair GF, Frost PM. New design for an artificial salivary reservoir for the mandibular complete denture. J Prosthet Dent. 1996;75:276–280. doi: 10.1016/S0022-3913(96)90484-9. [DOI] [PubMed] [Google Scholar]
- 6.Hirvikangas M, Posh J, Makila E. Treatment of xerostomia through use of dentures containing reservoirs of saliva substitute. Proc Finn Dent Soc. 1989;85:47–50. [PubMed] [Google Scholar]
- 7.Locker D. Subjective reports of oral dryness in older adult population. Community Dent Oral Epidemiol. 1993;21:165–168. doi: 10.1111/j.1600-0528.1993.tb00744.x. [DOI] [PubMed] [Google Scholar]